Abstract
Objective:
To analyze clinical pharmacist interventions in the intensive care units (ICUs) setting of a tertiary care Indian hospital and to assess the pharmacoeconomic impact on drug-related problems (DRPs).
Materials and Methods:
A postgraduate clinical pharmacist reviewed drug prescriptions over a period of 7 months. Whenever a DRP is identified, it was discussed with a physician and appropriate suggestions were provided, later it was documented on a preprepared form. Clinical significance of each intervention was graded based on the predicted clinical outcome. Acceptance of the interventions is entirely at the discretion of the medical staff. Each intervention was analyzed with respect to potential cost saving and/or additional cost incurred to existing drug therapy. An independent clinical panel was convened, and all the interventions made by the intervening pharmacist were critically reviewed for potential cost savings.
Results:
The intervening pharmacist made 117 recommendations, of which 94% was accepted by the medical professionals. The most frequent DRP identified was overdose (24%). The total net cost savings made was Rs. 77260.13 (USD 1796.73). This corresponds with Rs. 965.75 per patient and an annualized savings of Rs. 135205.22.
Conclusion:
Clinical pharmacist interventions had a significant impact on the cost of drug therapy and the patient outcome in intensive care settings of our hospital.
Keywords: Cost savings, drug-related problems, intensive care units, interventions, pharmacist
INTRODUCTION
Critical care is about specialized and dedicated care given by a team to a patient who is seriously ill.[1] It not only improves the chances of patients with desperate illness but also likes to promote an improvement in the general level of medical and nursing care.[2,3] Critically ill patients are treated with a large number of different drugs that have significant alterations in their pharmacokinetics and pharmacodynamics and great potential for drug misadventure.[4,5] Mortality, morbidity, and economic devastations are the most important consequence of medication errors.[6] Adverse drug events (ADEs) occur in approximately 30% of hospitalized patients, and the patients at intensive care units (ICUs) settings are at greater risk of developing ADEs.[7] The complexity of ICUs, combined with the high acuity of the patients treated in these areas, creates an environment that is more vulnerable to harmful patient's outcomes when medication errors occur.[8] Undoubtedly, drug-related problems (DRPs) have to be controlled or prevented to provide better patient care. Although few DRPs are not preventable as they are nonpredictable because of their idiosyncratic nature, the majority of the interventions are predictable and therefore be preventable.[9] The idea of a specialized intensive care pharmacist was first established in the world of pharmacy in 1982.[1] The increasing use of high-tech drugs and sophisticated drug delivery methods would seem to make the ICU a prime area for specialist pharmacy practitioners.[10] The involvement of a critical care pharmacist has been shown to decrease drug-related costs, prevent ADE, and reduce the morbidity[3] and today they are recognized as an integral member of critical care team along with the other health care professionals.[11] In a developing country like India increased expenditure for health care is not affordable by the majority of the patients. Hence, this study was indented to assess the impact of clinical pharmacist recommendations on the cost of drug therapy in ICU patients of a tertiary care teaching hospital .
MATERIALS AND METHODS
This was a prospective interventional study, conducted in the ICUs of JSS Hospital, Mysore, over a period of 7 months from July 2007 to January 2008. It is a 1000 bed multispecialty tertiary care teaching hospital. Patients of either sex aged ≥18 years who stayed at least overnight in surgical intensive care units (SICU), intensive cardiac care units (ICCU), and medical intensive care units (MICU) were included in our study. Exclusion criteria were critically ill patients receiving treatments in other units. The Institutional Human Ethical Committee of JSS College of Pharmacy, Mysore, approved the study. An intervening pharmacist reviewed the patient's progress charts and drug profile on day-to-day basis. This study considered the intervention as “any action by a pharmacist that directly resulted in a change to patient management or therapy”. All the data collected were documented in a suitably designed data collection form. Where a DRP was identified, it was discussed with the academic clinical pharmacist for further review and to seek his/her opinion. The DRPs identified during the study were categorized based on categories as described by Hepler and Strand.[12] Each DRP was assessed for its level of significance and was graded either as ‘minor’, ‘moderate’ or as ‘major’ based on the expected clinical outcome.
Independent panel assessment
An independent clinical panel was convened to review and assess the impact of clinical pharmacist interventions on cost savings. The three-member panel consisted of a consultant physician, a medical doctor, and an academic clinical pharmacy practitioner. An intervening pharmacist reviewed and assessed all those interventions that were accepted and changed by the physician, for any possible impact on length of stay (LOS), readmission probability, medical procedures, laboratory monitoring, and probability of mortality.
