Abstract
The combination of deep brain stimulation (DBS) and functional MRI (fMRI) is a powerful means of tracing brain circuitry and testing the modulatory effects of electrical stimulation on a neuronal network in vivo. The goal of this study was to trace DBS-induced global neuronal network activation in a large animal model by monitoring the blood oxygenation level-dependent (BOLD) response on fMRI. We conducted DBS in normal anesthetized pigs, targeting the subthalamic nucleus (STN) (n=7) and the entopeduncular nucleus (EN), the non-primate analogue of the primate globus pallidus interna (n=4). Using a normalized functional activation map for group analysis and the application of general linear modeling across subjects, we found that both STN and EN DBS significantly increased BOLD activation in the ipsilateral sensorimotor network (FDR < 0.001). In addition, we found differential, target-specific, non-motor network effects. In each group the activated brain areas showed a distinctive correlation pattern forming a group of network connections. Results suggest that the scope of DBS extends beyond an ablation-like effect and that it may have modulatory effects not only on circuits that facilitate motor function but also on those involved in higher cognitive and emotional processing. Taken together, our results show that the swine model for DBS fMRI, which conforms to human implanted DBS electrode configurations and human neuroanatomy, may be a useful platform for translational studies investigating the global neuromodulatory effects of DBS.
Keywords: Deep brain stimulation (DBS), Parkinson’s disease (PD), subthalamic nucleus (STN), globus pallidus interna (GPi), entopeduncular nucleus (EN), pedunculopontine nucleus (PPN), functional magnetic resonance imaging (fMRI), swine model, neural circuitry
Introduction
Deep brain stimulation (DBS) is a well-established restorative therapy for movement disorders, such as those associated with Parkinson’s disease (PD) (Benabid, 2003; Deuschl et al., 2006), essential tremor (Benabid et al., 1993), and dystonia (Greene, 2005). The nucleus ventralis intermedius of the thalamus, the globus pallidus interna (GPi), and the subthalamic nucleus (STN) are the most frequently used DBS targets for movement disorders (Benabid et al., 1998; Krack et al., 1999).
The two most common targets for the motor symptoms of advanced PD are GPi and STN (Anderson et al., 2005; DBS-study-group, 2001). Both have been found effective for treating tremor, rigidity, and bradykinesia (Anderson et al., 2005; Benabid et al., 1994; Burchiel et al., 1999; Ghika et al., 1998; Okun and Foote, 2005), but with some notable differences. For example, GPi DBS has been found more effective than STN for treating dyskinesias (Anderson et al., 2005; Wu et al., 2001). Conversely, STN DBS appears more effective in treating severe tremor (Krack et al., 1998), akinesia (Brown et al., 1999), and for reducing dependence on dopaminergic drugs such as L-Dopa and the dyskinesias associated with its use (Krack et al., 1999; Limousin et al., 1998). Finally, adverse cognitive and behavioral effects are more frequently associated with STN than with GPi (Anderson et al., 2005; DBS-study-group, 2001; Okun and Foote, 2005).
The cognitive and psychiatric complications induced by DBS may be partly attributed to current spread into structures and substructures adjacent to the implantation site, causing unintended neural network activation(Alexander et al., 1986; Chopra et al., 2011). Both STN and GPi are key relay areas in the basal ganglia-thalamocortical circuitries, and both project to sensorimotor, limbic, and associative areas in the cortex (McIntyre and Hahn, 2010). In accordance with the classic basal ganglia model, electrical stimulation of STN and GPi should facilitate projections to these cortical areas (Kringelbach et al., 2007).
To investigate the global effects of STN and GPi DBS stimulation in vivo, previous studies have used fMRI or PET in conjunction with DBS stimulation in human patients who have had DBS surgery for PD. These investigations have been single-case reports or within-subject studies of motor and behavioral changes with and without DBS stimulator activation. In general, these fMRI and PET studies have found activation or, in some cases, deactivation of ipsilateral primary sensorimotor cortex, premotor cortex, the supplementary motor area, dorsolateral prefrontal cortex, the basal ganglia, the brainstem and the contralateral cerebellum (Haslinger et al., 2003; Jech et al., 2001; Phillips et al., 2006; Stefurak et al., 2003).
