Abstract
Background
In angioimmunoblastic T-cell lymphoma, symptoms linked to B-lymphocyte activation are common, and variable numbers of CD20+ large B-blasts, often infected by Epstein-Barr virus, are found in tumor tissues. We postulated that the disruption of putative B-T interactions and/or depletion of the Epstein-Barr virus reservoir by an anti-CD20 monoclonal antibody (rituximab) could improve the clinical outcome produced by conventional chemotherapy.
Design and Methods
Twenty-five newly diagnosed patients were treated, in a phase II study, with eight cycles of rituximab + chemotherapy (R-CHOP21). Tumor infiltration, B-blasts and Epstein-Barr virus status in tumor tissue and peripheral blood were fully characterized at diagnosis and were correlated with clinical outcome.
Results
A complete response rate of 44% (95% CI, 24% to 65%) was observed. With a median follow-up of 24 months, the 2-year progression-free survival rate was 42% (95% CI, 22% to 61%) and overall survival rate was 62% (95% CI, 40% to 78%). The presence of Epstein-Barr virus DNA in peripheral blood mononuclear cells (14/21 patients) correlated with Epstein-Barr virus score in lymph nodes (P<0.004) and the detection of circulating tumor cells (P=0.0019). Despite peripheral Epstein-Barr virus clearance after treatment, the viral load at diagnosis (>100 copy/μg DNA) was associated with shorter progression-free survival (P=0.06).
Conclusions
We report here the results of the first clinical trial targeting both the neoplastic T cells and the microenvironment-associated CD20+ B lymphocytes in angioimmunoblastic T-cell lymphoma, showing no clear benefit of adding rituximab to conventional chemotherapy. A strong relationship, not previously described, between circulating Epstein-Barr virus and circulating tumor cells is highlighted.
Key words: angioimmunoblastic T-cell lymphoma, angioimmunoblastic T-cell lymphoma, CHOP-R, Epstein-Barr virus
Introduction
Angioimmunoblastic T-cell lymphoma (AITL), one of the most frequent peripheral T-cell lymphomas,1 usually affects elderly patients in their sixth or seventh decade.2 It is clinically characterized by widespread lymphadenopathy, and commonly, extranodal disease, immune-mediated hemolysis, and polyclonal hypergammaglobulinemia.3 The recent identification of the follicular helper T cell (TFH) as the cell of origin of this lymphoma4,5 represents a major step in the understanding of the clinicobiological characteristics of the disease.6 This T-cell subset promotes positive selection, proliferation and differentiation of germinal center antigen-specific B cells.7 The TFH derivation of AITL provides a rationale to explain the common expansion of B cells, the plasmacytic infiltrate in tumor biopsies, and the hypergammaglobulinemia as well as the immune dysfunction manifestations of the disease.8
The clinical course of AITL is variable, with occasional spontaneous remissions, but overall its prognosis is poor with affected patients having a median overall survival of less than 3 years in most studies.6 Various treatment strategies, ranging from watching and waiting to combination chemotherapy, have proven largely insufficient. Different combinations of chemotherapeutic drugs, such as cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) and CHOP-like regimens, have failed to increase the 5-year survival rate to more than 35%.9,2 Several attempts to add drugs to CHOP, such as etoposide10 and bleomycin in the MACOP-B,11 also proved unsuccessful. In a large, retrospective Groupe d’Etude des Lymphomes de l’Adulte (GELA) study of AITL patients who had been enrolled into different therapeutic protocols,2 no positive impact on survival was observed for any treatment, even among patients submitted to consolidation with autologous stem cell transplantation (ASCT). For younger and fitter patients the indication for consolidative ASCT remains under debate12,13 but alternative strategies need to be developed for elderly patients.
One peculiar pathological feature of AITL is the highly variable proportion of neoplastic T cells, sometimes minor, compared to the reactive component made up of small lymphocytes, histiocytes, eosinophils, plasma cells, and B immunoblasts, suggesting a role of the microenvironment in maintenance of tumor cell viability. Epstein-Barr virus (EBV)-infected B-blasts are detected in most AITL.14 The biological significance and pathophysiological implications of this observation are still unclear. EBV infection/reactivation can occur as a consequence of an underlying “immune dysfunction”, but no correlation between EBV and immune parameters has been documented in AITL. EBV may, through the modulation of cytokines, chemokines and membrane receptors, play a paracrine role either in the development of the tumor microenvironment,15 or in tumor cell survival, ultimately favoring disease progression.
Taking into account both the B-cell hyperstimulation stigmata associated with an increased number of B cells present in tumor tissue of AITL and the putative feeder role of B cells or EBV-infected B cells for neoplastic T cells, we postulated that AITL patients might benefit from treatment with an anti-CD20 monoclonal antibody (rituximab) in combination with an anthracycline-containing chemotherapy protocol. Here we report the results of a phase II clinical trial in which patients aged 60 to 80 years with newly diagnosed AITL were treated with a combination of rituximab and CHOP (R-CHOP). The pathological features of the tumors and the clinically relevant immuno-biological and viral parameters were analyzed in detail and correlated to the clinical features.
Design and Methods
Study design
The study was a multicenter, phase II, open-label, non-randomized trial evaluating the efficacy of R-CHOP, delivered every 3 weeks, in patients aged 60 to 80 years with a first diagnosis of AITL. Patients were enrolled in 11 participating centers of the GELA.
Patients were eligible if they had not been previously treated (except with steroids initiated less than 10 days before inclusion) and had good performance status (ECOG PS ≤2). Additional eligibility requirements included unaltered renal and hepatic function, and adequate bone marrow reserve (neutrophils > 1.5×109/L and platelets >100×109/L) unless alterations were related to the disease. Non-eligibility criteria included contra-indications to any drug included in the R-CHOP regimen, a life expectancy of less than 3 months, and central nervous system or meningeal involvement by lymphoma. Patients with human immunodeficiency virus infection or an active hepatitis B or hepatitis C infection were also excluded as were subjects with a previous history of cancer (except an adequately treated non-melanoma skin cancer or in situ cervical cancer) during the preceding 5 years.
Initial staging included physical examination, standard laboratory assessments, Coombs’ test, gammaglobulin levels, computed tomography (CT) scans of the chest, abdomen and pelvis, and a bone marrow biopsy.
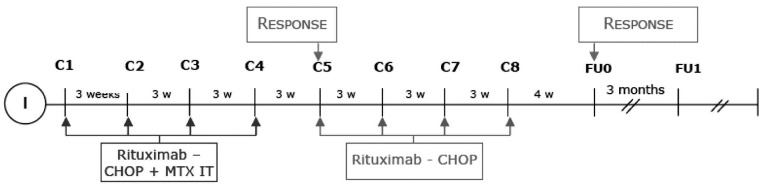
Patients were treated with R-CHOP (cyclophosphamide 750 mg/m2, vincristine 1.4 mg/m2 (capped at 2 mg), doxorubicin 50 mg/m2 on day 1, and prednisone 100 mg on days 1–5, each cycle repeated every 3 weeks combined with an infusion of 375 mg/m2 rituximab) as shown in Figure 1. Patients received 15 mg of intrathecal methotrexate on day 1 of the first four cycles. A midterm evaluation was performed after four cycles, and responders (see below) received four additional cycles. Granulocyte colony-stimulating factor (G-CSF) support was not planned. In the case of severe neutropenia or neutropenia-related infection, subcutaneous G-CSF was recommended from day 6 to day 13 or until the neutrophil count was ≥1.0x109/L, for subsequent cycles.
