Abstract
Acute kidney injury is a complication of open-heart surgery that carries a poor prognosis. Studies have shown that postoperative renal function deterioration in cardiovascular surgery patients increases in-hospital mortality and adversely affects long-term survival. Identifying individuals at risk for developing AKI and aggressive early intervention is extremely important to optimize outcomes. This paper provides an overview of the etiology, prognostic markers, risk factors, and prevention of AKI and treatments that may favorably affect outcomes.
Keywords: acute kidney injury, AKI, cardiovascular surgery, KDIGO staging classification, continuous venovenous hemodialysis, conventional hemodialysis

Introduction
The development of acute kidney injury (AKI) after cardiovascular surgery (CVS) has been well recognized in the past1 and is implicated as a contributing factor in the elevated mortality and poor outcomes of these patients.2-4 AKI following major CVS has a complex and multifactorial etiology. Despite advances in its management, AKI continues to contribute to the poor short- and long-term outcomes of CVS. The identification of high-risk individuals, development of protective maneuvers, and use of markers of early kidney injury are important in the early detection and proper treatment of this serious complication.
Definition of AKI after CVS
The definition of AKI after CVS differs in published studies; some describe it as a percent of increment from baseline creatinine, while others call it a doubling of the preoperative creatinine. As a rule, this syndrome is characterized by a deterioration of kidney function over a period of hours or days following surgery, with symptoms including oliguria (urine output less than 400 ml/day, which usually results in volume overload), paralleling elevations of serum blood urea nitrogen (BUN) and creatinine (Cr), and the development of serious electrolyte and acid-base disorders.
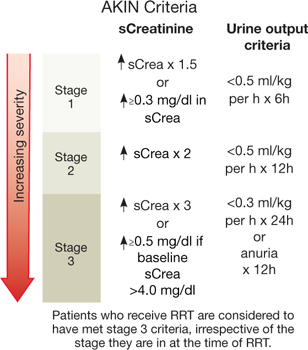
Recently, the Kidney Disease Improving Global Outcomes (KDIGO) developed a staging classification of AKI that includes three stages based on elevation of serum creatinine from baseline and urinary output (Figure 1). The hope is that this system will be universally adopted to enable future understanding of the incidence, outcomes, and effectiveness of therapeutic interventions for AKI.
Figure 1.
The KDIGO staging classification of AKI.
The proper clinical differentiation between pre-renal, intrinsic-renal, and post-renal causes of AKI remains a useful approach to this problem (Table 1). Frequently the history (vomiting, diarrhea, aggressive diuresis, exposure to nephrotoxin, cardiovascular collapse, complicated pelvic surgery, symptoms of prostatism) and physical examination (features of volume depletion, hypotension, bladder distention) provide important clues to help classify cases into pre-renal, intrinsic-renal, or post-renal categories. However, the history and physical examination are often inconclusive, and laboratory tests are necessary to better differentiate the problem.
Table 1.
Urinary findings in AKI.
| Pre-Renal | Intrinsic Renal | Post-Renal | |
| Urinalysis | Normal | Proteinuria/Casts | WBC/RBC |
| Fractional Sodium Excretion FeNa: U/P Na÷U/P Creat |
<1% | >1% | Acute <1% Cronic >1% |
| Fractional Uric Acid Excretion FeUA U/P U.A.÷U/P Creat |
<10% | >10% | Variable |
| Fractional Urea Excretion U/P BUN÷U/P Creat |
<35% | >35% | Variable |
| Urine Osmolality (mOsm/Kg) | >600 | ~300 | Variable |
Urinary tests need to be obtained before diuretics are given since, except for fractional excretion (FE) uric acid and FE urea, these tests would be equivocal due to diuretic-induced natriuresis and dissipation of medullary tonicity, thus falsely affecting fractional sodium excretion (FENa) and urine osmolality. Although BUN and serum Cr continue to be “the” markers of kidney function, their levels can be affected by several extra-renal factors. Moreover, their elevation is an indication that AKI had occurred earlier (Table 2).
Table 2.
