Abstract
Background
Standardization in clinical practice may lead to improved outcomes. Unfortunately, little is known about the variability of non-pharmacological anti-infective measures in children with cancer.
Design and Methods
A web-based survey assessed institutional recommendations regarding restrictions of social contacts, pets and food and instructions on wearing face masks in public for children with standard- risk acute lymphoblastic leuk emia and acute myeloid leukemia during intensive chemotherapy.
Results
A total of 336 institutions in 27 countries responded to the survey (range, 1-76 institutions per country; overall response rate 61%). Most institutions recommend that patients with acute myeloid leukemia avoid indoor public places and daycare, kindergarten and school, whereas recommendations for patients with acute lymphoblastic leukemia differ considerably by institution. In terms of restrictions related to pets, there was a wide variability between institutions for both acute lymphoblastic and acute myeloid leukemia patients. Most, but not all institutions do not allow children with either acute lymphoblastic or acute myeloid leukemia to eat raw meat, raw seafood or unpasteurized milk. Whereas most institutions do not routinely recommend that patients with acute lymphoblastic leukemia wear face masks in public, advice on this matter varies for patients with acute myeloid leukemia.
Conclusions
The survey demonstrates that there is a wide variation in recommendations on non-pharmacological anti-infective measures between different institutions, countries and continents. This information may be used to encourage harmonization of supportive care practices and future clinical trials.
Key words: acute lymphoblastic leukemia, acute myeloid leukemia, child, infection, non-pharmacological anti-infective measures
Introduction
Infections are common and important complications in children with cancer. In particular, children receiving high intensity chemotherapy such as those with relapsed acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML) and those undergoing allogeneic hematopoietic stem cell transplantation are at higher risk of infectious morbidity and mortality.1,2 In order to prevent infectious complications, a number of pharmacological strategies have been developed including prophylaxis with antimicrobial agents or growth factors.3-5
It has been demonstrated that there is wide variability in these pharmacological approaches,6 which is undesirable for many reasons. First, standardization of supportive care may result in improved outcomes. This has primarily been shown for disease treatment outcomes through standardization of cancer therapy and testing new regimens on a common backbone,7,8 but has also been demonstrated for supportive measures.9 Second, variability in management complicates care at an institutional level and may lead to dissatisfaction in patients if therapy changes as they move between different institutions. Third, variation in supportive care interventions makes it more difficult to identify treatment- or patient-related prognostic factors.
Pharmacological measures are often costly and may be associated with drug-drug interactions and toxicities. Thus, there is much interest in non-pharmacological strategies to prevent infections and these approaches are widely used. However, non-pharmacological approaches may reduce quality of life and increase burden of care from both an institutional and parental perspective.10 In contrast to pharmacological strategies, almost nothing is known about variability in non-pharmacological anti-infective practices in children with cancer. This knowledge is, however, important as it may help centers to benchmark their own practices and it may highlight where research could be feasible and useful.
The objectives of this survey were to describe variability in social contacts, contacts with pet, food restrictions and face mask policies among an international group of institutions that care for children with ALL and AML.
Design and Methods
We performed an international, web-based survey of non-pharmacological anti-infective-measures. The survey included questions on the institutions' demographics, whether policies were documented and standardized, and how policies were disseminated (Appendix 1, Online Supplementary Appendix). Institutional recommendations regarding restrictions of social contacts, pets and food, and policies on wearing face masks in public were also determined. Social restrictions evaluated were related to indoor public places, outdoor public places, friends visiting at home, daycare, kindergarten and school beyond kindergarten. Pet restrictions evaluated were related to dogs, cats, turtles, hamsters/guinea pigs and birds. Food restrictions evaluated were related to raw seafood or meat, unpasteurized milk/cheese, uncooked/unpeeled vegetables, salad, nuts, take-away food and tap water. Recommendations were described for two disease scenarios: children with standardrisk ALL and any risk AML during intensive chemotherapy. Activity restrictions were categorized as: always restricted, restricted under certain circumstances and never restricted. The survey was extensively pilot-tested prior to dissemination.