Figure 1.
Study design. Rituximab was administered on day 1, before doxorubicin (50 mg/m2), cyclophosphamide (750 mg/m2), and vincristine (total dose 1.4 mg) and after prednisone (40 mg/m2). A midterm evaluation was performed after four R-CHOP cycles, and responders received another four cycles.
Study management
The GELA was the sponsor of the study. On-site monitoring was organized in each center. All case report forms were sent to the GELA central operation office (GELA-RC) and double data entry was undertaken for verification purposes. Outliers and erroneous values were checked routinely. Queries and on-site monitoring data were used for final validation, and the GELA-RC had full control of the database. Statistical analyses were performed by the statistical department of the GELA-RC.
The protocol was approved by local ethic committees according to French laws and the study was conducted in accordance with the Declaration of Helsinki. Patients were required to provide written informed consent prior to registration. The study is registered with clinicaltrials.gov (NCT00169156) and had the EudraCT number 2005-002602-37.
Toxicity and response assessments
Hematologic and non-hematologic toxicities were graded according to the National Cancer Institute Common Toxicity Criteria (version 3.0). Toxicity was evaluated on day 1 of each treatment cycle and included a laboratory assessment with complete blood cell count and serum chemistry tests.
Response to induction was first evaluated at midterm, 2 weeks after the fourth cycle. Patients who obtained a complete response, an unconfirmed complete response or a partial response according the International Working Group Criteria16 received four additional cycles. Final response assessment was performed 3 to 4 weeks after the last cycle of R-CHOP and required a bone marrow biopsy unless the initial biopsy had been negative.
Follow-up assessments included clinical evaluation every 3 months and CT scans every 6 months for an additional 3-year period.
Histological and immunohistochemical analyses and scoring
Pathological specimens were centrally reviewed in the GELA-Pathology institute (GELA-P) and the diagnosis of AITL was confirmed by at least two expert hematopathologists based on the criteria of the World Health Organization classification.1 Slides were stained with hematoxylin-eosin and Giemsa and with an appropriate panel of antibodies directed against B-cell antigens (CD20, CD79a), T-cell antigens (CD3, CD2, CD5, CD7, CD4), follicular dendritic cell antigens, CD1017 and TFH-associated molecules, (PD1, CXCL13), as previously described.18 The diagnosis was based on the following criteria: partial or diffuse effacement of the nodal architecture, polymorphous cellular infiltrate, vascular proliferation with prominent arborization of high endothelial venules, extrafollicular meshwork of follicular dendritic cells, an atypical population of CD3+ T cells, and the presence of large CD20+ B-cell blasts with or without evidence of EBV infection. Cases were classified according to the three patterns described by Attygale.17 The presence of EBV was investigated by in situ hybridization with probes specific for EBV-encoded small RNA (EBER1 and 2) sequences.2
All cases were scored by two expert pathologists (LdL, PG) for the assessment of neoplastic T-cell content, large B-cell infiltration as well as for the number of EBV-infected cells. The abundance of tumor cells in proportion to overall cellularity was semi-quantitatively evaluated according to a score varying from 1 to 3, with score 1 signifying <30%; score 2 signifying 30-50% and score 3 signifying >50%. The abundance of B-blasts, based on counting large CD20+ cells in five to ten high-power microscopic fields (hpf) (Olympus BX40), was expressed as a mean per hpf and assigned score 1 when there were fewer than 5 B-blasts, score 2 when there were between 5 to 50 and score 3 when there were more than 50 and/or sheets/aggregates of large CD20+ cells. The abundance of EBV-infected cells was measured by counting the number of EBER-positive cells in five randomly selected hpf and expressed as a score ranging from 1 to 3 with score 1 indicating fewer than 5, score 2 indicating 5 to 15 and score 3 indicating more than 15 with or without sheets/aggregates.
Peripheral blood and lymph node sampling
Peripheral blood samples were referred at diagnosis and at the time of clinical response evaluation to the Immunobiology Laboratory of Henri Mondor Hospital Center, Creteil. Lymphocyte subpopulations were analyzed by flow cytometry on diagnostic fresh samples (see below). Plasma samples of 1 mL were placed in vials and stored at -80°C for further analyses. Mononuclear cells (PBMC) were isolated from 40 mL peripheral blood by Ficoll-hypaque density gradient centrifugation, dispatched to 10 million cell pellet aliquots and stored at -80°C. Frozen or fixed and paraffin embedded sections of lymph node were referred for DNA extraction.
DNA extraction
DNA was obtained from lymph node samples using a standard proteinase K digestion and phenol/chloroform extraction. PBMC DNA was obtained from the frozen pellets using qiasymphony automated extraction (Qiagen®), while DNA was extracted from plasma samples by means of a QIAamp DNA blood minikit from Qiagen®.
Flow cytometry
Absolute counts of T CD4 (CD3+ CD4+), T CD8 (CD3+ CD8+), and B (CD19+) peripheral blood lymphocyte subsets were determined directly using Cyto-Stat tetraCHROME™ (Beckman-Coulter). The presence of circulating tumor T cells was assessed by at least one of the following criteria: (i) CD3–CD4+ immunophenotype; 19 (ii) total or partial loss of pan-T antigens CD2, CD5, or CD7, using a combination of CD2-FITC, CD7-RD1, CD3-ECD, CD4-TRI, CD5-PC7; and (iii) co-expression of CD10.20 All antibodies were from Beckman-Coulter. Flow cytometry was performed on a Coulter FC500 within 24 h after staining. List-mode parameters were analyzed and stored on CXP™ software (Beckman-Coulter).
Normal values were as follow:21 CD3+ T cells (536–1787 cells/mm3); helper CD4+ T cells (309–1139 cells/mm3); cytotoxic CD8+ T cells (137–823 cells/mm3); B cells expressing CD19 (72–460 cells/mm3).
B and T lymphocyte clonality analyses
T-cell receptor gamma chain gene analysis was performed by GC-clamp multiplex polymerase chain reaction (PCR) and denaturing gradient gel electrophoresis as previously described.22 A dominant peripheral blood T-cell clone was considered as neoplastic when the same electrophoretic imprint could be documented in the tumor lymph node.23 For immunoglobulin heavy chain (FR1/JH, FR2/JH, FR3/JH) and light chain (IGK, IGKDE) rearrangement studies, PCR were performed according to the Biomed 2 protocol.24 Samples with an intense, unique or weak, dominant peak on a polyclonal background were considered as clonal, those with multiple dominant peaks were considered as oligoclonal and those with a polyclonal pattern as non-clonal.