Extra-renal causes that affect creatinine and BUN levels.
| Creatinine | BUN | ||
| Elevated | Low | Elevated | Low |
| ↑Muscle Mass | ↓Muscle Mass | Hypercatabolism | Liver Disease |
| Muscle Injury (rhabdornyolysis) | Volume Depletion | Starvation | |
| Drugs: Cefoxitin | Steroids | ||
| Cimetidine | CHF | ||
| TMP-SMZ | Hydroxyurea | ||
| Supplements: Creatine | Tissue Necrosis (gangrene) | ||
| Intraperitoneal Urine | |||
| Extravasation | |||
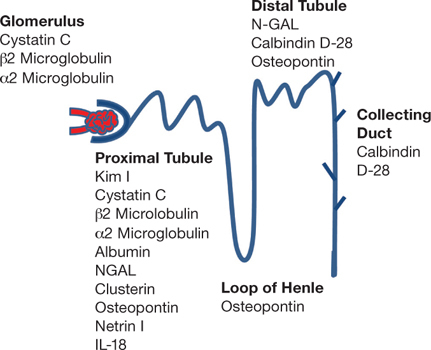
Minor elevation of serum creatinine after CVS is a poor prognostic marker.2 Lately, the use of urinary neutrophil gelatinase-associated lipocalin (NGAL) has been shown to be an early predictor of severity, duration of AKI, length of hospitalization, dialysis requirement, and mortality.5-7 Another marker of rapid and early detection of AKI is the Kim-1 dipstick, which provides important clinical information.8 Serum cystatin C appears to be better than urinary cystatin C at predicting AKI and providing prognostic information.9 However, there are factors other than glomerular filtration rate (GFR) that can affect this marker, such as inflammation, age, gender, and race.10 Together, urine IL-18, urine NGAL, and plasma NGAL were shown to significantly improve risk prediction and poor outcomes among patients undergoing cardiac surgery.11 Likewise, preoperative proteinuria appears to be an accurate predictor of AKI among adults after coronary artery bypass surgery.12
There have been several biomarkers of AKI identified according to the site of injury at the nephron (Figure 2).13 Hopefully in the future, a simple test simultaneously measuring some of these markers may become available for clinical use.
Figure 2.
Biomarkers of AKI.13
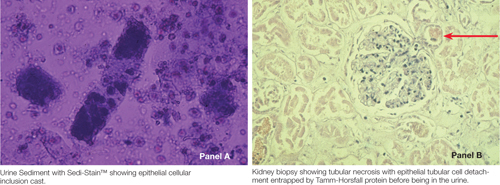
Despite advances in technology, a critical review of the urine sediment, preferably by the physician, continues to be an inexpensive, noninvasive, and dependable diagnostic tool (Figure 3).
Figure 3 A and B.
Critical review of urine sediment.14
Volume depletion (pre-renal) and obstruction (post-renal) can contribute to AKI if not recognized and properly corrected. However, AKI following CVS is mostly secondary to renal ischemia resulting from heart failure, cardiovascular collapse, interruption of renal circulation, vasopressors, and “post-pump syndrome” — with complement activation leading to mesangioproliferative changes that together result in decreased glomerular filtration. At times, AKI could result from intraoperative dye exposure or as a consequence of an atheroembolic renal insult, particularly following aortic aneurysm repair. Other contributing factors include pigment-induced tubular injury such as hemoglobinuria, a consequence of hemolysis and multiple transfusions, and myoglobinuria, which results from ischemic muscle injury (rhabdomyolysis). Of note is that both situations will show strongly positive occult blood in the urine dipstick without appreciable hematuria. Lactate dehydrogenase levels and total creatine phosphokinase would differentiate hemoglobinuria from myoglobinuria. Alternatively, gel acrylic urine electrophoresis would establish a more accurate diagnosis. Advanced age, hyperbilirubinemia, sepsis, and the use of angiotensin converting enzyme inhibitors (ACE-I), angiotensin receptor blockers (ARB), nonsteroidal anti-inflammatory drugs (NSAIDs), or radio-contrast dye immediately before surgery can predispose to AKI following CVS. However, the most predictable risk factor by far for AKI appears to be pre-existing CKD.
Pathogenesis of AKI after CVS
AKI develops under different clinical scenarios, and this complicates the understanding of the pathophysiology both clinically and experimentally. Age, race, gender, comorbid conditions, medication intake, type of surgery, duration of surgery, and certainly pre-existing CKD are all important variants to consider. The Cleveland Clinic has developed a score card to predict AKI after CVS (Table 3).15
Table 3.
