Abstract
Six patients with a clinical diagnosis of chronic posterior cruciate ligament (PCL) rupture, based on a positive posterior drawer test, had a normal appearance of the PCL on an MRI scan. It is postulated that the PCL had been ruptured but healed in a lengthened state. 12 volunteers with no history of knee trauma underwent an MRI scan of the knee. In this control group (n _ 12), there was a close correlation between the lateral femoral condylar width in the sagittal plane and the PCL length, with a ratio of 2:1 (95% confidence interval (CI) _ 1.817–2.095). In the clinically abnormal group (n _ 6), the ratio was 1.49:1 (95% CI _ 1.206–1.782) (p< 0.0005). In conclusion, the ratio of the lateral femoral condylar width in the sagittal plane to the PCL length is a useful index for diagnosing PCL attenuation and lengthening in the presence of a normal morphological MR appearance.
The posterior cruciate ligament (PCL) is the prime stabiliser of the knee joint and acts as a central axis about which normal rotation occurs [12]. Biomechanical studies have shown that the PCL is the primary restraint to posterior translation [3–5], contributing 95% restraint to tibial displacement [6].
Rupture of the PCL is an uncommon injury occurring after high-energy trauma to the knee. The reported incidence of PCL rupture has varied, with PCL injuries representing between 1% and 44% of all knee ligament injuries in various studies [7–10]. Clinically, this is detected by a positive posterior drawer test or tibial sag. The accuracy of clinical examination for detecting PCL tear is reported to be 96% (sensitivity of 90% and specificity of 99%) [11]. The sensitivity and specificity of MRI in diagnosing acute PCL rupture reaches 100% [12–18], but is only 23% for chronic PCL injuries [19].
We identified six patients with an obvious clinical PCL rupture who had a normal MRI scan. We postulate that, as the ruptured PCL heals in a lengthened state, measurement of absolute PCL length will not give information about the functional status of the PCL. An osseous parameter would give a more reproducible measurement and a ratio may be derived by comparing it to the length of the chronically ruptured PCL. This study was designed to identify an osseous parameter in the knee on the MRI scan that would correlate with PCL length.
Methods and materials
Six patients (Group 1) with a clinical Grade III PCL rupture were identified retrospectively. These patients had sustained PCL injury over a period of 5 years. The clinical findings were unequivocally positive and were recorded on cine film. The cine films obtained were merely for demonstration purposes and were not used for the purpose of publication. In addition, all patients had stress radiographs of both knees showing that the tibia subluxed posteriorly on the femur. The scans were performed with the patient in the supine position, with the knee in 10° of flexion and 20° of external rotation. Images were obtained in the sagittal plane with 3 mm slices. All of the scans were reported as normal by an experienced musculoskeletal radiologist (S.E.), who was aware of the clinical findings.