Epstein-Barr virus status: genome detection and quantification, serology
EBV DNA amplifications were performed using Mix fast DNA LC (Roche Molecular Systems®) and analyzed in real-time on a Light Cycler system (Roche Molecular Systems®). A sequence of 169 bp from the BXLF1 gene coding for viral thymidine kinase was amplified using primers and probes described by Brengel-Pesce et al.25 EBV DNA was quantified by means of an external standard curve constructed using 10-fold dilutions of a plasmid DNA containing the 169 bp fragment. Results were expressed as number of copies per mL of plasma or per μg of PBMC DNA by means of β-globin quantification. Specific anti-EBV antibodies (IgG anti-VCA, IgG anti-EBNA and IgM anti-VCA) were sought in serum samples using LIAISON® kits (Liaison® EBV VCA IgG, Liaison® EBV VCA IgM and Liaison® EBV EBNA).
Statistical methods
The primary endpoint was the complete response rate, including complete response and unconfirmed complete response at the end of treatment. Previous studies using CHOP reported an estimated overall response rate of 40% in patients with AITL.26 In order to detect an overall response rate higher than 40% after eight cycles of R-CHOP, we calculated, using a triangular test procedure every five patients, that a sample size of 25 assessable patients recruited over 2 years would provide 80% power at an overall 5% (2-sided) significance level. As one of the secondary endpoints, progression-free survival was measured from the date of inclusion into the study to date of progression/relapse or death from any cause. Overall survival was calculated from the date of enrollment until death from any cause.
Progression-free survival and overall survival were estimated using the product-limit method of Kaplan–Meier and compared using the log-rank test on an intent-to-treat basis; data were censored at the date of last evaluation when the stopping date (September 1, 2009) was not reached. Correlations between response rate, patients’ characteristics and biological data (circulating lymphocyte phenotype, EBV status, T/B clonality) were analyzed using Fisher’s exact test. Statistical tests were considered significant when the two-sided P value was less than 0.05. Confidence intervals (CI) were computed with a 95% coverage; 95% CI binomial exact bounds were computed for proportions. All statistical analyses were performed using SAS software (version 8.2; SAS Institute, Cary, NC, USA).
Results
Clinical presentation of patients
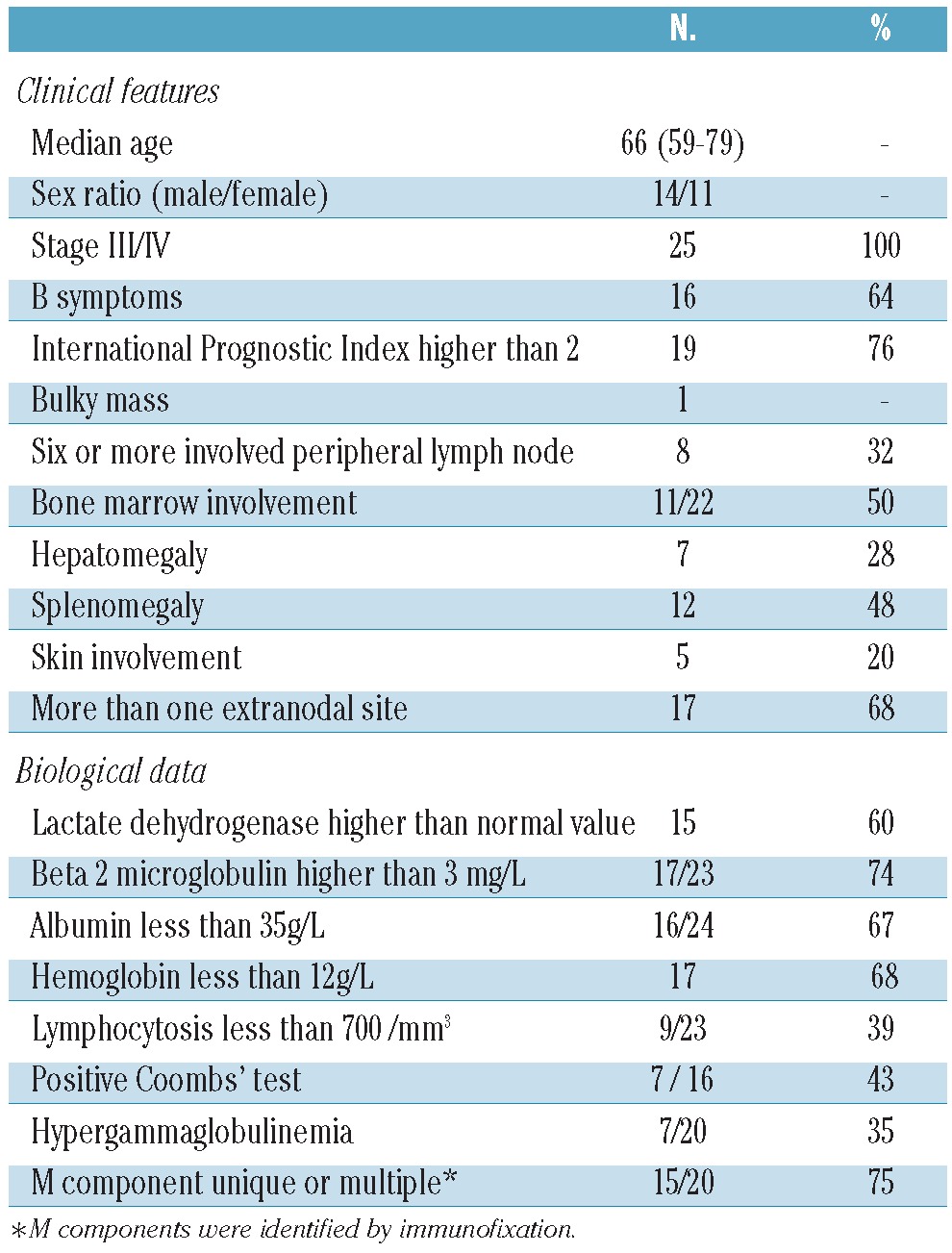
Between December 2005 and January 2008, 27 patients were enrolled and 25 were eligible for analysis: two patients were withdrawn before receiving any treatment, one retracted his informed consent and another had active hepatitis B. The patients’ pretreatment characteristics are summarized in Table 1. Their median age was 68 years (range, 60 to 79 years) and all had extensive disease including 22 (88%) with stage IV. Seventeen patients (68%) presented with more than one extranodal site involved.
Table 1.
Clinical and biological characteristics of the 25 enrolled patients at inclusion.
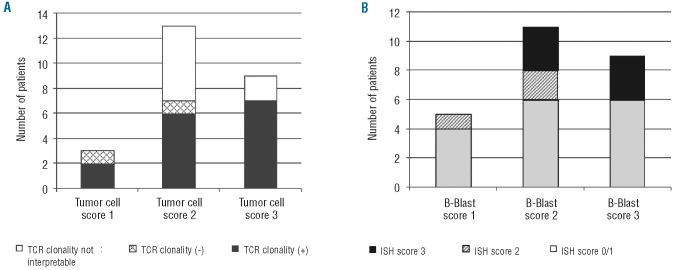
Pathological presentation
The pathological review process confirmed histopathological and immunophenotypic features of AITL in all cases. They corresponded to pattern III AITL with diffuse infiltration in most (n=17) cases. Results of tumor cell density scoring and T-cell clonality are summarized in Figure 2A. The abundance of B-blasts and EBER+ cells within the tumor was scored. Two-thirds of patients had more than five CD20+ blasts per hpf (score 2 and 3) (Figure 2B) whereas 23 patients (92%) had EBV-infected cells. The number of CD20+ B-blasts was not significantly correlated with either the number of EBV-infected cells (Figure 2B) (P=0.5) or with B-cell clonality (for details on individual patients, see Online Supplementary Table S1).