Centers in Europe, the United States of America, Canada, Central and South America, Australia and New Zealand were included. For each country, a single key person was identified and that person disseminated the survey within their country. One survey was distributed to each center, typically to the head of the pediatric hematology/oncology department. Up to two reminders were sent to non-respondents. The survey was distributed in English and Spanish.
In order to describe the global restriction for each center, a scoring system was developed in which each question received a score of 2 for always restricted, 1 for sometimes restricted, and 0 for no restrictions, thus creating a summary variable “restriction score” for social contacts, pets at home and food.10 The summary restriction score was a maximum of 12 for social contacts (6 items), 16 for food (8 items) and 10 for pets (5 items), with higher numbers representing more restrictions.
Institutional review board approval was obtained by centers that required approval for participation; however, almost all centers did not require submission or approval.
Statistical analysis
Descriptive analyses are reported for the demographics of the center and individual recommended policies regarding social contacts, pets at home and food. A comparison of the summary restriction scores was performed using the Wilcoxon rank sum test or analysis of variance (ANOVA). A two-sided P value of less than 0.05 was considered statistically significant. All analyses were conducted using GraphPadPrism (version 5.04).
Results
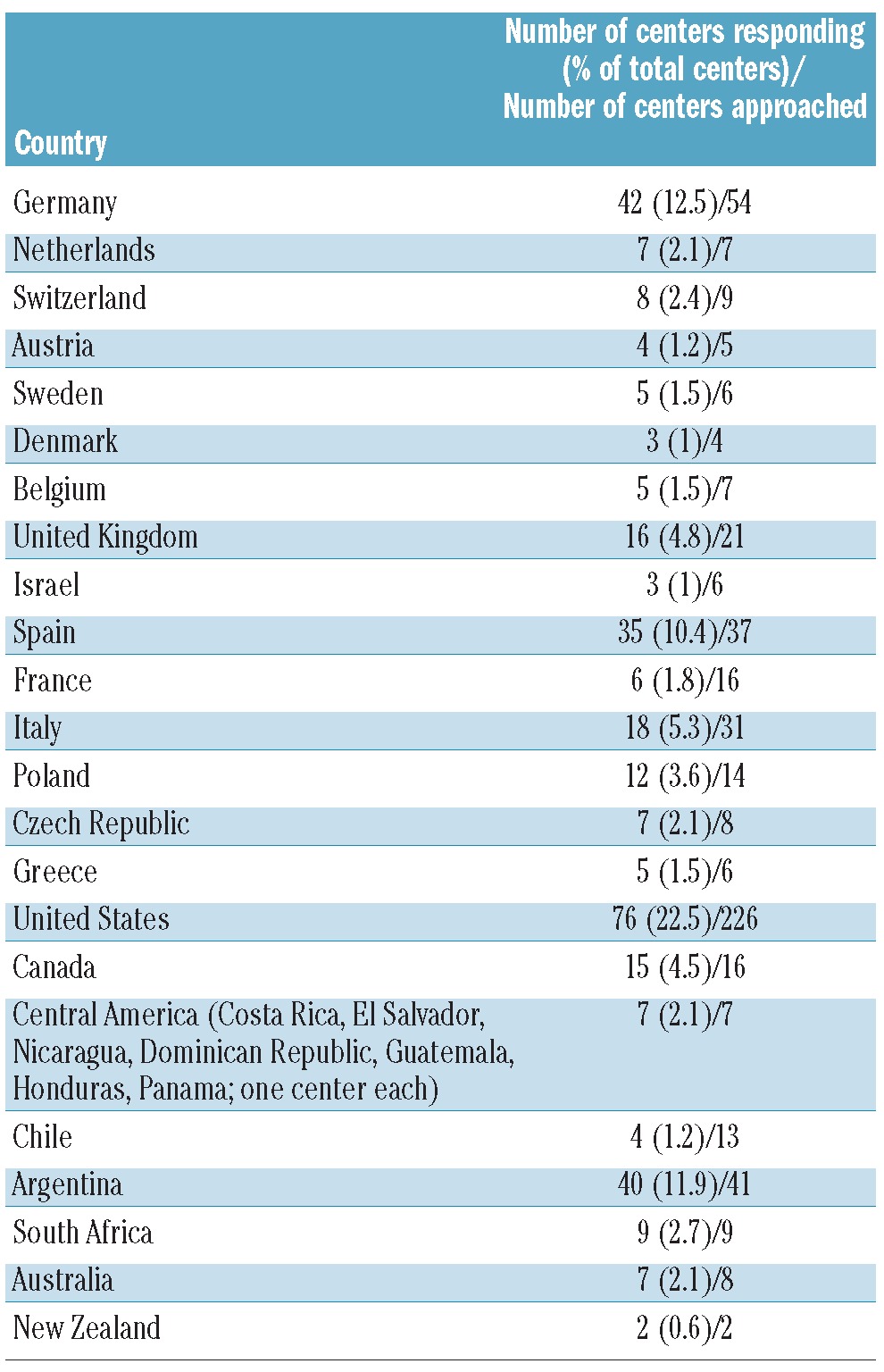
