Abstract
Transjugular intrahepatic portocaval shunt (TIPS) is performed in patients with symptomatic Budd–Chiari syndrome (BCS) who do not have repairable hepatic veins. We report the case of a patient who had an inferior vena cava (IVC) stent placed previously as part of the management for BCS, and who subsequently required TIPS. The TIPS tract was created through the strut of the previously placed IVC stent; the TIPS stent was placed after dilatation of the liver parenchyma as well as the strut of the IVC stent. This novel technique of “strutplasty” of a previously placed stent as part of TIPS has not been reported in the literature.
The transjugular intrahepatic portocaval shunt (TIPS) procedure, as well as stent technology, is continually being improved [1–5]. Direct intrahepatic portocaval shunt (DIPS) – a modification of the TIPS procedure – is especially useful when there are occluded hepatic veins or an unfavourable angle between the inferior vena cava (IVC) and the hepatic vein resulting from hydrothorax and hypertrophy of the caudate lobe of the liver [1]. Herein, we report a technical modification of the TIPS procedure in Budd–Chiari syndrome (BCS).
Case report
A 17-year-old man with ascites and an oesophageal variceal bleed (managed by endoscopic variceal ligation) was diagnosed to have BCS. He had significantly diseased hepatic veins, a dilated accessory hepatic vein with ostial stenosis, and focal stenosis of the IVC at the level of hepatic confluence. He underwent stenting of the accessory hepatic vein, angioplasty of the IVC and stenting of the IVC at different sittings, after which he showed a rapid improvement of symptoms. He was also on oral anticoagulation treatment. He remained asymptomatic for 14 months before he had recurrence of the ascites and variceal bleed. As a result, left hepatic venous intervention was planned through the transjugular route, but was unsuccessful. Percutaneous puncture of the left hepatic vein was then performed in an attempt to cannulate the ostium. As there was a relatively long segment of stenosis of the hepatic vein towards the ostium, the procedure failed and the liver puncture tract was closed with coils. The patient underwent endoscopic ligation of the oesophageal varices. There was moderate hepatosplenomegaly, volume redistribution of the liver with marked caudate lobe hypertrophy, intrahepatic collaterals and moderate ascites, with occlusion of the hepatic venous ostium and stenosis of a segment of the hepatic vein on imaging. Hence, a TIPS procedure was planned.
Under general anaesthesia, the right internal jugular vein was accessed with an 18G puncture needle under sonographic guidance and secured with a 9-French sheath, which was then upgraded to a 10-French sheath. A 0.035 inch J guide wire was advanced to the IVC through the IVC stent, and venography was performed. Initially, a transjugular liver biopsy (TJLB) cannula (Cook Inc, Bloomington, IN) was placed into the IVC, through which a Rosch–Uchida needle (Cook Inc) was advanced. Under transabdominal ultrasound guidance, the IVC was punctured through the struts of the previously placed IVC stent, and the needle extended to enter the bifurcation of the portal vein. A 5F pigtail catheter was placed in situ over a 0.035 inch. The pressure gradient was 31 mm Hg. Amplatz guidewire (Boston Scientific, Miami, FL). Angioplasty of the strut and hepatic parenchyma was performed using a 10 mm × 4 cm balloon (Bard Peripheral Vascular Inc, Murray Hill, NJ) (Figure 1). Portal venography showed hepatofugal flow (Figure 2); the pressure gradient was 31 mmHg. A 10 mm × 8 cm Viator TIPS endoprothesis (WL Gore and Associates, Flagstaff, AZ) was then deployed. A second covered 10 mm × 6 cm stent (Niti-S stent; Taewoong, Seoul, Korea) was required proximally, projecting into the IVC. A post-stenting angioplasty was performed using a 10 mm × 4 mm balloon (Cook Inc). Post-stenting portal venography showed prompt flow from the portal vein through the TIPS stent (Figure 3), with a reduction in the pressure gradient to 14 mmHg. He showed significant clinical improvement (i.e. the ascites regressed, with no further variceal bleed) and remains well clinically and radiologically on follow-up after nine months.
Figure 1.
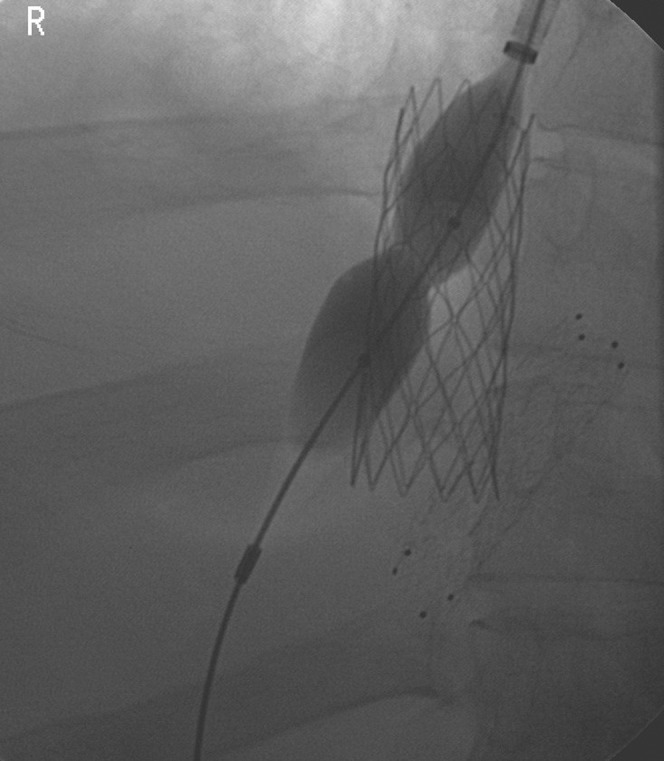
Digital subtraction angiography (DSA) image shows an inflated balloon in the strut of the inferior vena cava stent over a wire into the portal vein for the transjugular intrahepatic portocaval shunt procedure — “strutplasty”.