Figure 2.
T-cell, B-cell and EBV scoring in tumor biopsies. All the cases were scored by two expert pathologists (LdL, PG) for the assessment of (A) neoplastic T-cell content. Score 1: less than 30%; score 2: 30-50%, score 3, more than 50%, (B) large B-cell infiltration. score 1, less than 5; score 2, 5 to 50; score 3, more than 50 and/or sheets/aggregates of large CD20+ cells as well as for the number of EBV-infected cells. Score 1, less than 5; score 2, 5 to 15; score 3, more than 15 with or without sheets/aggregates). T-cell clonality (A) was analyzed by PCR on frozen or paraffin sections. All reported non-interpretable results were from fixed paraffin-embedded tissues.
Immunological presentation
Hypergammaglobulinemia was found in 7/20 patients. More precisely, two-thirds of the patients had over-representation of at least one immunoglobulin class in serum, mostly IgA. Immunofixation showed a monoclonal component in two patients, and an oligoclonal pattern (multiple peaks) in 11 patients. By including quantitative and qualitative alterations, only one patient had an apparently normal immunoglobulin repertoire (for details on individual patients, see Online Supplementary Table S2).
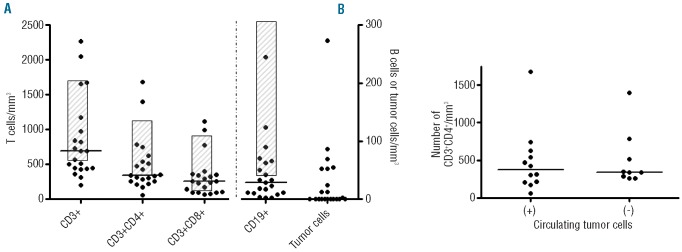
Flow cytometry was performed on peripheral blood in 21/25 patients. A highly variable absolute lymphocyte count was found (Figure 3A). The most frequent quantitative abnormality was T-cell lymphopenia (CD3+ <600/mm3) in 10/21 (47%) patients. It was related to a single subset deficiency, CD4 (n=3), or CD8+ (n=1), but more frequently to both (n=6). The same variability was found in the B-cell compartment, with often profound deficiency (<20/mm3, n=9) mostly associated with CD3+ deficiency (n=5) (for details on individual patients, see Online Supplementary Table S2).
Figure 3.
Peripheral blood T- and B-cell counts at presentation. Absolute counts of peripheral blood lymphocytes subsets were obtained from total blood on a Coulter FC500 flow cytometer (Beckman-Coulter). (A) Normal CD3+, CD4+, CD8+, CD19 values21 are indicated by hatched boxes. Median patients’ values are indicated by a horizontal line. The left scale is used for CD3, CD4, CD8 counts and the right scale for CD19+ and tumor cells. The presence of circulating tumor T cells was assessed by at least one of the following criteria (i) CD3-CD4+ immunophenotype, (ii) total or partial loss of pan-T antigens CD2, CD5, or CD7 (iii) co-expression of CD10. (B) Median and range of the CD4+ cell count in patients with (+) or without (-) circulating tumor cells.
Blood circulating tumor cells (3-273/mm3) were detected by flow cytometry and/or by PCR in 12 out of 22 patients (54%). Despite the CD4+ phenotype of lymphoma cells, the median absolute number of CD4 cells was similar and low in the group with [297/mm3 (63-1112)] and without [341/mm3 (257-1395)] circulating tumor cells (Figure 3B). Detection of circulating tumor cells was not related to bone marrow infiltration or tumor cell density in the diagnostic lymph node.
Epstein-Barr virus status in peripheral blood at diagnosis
Anti-VCA and anti-EBNA IgG were positive in 17/19 and 15/19 patients, respectively. EBV genome was found in PBMC in 14 out of 22 studied patients (median 1.103 cp/PBMC μg; range 6.100 to 5.104). This EBV detection correlated strongly with EBV quantification by EBER-in situ hybridization in lymph node biopsies (all patients with EBV in PBMC <100 copies/μg DNA had an EBER- in situ hybridization score <1, P=0.004) (Figure 4A).
Figure 4.
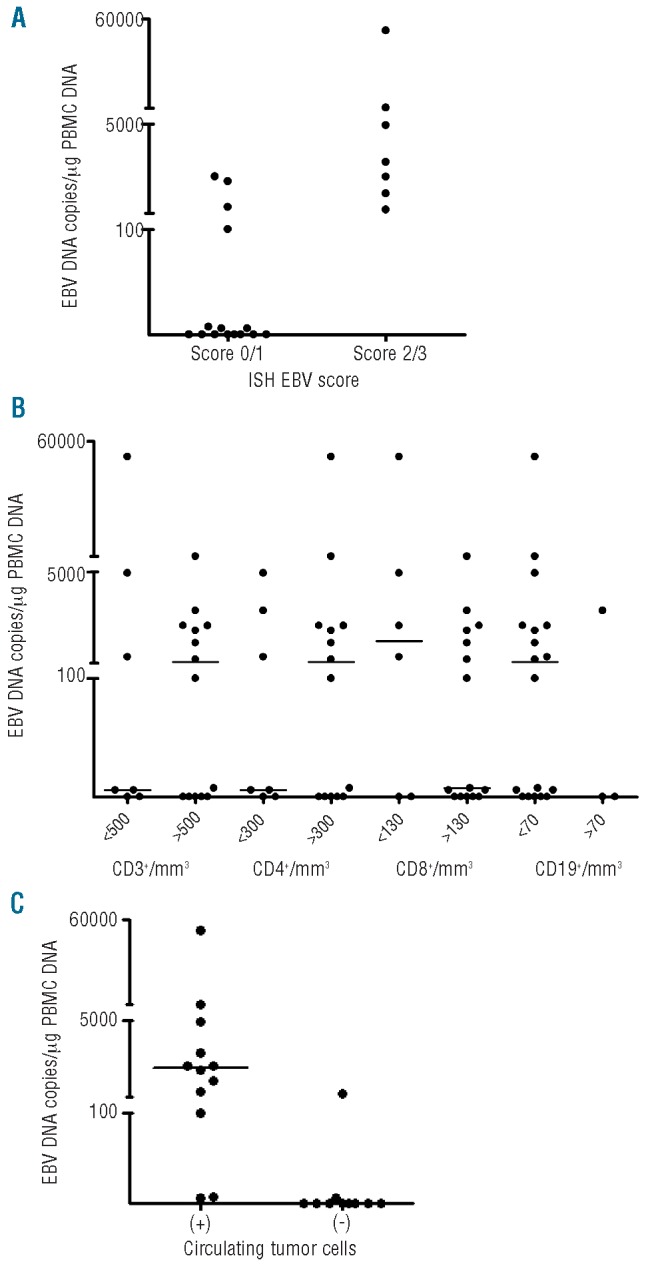
Peripheral EBV status at diagnosis. EBV DNA was quantified by real-time PCR on the Light Cycler system (Roche Molecular Systems®) using an external standard plasmid curve. Results were (A) correlated to in situ hybridization (ISH) EBV score, (B) lymphocyte subset count, and (C) circulating tumor cell detection.