The assessment and quantification of percentage probability was based on a review of the individual case, and the decision by the panel was taken on the basis of their expertise knowledge and referral of appropriate literatures and websites such as www.medal.org.com. Those interventions perceived to have had impact only on the drug cost were not assessed by the panel but instead the intervening pharmacist calculated the impact of cost savings arising directly from such interventions.
Pharmacoeconomic analysis
Cost analysis was made only for those interventions that were accepted and changed, cost savings was considered if the cost of therapy was reduced after the intervention, compared to the cost of therapy prior to the interventions. The cost analysis was made based on each intervention rather than each patient. The net cost saving was calculated by subtraction of the cost increment of any from the total savings made from that intervention. The cost savings increased during the interventions are expressed in Indian rupees value.
Cost evaluation
Probability of readmission
The probabilities of readmission were estimated based on the probability, expressed as a percentage likelihood, of a readmission event occurring without the intervention compared with the probability of a readmission after the intervention has occurred, as assessed by the independent clinical panel. Costs were then calculated by multiplying this probability with the average cost of the treatment for specific disease costing at our Hospital.
Probability of length of stay
The panel quantified the impact of each intervention on LOS by estimating the change in the number of days in either a general medical ward or ICUs. The change in LOS was on the basis of likelihood of changes in LOS occurring if the intervention had not done. The local independent clinical panel decided as to subclassification of the wards based on the individual case. The cost impact of changes in LOS was then calculated based on JSS hospital's average treatment cost for the specific condition at that particular ward.
Probability of laboratory monitoring changes and medical procedures
The independent clinical panel examined the changes to laboratory monitoring or medical procedures and allocated a probability of the event being changed as a result of the intervention. The cost impact was then calculated by multiplying this probability by the JSS hospital's costs for the particular medical procedure or the laboratory test.
Evaluation of direct drug cost
Direct drug cost saving arising from interventions consisted of discontinuation of medication due to inappropriate use (e.g. duplicate therapy, lack of indication, and drug interactions); substitution of less expensive alternative (e.g. oral vs. intravenous route of administrations); dosage adjustment in elderly patients or patients with hepatic and renal impairment. Daily drug cost savings were calculated based on the frequency of drug administration and the total drug cost savings were calculated by multiplying daily cost savings and number of days of prescription from the day of intervention till the last day of therapy or day of discharge from the intensive care settings whichever was earlier.
Annualized cost savings
Annualized cost savings were calculated by extrapolating the net cost savings made during the 7 months to over a period of 1 year.
RESULTS
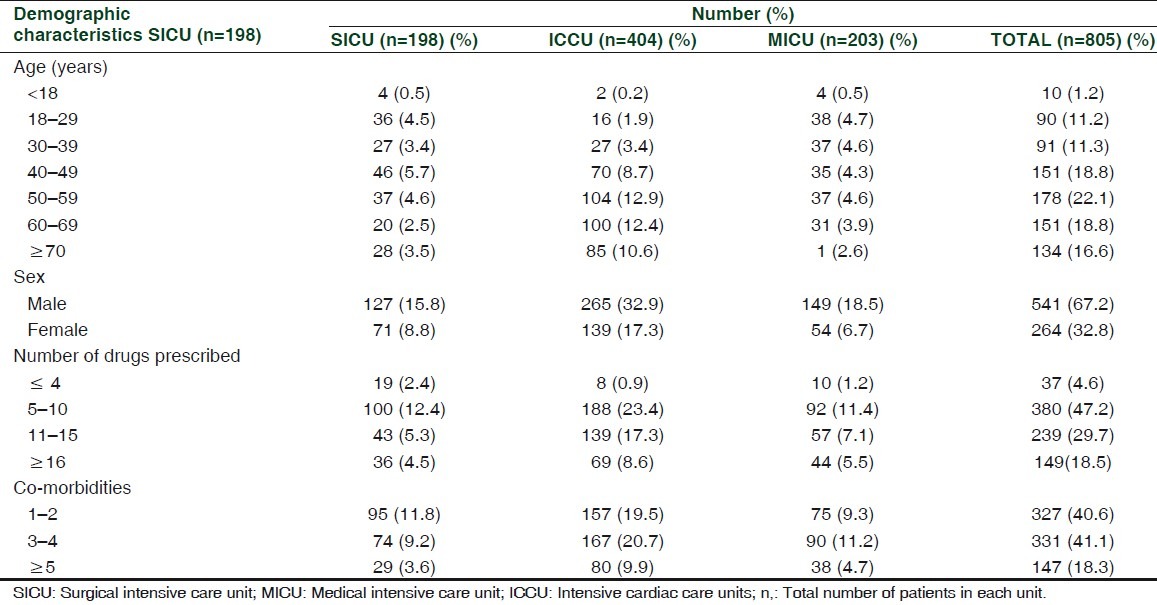
A total of 895 patients were admitted to three ICUs during the 7-month study period from July 2007 to January 2008. Of the total cases admitted, 805 cases were reviewed giving a review rate of 89.9%. Out of 805 cases reviewed, 67.2% (n = 541) of patients were male and the average age of the patients admitted to the ICUs was 51.21 + 17.23 (mean + SD) years. The average number of drugs received by the ICU patient was 10.2 per patient. The average LOS in ICU was 5.25 days [Table 1].