Figure 2.

A royal flush pigtail catheter tip seen in the portal vein through the inferior vena cava (IVC) strut and parenchymal track opacifies the portal vein. The dilated strut can be seen clearly in the IVC stent. The previously deployed accessory hepatic venous stenting can also be seen. A branching column of contrast with coils at the upper end represents a previous intervention attempted 1 week previously (percutaneous left hepatic vein access with failed access into the IVC owing to long segment stenosis and narrow ostium).
Figure 3.

Transjugular intrahepatic portocaval shunt stent deployed into the parenchymal track — one end into the inferior vena cava stent and the other end into the main portal vein, with opacification of contrast.
Discussion
Increasingly, interventional radiological treatment is the preferred choice for the management of BCS [6]. TIPS is indicated in patients with symptomatic BCS whose hepatic veins are absent or thrombosed. A TIPS shunt is usually created from the right hepatic vein to the right branch of the portal vein; in BCS patients, the tract may have to be created from the remnant hepatic stump if available or directly from the IVC (cavoportal shunts).
In our case, the cavoportal shunt was created by deploying a stent through the strut of the previously placed IVC stent. When the side branch of the vessel is to be stented, “classic crush” and “DK crush” techniques have been described in coronary interventions [7, 8]. In our procedure, angioplasty of the strut was performed to deploy the stent through the dilated strut of the stent — “strutplasty”. We deployed two stents through this dilated opening in the strut of the IVC stent into the portal vein through the liver parenchyma, with one overlapping the other. Strutplasty was also used to place a dialysis access through a previously placed stent in the brachiocephalic vein [9].
In our patient, strutplasty was safe and effective at controlling symptoms at nine months' follow-up; however, longer term follow-up is needed. In conclusion, strutplasty may be considered for the TIPS procedure in selected BCS patients, especially in those who have had previous IVC stent placement.
References
- 1.Petersen B, Uchida BT, Timmermans H, Keller FS, Rosch J. Intravascular US-guided direct intrahepatic portacaval shunt with a PTFE-covered stent-graft: feasibility study in swine and initial clinical results. J Vasc Interv Radiol 2001;12:475–86 [DOI] [PubMed] [Google Scholar]
- 2.Keshava SN, Kota GK, Mammen T, Jeyamani R, Moses V, Govil S, et al. Direct intrahepatic cavo-portal shunts in Budd-Chiari syndrome: role of simultaneous fluoroscopy and trans-abdominal ultrasonography. Indian J Gastroenterol 2006;25:248–50 [PubMed] [Google Scholar]
- 3.Quinn SF, Sheley RC, Semonsen KG. Creation of a portal vein to inferior vena cava shunt using CT guidance and a covered endovascular stent. AJR Am J Roentgenol 1997;169:1159–60 [DOI] [PubMed] [Google Scholar]
- 4.Hoppe H, Wang SL, Petersen BD. Intravascular US-guided direct intrahepatic portocaval shunt with an expanded polytetrafluoroethylene-covered stent-graft. Radiology 2008;246:306–14 [DOI] [PubMed] [Google Scholar]
- 5.Murad SD, Luong TK, Pattynama PM, Hansen BE, van Buuren HR, Janssen HL. Long-term outcome of a covered vs. uncovered transjugular intrahepatic portosystemic shunt in Budd-Chiari syndrome. Liver Int 2008;28:249–56 [DOI] [PubMed] [Google Scholar]
- 6.Eapen CE, Velissaris D, Heydtmann M, Gunson B, Olliff S, Elias E. Favourable medium term outcome following hepatic vein recanalisation and/or transjugular intrahepatic portosystemic shunt for Budd Chiari syndrome. Gut 2006;55:878–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Colombo A, Stankovic G, Orlic D, Corvaja N, Liistro F, Airodi F, et al. Modified T-stenting technique with crushing for bifurcation lesions: immediate results and 30-day outcome. Cathet Cardiovasc Interv 2003;60:145–51 [DOI] [PubMed] [Google Scholar]
- 8.Chen SL, Ye F, Zhang JJ, Zhu ZS, Lin S, Shan SJ, et al. Crush technique: modified treatment of bifurcation lesions in coronary artery. Chin Med J 2005;118:1746–50 [PubMed] [Google Scholar]
- 9.Joseph R, Keshava SN, Narayanam RS, John GT. Placement of a catheter through the struts of a previously placed stent for maintenance hemodialysis: a case report. Semin Dial 2008;21:575–7 [DOI] [PubMed] [Google Scholar]