EBV DNA normally lies inside circulating B lymphocytes, whereas patients with active EBV replication also have detectable viral DNA in plasma.27 We, therefore, decided to quantify EBV genome in plasma. Out of 20 tested patients, eight had detectable EBV DNA, including five with more than 1000 copies/mL plasma (Online Supplementary Table S3). Of note, one patient with negative EBV detection in lymph node, PBMC and sera had negative anti-EBV serology.
EBV genome in PBMC or in plasma was not associated with CD3+ lymphopenia, or with deficiency of CD4+ or CD8+ subsets (Figure 4B). By contrast, the presence of circulating EBV genome was strongly correlated with the presence of circulating tumor cells (P=0.0019) (Figure 4C).
Treatment exposure and toxicities
Four patients stopped treatment prematurely, two because of death from toxicity (one case of septicemia after cycle 2 and one case of septicemia with intestinal perforation after cycle 3), one because of disease progression (after cycle 4) and one after the physician’s decision (partial response after cycle 4). As a result, 21 patients (84%) completed the planned eight cycles, most of them receiving their treatment on an outpatient basis. The most common adverse events were hematologic toxicity. Grade 3–4 neutropenia and thrombocytopenia were reported in 72% and 25% of patients, respectively, during the first four cycles and in 60% and 4% during the subsequent four cycles. Accordingly, 21 patients required G-CSF. Only six documented infections were observed during the period of neutropenia. Of note, 14 of the 22 (64%) serious adverse events declared in nine patients were related to infections. One additional toxic death due to a chronic inflammatory demyelinating polyradiculoneuropathy was observed 5 months after the end of treatment, leading to a total number of three toxic deaths.
Clinical outcome
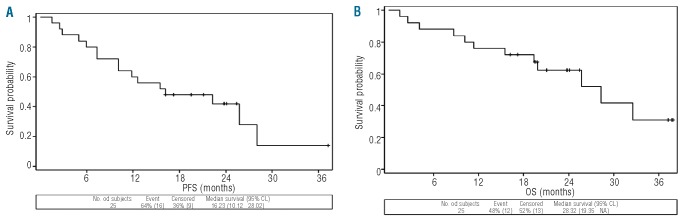
Response at the end of treatment was assessed after treatment completion for 21 patients and at premature withdrawal for four patients. Eleven patients achieved a complete or unconfirmed complete response (44%; 95% CI, 24% to 65%). Nine patients (36%) had a partial response, two patients progressed, and three died, including one with progressive lymphoma, leading to an overall response rate of 80% (CI, 59% to 93%). The median response duration was 25 months for patients achieving a complete or unconfirmed complete response (13.5-not reached).
With a median follow-up of 24 months (range, 2 to 38 months), the 2-year progression-free survival rate was 42% (95% CI, 22% to 61%) (Figure 5A) and the overall survival rate was 62% (95% CI, 40% to 78%) (Figure 5B). Six of the nine deaths that occurred between the end of treatment and the stopping date were attributed to lymphoma. Of note, no patients developed diffuse large B-cell lymphoma during the follow-up period, although some of them had sheets/clusters of B-blasts.
Figure 5.
Clinical outcome. (A) Progression-free survival (PFS). (B) Overall survival (OS).
Clinicobiological correlations
A relationship between rituximab-targeted cells evaluated at diagnosis and clinical outcome was determined. In univariate analysis, B-blast density in the tumor biopsy had no influence on clinical outcome, including response rate (Table 2). Although the detection of EBV copies in PBMC was not associated with response to treatment (P=0.6), (Table 2), it tended to be associated with a shorter progression-free survival (log-rank P=0.06) (Figure 6, Table 2). Circulating EBV was reviewed after treatment in 11 patients, five of whom were positive at diagnosis. Conversion to seronegativity was observed in four patients of whom three were in complete or complete unconfirmed response. The patient who remained positive was in partial response. Of note, out of the six EBV-negative patients at diagnosis, only one converted to being positive after treatment and was in partial response.
Table 2.
Main pathological and biological features and correlation with outcome.
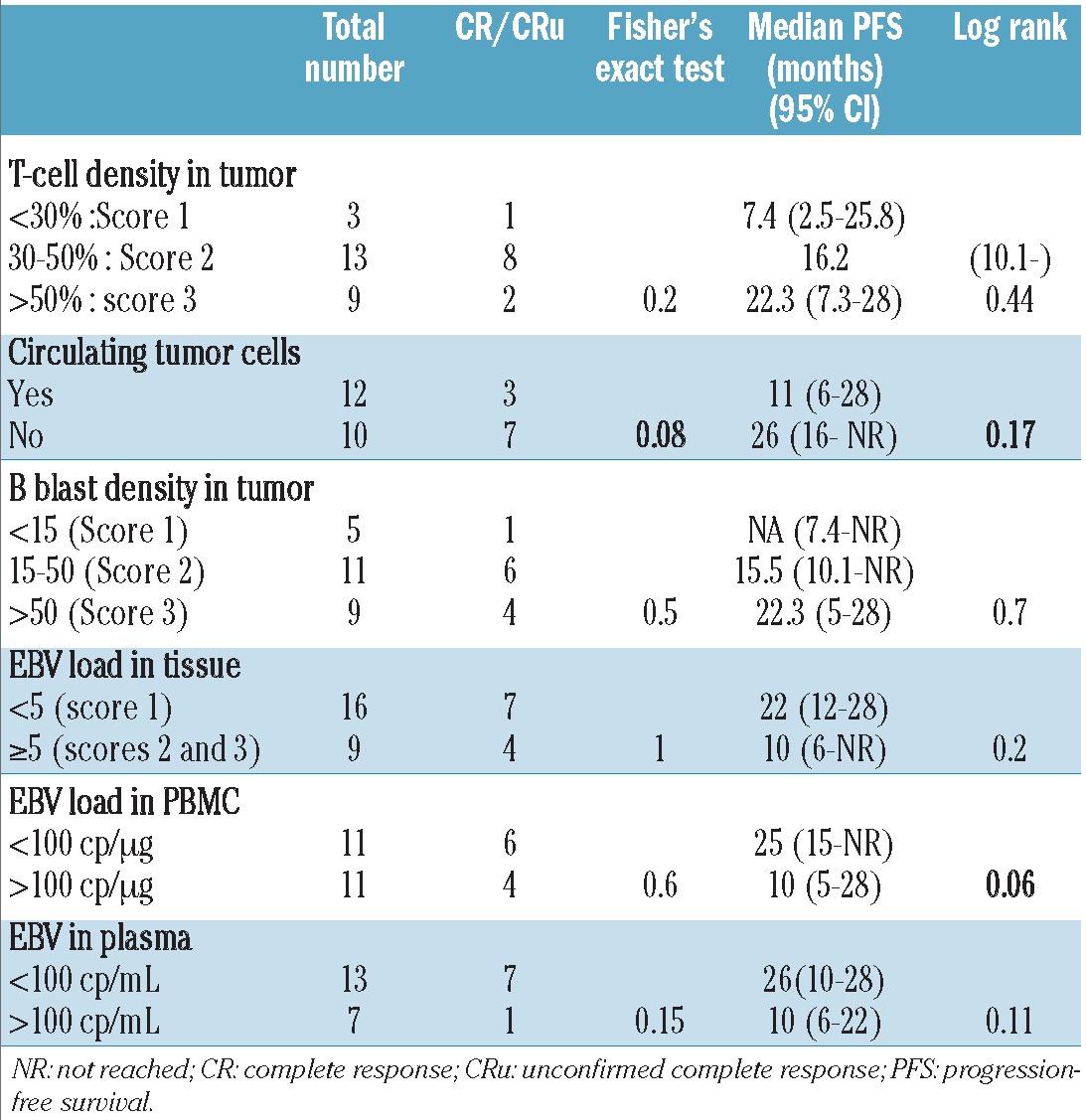
Figure 6.
