Abstract
Odontogenic myxofibroma of the temporomandibular joint (TMJ) is a rare tumour; moreover, primary splenic angiosarcoma (PAS) in paediatric patients is extremely rare. We report on a 15-year-old boy who presented with right TMJ swelling and subsequently developed epigastric and right upper quadrant pain. The TMJ swelling proved to be odontogenic myxofibroma and the abdominal pain was a result of primary splenic angiosarcoma with hepatic metastasis. We report for the first time the synchronous presentation of PAS and odontogenic myxofibroma in a paediatric patient, and we describe the radiological features along with the histological diagnosis and clinical outcome. Uptake in 18F-2-fluoro-2-deoxy-D-glucose positron emission tomography is also described for the first time for both these tumours.
Langhans in 1879 was the first to identify primary angiosarcoma of the spleen (PAS). Since then, approximately 200 cases of PAS have been reported in the literature [1]. PAS is a very rare and aggressive neoplasm with poor prognosis, especially in paediatric patients. Only 10 paediatric cases have been reported in the literature [2–6].
Odontogenic myxofibroma was first described by Virchow in 1863. It is a rare, locally aggressive, slowly growing benign neoplastic lesion. It is not found in bones outside the facial skeleton. The tumour is asymptomatic, although some patients complain of pain. It occurs in individuals between the ages of 10 years and 30 years, and its occurrence is unusual in people younger than 10 years or older than 50 years [7, 8].
18F-2-fluoro-2-deoxy-D-glucose (18FDG) positron emission tomography (PET) provides a means of diagnosing cancer based on altered tissue metabolism. This “functional” imaging technique relies on a radioactive substance that decays by positron emission; 18FDG is an analogue of glucose. Malignant cells trap more radiotracer compared with non-malignant cells, and the local tracer concentration can be measured (standard uptake value (SUV)) [9].
We present the case of a 15-year-old male patient with primary angiosarcoma of the spleen, with liver and bone metastases. The patient also had a synchronous temporomandibular joint (TMJ) mass, which proved to be an odontogenic myxofibroma of the TMJ. To our knowledge, this is the first time that both of these neoplasms have presented synchronously and the first time that 18FDG–PET findings are described for either tumour.
Case report
A 15-year-old male patient presented to the department of dentistry at Jordan University Hospital with pain and swelling of the right TMJ. The clinical impression was of an infectious process of the TMJ. An MRI scan showed abnormal bone marrow signal of the right mandibular condyle and upper part of the ramus, surrounded by soft-tissue oedema associated with moderate post-contrast enhancement; accordingly, a clinical diagnosis of acute osteomyelitis of the TMJ and mandible was presumed.
Two months later, he presented to the emergency department with severe right-upper quadrant abdominal and epigastric pain. The pain was colicky in nature and 12 h in duration.
Physical examination revealed epigastric and right-upper quadrant tenderness. Laboratory results showed only a slightly elevated white blood cell count and alkaline phosphatase level.
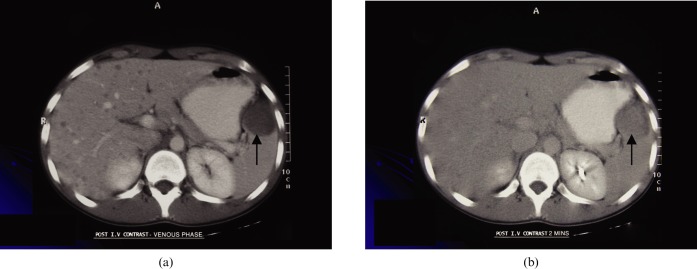
Radiological work-up at that time included abdominal ultrasonography, which showed hepatomegaly with diffuse numerous hyperechoic lesions and a single large hypoechoeic mass lesion in the spleen. The patient was admitted to hospital for further work-up; his abdominal CT scan confirmed the presence of hepatomegaly with multiple diffuse small lesions, which appeared hypodense on the portovenous phase (Figure 1a). On delayed venous images, these lesions were indistinguishable from liver parenchyma (Figure 1b). In addition, CT showed a hypodense mass lesion in the spleen with the same enhancement pattern as the liver lesions.
