In a recent Editorial on the role of antifungal treatment in hematology, Maertens et al. analyzed the diagnostic and therapeutic antifungal strategies which are used in particular in neutropenic patients.1 Among the various topics covered, some observations concerned antifungal prophylaxis. They underlined some critical issues of antifungal prophylaxis including the lack of evidence of its impact on overall survival, the need to redefine clinical end points for future studies on antifungal prophylaxis, and the problem of the reduced incidence of invasive Aspergillus disease in patients receiving a mold-active antifungal which may be partially explained by the lower performance of the galactomannan (GM) enzyme immunoassay.
A retrospective evaluation of the diagnostic performance of the GM assay in patients with invasive aspergillosis was carried out in three trials of prophylaxis and treatment of invasive fungal diseases in stem cell transplant patients.2 Here, for the first time, it was shown that the diagnostic usefulness of this test while receiving prophylactic treatment or treatment with antifungal drugs is compromised.
Administration of a mold-active antifungal drug on the day of testing decreased the sensitivity of the GM assay from 89% to 52% using a 0.5 cut off. However, in this study it was not specified how many samples had been collected for GM assay while patients were under antifungal prophylaxis or under intravenous antifungal therapy. Furthermore, GM detection tests and radiological exams were performed in absence of a pre-specified diagnostic strategy.
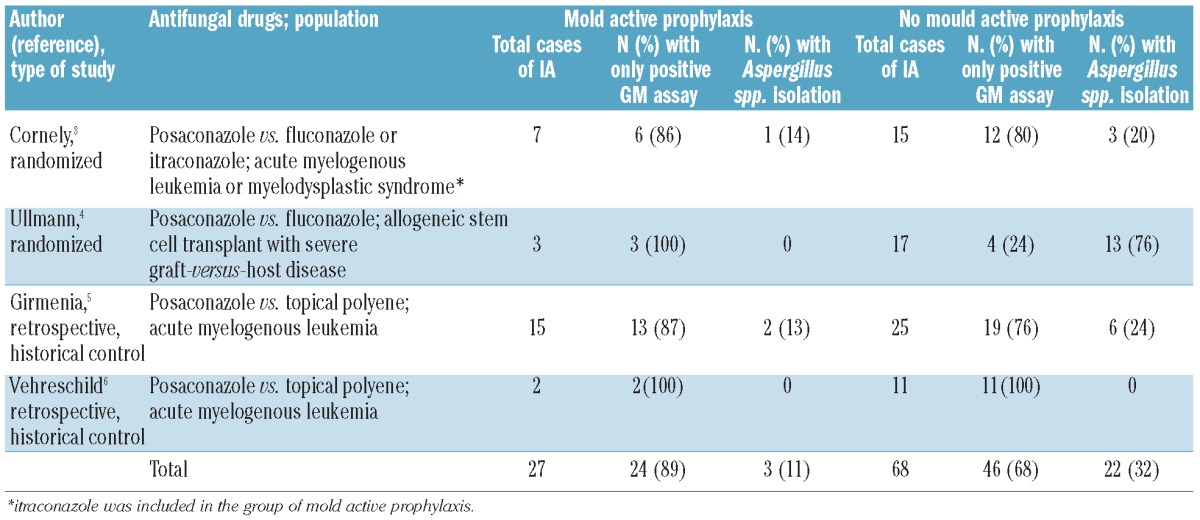
Recent controlled studies demonstrating the efficacy of posaconazole antifungal prophylaxis do not seem to confirm these findings.3-6 GM assay sensitivity was not reduced by the mold active prophylaxis: 89% in patients receiving posaconazole or itraconazole versus 68% in patients receiving fluconazole or topical polyene (Table 1). In particular, in our center we recently applied the same pre-defined intensive diagnostic workup in patients with persistent or recurrent febrile neutropenia regardless of the type of antifungal prophylaxis. It included GM serum detection over three consecutive days, chest computed tomography and other examinations as indicated.5,7 There was no reduction in the rate of Aspergillus infections documented with the GM assay or in the median value of the serum GM peak in patients receiving posaconazole, and we did not observe any increase in purely clinically documented (possible) pulmonary fungal infections in this group. This would have happened if there had been a lower performance of the GM assay.
Table 1.
Microbiological diagnosis in patients with invasive aspergillosis in recent controlled trials of antifungal prophylaxis according to antimold activity of the antifungal drug.
A well known cause of failure of antifungal prophylaxis with posaconazole is represented by the erratic gastrointestinal absorption of the drug.8 Assuming that reduced absorption of posaconazole, leading to sub-therapeutic serum concentrations, could explain the occurrence of breakthrough Aspergillus infections, normal production and spread of GM by the fungal pathogen in these cases seems to be likely, as confirmed by the above studies.
In conclusion, GM assay continues to be the gold standard of microbiological diagnosis of invasive Aspergillus infections in hematologic patients regardless of the antifungal prophylaxis used.
Supplementary Material
Footnotes
The information provided by the authors about contributions from persons listed as authors and in acknowledgments is available with the full text of this paper at www.haematologica.org.
Financial and other disclosures provided by the authors using the ICMJE (www.icmje.org) Uniform Format for Disclosure of Competing Interests are also available at www.haematologica.org.
References
- 1.Maertens JA, Nucci M, Donnelly JP. The role of antifungal treatment in hematology. Haematologica. 2012;97(3):325-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marr KA, Laverdiere M, Gugel A, Leisenring W. Antifungal therapy decreases sensitivity of the Aspergillus galactomannan enzyme immunoassay. Clin Infect Dis. 2005;40(12):1762-9 [DOI] [PubMed] [Google Scholar]
- 3.Cornely OA, Maertens J, Winston DJ, Perfect J, Ullmann AJ, Walsh TJ, et al. Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med. 2007;356(4):348-59 [DOI] [PubMed] [Google Scholar]
- 4.Ullmann AJ, Lipton JH, Vesole DH, Chandrasekar P, Langston A, Tarantolo SR, et al. Posaconazole or fluconazole for prophylaxis in severe graft-versus-host disease. N Engl J Med. 2007;356(4):335-47 [DOI] [PubMed] [Google Scholar]
- 5.Girmenia C, Frustaci AM, Gentile G, Minotti C, Cartoni C, Capria S, et al. Posaconazole prophylaxis during front-line chemotherapy of acute myeloid leukemia: a single-center, real-life experience. Haematologica. 2012;97(4):560-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vehreschild JJ, Rüping MJ, Wisplinghoff H, Farowski F, Steinbach A, Sims R, et al. Clinical effectiveness of posaconazole prophylaxis in patients with acute myelogenous leukaemia (AML): a 6 year experience of the Cologne AML cohort. J Antimicrob Chemoth. 2010;65(7):1466-71 [DOI] [PubMed] [Google Scholar]
- 7.Girmenia C, Micozzi A, Gentile G, Santilli S, Arleo E, Cardarelli L, et al. Clinically driven diagnostic antifungal approach in neutropenic patients: a prospective feasibility study. J Clin Oncol. 2010;28(4):667-74 [DOI] [PubMed] [Google Scholar]
- 8.Girmenia C. New generation azole antifungals in clinical investigation. Expert Opin Inv Drugs. 2009;18(9):1279-95 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


