Abstract
The deep inferior epigastric artery perforator (DIEP) flap has recently become the first option for breast reconstruction. However, the anatomy of the deep inferior epigastric artery varies greatly from one individual to another and even from one hemiabdomen to the other. An optimal pre-operative evaluation method that adequately maps the underlying vasculature has been lacking. The advent of multidetector-row CT (MDCT) angiography has proven highly accurate at detailing the vasculature, but no reports have documented its value during pre-operative planning. From December 2006 to May 2008, 22 consecutive patients who underwent MDCT angiography before breast reconstruction using DIEP flaps were selected as the test group, and 22 former patients who did not undergo MDCT before the same procedure were selected as the control group. The two groups were evaluated for the ratio of pre-operative redesign, intra-operative method changes, time spent on flap harvest and the ratio of flap-associated complications. The pre-operative redesign ratio was 22.7% in the test group and 0% in the control group. The intra-operative method change ratio was 0% in the test group and 13.6% in the control group. The mean time spent on flap harvest was 2.8 ± 0.2 h in the test group and 4.4 ± 0.2 h in the control group (p<0.05). The flap complication rate was 1/22 in the test group and 3/22 in the control group (p _ 0.04). In conclusion, use of MDCT angiography during pre-operative planning promotes a significant reduction in operating time and complication rate.
Abdominal flaps have become the first option for breast reconstruction owing to their similar texture to that of the natural breast. The use of the deep inferior epigastric artery perforator (DIEP) flap for these procedures has become more popular in recent years owing to its minimal donor site morbidity [1]. However, the anatomy of the deep inferior epigastric artery (DIEA) varies greatly in its location, branch pattern, intramuscular course and number of perforators from one individual to another, and even from one hemiabdomen to the other. This makes it hard to plan a suitable pre-operative approach and to locate proper perforators intra-operatively. Doppler sonography has been used routinely for pre-operative planning in our department for many years, with mixed results [2]. As multidetector-row CT (MDCT) angiography was adopted in our department in 2006, the technique has proved to be the method of choice [3], but no reports document the value of MDCT for pre-operative planning of surgery. In this study, we describe the benefits of this method for pre-operative planning before breast reconstruction with DIEP flaps.
Methods and materials
Between December 2006 and May 2008, 22 consecutive patients who underwent MDCT angiography prior to breast reconstruction with DIEP flaps were selected as the test group, and 22 former patients who did not undergo MDCT angiography prior to breast reconstruction with DIEP flaps were selected as the control group. Patient ages ranged from 25–63 years old. This study was approved by the ethical committee of our hospital, and all of the patients who participated in the study were volunteers. All investigations and procedures were undertaken with the same team of surgeons and radiologists, and the same surgeon performed all Doppler ultrasound examinations.
Pre-operative planning was performed using both Doppler sonography and MDCT angiography in the test group, and only Doppler sonography was performed in the control group. MDCT angiography (64-row Light Speed VCT; GE Healthcare, Milwaukee, WI) utilised the following parameters: 120 kv, 300–350 mA, 0.35 s gantry rotation speed, 64 × 0.625 mm detector configuration, and a 0.98 detector pitch. All scanning was performed after antecubital injection of 100 ml of non-ionic contrast medium (Iopamiro 370; Bracco Sine Pharmaceutical Co, Shanghai, China) at a concentration of 370 mg ml–1. The patient was set in a supine position and administered contrast medium at a rate of 5 ml s–1. The scan ranged from 5 cm above the umbilicus to the pubic symphysis. The volumetric data were then transferred to an analytic workstation (Deep Blue ADW4.3; GE Healthcare, Milwaukee, WI) to generate reconstructed images in multiple planes (coronal, axial and sagittal) and subsequent three-dimensional images using volume rendering, maximum intensity projection and multiplanar reconstruction techniques (Figures 1–3).
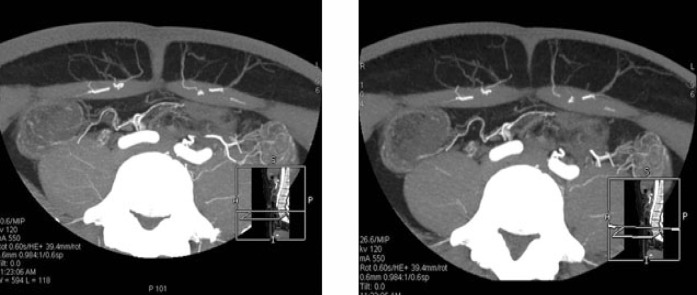
Figure 1.
Transverse views reconstructed using thin-slab maximum intensity projections.