A total of 336 institutions in 27 countries responded to the survey [range, 1-76 institution per country; overall response rate 61% (range per country, 34-100%)] (Table 1). Most centers had fewer than 20 newly diagnosed patients with ALL [<10: 120 centers (36%); 10-19: 112 centers (33%); 20-40: 73 centers (22%); >40: 31 centers (9%)] and fewer than five newly diagnosed patients with AML per year [<5: 231 centers (68%); 5-10: centers 26 (8%); >10: 79 centers (24%)].
TABLE 1.
Participating centers by country and size of institutions.
Thirty-two percent of centers (n=107) had a written policy for non-pharmacological anti-infective approaches and 64% (n=64) a general agreement without a written policy, whereas in 25% (n=85), an individualized approach was used by each practitioner. A physician and a nurse were involved in the instruction of parents in 89% (n=299) and 71% (n=238) of cases, respectively, and a handout was distributed in 52% of cases (n=174) (the percentages do not add up to 100% since respondents could choose more than one response). A handout was the only information given in 4% of cases (n=14), whereas 42% of the parents received a handout and were additionally instructed verbally by both a physician and a nurse (n=141).
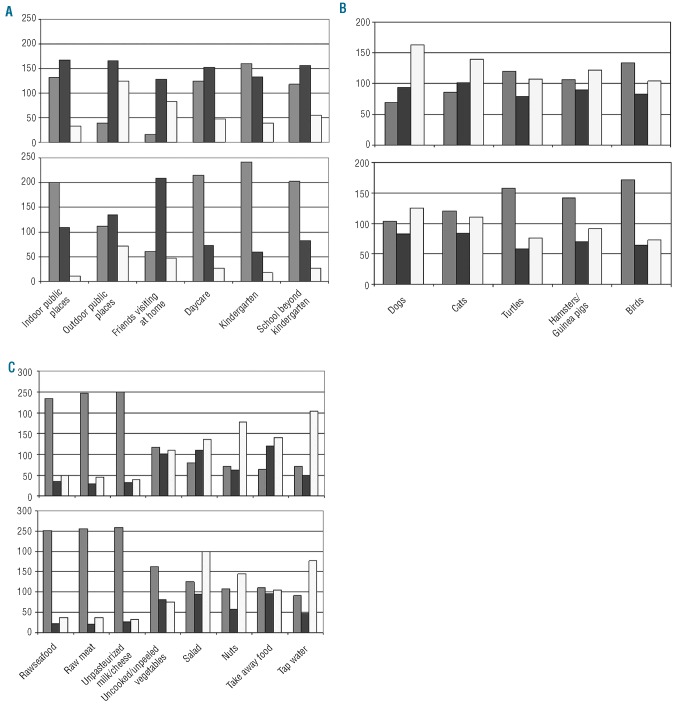
Figures 1 illustrates the frequency that social contacts, pets and food are restricted when categorized as always restricted, restricted under certain circumstances and never restricted. Most centers do not allow children with AML to visit indoor public places or to attend daycare, kindergarten or school (Figure 1A). In contrast, recommendations for patients with ALL vary considerably. Restrictions under certain circumstances are mostly related to neutropenia (58%) and to chemotherapy regimens (e.g., more restrictions during induction; 17%). The health of surrounding people (friends without cold allowed to visit, school only if others are healthy, etc.) is a common pre-condition for reduced restrictions (16%).
