Sir,
The use of loading dose diazepam for the treatment of alcohol withdrawal was first described by Sellers et al.[1] The same was used successfully in Indian patients by Manikant et al.[2] It involves the administration of 20mg oral diazepam every 2 h until the patient is drowsy, but arousable. Symptoms of alcohol withdrawal are monitored using the Clinical Institutes Withdrawal Assessment for Alcohol - Revised (CIWA-Ar) scale.[3] Further doses are withheld whenever CIWA-Ar scores fall below 8. The major advantages of this method include faster recovery from delirium, lower total doses of diazepam and a lesser risk of complications like withdrawal seizures and arrhythmias.
We use loading dose diazepam to treat alcohol withdrawal in our in-patient de-addiction unit at JIPMER. A chart review involving 25 consecutive admissions of alcohol use disorders between 1st August and 15th November, 2011 was conducted. The goals of the review were to identify the following:
-
1)
The success of loading dose diazepam in the treatment of the alcohol withdrawal state; and
-
2)
The clinical variables that determine the success or failure of loading dose regimen.
“Successful treatment” was defined as follows:
-
a)Resolution of delirium within 24 h; or
-
b)The ability to prevent any complications like seizures or delirium after admission in patients who presented with severe but uncomplicated withdrawal.
-
a)
As noted in Figure 1, out of the 25 admissions, 15 patients (60%) had significant withdrawal symptoms at admission (CIWA-Ar > 8). Nine (60%) of them had a complicated withdrawal state at presentation (one with seizures alone, three with withdrawal seizures and delirium and five with delirium alone).
Figure 1.
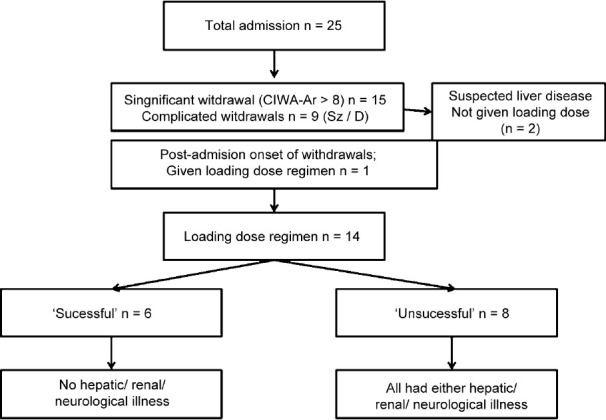
Number of patients admitted and given loading dose diazepam
In six out of fourteen (42.85%) patients given loading dose diazepam, it was successful. Four of them did not have any comorbid illness. One was hypertensive. One had panic disorder. None of them had hepatic, renal or neurological disease. All six had bilirubin levels under 1mg/dl. The diazepam dose required in this group was 40 to 80mg. Only one of them required haloperidol (5mg) for control of his agitation. Four of the six patients were delirious at presentation. None had seizures.
All eight patients who failed to respond to the loading dose strategy had medical comorbidities. The comorbidities are presented in Table 1. This group of patients required between 40 to 200mg diazepam during the loading phase. Four (50%) of them required haloperidol or other antipsychotic medications in addition.
Table 1.