Table 1.
Demographic details of the patients admitted to intensive care units
The most frequent DRP detected was overdose [(25%) n = 28] followed by drug interactions [17% (n = 19)] [Figure 1]. The overall rate of acceptance of pharmacist interventions was 94. Of the 94 interventions accepted and changed, 60 interventions resulted in cost saving amounting to Rs. 89096.13 while 26 interventions resulted in addition of cost amounting to Rs. 11836.00. The total net cost savings made was Rs. 77260.13. The cost savings made in interventions range between Rs. 4840.00 and Rs. 2.00, and the average cost savings per intervention were Rs. 821.91 [Table 2]. The total net cost savings was higher for overdose (Rs. 45048.31) followed by drug interactions (Rs. 24723.30). However, the average net cost savings per intervention were higher with drug interaction (Rs. 1901.79) followed by overdose (Rs. 1801.93). Net cost savings were higher (Rs. 54560.40) with a ‘moderate’ level of DRPs followed by ‘major’ DRPs (Rs. 21664.11). However, the average cost savings per interventions were higher (Rs. 1969.46) with ‘major’ DRPs followed by ‘moderate’ DRPs (Rs. 992.01).
Figure 1.
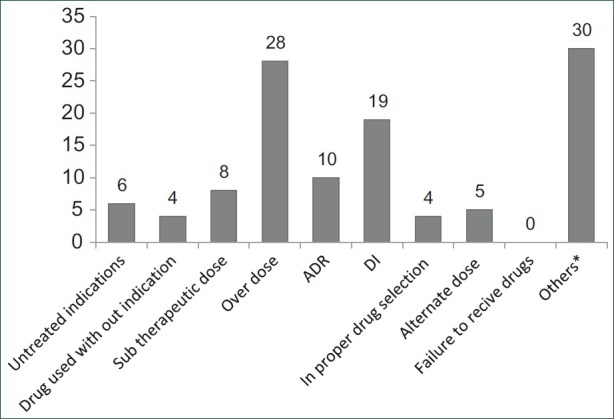
Types of drug-related problems detected. Class duplication (n = 9), drug duplication (n = 5), dispensing errors (n = 1), drug use without prescription (n = 2), sound-like errors (6), contraindications (3), wrong time of administration (n = 2). A dose of drug was prescribed with multiple number of lower strengths (2)
Table 2.
Impact of pharmacist-initiated changes to the drug therapy on cost

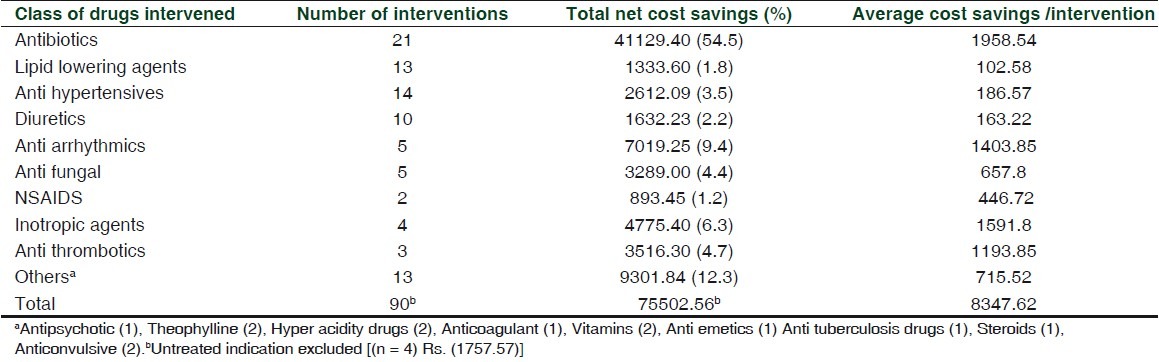
The majority [(25.6%) n = 21] of the interventions were associated with antibiotics followed by antihypertensive [(12.2%) n = 14] and lipid lowering drugs [(13.4 %) n = 11]. The class of drugs intervened and associated cost savings are summarized in Table 3.