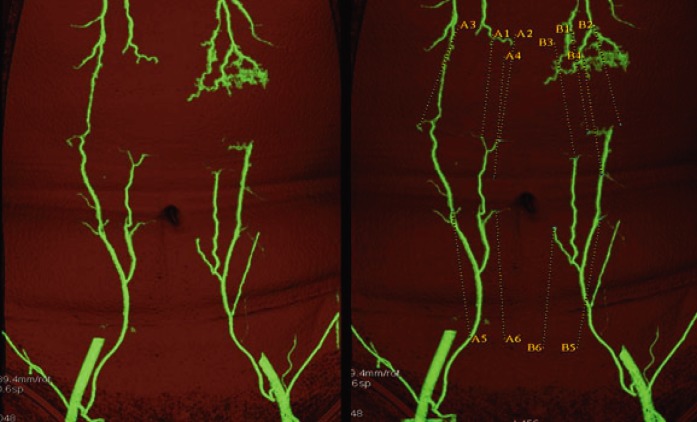
Figure 3.
The image of the final reconstruction with the perforators highlighted (right-hand image).
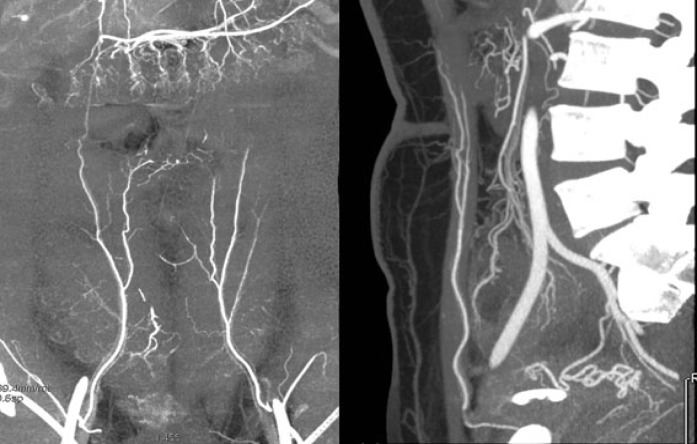
Figure 2.
Coronal and sagittal views reconstructed using thin-slab maximum intensity projections.
In the test group, the surgery was planned twice: first based on the Doppler findings and then subsequently based on the MDCT findings. This allowed us to obtain a redesign ratio. During the procedure, some planned procedures had to be changed, indicated by the intra-operative method change ratio. The time spent on each single-side DIEP flap harvest was recorded separately. Post-operatively, the flap-associated complication rate was also recorded. All data were then statistically compared between the two groups using the Wilcoxon sign rank test. A p-value of <0.05 was considered statistically significant.
Results
Redesign ratio
In the test group, there were two patients whose superficial inferior epigastric artery (SIEA) diameter was >1.5 mm based on the MDCT angiography, and so we changed the design method from a DIEP to a SIEA flap. In another two cases, we switched the DIEP flap to the other side of the abdominal wall owing to the MDCT findings. In the last redesigned case, we changed from a DIEP to a transverse rectus abdominis myocutaneous (TRAM) flap because of an unfit vascular branch pattern [4]. Thus, the total redesign ratio in the test group was 22.7%, compared with 0% in the control group (p<0.05).
Intra-operative method change ratio
During the procedure in the control group, we switched the DIEP flap to the other side of the abdominal wall in two cases because of the poor vascular perforators. In another case, we changed from a DIEP flap to a TRAM flap in the other side of the abdominal wall because of the small calibre of the perforators and the unfit vascular branch pattern. However, in the test group, no method change was made intra-operatively. Therefore, the intra-operative method change ratio was 0% in the test group and 13.6% in the control group (p<0.05).
Flap harvest time
The time spent on a single side DIEP flap harvest was recorded and the values were compared using an independent sample t-test. In the test group, this value was 2.8 ± 0.2 h, whereas in the control group it was 4.4 ± 0.2 h (p<0.05).
Flap complication rate
Complications included flap necrosis, as well as partial or total flap failure. In the test group, there was only a single complication (1/22) in one patient whose flap appeared to have necrosis at the distal side on post-operative day five. Debridement was performed two days later with good results. In the control group, one patient presented with a pale flap 72 h after the procedure. After four repeat operations, the flap was lost. There were another two patients who had partial flap loss, and debridement was performed. The flap complication rate in the control group was 3/22 (p _ 0.04) (Table 1).
Table 1. The main index of the study.
| Test group | Control group | p-Value | |
| Redesign ratio | 22.7% | 0% | <0.05 |
| Method change ratio | 0% | 13.6% | <0.05 |
| Flap harvesting time | 2.8 ± 0.2 h | 4.4 ± 0.2 h | <0.05 |
| Flap complication | 1/22 | 3/22 | 0.04 |
Discussion
It is crucial to obtain an optimal pre-operative plan prior to breast reconstruction using DIEP flaps, as it can have vital effects on operation time and post-operative flap complication rates. Unidirectional Doppler sonography has been used routinely for many years as it is inexpensive and convenient. However, it commonly produces significant inconsistencies and often obtains limited information. Information not obtained via Doppler sonography, such as branch pattern, perforator calibre, intramuscular trajectory etc, is often needed prior to surgery. Given these disadvantages, Doppler sonography is not the first choice for pre-operative imaging prior to DIEP breast reconstruction [2, 5].