Comorbidities in patients who failed loading dose diazepam therapy
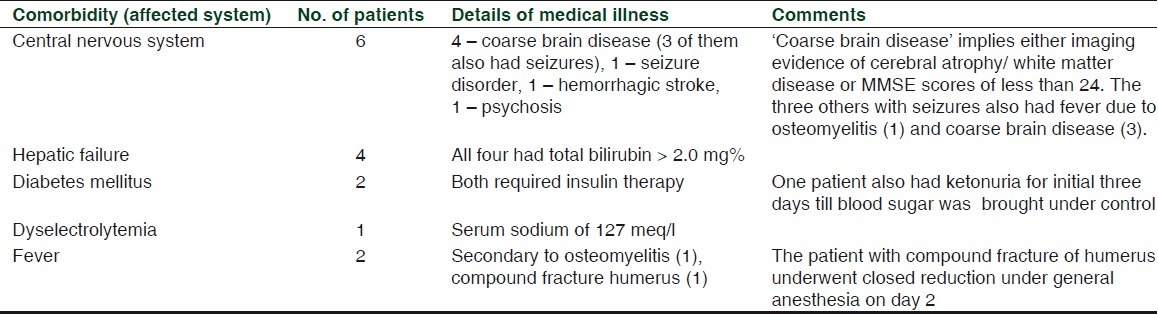
The most striking finding in this chart review is that all eight patients who failed diazepam loading had medical comorbidities, including three with multiple comorbidities. The most common comorbid condition in our experience was neurological disorder. This included evidence of coarse brain disease in the form of brain atrophy on imaging and/or cognitive decline on Mini-Mental Status Examination. Hepatic dysfunction was the second most common comorbidity. The CIWA-Ar total and orientation item scores remained high in patients who had failed the loading dose regimen. These patients had persistent disorientation and delirium despite adequate control of autonomic signs (such as tachycardia and hypertension) within a period of 24 to 36 h. They were not given further doses of diazepam. This alerts us to the pitfall of excessive reliance on the CIWA-Ar to monitor treatment of alcohol withdrawal delirium. The diagnosis of delirium tremens remains a clinical one. The CIWA-Ar scale should be used to assess the severity alone. The CIWA-Ar does not take into account the signs of autonomic overactivity which are important features of alcohol withdrawal. So the CIWA-Ar may not be useful in medically ill patients in alcohol withdrawal has been pointed out previously.[4]
Alcohol users with medical illnesses have increased morbidity.[5] Periodic review of the patient's clinical status and further investigations to detect other comorbidities should be strongly considered in those whose delirium fails to resolve in 24 to 36 h after 60 to 80mg of loading dose diazepam. The landmark trial by Sellers et al.[1] showed a similar dose requirement of diazepam (median dose = 60mg). Physicians who manage alcohol withdrawal delirium need to be alert to this subset of patients with “DT plus” syndromes whose delirium may have other underlying medical causes in addition to alcohol withdrawal which need to be promptly detected and treated.
This study, despite the limitations of a chart review, has two important learning points for physicians managing alcohol withdrawal states in a general hospital setting. First, extensive evaluation for medical comorbidities, particularly neurological and hepatic diseases should be repeated in patients whose delirium tremens does not resolve with 60 to 80mg of diazepam loading and within 24 to 36 h. Second, the CIWA-Ar alone may not be a useful indicator of delirium tremens as patients with “DT plus” syndromes score high on it. Monitoring autonomic signs and the clinical status remain important for safe administration of the loading dose.
REFERENCES
- 1.Sellers EM, Naranjo CA, Harrison M, Devenyi P, Roach C, Sykora K. Diazepam loading: Simplified treatment of alcohol withdrawal. Clin Pharmacol Ther. 1983;34:822–6. doi: 10.1038/clpt.1983.256. [DOI] [PubMed] [Google Scholar]
- 2.Manikant S, Tripathi BM, Chavan BS. Loading dose diazepam therapy for alcohol withdrawal state. Indian J Med Res. 1993;98:170–3. [PubMed] [Google Scholar]
- 3.Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. Assessment of alcohol withdrawal: The revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar) Br J Addict. 1989;84:1353–7. doi: 10.1111/j.1360-0443.1989.tb00737.x. [DOI] [PubMed] [Google Scholar]
- 4.Bostwick JM, Lapid MI. False positives on the clinical institute withdrawal assessment for alcohol-revised: Is this scale appropriate for use in the medically ill? Psychosomatics. 2004;45:256–61. doi: 10.1176/appi.psy.45.3.256. [DOI] [PubMed] [Google Scholar]
- 5.Rosenbaum M. Change diagnosis to “alcohol withdrawal delirium”? Am J Psychiatry. 2003;160:1357–8. doi: 10.1176/appi.ajp.160.7.1357-a. [DOI] [PubMed] [Google Scholar]