A group of 12 volunteers (Group 2) who had no knee symptoms and no history of trauma to the knee were enlisted prospectively. Informed verbal consent was obtained after the nature of study was explained to these volunteers. Clinical examination in this group was normal. A single operator performed MRI scans of the unaffected knees on a pre-arranged day. MRI scan of their knees was performed according to the aforementioned protocol, and the same radiologist reported on the findings.
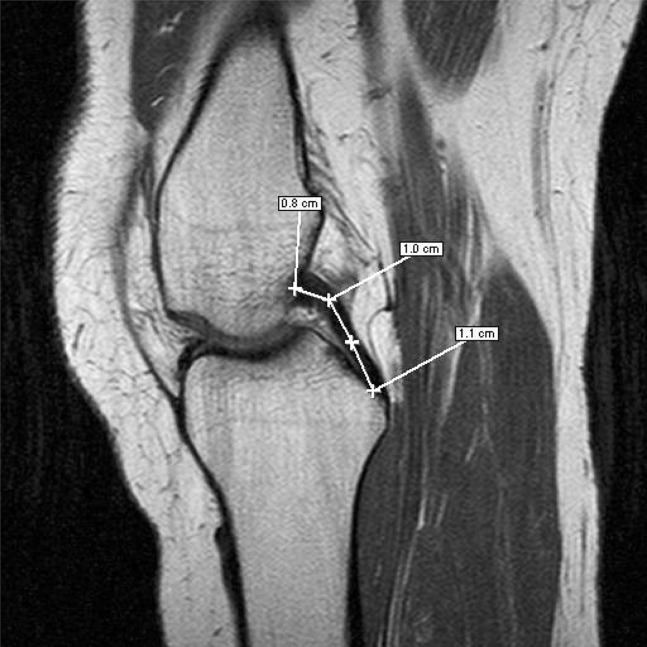
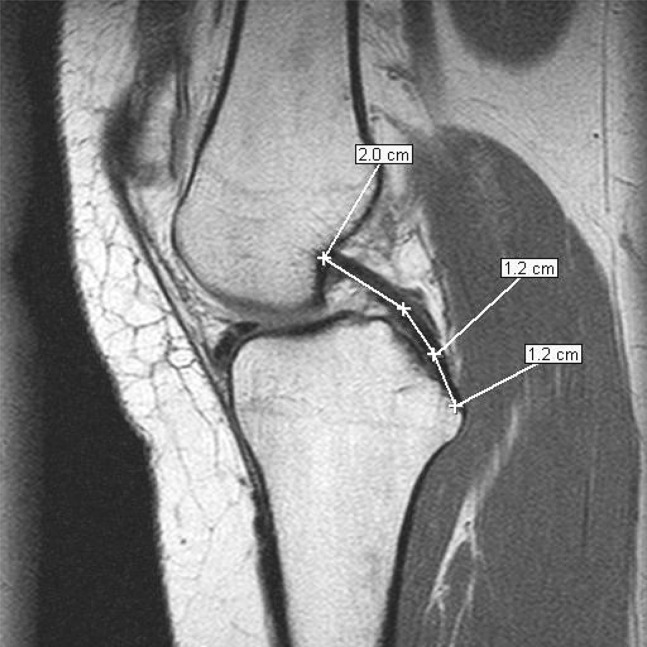
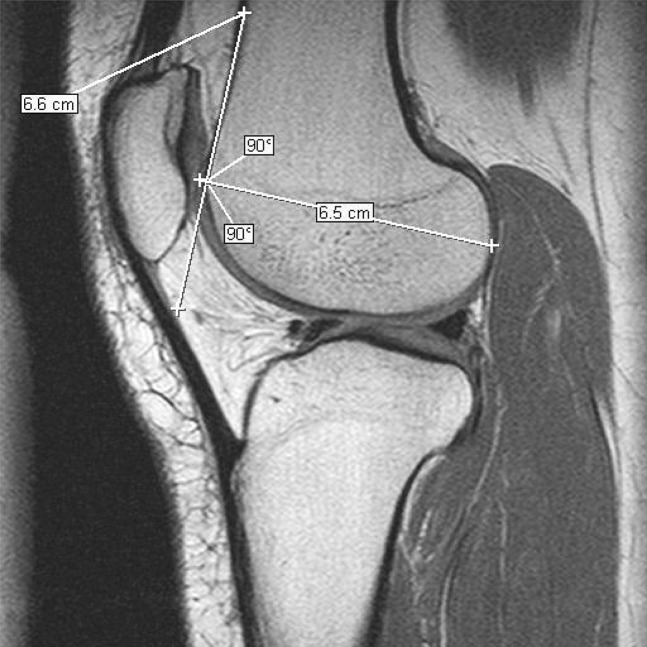
The scans were measured digitally with a software programme (eFilm Workstation, version 1.8.3®; Merge Healthcare, WI, USA). This software permits accurate readings of DICOM (Digital Imaging and Communication in Medicine) images. The PCL length was measured along a line in the median width of the ligament, from its origin to insertion, on the slice of the scan that showed the entire length of the PCL (see Figures 1 and 3). The lateral femoral condylar width was measured in the sagittal plane by a line tangential to the physeal scar and perpendicular to the anterior femoral cortex (see Figures 2 and 4). The sagittal slice chosen for measurement of the lateral femoral condoyle was widest in the anteroposterior plane (Figure 5). The ratio obtained between the lateral femoral condoyle width and the PCL length was calculated for each patient and compared between Groups 1 and 2. This ratio was chosen for calculations because the absolute PCL length varies between individuals according to gender and build of the person.
Figure 1.
Posterior cruciate ligament (PCL) length measurement: “normal” (Volunteer 3). This PCL measures 2.9 cm.
Figure 3.
Posterior cruciate ligament (PCL) length measurement: “abnormal” (Patient 5). This PCL measures 4.4 cm.
Figure 2.
Lateral femoral condyle width in sagittal image: “normal” (Volunteer 3).
Figure 4.
Lateral femoral condyle width in sagittal image: “abnormal” (Patient 5).
Figure 5.
Measuring the lateral femoral condoyle; the widest anteroposterior sagittal slice was chosen (slice 7 in this figure).
The first radiologist (S.E.) was aware of the clinical findings for qualitative reporting on the status of the PCL, but was blinded to all of the measurements. A second radiologist (N.H.) who was blinded to the clinical status of the two groups repeated all of the measurements.