To better characterize the neural network and circuitry fed by STN and EN/GPi in the normal brain and to better understand the global effects of DBS, we combined DBS with fMRI studies in a large animal model, focusing on cortical as well as subcortical pathways activated by electrical stimulation. The combination of functional imaging with DBS is a powerful technique for tracing the brain’s circuitry (Grafton and DeLong, 1997). For example, selective and reversible changes can be made in stimulation parameters during a single fMRI scanning session, which allows one to vary, and thus test, the modulatory potential of electricity on a subcortical-cortical pathway (Ceballos-Baumann et al., 1999; Ceballos-Baumann et al., 2001; Davis et al., 2000; Deiber et al., 1993; Haslinger et al., 2003; Jech et al., 2001; Rezai et al., 1999; Stefurak et al., 2003).
To investigate the global neuronal network effect of DBS we compared the blood oxygenation level-dependent (BOLD) response evoked by STN stimulation in anesthetized normal pigs with that evoked by stimulation of the entopeduncular nucleus (EN), which is the non-primate analog of the human GPi segment. Prior to the initiation of the experiment, we targeted the substantia nigra (SN) in a single pig for proof-of-principle.
The swine model was chosen because the large brain volume (pig brain:~160g) is comparable to that of the non-human primate (rhesus monkey brain:~100g) (Hardman et al., 2002; Shon et al., 2010), and with a gyrencephalic cortex, more closely represents human brain anatomy than do the brains of small animal models, such as rodents (Pour-El, 2006; Shon et al., 2010; Van Gompel et al., 2011; Wakeman et al., 2006). We took a novel approach using a high-resolution 3-dimensional pig brain atlas (Saikali et al., 2010), which allowed us to normalize the functional activation map and to apply general linear modeling in each subject group. This method has the advantage of permitting regression analysis for every voxel across subjects, resulting in a high statistical power that corresponds to the predictor variables (e.g., electrical stimulation parameters and target location).
Materials and Methods
Animals and DBS Electrode Implantation
All study procedures were performed in accordance with the National Institutes of Health Guidelines for Animal Research (Guide for the Care and Use of Laboratory Animals) and approved by Mayo Clinic Institutional Animal Care and Use Committee. The subject groups consisted of 7 pigs with STN as the stimulation target and 4 pigs with EN/GPi as the stimulation target. Prior to the STN-EN/GPi comparison study, we targeted the SN in a single pig for proof of principle. The domestic male pigs weighed 30±5 kg at the time of the fMRI experiment. They were fed once a day, had ad libitum access to water, and were housed individually, but with visual access to each other, in a controlled environment with humidity at 45% and temperature at 21°C. Each subject was initially sedated with Telazol (5 mg/kg i.m.) and Xylazine (2 mg/kg i.m.), followed by intubation. Sedation was maintained with a solution of 1.5–3% isoflurane during surgery and 1.5–2% isoflurane during the fMRI experiment. The vital signs (heart rate:~120bpm, respiration rate:12/min, and temperature:36–37°C) were continuously monitored throughout the procedure.
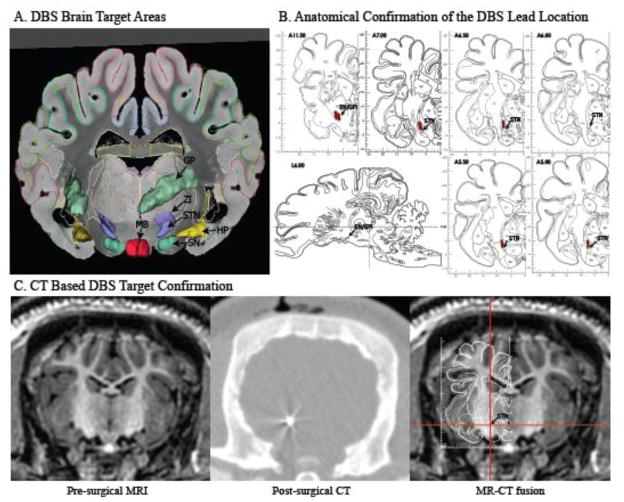