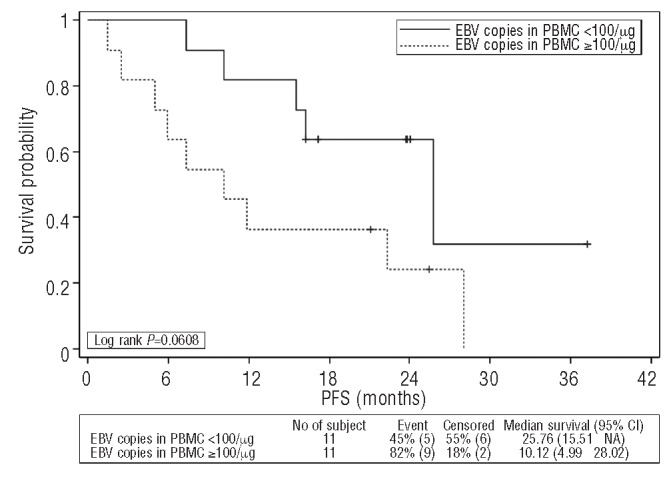
Progression-free survival (PFS) according to circulating EBV.
The close relationship between circulating EBV and circulating tumor cells prompted us to investigate the prognostic value of circulating tumor cells before treatment. The detection of circulating tumor cells tended to correlate with a poor response to treatment (75% of non-responders had detectable circulating tumor cells (P=0.08). However, in this limited series, it did not translate into a significantly worse progression-free survival (log-rank P=0.17) or overall survival (log-rank P=0.8).
Discussion
In this trial, rituximab combined with the CHOP regimen produced a high overall response rate (80%), including complete responses in 44% of elderly patients with AITL. Our goal was to target CD20+ cells, including EBV-infected B-blasts present in most AITL tumors, which might play a feeder role for tumor cell survival in lymph nodes. The hypothesis remains pertinent with regard to the recently published data showing that intrafollicular maintenance of the TFH phenotype requires the continued presence of antigen-specific B cells.28,29 However, in the absence of published data focusing specifically on AITL – and not on the more heterogeneous group of peripheral T-cell lymphomas – and more specifically on AITL patients over 60 treated with chemotherapy, it remains difficult to speculate on the potential benefit of R-CHOP in this small cohort. In the statistical design of the study, we might have overestimated the response to CHOP we referred to in this elderly population (40 to 45% of complete/unconfirmed complete response). Nevertheless, the response duration observed in this series is short and the progression-free survival is quite disappointing and close to that previously reported with CHOP alone.2 It is tempting to speculate that even if rituximab reduces the impact of B cells on tumor cell survival, part of the microenvironment persists after treatment and may favor residual TFH tumor cell re-emergence. Alternatively, residual TFH tumor cells could reconstitute a favorable microenvironment leading to subsequent relapse. For example, a recent report suggests that mast cells, recruited by CXCL13-secreting tumor TFH, could constitute a major component of the AITL microenvironment.30 Finally, treatment could select tumor cells with an acquired environmental autonomy. In the first hypothesis, the microenvironment has to be targeted more broadly and immunomodulatory drugs represent potential, good candidates.31 In the last two hypotheses, more effective therapies targeting neoplastic TFH cells are needed. Since our study design in 2006, numerous phase II studies have tested new drugs targeting T cells in patients with peripheral T-cell lymphoma, in association with CHOP or CHOP-like regimens, including alemtuzumab, a monoclonal anti-CD52 antibody,32 and denileukin diftitox, an interleukin-2 protein combined with diphtheria toxin.33 In addition to alemtuzumab, several novel monoclonal antibodies have shown some early promise in peripheral T-cell lymphoma, such as zanolimumab, a human monoclonal antibody targeting CD4 antigen.34 More exciting are novel monoclonal antibodies, currently being evaluated in autoimmune diseases, graft tolerance or antitumor immunity, which specifically target molecules expressed on AITL tumor cells, such as PD135 and ICOS.36
Our biological study focusing on B cells and EBV, which was conducted in parallel to the clinical trial in order to correlate a potential benefit of rituximab with biological features at diagnosis, provided original data regarding clinical practice and pathophysiological hypotheses. We found circulating tumor cells in 54% of patients. By comparing results of flow cytometry and PCR clonality analyses in routine practice, we found that an abnormal circulating T-cell clone is demonstrated more easily and more effectively by flow cytometry than by PCR. Moreover, in the clinical setting of a patient with clinically suspected AITL, complete T-cell phenotyping, including pan-T and CD10 markers, must be performed independently of the absolute T-cell count. Indeed, tumor cells were detected both in patients with (6/10) and without (3/11) lymphopenia.
As previously reported,14 we found the EBV genome in the great majority of tumor samples. This observation has been proposed as a strong argument for a pathophysiological driving role of EBV in AITL.6 In contrast, our results demonstrate that AITL can develop in the absence of EBV. Indeed, one patient had negative EBV serology, in addition to the absence of EBV genome in tumor tissue and blood. In another model, the presence of EBV is the consequence of immune deficiency. Arguments for immunodeficiency are the frequency of infections, which are a common cause of death, and the occurrence of EBV-associated B-cell proliferations in AITL patients.37,38 However, immune status has not yet been well characterized in AITL. Here we determined the CD4+ and CD8+ T-cell counts and correlated their absolute values to EBV status, in the tumor and in the periphery. We found a high frequency of lymphopenia (CD4+ or CD8+), but no correlation with EBV status, either in the tumor or in PBMC, and, more relevant with regards to immunodeficiency, in sera. Given the demonstration that normal TFH cells could exert immunosuppressive effects on CD4+ TH1 cells,39 it is possible that immune deficiency in AITL could be related, at least in part, to the suppressive activity of tumoral TFH. If we speculate that the detection of circulating tumor cells reflects a high tumor load, the suppressive activity of tumoral TFH could explain the intriguing close relationship that we observed between circulating EBV and circulating tumor cells (P=0.001).