Cleveland Clinic risk score for predicting AKI.15
| Risk Score for Acute Renal Failure after Cardiac Surgery | |||
| ARF Score Risk Factor | Points | Risk for Dialysis Dependent ARF Score | Risk |
| Female Gender | 1 | 0-2 | 0.4% |
| LV Ejection Fraction <35% | 1 | 3-5 | 1.8% |
| Preoperative use of IABP | 2 | 6-8 | 9.5% |
| COPD | 1 | 9-13 | 21.3% |
| Insulin-required diabetes | 1 | Based on review of 33,217 cases of open-heart surgery at Cleveland Clinic from 1993-2002. | |
| Previous Cardiac Surgery | 1 | ||
| Emergency Surgery | 2 | ||
| Valve Surgery Only | 1 | ||
| CABG + Valve Surgery | 2 | ||
| Other Cardiac Surgery | 2 | ||
| Preoperative Creatinine 1.2-2.1 mg/dL | 2 | ||
| Preoperative Creatinine >2.1 mg/dL | 5 | ||
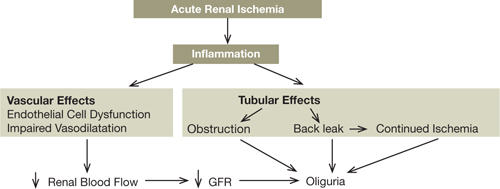
Renal ischemia results in decreased GFR by a complex mechanism stemming from reduction in renal blood flow; this leads to vasoconstriction, which in turn leads to endothelial cell swelling that can be patchy and temporal. Other findings include thickening and fibrosis of the adventitia of interlobular arteries and afferent arterioles. Vasoconstrictive humoral factors such as increased intrarenal renin activity, increased production of adenosine, thromboxanes, and endothelin have also been implicated in the genesis of AKI. Increased sensitivity to the adrenergic system could also play a role in the diminished GFR.
Disrupting the integrity of the ischemic tubules has been shown to result in back leak of the glomerular filtrate into the interstitium. The more severe the ischemic insult, the worse the back leak. This leads to interstitial edema that impairs arterial microcirculation due to external interstitial pressure buildup, resulting in diminished filtration, severe oliguria, and anuria. Tubular obstruction from desquamated proximal tubule microvilli and cellular debris (resulting from ischemic damage) mixed with Tamm-Horsfall protein casts also contribute to oliguria (Figure 4).
Figure 4.
Causes of oliguria.
Strategies to promote renal recovery remain limited; however, studies using growth factors are underway and may be promising for future use. Epidermal growth factor (EGF) is capable of stimulating proliferation of epithelial cells. In experimental models of ischemic AKI, EGF shortened recovery time. However, EGF has been implicated in the development of human cancers including renal cell carcinoma, thus limiting its use.16 Insulin-like growth factor 1 (IGF-1) initially was considered a good therapeutic choice to enhance renal recovery based on its beneficial effects in experimental models of AKI. However, human trials have failed to demonstrate a beneficial effect.17 Thyroxine had beneficial effects in ischemic and toxic animal experimental models of AKI, but they too have not been supported in human trials.18 Hepatocyte growth factor (HGF), initially identified as a mitogenic factor for hepatocytes, was subsequently found to have nonspecific cellular proliferative effects including oncogenic cells, thus limiting its use in clinical trials.19 Bone morphogenic protein 7 (BMP-7) has been shown to be essential for kidney, skeletal, and ocular development. Renal ischemia reduces BMP-7, and exogenous administration of BMP-7 in experimental renal ischemia attenuates the severity of the injury histologically and chemically.20 As such, BMP-7 remains a promising pharmacologic strategy once the mechanism for its beneficial effect is fully elucidated.