Figure 1.
Abdominal CT scan in the (a) portovenous and (b) delayed venous phases showing the hypodense splenic lesion (arrows) and multiple liver lesions.
Liver and spleen MRI showed that the aforementioned lesions appeared hypointense on T1 and hyperintense on T2. After injection of intravenous gadolinium, the lesions were indistinguishable from normal parenchyma on delayed images. The differential diagnosis of the radiological appearances included multiple haemangiomas, haemangioendithelioma, angiosarcoma and metastasis from a vascular tumour.
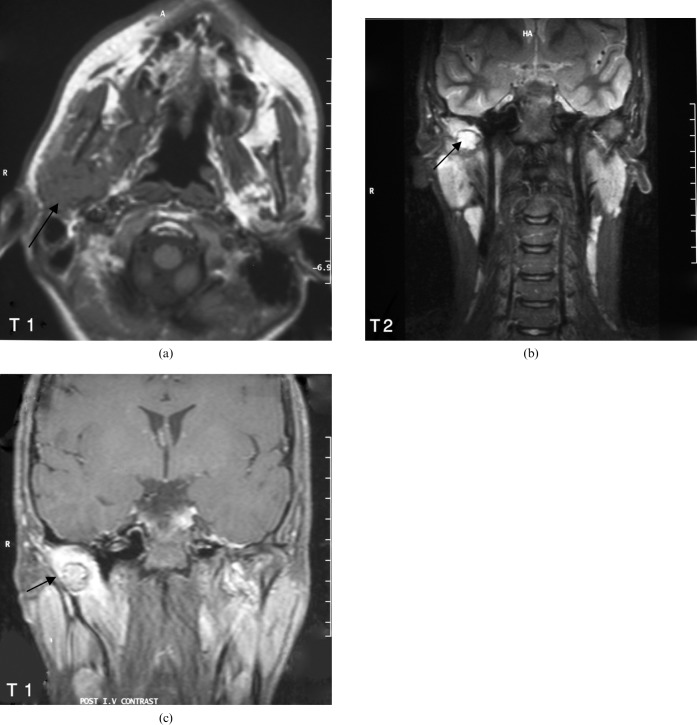
During admission, the patient developed constant low back pain. Lumbar spine MRI showed high signal intensity on T2 weighted images in the L1 vertebral body, which was suspicious for metastasis. An 18FDG–PET/CT scan (Figure 2) was performed to complete the patient's staging. It showed avid 18FDG uptake in the spleen (SUVmax _ 6.8), multiple liver lesions (SUVmax _ 6.8), first lumbar vertebral body and the right TMJ (SUVmax _ 7.7). Repeat MRI of the TMJ (Figure 3a,b) revealed the presence of a mass in the right mandibular condyle with a similar appearance and enhancement pattern (Figure 3c) to that of the liver and spleen lesions.
Figure 2.

Whole-body 18F-2-fluoro-2-deoxy-D-glucose (18FDG) positron emission tomography (PET) showing focally increased uptake in the right mandible (arrow) and increased uptake in both the liver and spleen.
Figure 3.
MRI of the temporomandibular joints — (a) axial T1, (b) coronal T2 fat-saturated and (c) coronal T1 post-contrast scans — showing the right mandibular mass lesion (arrows).
At this point, malignancy was suspected but no diagnosis was made. The patient underwent splenectomy with hilar lymph node excision. Liver and right TMJ biopsies were also performed.
Histopathology revealed the diagnosis of angiosarcoma of the spleen (Figure 4) with multiple liver and lymph nodes metastases, while the biopsy of the right TMJ proved to be an odontogenic myxofibroma (Figure 5). The patient received four courses of chemotherapy (including 400 mg Avastin, 60 mg cisplatinum, 60 mg lopisomal doxorubicin (Caelyx), and 3 g m–2 ifosfamide for two days and 3 g of mesna for two days 3 g m–2 ). He was given an additional six radiotherapy sessions of 2000 cGy each for the lumbar spine.