We have recently shown that the number of T regulatory cells (Treg) was significantly decreased in AITL lymph nodes compared with in follicular lymphoma and reactive lymph nodes.40 Interestingly, two recent studies41,42 identified a new germinal center regulatory population, named TFR, which expresses Foxp3. Experimental data from mice suggest that TFR cells are specialized in controlling the germinal center reaction by limiting the numbers of TFH cells and inhibiting selection and outgrowth of non–antigen-specific B cells, including those carrying self-reactive receptors. The deficiency of Foxp3+ cells in AITL could explain the frequent observation of AITL rich in large B-blasts37 as confirmed in 36% cases of our series, independently of EBV infection.
In conclusion, we report here the results of the first clinical trial targeting both neoplastic T cells and the microenvironment-associated CD20+ B cells in AITL. Our clinical and biological data combined with information from the literature argue against B-blasts and/or EBV having a driving role in AITL, and point to the need for more efficient tumor cell targeting associated with action on microenvironment beyond the B cells.
Supplementary Material
Acknowledgments
the authors would like to thank Hélène Poirel and Jean-Pierre Farcet for their critical review of the manuscript, Marion Fournier and Sophie Pillardy for their skillful assistance with the statistical analyses, and Nadine Martin-Garcia, Tony Noel, Lily Wan, Jérôme Eknagi, and Jérôme Cuvillier for their technical assistance.
Funding: this work was supported by the Association pour la Recherche Thérapeutique, Génétique et Immunologique dans les Lymphomes (ARTGIL), and by the Fondation pour la Recherche Médicale (DEQ 2010/0318253).
Footnotes
The online version of this article has a Supplementary Appendix.
Authorship and Disclosures: The information provided by the authors about contributions from persons listed as authors and in acknowledgments is available with the full text of this paper at www.haematologica.org.
Financial and other disclosures provided by the authors using the ICMJE (www.icmje.org) Uniform Format for Disclosure of Competing Interests are also available at www.haematologica.org.
References
- 1.Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues IARC Press; Lyon: 2008 [Google Scholar]
- 2.Mourad N, Mounier N, Brière J, Raffoux E, Delmer A, Feller A, et al. Clinical, biologic, and pathologic features in 157 patients with angioimmunoblastic T-cell lymphoma treated within the Groupe d’Etude des Lymphomes de l’Adulte (GELA) trials. Blood. 2008;111(9):4463-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lachenal F, Berger F, Ghesquières H, Biron P, Hot A, Callet-Bauchu E, et al. Angioimmunoblastic T-cell lymphoma. Medicine. 2007;86(5):282-92 [DOI] [PubMed] [Google Scholar]
- 4.Dupuis J, Boye K, Martin N, Copie-Bergman C, Plonquet A, Fabiani B, et al. Expression of CXCL13 by neoplastic cells in angioimmunoblastic T-cell lymphoma (AITL): a new diagnostic marker providing evidence that AITL derives from follicular helper T cells. Am J Surg Pathol. 2006;30(4):490-4 [DOI] [PubMed] [Google Scholar]
- 5.de Leval L, Rickman DS, Thielen C, Reynies AD, Huang Y, Delsol G, et al. The gene expression profile of nodal peripheral T-cell lymphoma demonstrates a molecular link between angioimmunoblastic T-cell lymphoma (AITL) and follicular helper T (TFH) cells. Blood. 2007;109(11):4952-63 [DOI] [PubMed] [Google Scholar]
- 6.de Leval L, Gisselbrecht C, Gaulard P. Advances in the understanding and management of angioimmunoblastic T-cell lymphoma. Br J Haematol. 2010;148(5):673-89 [DOI] [PubMed] [Google Scholar]
- 7.Fazilleau N, Mark L, McHeyzer-Williams LJ, McHeyzer-Williams MG. Follicular helper T cells: lineage and location. Immunity. 2009;30(3):324-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vinuesa CG, Tangye SG, Moser B, Mackay CR. Follicular B helper T cells in antibody responses and autoimmunity. Nat Rev Immunol. 2005;5(11):853-65 [DOI] [PubMed] [Google Scholar]
- 9.Siegert W, Agthe A, Griesser H, Schwerdtfeger R, Brittinger G, Engelhard M, et al. Treatment of angioimmunoblastic lymphadenopathy (AILD)-type T-cell lymphoma using prednisone with or without the COP-BLAM/IMVP-16 regimen. A multicenter study. Kiel Lymphoma Study Group. Ann Intern Med. 1992;117(5):364-70 [DOI] [PubMed] [Google Scholar]
- 10.Nickelsen M, Ziepert M, Zeynalova S, Glass B, Metzner B, Leithaeuser M, et al. High-dose CHOP plus etoposide (MegaCHOEP) in T-cell lymphoma: a comparative analysis of patients treated within trials of the German High-Grade Non-Hodgkin Lymphoma Study Group (DSHNHL). Ann Oncol. 2009;20(12):1977-84 [DOI] [PubMed] [Google Scholar]
- 11.Karakas T, Bergmann L, Stutte HJ, Jäger E, Knuth A, Weidmann E, et al. Peripheral T-cell lymphomas respond well to vincristine, adriamycin, cyclophosphamide, prednisone and etoposide (VACPE) and have a similar outcome as high-grade B-cell lymphomas. Leuk Lymphoma. 1996;24(1-2):121-9 [DOI] [PubMed] [Google Scholar]
- 12.Kyriakou C, Canals C, Goldstone A, Caballero D, Metzner B, Kobbe G, et al. High-dose therapy and autologous stem-cell transplantation in angioimmunoblastic lymphoma: complete remission at transplantation is the major determinant of Outcome-Lymphoma Working Party of the European Group for Blood and Marrow Transplantation. J Clin Oncol. 2008;26(2):218-24 [DOI] [PubMed] [Google Scholar]
- 13.Reimer P, Rüdiger T, Geissinger E, Weissinger F, Nerl C, Schmitz N, et al. Autologous stem-cell transplantation as first-line therapy in peripheral T-cell lymphomas: results of a prospective multicenter study. J Clin Oncol. 2009;27(1):106-13 [DOI] [PubMed] [Google Scholar]
- 14.Zhou Y, Attygalle AD, Chuang S, Diss T, Ye H, Liu H, et al. Angioimmunoblastic T-cell lymphoma: histological progression associates with EBV and HHV6B viral load. Br J Haematol. 2007;138(1):44-53 [DOI] [PubMed] [Google Scholar]
- 15.Hsu SM, Hsu PL. Autocrine and paracrine functions of cytokines in malignant lymphomas. Biomed Pharmacother. 1994;48(10):433-44 [DOI] [PubMed] [Google Scholar]
- 16.Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM, et al. Report of an international workshop to standardize response criteria for non-Hodgkin’s lymphomas. NCI Sponsored International Working Group. J Clin Oncol. 1999;17(4):1244-52 [DOI] [PubMed] [Google Scholar]
- 17.Attygalle A, Al-Jehani R, Diss TC, Munson P, Liu H, Du M, et al. Neoplastic T cells in angioimmunoblastic T-cell lymphoma express CD10. Blood. 2002;99(2):627-33 [DOI] [PubMed] [Google Scholar]