Risk Factors for AKI after CVS
In general, it is agreed that pre-existing CKD, advanced age, diabetes mellitus, congestive heart failure, generalized atherosclerosis, cardiovascular collapse, and dye exposure immediately followed by surgery are all risk factors for AKI after CVS and warrant the need for preoperative nephrology consultation.21-24 Studies have shown that race may affect mortality with AKI after CVS, indicating better survival in African American versus white patients.25 Female gender appears to have an increased incidence of AKI after open-heart surgery.26 Lower serum ferritin levels (<130 mg/dL) appear to be associated with AKI due to the inability to bind free iron (a potent oxidative stress inducer) generated during cardiopulmonary bypass-induced hemolysis.27
Prevention of Post-CVS AKI
AKI is a complex process involving apoptosis and necrosis of injured tubular cells with simultaneous repair and proliferation of the surviving tubular cells. In addition to general maneuvers designed to optimize the patient’s overall condition, such as discontinuation of potentially detrimental drugs at least 48 hours prior to surgery (including ACE-Is, ARBs, NSAIDs, metformin, diuretics, when possible) and achieving normovolemia, there have been many different attempts to prevent AKI after CVS. Observational studies using calcium channel blockers such as nifedipine,28 diltiazem,29 and nicardipine30 showed beneficial effects, but their use never qualified as accepted standards of care. A meta-analysis of 16 randomized studies showed beneficial effects using Fenoldopam, which appears to reduce the need for dialysis and mortality in critically ill patients with or at risk of AKI.31 Mannitol and dopamine failed to protect against AKI during thoracic aortic cross-clamping.32 Likewise, dopamine and furosemide were shown to lack renoprotective effects during cardiac surgery.33 The use of atrial natriuretic peptide in AKI also failed to show beneficial renoprotective effects.34 Low-dose dopamine has been found to have negative results.35 However, at times dopamine can help to initiate diuresis when a loop diuretic alone is insufficient. Although ACE-I/ARB therapy should be avoided in most cases, the use of intravenous enalaprilat36 has improved kidney performance in patients who have undergone coronary artery bypass complicated by left ventricular dysfunction. Intravenous pentoxifylline in elderly patients showed a prophylactic beneficial effect on postoperative organ function, but more studies are needed to assess its efficacy;37 moreover, this compound is not available in the United States. The use of automatic pulsatile intra-aortic balloon pumps during cardiopulmonary bypass has been associated with better kidney function.38 Off-pump coronary artery bypass may be associated with a lower incidence of postoperative AKI but did not affect the need for dialysis.39, 40 In a randomized, single-blind, controlled pilot trial of 120 adult patients undergoing cardiopulmonary bypass, remote ischemic preconditioning resulted in a 27% absolute risk reduction of AKI.41
Treatment of AKI after CVS
There are different degrees of AKI, but the term “kidney failure” implies the need for renal replacement therapy. There is no agreement in terms of timing for initiating dialysis, duration, and modality of conventional hemodialysis (HD) versus continuous venovenous hemodialysis (CVVHD).42 However, there are standards of care that mandate the initiation of dialysis in severe refractory acidemia (pH <7.2) or persistent intractable alkalemia (pH >7.6), hyponatremia (sodium <125 mEq/L), hyperkalemia (potassium >6 mEq/L), complicating oliguria, severe azotemia (BUN >100 mg/dL), rapidly progressive azotemia (BUN >20 mg/dL daily increment), as well as intractable fluid overload. The latter appears to be a poor prognostic factor frequently associated with hypoalbuminemia, a marker of inflammatory response.43 Although CVVHD may be superior to HD in the hemodynamically unstable patient and in the removal of cytokines (Interleukin-1, Interleukin-6, tumor necrosis factor-alpha), there is no evidence that one modality of dialytic therapy improves outcomes over the other; ultimately, the proper modality of dialysis becomes an individual decision based on the clinical situation.44, 45 It is possible that there is a selection bias whereby critically ill individuals are assigned to CVVHD compared to those more stable undergoing conventional HD, making it difficult to assess the advantages of one treatment modality over the other. Frequently, patients are started on CVVHD and are converted to HD once their condition is more stable to allow early mobilization, which is an important part of their treatment. Multisystem organ failure often complicates cases of CVS and worsens the prognosis by increasing mortality.46 Regrettably, acute renal failure continues to be listed as cause of death when in reality these patients are dying from combined cardiac, hepatic, pulmonary, and renal failure often complicated by bleeding and sepsis. In general, the mortality of AKI varies according to the patient population studied, ranging from 10% in those with uncomplicated AKI to 80% in those with multiple organ and system failure.47, 48
Summary
AKI continues to complicate CVS and is an important contributor of short- and long-term mortality. Elderly patients (above age 65) with underlying CKD preoperatively may never regain kidney function following AKI and may require lifetime renal replacement therapy. Identifying at-risk individuals and proactive early intervention to optimize outcomes is extremely important. If AKI develops, proper daily modification of medication dosing and avoidance of potentially nephrotoxic agents is mandatory. Likewise, restoration of hemodynamics using inotropic and vasopressor agents as well as intra-aortic balloon when indicated should help minimize the extent of AKI. Cautious volume replacement or the use of loop diuretics can be used depending on the clinical setting. Early termination of ventilator support as well as sepsis prevention (i.e., removing unnecessary lines, aggressive wound care) can favorably impact the course of AKI. Proper nutrition to promote tissue repair and to secure immunocompentence is also an important part of the overall treatment. Finally, timely initiation of HD or CVVHD to simultaneously correct fluid overload and metabolic disarray should be initiated as the clinical setting dictates.