Figure 4.
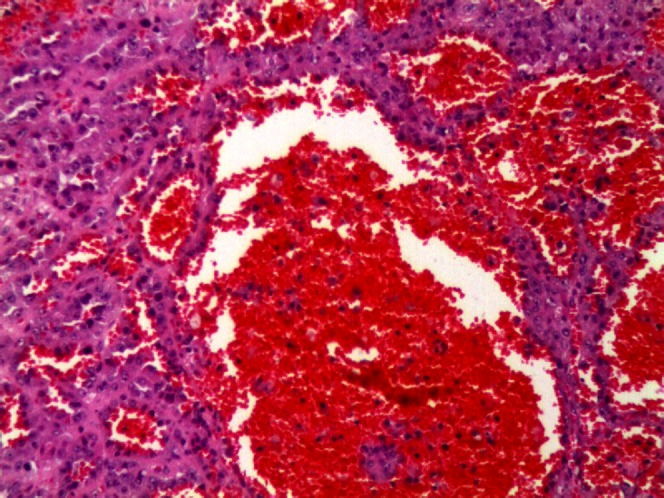
Angiosarcoma of the spleen. The tumour has (a) sinusoidal and (b) cavernous growth patterns (haematoxylin and eosin stain, ×200)
Figure 5.
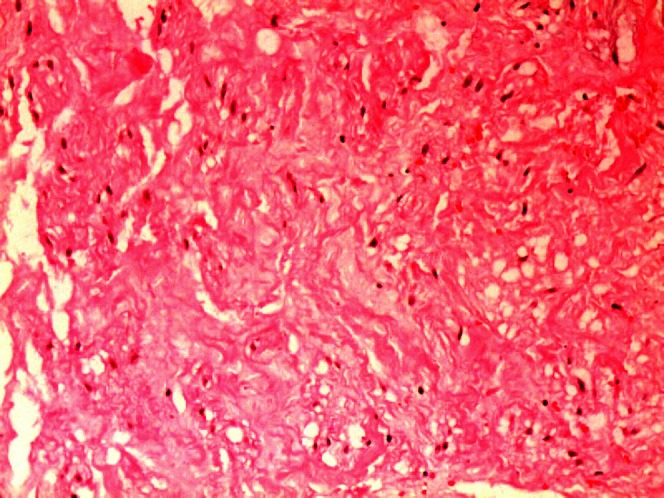
Odontogenic myxofibroma. The high magnification shows a loose arrangement of spindle or stellate cells in a myxomatous background. Also of note is the prominent vascularity (haematoxylin and eosin stain, ×200).
Two and a half months later, a follow-up CT scan showed an increase in the number and size of the hepatic lesions and the appearance of a new adrenal metastasis, indicating disease progression. The patient was started on palliation therapy, but died five months after his admission.
Discussion
Angiosarcoma is a mesenchymal malignancy of vascular origin and consists of atypical and anaplastic endothelial cell proliferation. It usually involves the spleen, soft tissue, breast, bone marrow and liver. The mean age at presentation is 55 years. Approximately 200 cases of PAS have been reported in literature, of which only 10 cases were in the paediatric age group. The outcome of paediatric PAS is typically bad, with only 20% of patients surviving for six months. The survival rate does not correlate with histological grade, tumour size, mitotic count, metastasis or mode of treatment; however, early diagnosis with splenectomy before rupture has a favourable effect on survival rate [2, 3].
Reported concomitant or synchronous neoplasms with PAS have included lymphoma and cancer of the breast, colon, kidneys and skin. The occurrence of synchronous benign tumour has not been reported previously [2].
Odontogenic myxofibroma was linked histologically to the Wharton's jelly of the umbilical cord. It is a locally aggressive benign neoplasm and rarely occurs in bony sites other than the alveolar regions of the maxilla or mandible. When it grows to a large size, it causes cortical expansion, rather than perforation, of the cortical bone. The body and posterior portion of the mandible are the favoured sites. Radiologically, the lesion appears as a radiolucency containing extremely delicate septae, giving it a multilocular or honeycomb appearance similar to an ameloblastoma, a giant cell granuloma or a fibrous dysplasia. The margins of the lesion are poorly defined and the roots of adjoining teeth may be displaced.