- 18.Huang Y, Moreau A, Dupuis J, Streubel B, Petit B, Le Gouill S, et al. Peripheral T-cell lymphomas with a follicular growth pattern are derived from follicular helper T cells (TFH) and may show overlapping features with angioimmunoblastic T-cell lymphomas. Am J Surg Pathol. 2009;33(5):682-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Serke S, van Lessen A, Hummel M, Szczepek A, Huhn D, Stein H. Circulating CD4+ T lymphocytes with intracellular but no surface CD3 antigen in five of seven patients consecutively diagnosed with angioimmunoblastic T-cell lymphoma. Cytometry. 2000;42(3):180-7 [DOI] [PubMed] [Google Scholar]
- 20.Baseggio L, Berger F, Morel D, Delfau-Larue M, Goedert G, Salles G, et al. Identification of circulating CD10 positive T cells in angioimmunoblastic T-cell lymphoma. Leukemia. 2006;20(2):296-303 [DOI] [PubMed] [Google Scholar]
- 21.Bisset LR, Lung TL, Kaelin M, Ludwig E, Dubs RW. Reference values for peripheral blood lymphocyte phenotypes applicable to the healthy adult population in Switzerland. Eur J Haematol. 2004;72(3):203-12 [DOI] [PubMed] [Google Scholar]
- 22.Theodorou I, Bigorgne C, Delfau MH, Lahet C, Cochet G, Vidaud M, et al. VJ rearrangements of the TCR gamma locus in peripheral T-cell lymphomas: analysis by polymerase chain reaction and denaturing gradient gel electrophoresis. J Pathol. 1996;178(3):303-10 [DOI] [PubMed] [Google Scholar]
- 23.Delfau-Larue MH, Laroche L, Wechsler J, Lepage E, Lahet C, Asso-Bonnet M, et al. Diagnostic value of dominant T-cell clones in peripheral blood in 363 patients presenting consecutively with a clinical suspicion of cutaneous lymphoma. Blood. 2000;96(9):2987-92 [PubMed] [Google Scholar]
- 24.Brüggemann M, White H, Gaulard P, Garcia-Sanz R, Gameiro P, Oeschger S, et al. Powerful strategy for polymerase chain reaction-based clonality assessment in T-cell malignancies. Report of the BIOMED-2 Concerted Action BHM4 CT98-3936. Leukemia. 2007;21(2):215-21 [DOI] [PubMed] [Google Scholar]
- 25.Brengel-Pesce K, Morand P, Schmuck A, Bourgeat M, Buisson M, Barguès G, et al. Routine use of real-time quantitative PCR for laboratory diagnosis of Epstein-Barr virus infections. J Med Virol. 2002;66(3):360-9 [DOI] [PubMed] [Google Scholar]
- 26.Gisselbrecht C, Gaulard P, Lepage E, Coiffier B, Brière J, Haioun C, et al. Prognostic significance of T-cell phenotype in aggressive non-Hodgkin’s lymphomas. Groupe d’Etudes des Lymphomes de l’Adulte (GELA). Blood. 1998;92(1):76-82 [PubMed] [Google Scholar]
- 27.Gulley ML, Tang W. Using Epstein-Barr viral load assays to diagnose, monitor, and prevent posttransplant lymphoproliferative disorder. Clin Microbiol Rev. 2010;23(2):350-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Choi YS, Kageyama R, Eto D, Escobar TC, Johnston RJ, Monticelli L, et al. ICOS receptor instructs T follicular helper cell versus effector cell differentiation via induction of the transcriptional repressor Bcl6. Immunity. 2011;34(6):932-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kerfoot SM, Yaari G, Patel JR, Johnson KL, Gonzalez DG, Kleinstein SH, et al. Germinal center B cell and T follicular helper cell development initiates in the interfollicular zone. Immunity. 2011;34(6):947-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tripodo C, Gri G, Piccaluga PP, Frossi B, Guarnotta C, Piconese S, et al. Mast cells and Th17 cells contribute to the lymphoma-associated pro-inflammatory microenvironment of angioimmunoblastic T-cell lymphoma. Am J Pathol. 2010;177(2):792-802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li S, Gill N, Lentzsch S. Recent advances of IMiDs in cancer therapy. Curr Opin Oncol. 2010;22(6):579-85 [DOI] [PubMed] [Google Scholar]
- 32.Gallamini A, Zaja F, Patti C, Billio A, Specchia MR, Tucci A, et al. Alemtuzumab (Campath-1H) and CHOP chemotherapy as first-line treatment of peripheral T-cell lymphoma: results of a GITIL (Gruppo Italiano Terapie Innovative nei Linfomi) prospective multicenter trial. Blood. 2007;110(7):2316-23 [DOI] [PubMed] [Google Scholar]
- 33.Foss F, Shak-Shie N, Goy A, Jacobson E, Avandii R, Komrokji M, et al. Phase II study of denileukin diftitox with CHOP in PTCL. Ann Oncol. 2008;19(suppl 4):iv113-4 [Google Scholar]
- 34.d’Amore F, Radford J, Relander T, Jerkeman M, Tilly H, Osterborg A, et al. Phase II trial of zanolimumab (HuMax-CD4) in relapsed or refractory non-cutaneous peripheral T cell lymphoma. Br J Haematol. 2010;150(5):565-73 [DOI] [PubMed] [Google Scholar]
- 35.Ascierto PA, Simeone E, Sznol M, Fu Y, Melero I. Clinical experiences with anti-CD137 and anti-PD1 therapeutic antibodies. Semin Oncol. 2010;37(5):508-16 [DOI] [PubMed] [Google Scholar]
- 36.Simpson TR, Quezada SA, Allison JP. Regulation of CD4 T cell activation and effector function by inducible costimulator (ICOS). Curr Opin Immunol. 2010;22(3):326-32 [DOI] [PubMed] [Google Scholar]
- 37.Lome-Maldonado C, Canioni D, Hermine O, Delabesse E, Damotte D, Raffoux E, et al. Angio-immunoblastic T cell lymphoma (AILD-TL) rich in large B cells and associated with Epstein–Barr virus infection. A different subtype of AILD-TL?. Leukemia. 2002;16(10):2134-41 [DOI] [PubMed] [Google Scholar]
- 38.Tan BT, Warnke RA, Arber DA. The frequency of B- and T-cell gene rearrangements and epstein-barr virus in T-cell lymphomas: a comparison between angioimmunoblastic T-cell lymphoma and peripheral T-cell lymphoma, unspecified with and without associated B-cell proliferations. J Mol Diagn. 2006;8(4):466-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marinova E, Han S, Zheng B. Germinal center helper T cells are dual functional regulatory cells with suppressive activity to conventional CD4+ T cells. J Immunol. 2007;178(8):5010-7 [DOI] [PubMed] [Google Scholar]
- 40.Bruneau J, Canioni D, Renand A, Marafioti T, Paterson JC, Martin-Garcia N, et al. Regulatory T-cell depletion in angioimmunoblastic T-cell lymphoma. Am J Pathol. 2010;177(2):570-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Linterman MA, Pierson W, Lee SK, Kallies A, Kawamoto S, Rayner TF, et al. Foxp3+ follicular regulatory T cells control the germinal center response. Nat Med. 2011;17(8):975-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Amé-Thomas P, Le Priol J, Yssel H, Caron G, Pangault C, Jean R, et al. Characterization of intratumoral follicular helper T cells in follicular lymphoma: role in the survival of malignant B cells. Leukemia. 2012;26(5):1053-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.