Conflict of Interest Disclosure: All authors have completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
Funding/Support: The authors have no funding disclosures.
Contributor Information
Juan Jose Olivero, Methodist DeBakey Heart & Vascular Center, The Methodist Hospital, Houston, Texas
Juan Jorge Olivero, Methodist DeBakey Heart & Vascular Center, The Methodist Hospital, Houston, Texas
Peter Tuan Nguyen, Methodist DeBakey Heart & Vascular Center, The Methodist Hospital, Houston, Texas
Anna Kagan, Methodist DeBakey Heart & Vascular Center, The Methodist Hospital, Houston, Texas
References
- 1.Bhat JG, Gluck MC, Lowenstein J, Baldwin DS. Renal failure after open heart surgery. Ann Intern Med. 1976 Jun;84(6):677–82. doi: 10.7326/0003-4819-84-6-677. [DOI] [PubMed] [Google Scholar]
- 2.Lassnigg A, Schmidlin D, Mouhieddine M, Bachmann LM, Druml W, Bauer P, et al. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol. 2004 Jun;15(6):1597–605. doi: 10.1097/01.asn.0000130340.93930.dd. [DOI] [PubMed] [Google Scholar]
- 3.Loef BG, Epema AH, Smilde TD, Henning RH, Ebels T, Navis G, et al. Immediate postoperative renal function deterioration in cardiac surgical patients predicts in-hospital mortality and long-term survival. J Am Soc Nephrol. 2005 Jan;16(1):195–200. doi: 10.1681/ASN.2003100875. [DOI] [PubMed] [Google Scholar]
- 4.Parker RA, Himmelfarb J, Tolkoff-Rubin N, Chandran P, Wingard RL, Hakim RM. Prognosis of patients with acute renal failure requiring dialysis: results of a multicenter study. Am J Kidney Dis. 1998 Sep;32(3):432–43. doi: 10.1053/ajkd.1998.v32.pm9740160. [DOI] [PubMed] [Google Scholar]
- 5.Bennett M, Dent CL, Ma Q, Dastrala S, Grenier F, Workman R, et al. Urine NGAL predicts severity of acute kidney injury after cardiac surgery: a prospective study. Clin J Am Soc Nephrol. 2008 May;3(3):665–73. doi: 10.2215/CJN.04010907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McIlroy DR, Wagener G, Lee HT. Neutrophil gelatinase-associated lipocalin and acute kidney injury after cardiac surgery: the effect of baseline renal function on diagnostic performance. Clin J Am Soc Nephrol. 2010 Feb;5(2):211–9. doi: 10.2215/CJN.04240609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wagener G, Gubitosa G, Wang S, Borregaard N, Kim M, Lee HT. Urinary neutrophil gelatinase-lipocalin and acute kidney injury after cardiac surgery. Am J Kidney Dis. 2008 Sep;52(3):425–33. doi: 10.1053/j.ajkd.2008.05.018. [DOI] [PubMed] [Google Scholar]
- 8.Vaidya VS, Ford GM, Waikar SS, Wang Y, Clement MB, Ramirez V, et al. A rapid urine test for early detection of kidney injury. Kidney Int. 2009 Jul;76(1):108–14. doi: 10.1038/ki.2009.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang Z, Lu B, Sheng X, Jin N. Cystatin C in prediction of acute kidney injury: a systemic review and meta-analysis. Am J Kidney Dis. 2011 Sep;58(3):356–65. doi: 10.1053/j.ajkd.2011.02.389. [DOI] [PubMed] [Google Scholar]