Colour duplex imaging has significant advantages over unidirectional Doppler sonography. It can provide more detail, especially in relation to branch patterns, perforator calibres and haemodynamic variations, and it has a higher sensitivity and specificity. Despite these advantages, the method is time consuming and has a low patient tolerance. Furthermore, the results cannot be easily read by a surgeon without special imaging knowledge [5].
MRI without intravenous contrast is a technique based on the flowing void effect. Theoretically, it can differentiate between both arteries and veins simultaneously. It requires no radiation or contrast medium but, based on the work by Ahn et al [6], it does not produce adequate results. The use of magnetic resonance angiography (MRA) for the imaging of DIEP flaps was first described by Rozen et al in 2009 [7]. Although it requires no radiation or contrast medium, it is less accurate than MDCT angiography, has a lower space resolution, and has a greater cost.
In recent years, MDCT has become established as the gold standard for pre-operative imaging before breast reconstruction using DIEP flaps [8], and it has been shown to be of great benefit to surgeons in this field. MDCT can visualise the DIEA accurately, reducing intra-operative dissection time and helping to avoid surgical errors. This approach is also convenient for both the patient and surgeon, as the whole process takes ∼20 min in total. Although it has many benefits and is treated as a non-invasive method, it does have a radiation effect. However, the mean dose received by patients undergoing this examination is about 4.8 ± 0.4 mSv, which is no more than that of an conventional abdominal CT scan [3, 8–10]. Another possible drawback of this approach is the contrast medium used, i.e. a non-ionic iodine that has demonstrated a low level of nephrotoxicity. Finally, the cost of MDCT angiography in China (∼1 000 Renminbi) is unfortunately cost prohibitive for many patients.
Conclusions
MDCT is a convenient and reliable tool for accurate pre-operative assessment of the vascular supply to the DIEP flap. It can help surgeons make informed choices, reduce operation time, and lower complication rates. Therefore, using this technique allows better and more efficient breast reconstruction via DIEP flaps, and it is likely that this approach will become more routine prior to microsurgery.
References
- 1.Granzow JW, Levine JL, Chiu ES, Allen RJ. Breast reconstruction with the deep inferior epigastric perforator flap: history and an update on current technique. J Plast Reconstr Aesthet Surg 2006;59:571–9 [DOI] [PubMed] [Google Scholar]
- 2.Blondeel PN, Beyens G, Verhaeghe R, Van Landuyt K, Tonnard P, Monstrey SJ, et al. Doppler flowmetry in the planning of perforator flaps. Br J Plast Surg 1998;51:202–9 [DOI] [PubMed] [Google Scholar]
- 3.Masia J, Clavero JA, Larraãaga JR, Alomar X, Pons G, Serret P. Multidetector-row computed tomography in the planning of abdominal perforator flaps. J Plast Reconstr Aesthet Surg 2006;59:594–9 [DOI] [PubMed] [Google Scholar]
- 4.Rozen WM, Palmer KP, Suami H, Pan WR, Ashton MW, Corlett RJ, et al. The DIEA branching pattern and its relationship to perforators: the importance of preoperative computed tomographic angiography for DIEA perforator flaps. Plast Reconstr Surg 2008;121:367–73 [DOI] [PubMed] [Google Scholar]
- 5.Hallock GG. Doppler sonography and colour duplex imaging for planning a perforator flap. Clin Plast Surg 2003;30:345–57 [DOI] [PubMed] [Google Scholar]
- 6.Ahn CY, Narayanan K, Shaw WW. In vivo anatomic study of cutaneous perforators in free flaps using magnetic resonance imaging. J Reconstr Microsurgery 1994;10:157–63 [DOI] [PubMed] [Google Scholar]
- 7.Rozen WM, Stella DL, Bowden J, Taylor GI, Ashton MW. Advances in the preoperative planning of deep inferior epigastric artery perforator flaps: magnetic resonance angiography. Microsurgery 2009;29:119–23 [DOI] [PubMed] [Google Scholar]
- 8.Masia J, Larraãaga J, Clavero JA, Vives L, Pons G, Pons JM. The value of the multidetector row computed tomography for the preoperative planning of deep inferior epigastric artery perforator flap. Ann Plast Surg 2008;60:29–36 [DOI] [PubMed] [Google Scholar]
- 9.Rozen WM, Phillips TJ, Ashton MW, Stella DL, Gibson RN, Taylor GI. Preoperative imaging for DIEA perforator flaps: a comparative study of computed tomographic angiography and Doppler ultrasound. Plast Reconstr Surg 2008;121:9–16 [DOI] [PubMed] [Google Scholar]
- 10.Rosson GD, Williams CG, Fishman EK, Singh NK. 3D CT angiography of abdominal wall vascular perforators to plan DIEAP flaps. Microsurgery 2008;10:641–6 [DOI] [PubMed] [Google Scholar]