Figure 1.
(A) Social restrictions in acute lymphoblastic leukemia (ALL; top) and acute myeloid leukemia (AML; bottom). (B) Pet restrictions in acute lymphoblastic (ALL; top) and acute myeloid leukemia (AML; bottom). (C) Food restrictions in acute lymphoblastic leukemia (ALL, top) and acute myeloid leukemia (AML; bottom). Gray bars represent always restricted, black bars represent restricted under certain circumstances and white bars represent never restricted.
In terms of restrictions related to pets, there is wide variability between institutions with regards to patients with both ALL and AML (Figure 1B). Restrictions under certain circumstances were related to appropriate hand-washing after contact (27%), keeping animals already in the home but restricting the purchase of new pets (25%), restriction of pets in the bedroom or on the bed (22%), ensuring that pets were assessed by a veterinary specialist (17%) and restriction of cleaning cages or litter (16%).
Figure 1C illustrates restrictions related to food. Most institutions do not allow raw meat, raw seafood, or unpasteurized milk for either ALL or AML patients. Nonetheless, some institutions do permit these food items, even for patients with AML. In contrast, there is a wide variability, seen across all countries, in other food restrictions, regarding salad, nuts, take-away food, and unpeeled vegetables. Restrictions under certain circumstances are generally related to neutropenia and specific chemotherapy regimens (for example, restriction during induction therapy or with steroid therapy) (68%). If uncooked vegetables or salad are allowed, appropriate cleaning of food was advised (12%).
Thirty institutions (9%) suggest that children with ALL always wear face masks in public while 114 (34%) suggest this for children with AML. Conversely, 181 institutions (54%) never suggest face masks in public in childhood ALL, while 138 institutions (41%) never suggest face masks in public for children with AML.
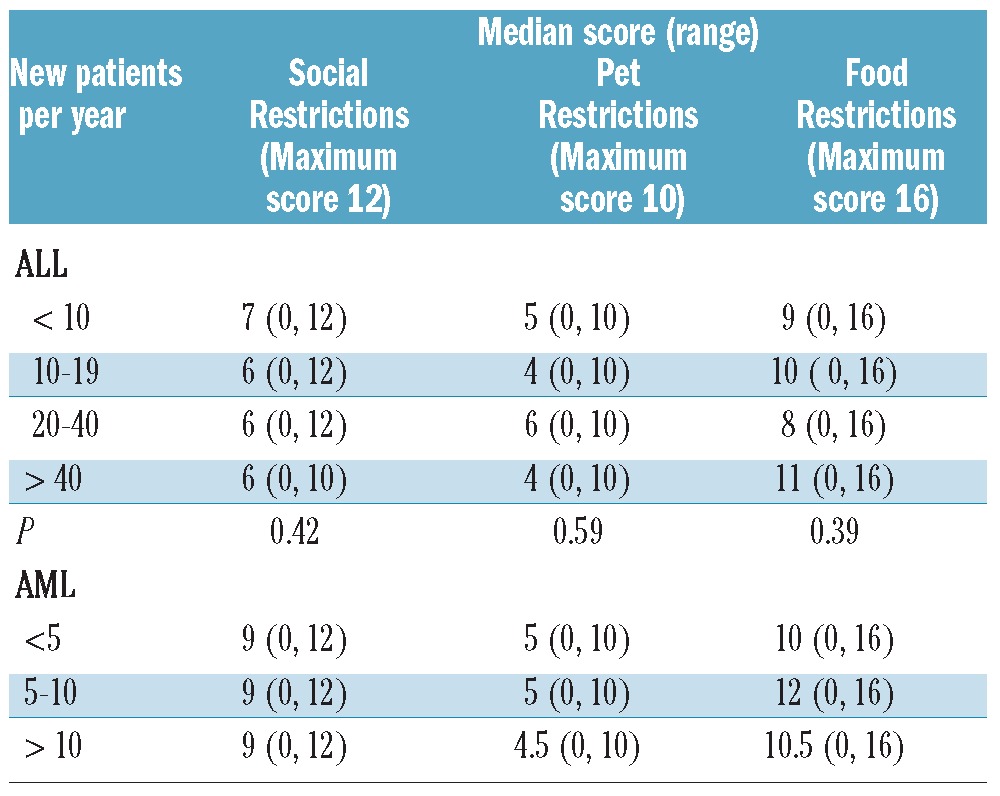
Tables 2 and 3 and Online Supplementary Table S1 show the restriction summary scores for social contacts, pets and food depending on continent and on center size; higher scores reflect more restrictions. Great variability was demonstrated in all the analyses, independently of whether the population considered had ALL or AML. This variability was also demonstrated within countries, independently of the continent (Online Supplementary Table S1). The restriction scores were higher in Europe than in the USA/Canada and the difference was statistically significant for almost all comparisons (Table 2). Similarly, for restrictions of social contacts, pets at home, and food, the restriction sores were significantly lower for ALL patients than for AML patients (Table 2). In contrast, the restriction scores did not differ significantly between centers of different sizes (Table 3).