- 10.Stevens LA, Schmid CH, Greene T, Li L, Beck GJ, Joffe MM, et al. Factors other than glomerular filtration rate affect serum cystatin C levels. Kidney Int. 2009 Mar;75(6):652–60. doi: 10.1038/ki.2008.638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parkih CR, Devarajan P, Zappitelli M, Sint K, Thiessen-Philbrook H, Li S, et al. Postoperative biomarkers predict acute kidney injury and poor outcomes after adult cardiac surgery. J Am Soc Nephrol. 2011 Sep;22(9):1737–47. doi: 10.1681/ASN.2010111163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang TM, Wu VC, Young GH, Lin YF, Shiao CC, Wu PC, et al. Pre-operative proteinuria predicts adverse renal outcomes after coronary artery bypass grafting. J Am Soc Nephrol. 2011 Jan;22(1):156–63. doi: 10.1681/ASN.2010050553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bonventre JV, Vaidya VS, Schmouder R, Feig P, Dieterie F. Next-generation biomarkers for detecting kidney toxicity. Nat Biotechnol. 2010 May;28(5):436–40. doi: 10.1038/nbt0510-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perazella MA, Coca SG. Traditional urinary biomarkers in the assessment of hospital-acquired AKI. Clin J Am Soc Nephrol. 2012 Jan;7(1):167–74. doi: 10.2215/CJN.09490911. [DOI] [PubMed] [Google Scholar]
- 15.Thakar CV, Arrigain S, Worley S, Yared JP, Paganini EP. A Clinical Score to Predict Acute Renal Failure after Cardiac Surgery. J Am Soc Nephrol. 2005 Jan;16(1):162–8. doi: 10.1681/ASN.2004040331. [DOI] [PubMed] [Google Scholar]
- 16.Arteaga CL. The epidermal growth factor receptor: from mutant oncogene in nonhuman cancers to therapeutic target in human neoplasia. J Clin Oncol. 2001 Sep 15;19(18 Suppl):32S–40S. [PubMed] [Google Scholar]
- 17.Hirschberg R, Kopple J, Lipsett P, Benjamin E, Minei J, Albertson T, et al. Multicenter clinical trial of recombinant human insulin-like growth factor 1 in patients with acute renal failure. Kidney Int. 1999 Jun;55(6):2423–32. doi: 10.1046/j.1523-1755.1999.00463.x. [DOI] [PubMed] [Google Scholar]
- 18.Acker CG, Singh AR, Flick RP, Bernardini J, Greenberg A, Johnson JP. A trial of thyroxine in acute renal failure. Kidney Int. 2000 Jan;57(1):293–8. doi: 10.1046/j.1523-1755.2000.00827.x. [DOI] [PubMed] [Google Scholar]
- 19.Vargas G, Hoeflich A, Jehle P. Hepatocyte growth factor in renal failure: promise and reality. Kidney Int. 2000 Apr;57(4):1426–26. doi: 10.1046/j.1523-1755.2000.00987.x. [DOI] [PubMed] [Google Scholar]
- 20.Vukicevic S, Basic V, Rogic D, Basic N, Shih MS, Shepard A, et al. Osteogenic protein-1 (bone morphogenic protein-7) reduces severity of kidney injury after ischemic acute renal failure in rat. J Clin Invest. 1998 Jul 1;102(1):202–14. doi: 10.1172/JCI2237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Landoni G, Biondi-Zoccai GG, Tumlin JA, Bove T, De Luca M, Calabrò MG, et al. Beneficial impact of fenoldepam in critically ill patients with or at risk for acute renal failure: a meta-analysis of randomized clinical trials. Am J Kidney Dis. 2007 Jan;49(1):56–68. doi: 10.1053/j.ajkd.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 22.Coca SG, Yusuf B, Shlipak MG, Garg AX, Parikh CR, et al. Long-term risk of mortality and other adverse outcomes after acute kidney injury: a systematic review and meta-analysis. Am J Kidney Dis. 2009 Jun;53(6):961–73. doi: 10.1053/j.ajkd.2008.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.LeMaire S, Miller CC 3rd, Conklin LD, Schmittling ZC, Köksoy C, Coselli JS. A new predictive model for adverse outcomes after elective thoracoabdominal aortic aneurysm repair. Ann Thorac Surg. 2001 Apr;71(4):1233–8. doi: 10.1016/s0003-4975(00)02678-3. [DOI] [PubMed] [Google Scholar]