Statistical analysis was performed using Graph Pad InStat software (Reed Business Information, AZ, USA). The ratios obtained were compared between two groups using an unpaired t-test. Normality of data was tested using the Kolmogrov and Smirnov method. Interobserver variations were compared.
Results
Table 1 shows the ratio of PCL length to lateral femoral condyle width of individual subjects in the two groups. The mean ratio of lateral femoral condylar width to PCL length in Group 1 was 1.49:1. The minimum ratio was 1.23 and the maximum ratio was 1.86. The 95% confidence interval (CI) was 1.27–1.70 (Table 2).
Table 1. Ratios between posterior cruciate ligament length and lateral femoral condylar width in two groups.
| Serial No. | Group 1 | Group 2 |
| 1 | 1.233 | 1.709 |
| 2 | 1.394 | 2.046 |
| 3 | 1.857 | 1.943 |
| 4 | 1.483 | 2.257 |
| 5 | 1.480 | 2.279 |
| 6 | 1.490 | 1.829 |
| 7 | 1.982 | |
| 8 | 1.752 | |
| 9 | 1.830 | |
| 10 | 1.879 | |
| 11 | 1.685 | |
| 12 | 2.279 |
Table 2. Comparison of posterior cruciate ligament length to lateral femoral condyle width ratios in two groups.
| Group 1 | Group 2 | |
| Mean | 1.49 | 1.96 |
| Minimum | 1.23 | 1.69 |
| Maximum | 1.86 | 2.28 |
| Median | 1.48 | 1.91 |
| 95% confidence interval | 1.27–1.70 | 1.82–2.09 |
In Group 2, the mean ratio of lateral femoral condylar width to PCL length was 1.96:1. The minimum ratio was 1.69 and the maximum ratio was 2.28. The 95% confidence interval was 1.82–2.09 (Table 2).
The ratios between the lateral femoral condyle width and PCL length in Groups 1 and 2 show significant statistical difference. The two-tailed p-value was 0.0005 (t _ 4.359 with 16 degrees of freedom). The difference between standard deviations in the two groups was not significant. The data passed the normality test using the Kolmogorov and Smirnov method.
The interobserver error between measurements of the two radiologists was not significant. The two-tailed p-value was 0.769. The 95% CI of the difference was –0.04237 to 0.03184, with a mean difference of −0.005263 (mean of paired differences).
Discussion
Conventional interpretation of MRI scans in PCL injury is by morphological appearance. Three normal appearances are identified: arcuate, U-shaped and kinked [14]. MRI is considered to be the most accurate modality for identifying PCL injury in acute cases [12–15] but its sensitivity is comparatively lower in chronic cases [19]. The diagnosis of an acute rupture is apparent from the abnormal morphological appearance of the PCL, including indistinct margins, abnormal thickening, increased signal intensity and focal areas of ligamentous discontinuity [13, 18]. In chronic cases, a torn PCL may reattach to the bone, the covering synovial sheath may repair without PCL healing or the PCL may repair in a lengthened state. In addition, increased signal intensity may be lost in the chronic situation. Shelbourne et al [20] reported that all low- and mid-grade PCL injuries healed and looked normal on follow up MRI scans at 3 months. In addition, the majority of high-grade injuries had healed and, although some had an altered contour, several had a normal contour. Our six cases fall into the latter category, i.e. the PCL looks normal but it is lengthened and consequently dysfunctional.
The reduction in the ratio of lateral femoral condylar width to PCL length indicates lengthening of the PCL. Anatomical studies have shown that the PCL averages 32–38 mm in length [2]. In view of the significant variation in knee size in the normal population, absolute PCL length in isolation was regarded as too inaccurate a method for diagnosing PCL injury [20]. In patients who have a clinically suspected PCL rupture, and who have a normal MRI scan, the lateral femoral condylar width should be measured. This will allow accurate correlation of the MRI scan with the clinical findings in cases of chronic PCL ruptures.
Acknowledgment
We acknowledge Dr Neil Hickey, Consultant Radiologist, Connolly Hospital Blanchardstown, Dublin.