Table 3.
Class of drugs intervened and associated cost savings
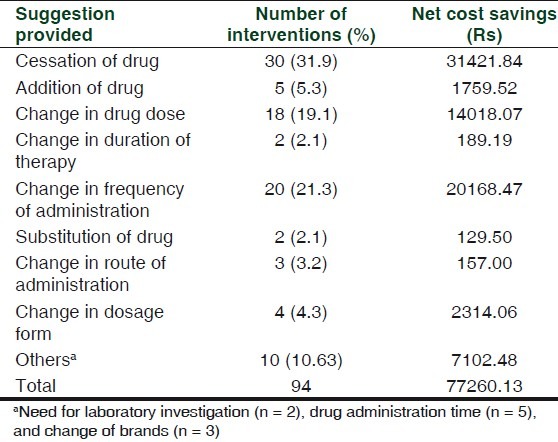
Cessation of drugs was the most frequent [(31.9%) n = 30] suggestion provided by the intervening pharmacist resulting in net cost savings of Rs. 31421.84 followed by changes in the frequency of administration (Rs. 20168.47) and changes in the drug dose (Rs. 14018.07) [Table 4].
Table 4.
Intervening pharmacist suggestions and associated cost savings
During the 7-month study period, the study pharmacist spent a total of 1018.18 h in different ICUs. The total time spent for interventions was 21.35 h while the average time spent for each intervention was 14.17 min. The maximum and minimum time spent for an intervention was 42 min and 4 min, respectively. The total net cost savings per hour was Rs. 3619.14.
DISCUSSION
Undoubtedly, clinical pharmacy services have made a positive impact on health care system.[13] Although many studies[4] were conducted to evaluate the value of addition of clinical pharmacy services into the patient care in critical care settings, its economic impact was very rarely studied. Therefore this study aimed to demonstrate the economic impact of clinical pharmacist services in critical care settings of a tertiary care teaching hospital.
Of the 895 patients admitted to the various intensive care settings, 805 patients were reviewed. In our study, we could not review 90 patients as they were either shifted from the ICU settings within few hours or within a day of admission, death occurred or due to admission and discharge of patients during the weekend holidays.
Of the total (161) DRPs identified, recommendations/suggestions were provided only for 117 interventions. Remaining 44 interventions were not considered for resolutions as they were considered to be minor DRPs and did not have any clinical significance in terms of patient's outcome. Of the 99 patients in whom DRPs identified, 48 patients received 6–10 drugs/patient/day and 32 patients received 11–15 drugs/patient/day. An increase in number of medication consumption would have resulted in the increased occurrence of DRPs. Other reasons for the increased occurrence of DRPs could be increased workload of doctors/medicine PGs and lack of adequate knowledge especially about the newly marketed drugs, urgency in providing the treatment, and possible stress on health care professionals.
Among the 94% of interventions accepted, 85% of interventions led to the change in drug therapy, while there was no change in drug therapy in 10% of interventions. This observation correlates with other studies[7,15] wherein the acceptance rate was reported to be 85% and 90%, respectively. However, in 10% of interventions there was no change in drug therapy as in few cases physicians were hesitant/reluctant to change the prescription immediately while in other cases suggestions provided were considered as either to be insignificant or with inadequate evidences. In seven cases, suggestions were neither accepted nor were therapy changed. One of the major reasons for this could be that the pharmacist failed to understand the sophisticated prescribing behavior, i.e., prescribing decisions governed by the clinical experiences of the physicians. In few cases, experienced physicians did not change their routine prescribing pattern especially in the case of interventions of ‘minor’ significance. In few cases, it could be due to the lack of convincible answer provided by the pharmacist. In four cases, it was unclear whether or not there was change in drug therapy as patients were not follow-up owing to their discharge or death of the patients.