- 24.Anderson RJ, O’brien M, MaWhinney S, VillaNueva CB, Moritz TE, Sethi GK, et al. Renal failure predisposes patients to adverse outcomes after coronary artery bypass surgery. VA Cooperative Study#5. Kidney Int. 1999 Mar;55(3):1057–62. doi: 10.1046/j.1523-1755.1999.0550031057.x. [DOI] [PubMed] [Google Scholar]
- 25.Waikar SS, Curhan GC, Ayanian JZ, Chertow GM. Race and mortality after acute renal failure. J Am Soc Nephrol. 2007 Oct;18(10):2740–48. doi: 10.1681/ASN.2006091060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thakar CV, Liangos O, Yared JP, Nelson D, Piedmonte MR, Hariachar S, et al. ARF after open heart surgery: influence of gender and race. Am J Kidney Dis. 2003 Apr;41(4):742–51. doi: 10.1016/s0272-6386(03)00021-0. [DOI] [PubMed] [Google Scholar]
- 27.Davis CL, Kausz AT, Zager RA, Kharasch ED, Cochran RP. Acute renal failure after cardiopulmonary bypass is related to decreased serum ferritin levels. J Am Soc Nephrol. 1999 Nov;10(11):2396–402. doi: 10.1681/ASN.V10112396. [DOI] [PubMed] [Google Scholar]
- 28.Antonucci F, Calo L, Rizzolo M, Cantaro S, Bertolissi M, Travaglini, et al. Nifedipine can preserve renal function in patients undergoing aortic surgery with infrarenal crossclamping. Nephron. 1996;74(4):668–73. doi: 10.1159/000189472. [DOI] [PubMed] [Google Scholar]
- 29.Bergman AS, Odar-Cederlof, Westman L. Renal and hemodynamic effects of diltiazem after elective major vascular surgery–a potential renoprotective agent? Ren Fail. 1995 Mar;17(2):155–63. doi: 10.3109/08860229509026252. [DOI] [PubMed] [Google Scholar]
- 30.Colson P, Ribstein J, Séguin JR, Marty-Ane C, Roguefeuil B. Mechanisms of renal hemodynamic impairment during infrarenal aortic cross-clamping. Anesth Analg. 1992 Jul;75(1):18–23. doi: 10.1213/00000539-199207000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Tumlin JA, Finkel KW, Murray PT, Samuels J, Cotsonis G, Shaw AD. Fenoldepam mesylate in early acute tubular necrosis: a randomized double-blind, placebo-controlled clinical trial. Am J Kidney Dis. 2005 Jul;46(1):26–34. doi: 10.1053/j.ajkd.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 32.Pass LJ, Eberhart RC, Brown JC, Rohn GN, Estrera AS. The effect of mannitol and dopamine on the renal response to thoracic aortic cross-clamping. J Thorac Cardiovasc Surg. 1998 Apr;95(4):608–12. [PubMed] [Google Scholar]
- 33.Lassnigg A, Donner E, Grubhofer G, Presterl E, Druml W, Hiesmayr M. Lack of renoprotective effects of dopamine and furosemide during cardiac surgery. J Am Soc Nephrol. 2000 Jan;11(1):97–104. doi: 10.1681/ASN.V11197. [DOI] [PubMed] [Google Scholar]
- 34.Rahman SN, Kim GE, Mathen AS, Goldberg CA, Allgren RW, Schrier RW, et al. Effects of atrial natruretic peptide in clinical acute renal failure. Kidney Int. 1994 Jun;45(6):1731–8. doi: 10.1038/ki.1994.225. [DOI] [PubMed] [Google Scholar]
- 35.Lauschke A, Teichgräber UK, Frei U, Eckardt KU. ‘Low dose’ dopamine worsens renal perfusion in patients with acute renal failure. Kidney Int. 2006 May;69(9):1669–74. doi: 10.1038/sj.ki.5000310. [DOI] [PubMed] [Google Scholar]
- 36.Wagner F, Yeter R, Bisson S, Siniawski H, Hetzer R. Beneficial hemodynamic and renal effects of intravenous enalaprilat following coronary artery bypass surgery complicated by left ventricular dysfunction. Crit Care Med. 2003 May;31(5):1421–8. doi: 10.1097/01.CCM.0000063050.66813.39. [DOI] [PubMed] [Google Scholar]