TABLE 2.
Restriction scores* by country and underlying malignancy.
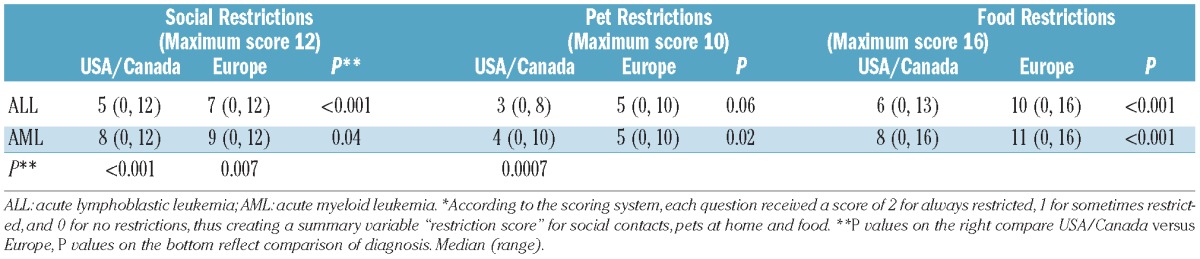
TABLE 3.
Restriction scores by center size.
Discussion
We found that there are wide variations in non-pharmacological anti-infective measures between different institutions, countries and continents, and that the restriction score is driven mainly by underlying diagnosis and geography and not by center size. This variability is similar to the variation in pharmacological anti-infective strategies used in Europe and USA/Canada for children with AML.6
The current rationale for recommending restrictions of social contacts, pets and food is based on prospective cohort studies performed in the 1970s. For example, in one of these trials, leukemia patients were placed in a total protective environment including isolation tents, laminar air flow and sterile diet (“neutropenic diet”).11 In this setting, patients were found to tolerate higher doses of chemotherapy with less toxicity, including infections. Although these early studies suggested that a protective environment may offer some protection from infection, most of the recommendations have never been tested in larger randomized trials. Smaller randomized studies did not find positive effects of well-fitting face-masks in the prevention of invasive mold infection in 80 adults with leukemia or patients undergoing allogeneic hematopoietic stem cell transplantation,12 or of a neutropenic diet in 19 children receiving myelosuppressive chemotherapy.13 The latter trial corroborates the results of studies in adults.14,15 However, most of the studies are weakened by a number of limitations such as insufficient sample size or the absence of documentation of other variables that affect the incidence of infectious complications.
Given the paucity of evidence, it is not surprising that available recommendations are not standardized,16-18 which may account, at least in part, for the variations demonstrated in our survey. Notably, we found that some centers, independently of geographic location, did not restrict the consumption of unpasteurized milk or raw meat even though most recommendations suggest that these items should be excluded from the diet of even non-immunocompromised individuals.19 Consequently, variability in these practices suggests that education may be important. In contrast, some variability may be legitimately related to unique geographical needs such as the risk of contaminated tap water, although we have demonstrated large variability among similar countries with universally safe tap water.