Although odontogenic myxofibromas are benign, they are locally invasive and therefore have a high recurrence rate following attempts of curettage. The overall prognosis for this lesion, however, is good [7, 8].
18FDG–PET scan is sensitive for detecting malignancy; however, avid FDG uptake is not specific for malignancy. Many false-positive cases were reported in benign neoplasms, such as pituitary adenoma, adrenal adenoma, thyroid follicular adenoma, salivary gland tumours (e.g. Warthin's tumour or pleomorphic adenoma) and colonic adenomatous polyps, and villous adenoma, ovarian thecoma and cystadenoma, giant cell tumour, aneurysmal bone cysts and leiomyoma. 18FDG–PET uptake has also been described in many fibro-osseous defects such as non-ossifying fibromas, fibrous cortical defects and cortical desmoids in paediatric patients mimicking metastasis [9, 10]. This is the first time in the literature that avid 18FDG uptake is reported in myxofibroma, which represents a false-positive PET finding. In addition, for the first time, FDG appearance in PAS and its synchronous occurrence with odontogenic myxofibroma are reported.
References
- 1.Manouras A, Giannopoulos P, Toufektzian L, Markogiannakis H, Lagoudianakis E, Papadima A, et al. Splenic rupture as the presenting manifestation of primary splenic angiosarcoma in a teenage woman: a case report. J Med Case Reports 2008;2:133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hsu J, Ueng S, Hwang T, Chen H, Jan Y, Chen M. Primary angiosarcoma of the spleen in a child with long-term survival. Pediatr Surg Int 2007;23:807–10 [DOI] [PubMed] [Google Scholar]
- 3.Vrchliotis T, Bennett W, Vaswani K, Niemann T, Bova J. Primary angiosarcoma of the spleen- CT, MR, and sonographic characteristics: report of two cases. Abdom Imaging 2000;25:283–5 [DOI] [PubMed] [Google Scholar]
- 4.Hoed I, Granzen B, Aronson D, Pauwels P, Kraker J, Heurn L. doi: 10.1080/08880010590964228. Metastasized angiosarcoma of the spleen in a 2-year-old girl. Pediatr Hematol Oncol 2005; 22:5,387–90. [DOI] [PubMed] [Google Scholar]
- 5.Thompson W, Aguilera N, Gorospe L, Abbott R. Angiosarcoma of the spleen: Imaging characteristics in 12 patients. Radiology 2005;235:106–15 [DOI] [PubMed] [Google Scholar]
- 6.Abbott R, Levy A, Aguilera N, Gorospe L, Thompson W. From the archives of the AFIP. Primary vascular neoplasms of the spleen: radiologic- pathologic correlation. Radiographics 2004;24:1137–63 [DOI] [PubMed] [Google Scholar]
- 7.Rotenberg B, Daniel S, Nish L, Ngan B, Forte V. Myxomatous lesions of the maxilla in children: a case series and review of management. Int J Pediatr Otorhinolaryngol 2004;68:1251–6 [DOI] [PubMed] [Google Scholar]
- 8.Maeda T, Tateishi U, Hasegawa T, Ojima H, Arai Y, Sugimura K. Primary hepatic angiosarcoma on coregistered FDG PET and CT images. AJR Am J Roentgenol 2007;188:1615–7 [DOI] [PubMed] [Google Scholar]
- 9.Delbeke D, Coleman R, Guiberteau M, Brown M, Royal H, Siegel B, et al. Procedure guideline for tumour imaging with 18F- FDG PET/CT. J Nucl Med. 2006;47:885–95 [PubMed] [Google Scholar]
- 10.Goodin G, Shulkin B, Kaufman R, McCarville M. PET/CT characterization of fibroosseous defects in children: 18F-FDG uptake can mimic metastatic disease. AJR Am J Roentgenol 2006;187:1124–8 [DOI] [PubMed] [Google Scholar]