- 37.Boldt J, Brosch C, Piper SN, Suttner S, Lehmann A, Weling C. Influence of prophylactic use of pentoxifylline on postoperative organ function in elderly cardiac surgery patients. Crit Care Med. 2001 May;29(5):952–8. doi: 10.1097/00003246-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 38.Onorati F, Presta P, Fuiano C, Mastroroberto P, Comi N, Pezzo F, et al. A randomized trial of pulsatile perfusion using an intra-aortic balloon pump versus nonpulsatile perfusion on short-term changes in kidney function during cardiopulmonary bypass during myocardial reperfusion. Am J Kidney Dis. 2007 Aug;50(2):229–38. doi: 10.1053/j.ajkd.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 39.Nigwekar SU, Kandula P, Hix JK, Thakar CV. Off-pump coronary artery bypass surgery and acute kidney injury: a meta-analysis of randomized and observational studies. Am J Kidney Dis. 2009 Sep;54(3):414–23. doi: 10.1053/j.ajkd.2009.01.267. [DOI] [PubMed] [Google Scholar]
- 40.Seabra VF, Alobaidi S, Balk EM, Poon AH, Jaber BL. Off-pump coronary artery bypass surgery and acute kidney injury: a meta-analysis of randomized controlled trials. Clin J Am Soc Nephrol. 2010 Oct;5(10):1734–44. doi: 10.2215/CJN.02800310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zimmerman RF, Ezeanuna PU, Kane JC, Cleland CD, Kempananjappa TJ, Lucas FL, et al. Ischemic preconditioning at a remote site prevents acute kidney injury in patients following cardiac surgery. Kidney Int. 2011 Oct;80(8):861–7. doi: 10.1038/ki.2011.156. [DOI] [PubMed] [Google Scholar]
- 42.Gibney N, Hoste E, Burdmann EA, Bunchman T, Kher V, Viswanathan R, et al. Timing of initiation and discontinuation of renal replacement therapy in AKI: unanswered key questions. Clin J Am Soc Nephrol. 2008 May;3(3):876–80. doi: 10.2215/CJN.04871107. [DOI] [PubMed] [Google Scholar]
- 43.Bouchard J, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, et al. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 2009 Aug;76(4):422–7. doi: 10.1038/ki.2009.159. [DOI] [PubMed] [Google Scholar]
- 44.Davenport A, Bouman C, Kirpalani A, Skippen P, Tolwani A, Mehta RL, et al. Delivery of renal replacement therapy in acute kidney injury: what are the key issues? Clin J Am Soc Nephrol. 2008 May;3(3):869–75. doi: 10.2215/CJN.04821107. [DOI] [PubMed] [Google Scholar]
- 45.DuBose TD, Jr, Warnock DG, Mehta RL, Bonventre JV, Hammerman MR, Molitoris BA, et al. Acute renal failure in the 21st century: recommendation for management and outcome assessment. Am J Kidney Dis. 1997 May;29(5):793–9. doi: 10.1016/s0272-6386(97)90136-0. [DOI] [PubMed] [Google Scholar]
- 46.Bartlett RH. Continuous renal replacement therapy in multiple organ failure. Am J Kidney Dis. 1996 Nov;28(5 Suppl 3):S97–99. [Google Scholar]
- 47.Cosentino F, Chaff C, Piedmonte M. Risk factors influencing survival in ICU acute renal failure. Nephrol Dial Transplant. 1994;(9 Suppl 4):179–82. [PubMed] [Google Scholar]
- 48.Liaño F, Junco E, Pascual J, Madero R, Verde E. The spectrum of acute renal failure in the intensive care unit compared with that seen in other settings. The Madrid Acute Renal Failure Study Group. Kidney Int Suppl. 1998 May;66:S16–24. [PubMed] [Google Scholar]