We acknowledge many limitations in this study. First, this study was primarily descriptive and we could not assess whether the interventions were effective. Secondly, there are likely to be legitimate unique features such as availability of clean tap water that may affect some practices. Thirdly, our study recorded an institutional practice from the perspective of a single individual. There is likely to be intra-institutional variability in practices and we did not measure this variability in the study. Lastly, there is likely to be a significant difference between an institutional recommendation and implementation of that recommendation with variable levels of compliance; we did not measure these elements in our study.
Nonetheless, the results of this survey may have important implications. First, since standardization of therapy and testing new regimens on a common backbone was thought to be important to the improvement of disease control, by analogy, standardization of supportive care measures and testing of interventions with a common backbone of supportive care strategies may allow us to reduce infectious complications in a more rapid and more efficient manner.7,8 Secondly, since restrictions may negatively affect the quality of life of children and their families, variability in supportive care measures may ultimately result in dissatisfaction of patients and lower compliance.10 On the other hand, we may be able to describe comparative effectiveness of such practices if we could identify institutions that are otherwise similar with different practices although such an analysis would be highly susceptible to confounding variables. Finally, this variability highlights the need for evidence- based guidelines regarding these issues.
In conclusion, this survey demonstrates that there are wide variations in non-pharmacological anti-infective measures for children with cancer between different institutions, countries and continents. This information may be used to encourage harmonization of supportive care practices and future clinical trials.
Supplementary Material
Acknowledgments
we thank all the participating physicians for the time they spent responding to the survey. We thank Marie-Chantal Ethier for her help in developing the survey, María Laura Lanzeni and Marco Baz Bartels for translating the survey, and Roswitha Lehne for assistance in preparing the manuscript.
Funding: this study had no sponsor or funding source.
Footnotes
Part of this work was presented at the 43rd Congress of the International Society of Paediatric Oncology (SIOP), October 26-30 2011, Auckland, New Zealand.
The online version of this article has a Supplementary Appendix.
Authorship and Disclosures: The information provided by the authors about contributions from persons listed as authors and in acknowledgments is available with the full text of this paper at www.haematologica.org.
Financial and other disclosures provided by the authors using the ICMJE (www.icmje.org) Uniform Format for Disclosure of Competing Interests are also available at www.haematologica.org.
References
- 1.Castagnola E, Bagnasco F, Faraci M, Caviglia I, Caruso S, Cappelli B, et al. Incidence of bacteremias and invasive mycoses in children undergoing allogeneic hematopoietic stem cell transplantation: a single center experience. Bone Marrow Transplant. 2008; 41(4):339–47 [DOI] [PubMed] [Google Scholar]
- 2.Sung L, Lange BJ, Gerbing RB, Alonzo TA, Feusner J. Microbiologically documented infections and infection-related mortality in children with acute myeloid leukemia. Blood 2007; 110(10):3532–9 [DOI] [PubMed] [Google Scholar]
- 3.Rungoe C, Malchau EL, Larsen LN, Schroeder H. Infections during induction therapy for children with acute lymphoblastic leukemia. the role of sulfamethoxazoletrimethoprim (SMX-TMP) prophylaxis. Pediatr Blood Cancer. 2010;55(2):304–8 [DOI] [PubMed] [Google Scholar]