References
- 1.Cain TE, Schwab GH. Performance of an athlete with straight posterior knee instability. Am J Sports Med 1981;9:203–8 [DOI] [PubMed] [Google Scholar]
- 2.Girgis FG, Marshall JL, Al Mongem ARS. The cruciate ligaments of knee joint: anatomical, functional and experimental analysis. Clin Orthop 1975;106:216–31 [DOI] [PubMed] [Google Scholar]
- 3.Gollehon DL, Torzilli PA, Warren PA. The role of posterolateral and cruciate ligaments in the stability of human knee. J Bone Joint Surg Am 1987;69A:233–42 [PubMed] [Google Scholar]
- 4.Grood ES, Stowers SF, Noyes FR. Limits of movement in human knee. Effect of sectioning the posterior cruciate ligament and posterolateral structures. J Bone Joint Surg Am 1988;70A:88–97 [PubMed] [Google Scholar]
- 5.Velteri DM, Deng X-H , Torzilli PA, Warren RF, Maynard MJ, et al. The role of cruciate and posterolateral ligaments in stability of the knee. A biomechanical study. Am J Sports Med 1995;23:436–43 [DOI] [PubMed] [Google Scholar]
- 6.Butler DL, Noyes FR, Good ES. Ligamentous restraints to anterior – posterior drawer in human knee. A biomechanical study. J Bone Joint Surg Am 1987;69A:233–42 [PubMed] [Google Scholar]
- 7.Shelbourne KD, Davis TJ, Patel DV. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries. A prospective study. Am J Sports Med 1999;27:276–83 [DOI] [PubMed] [Google Scholar]
- 8.Hochstein P, Schmickal T, Grutzner PA, Wentzensen A. Diagnostic and incidence of the rupture of the posterior cruciate ligament. Unfallchirurg 1999;102:753–62 [DOI] [PubMed] [Google Scholar]
- 9.Fanelli GC. Posterior cruciate ligament injury in trauma patients. Arthroscopy 1993;9:291–4 [DOI] [PubMed] [Google Scholar]
- 10.Fanelli GC, Edson CJ. Posterior cruciate ligament injury in trauma patients: part II. Arthroscopy 1995;11:526–9 [DOI] [PubMed] [Google Scholar]
- 11.Rubinstein RA, Jr, Shelbourne KD, McCarrell JR, Van Meter CD, Rettig AC, et al. The accuracy of clinical examination in the setting of posterior cruciate ligament injury. Am J Sports Med 1994;22:550–7 [DOI] [PubMed] [Google Scholar]
- 12.Fischer SP, Fox JM, Del Pizzo W, Friedman MJ, Snyder SJ, Ferkel RD, et al. Accuracy of diagnoses from magnetic resonance imaging of the knee. A multicenter analysis of one thousand and fourteen patients. J Bone Joint Surg Am 1991;73A:2–10 [PubMed] [Google Scholar]
- 13.Heron CW, Calvert PT. Three-dimensional gradient-echo MR imaging of the knee: Comparison with arthroscopy in 100 patients. Radiology 1992;183:839–44 [DOI] [PubMed] [Google Scholar]
- 14.Gross ML, Grover JS, Bassett LW, Seeger LL, Finerman AM. Magnetic resonance imaging of the posterior cruciate ligament. Clinical use to improve diagnostic accuracy. Am J Sports Med 1992;20:732–7 [DOI] [PubMed] [Google Scholar]
- 15.Polly DW, Jr, Callaghan JJ, Sikes RA, McCabe JM, McMahon K, Savory CG, et al. Accuracy of selective magnetic resonance imaging compared with findings of arthroscopy of the knee. J Bone Joint Surg Am 1998;70A:192–8 [PubMed] [Google Scholar]
- 16.Turner DA, Prodomos CC, Petasnick JP, Clark JW. Acute injuries of the ligaments of the knee: magnetic resonance evaluation. Radiology 1985;154:717–22 [DOI] [PubMed] [Google Scholar]
- 17.Chen MC, Shih TT, Jiang CC, Su CT, Huang KM. MRI of meniscus and cruciate ligament tears correlated with arthroscopy. J Formos Med Assoc 1995;94:605–11 [PubMed] [Google Scholar]
- 18.Patten RM, Richardson ML, Zink-Brody G, Rolfe BA. Complete vs. partial thickness tears of the posterior cruciate ligament: MR findings. J Computed Assisted Tomography 1994;18:793–9 [PubMed] [Google Scholar]
- 19.Tewes DP, Fritts HM, Fields RD, Quick DC, Buss DD. Chronically injured posterior cruciate ligament: magnetic resonance imaging. Clin Orth Related Research 1997;335:224–32 [PubMed] [Google Scholar]
- 20.Shelbourne KD, Jennings RW, Vahey TN. Magnetic resonance imaging of posterior cruciate ligament injuries: assessment of healing. Am J Knee Surg 1999;12:209–13 [PubMed] [Google Scholar]