Only those interventions that were accepted and resulted in change in drug therapy were considered for the cost implications. In our study, the annualized cost savings due to pharmacist-initiated changes to drug therapy was found to be Rs.135205.22. Dooley et al.[14] reported the annualized cost savings of Rs: 21,33,50,112 [US$4444794]. The difference in the annualized cost savings between these two studies is due to the fact that difference in the study population and number of hospitals included in the study. Dooley et al.[14] study was conducted at eight major acute care hospitals with a well-trained and experienced pharmacists. However, our study was conducted in a single teaching hospital. Moreover, in our study, the intervening pharmacist is a postgraduate student with minimal experience on drug therapy reviewing and managing DRPs. In addition, there could be differences in the charges of laboratory tests, hospital stay charges, drug cost, etc.
The overall observation made from this study was that pharmacists have greater responsibility preventing and/or minimizing DRPs occurring in intensive care settings.
CONCLUSION
In conclusion, clinical pharmacists not only have greater potential in preventing and/or minimizing the DRPs, but also have potential to reduce the unnecessary healthcare expenditures arising from DRPs occurring in patients treated in intensive care settings.
RECOMMENDATIONS
Identifying DRPs and making patient-specific recommendations by a trained clinical pharmacist may reduce the unnecessary healthcare expenditures. Active participation of a clinical pharmacist in the intensive care settings may greatly improve the patient outcome. The clinical pharmacist involvement in the drug therapy decision may help/assist healthcare professionals in the overall management of patient.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Haley hill. A career as a critical care pharmacist. Hos Pharm. 2005;12:359–61. [Google Scholar]
- 2.Rao M, Suhasini T. Organization of intensive care unit and predicting outcome of critical illness. Indian J Anaesth. 2003;47:328–37. [Google Scholar]
- 3.Said M, Takrouri M. Intensive Care Unit. Internet J Health. 2004;3 Available from: http://www.ispub.com/ostia/index.php?xmlFilePath=journals/ijh/vol3n2/icu.xml . [Google Scholar]
- 4.Task force on position paper on Critical care pharmacy service, Society of Critical Care Med and American Collage of Clinical Pharmacy. Position paper on Critical care pharmacy services. Pharmacotherapy. 2000;20:1400–6. [PubMed] [Google Scholar]
- 5.Lee AJ, Chiao TB, Lam JT, Khan S, Maureen S. Improving medication safety in the ICU: The pharmacist's role. Hos Pharm. 2007;42:337–44. [Google Scholar]
- 6.Capsy A, Rozenfeld V, Kleyman J. Prevention of medication errors in the hospital settings; The role of pharmacy students. PandT. 2005;30:183–5. [Google Scholar]
- 7.Sandra KG, Rhonda SR, Margaret M, Verrico, Weber RJ. Adverse drug event rates for high cost and high use drugs in the intensive care units. Am J HealthSyst Pharm. 2006;19:1876–81. doi: 10.2146/ajhp060045. [DOI] [PubMed] [Google Scholar]
- 8.Santell JP. Medication errors in intensive care units. US Pharm. 2006;5:56–9. [Google Scholar]
- 9.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am JHosp Pharm. 1990;47:533–4. [PubMed] [Google Scholar]
- 10.Timmins A. The contribution of intensive care pharmacist in the United Kingdom. Pharm J. 2000;265:341–4. [Google Scholar]
- 11.MacLaren R, Devlin JW, Martin SJ, Dasta JF, Rudis MI, Bond CA. Critical care pharmacy services in United States hospitals. Ann Pharmacother. 2006;40:612–8. doi: 10.1345/aph.1G590. [DOI] [PubMed] [Google Scholar]
- 12.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am JHosp Pharm. 1990;47:533–4. [PubMed] [Google Scholar]
- 13.Rasmussen M, Struck P. A. Pilot study of pharmacist initiated interventions in drug therapy in an Australian pediatric hospital. EJHP. 2007;13:105–12. [Google Scholar]
- 14.Dooley MD, Allen MK, Doecke JC, Galbraith JK, Taylor GR, Bright J, et al. Prospective multicentre study of pharmacist initiated changes to drug therapy and patient management in acute care government funded hospitals. BrJ ClinPharmacol. 2003;57:513–21. doi: 10.1046/j.1365-2125.2003.02029.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parthasarathi G, Ramesh M, Krishna Kumar J, Madaki S. Assessment of drug-related problems and clinical pharmacists’ interventions in an Indian teaching hospital. J Pharm PractRes. 2003;33:272–4. [Google Scholar]