- 4.Bochennek K, Tramsen L, Schedler N, Becker M, Klingebiel T, Groll AH, et al. Liposomal amphotericin B twice weekly as antifungal prophylaxis in pediatric high risk patients. Clin Microb Infect. 2011; 17(12):1868–74 [DOI] [PubMed] [Google Scholar]
- 5.Sung L, Nathan PC, Lange B, Beyene J, Buchanan GR. Prophylactic granulocyte colony-stimulating factor and granulocytemacrophage colony-stimulating factor decrease febrile neutropenia after chemotherapy in children with cancer: a meta-analysis of randomized controlled trials. J Clin Oncol. 2004; 22(16):3350–6 [DOI] [PubMed] [Google Scholar]
- 6.Lehrnbecher T, Ethier MC, Zaoutis T, Creutzig U, Gamis A, Reinhardt D, et al. International variations in infection supportive care practices for paediatric patients with acute myeloid leukaemia. Br J Haematol. 2009; 147(1):125–8 [DOI] [PubMed] [Google Scholar]
- 7.Schrappe M, Reiter A, Zimmermann M, Harbott J, Ludwig WD, Henze G, et al. Longterm results of four consecutive trials in childhood ALL performed by the ALL-BFM study group from 1981 to 1995. Berlin- Frankfurt-Münster. Leukemia. 2000; 14(12):2205–14 [DOI] [PubMed] [Google Scholar]
- 8.Sander A, Zimmermann M, Dworzak M, Fleischhack G, von Neuhoff C, Reinhardt D, et al. Consequent and intensified relapse therapy improved survival in pediatric AML: results of relapse treatment in 379 patients of three consecutive AML-BFM trials. Leukemia. 2010; 24(8):1422–8 [DOI] [PubMed] [Google Scholar]
- 9.Hargrave DR, Hann II, Richards SM, Hill FG, Lilleyman JS, Kinsey S, et al. Progressive reduction in treatment-related deaths in Medical Research Council childhood lymphoblastic leukaemia trials from 1980 to 1997 (UKALL VIII, X and XI). Br J Haematol. 2001; 112(2):293–9 [DOI] [PubMed] [Google Scholar]
- 10.Lehrnbecher T, Laws HJ, Boehm A, Dworzak M, Janssen G, Simon A, et al. Compliance with anti-infective preventive measures: a multicentre survey among paediatric oncology patients. Eur J Cancer. 2008; 44(13):1861–5 [DOI] [PubMed] [Google Scholar]
- 11.Moody K, Charlson ME, Finlay J. The neutropenic diet: what's the evidence? J Ped Hematol Oncol. 2002; 24(89):717–21 [DOI] [PubMed] [Google Scholar]
- 12.Maschmeyer G, Neuburger S, Fritz L, Böhme A, Penack O, Schwerdtfeger R, et al. A prospective, randomised study on the use of well-fitting masks for prevention of invasive aspergillosis in high-risk patients. Ann Oncol. 2009; 20(9):1560–4 [DOI] [PubMed] [Google Scholar]
- 13.Moody K, Finlay J, Mancuso C, Charlson M. Feasibility and safety of a pilot randomized trial of infection rate: neutropenic diet versus standard food safety guidelines. J Ped Hematol Oncol. 2006; 28(3):126–33 [DOI] [PubMed] [Google Scholar]
- 14.DeMille D, Deming P, Lupinacci P, Jacobs LA. The effect of the neutropenic diet in the outpatient setting: a pilot study. Oncol Nurs Forum. 2006; 33(2):337–43 [DOI] [PubMed] [Google Scholar]
- 15.Gardner A, Mattiuzzi G, Faderl S, Borthakur G, Garcia-Manero G, Pierce S, et al. Randomized comparison of cooked and noncooked diets in patients undergoing remission induction therapy for acute myeloid leukemia. J Clin Oncol 2008; 10(35):5684–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kommission für Krankenhaushygiene und Infektionsprävention beim Robert Koch- Institut (RKI) Anforderungen an die Hygiene bei der medizinischen Versorgung von immunsupprimierten Patienten. Bundesgesundheitsbl. 2010; 53:357–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zitella LJ, Friese CR, Hauser J, Holmes Gobel B, Woolery M, O′Leary C, et al. Putting evidence into practice: prevention of infection. Clin J Oncol Nurs. 2006; 10(6):739–50 [DOI] [PubMed] [Google Scholar]
- 18. U.S. Department of Agriculture Food safety of people with cancer. http://www.fsis.usda.gov/PDF/Food_Safety_for_People_with_Cancer.pdf Accessed November 14, 2011
- 19.U.S. Food and Drug Administration (FDA) Raw milk may pose health risk. http://www.fda.gov/ForConsumers/ConsumerUpdates/ucm232980.htm Accessed November 18, 2011
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.