An MR image-guided stereotactic targeting system for large animals, developed by our group, was used for DBS electrode targeting and has been previously described (Figure S1) (Shon et al., 2010). The preoperative anatomical 3D MP-RAGE image obtained for targeting was generated from a General Electric (GE) Signa HDx 3.0 Tesla (T) whole-body MRI scanner with the following parameters: repetition time (TR), 11 ms; echo time (TE), 5.16 ms; inversion time (TI), 1000 ms; flip angle (FA), 8°; slice thickness (ST), 1 mm; field of view (FOV), 24 × 24 mm; matrix, 256 × 256; slice number, 128; frequency direction (FD), A/P; Fast SPGR; ZIPx2; ZIP 512; number of excitations (NEX), 3; acquisition time (TA), 38.20 min. A custom 3.0 T radiofrequency (RF) coil, developed in our institution’s MRI RF coil laboratory specifically for this research, was used for all imaging. This fabricated RF coil is a four channel, receive-only, phased array coil with four overlapping octagon-shaped elements with each element measuring 7.3 centimeters in diameter. The coil array is small enough to fit just above the pig’s skull inside the stereotactic head frame, a set-up that provides excellent signal-to-noise ratio. MR image-based targeting using a pig brain atlas as a reference (Felix et al., 1999; Saikali et al., 2010) was performed using COMPASS navigational software (modified for large animals) to determine the Leksell coordinates for targets STN, EN/GPi or SN and to determine a safe trajectory for delivery of the electrode (Figure S1B). A DBS electrode (Model 3389, Medtronic Inc.) was introduced using an Alpha-Omega computer-controlled microdrive (Alpha Omega Co.). The DBS lead was secured on the skull using an anchoring system of burr hole ring and cap before being transferred from the surgical suite. Additionally, the animals were firmly secured on a carrying plate to minimize motion while moving to the MR/CT scanner. The location of the electrode was confirmed through a post-surgical CT (Dual source Somatom Definition, Siemens AG) scan (Image resolution 0.6 × 0.6 × 0.6 mm) which was co-registered using a 6-parameter rigid-body transformation with the pre-MRI MP-RAGE scan (FSL, FM-RIB Analysis group) (Cho et al., 2010; Smith et al., 2004; Starr et al., 2002) (Figure 1C).
Figure 1.
DBS electrode target localization in the pig brain. A) 3D rendering of target structures (left) and atlas-based location of the STN, GP and SN (Saikali et al., 2010). B) Antatomical confirmation of the DBS lead location was marked in the pig brain atlas (Felix et al., 1999). C) Pre-surgical MRI scan (left), post-surgical CT scan (middle), and MR-CT fusion with atlas overlay demonstrating the location of the electrode tip in the STN (right).
Abbreviations CT, Computed tomography; DBS, Deep brain stimulation, EN, Entopeduncular nucleus; GP, Globus pallidus; GPi. Globus pallidus interna; HP, Hippocampus; MB, Mammillary body; MRI Magnetic resonance imaging; STN, Subthalamic nucleus; ZI, Zona incerta
fMRI and DBS
Following electrode implantation, subjects were transferred to the MRI scanner. For anatomical registration, 2D T2-weighted fast spin-echo (FSE) images were obtained with the following parameters: TR, 3000 ms; TE, 110 ms; FA, 90°; BW, 8.33 kHz; echo train length, 10; ST, 2.4 mm; FOV, 15 × 15 mm; matrix, 320 × 320; slice number, 32; NEX, 1; TA, 5.07 min. fMRI was performed using a gradient echo (GRE) echo-planar imaging (EPI) pulse sequence with the following parameters: TR, 3000 ms; TE, 34.1 ms; FA, 90°; BW, 62.5 kHz; ST, 2.4 mm; FOV, 15 ×15 mm; matrix, 64 × 64; slice number, 32; FD, R/L; TA, 12.45 min. GRE EPI integrated spatial spectral pulse was used for fat suppression. To eliminate any movement during the fMRI experiment, the pigs were administered a 2mg bolus of pancuronium bromide, and maintained with 3mg/hr throughout the remainder of the experiment. To detect a putative BOLD signal response within the brain after electrical stimulation of either STN or EN/GPi, the following general stimulation block design was applied. After scanning 15s (5 volumes) of discarded acquisitions to allow for scanner equilibrium, 120 s of initial scanning at rest (40 volumes of fMRI) were performed followed by five stimulus/rest blocks. These blocks each consisted of 6 s electrical stimulus (two volumes of fMRI) followed by 120 s rest (40 volumes of fMRI). This provided for a total scanning time of 12 min 45 sec (255 volumes of fMRI). For STN and EN/GPi, the subjects received stimulation parameters of biphasic 1V pulses at 130Hz and pulse widths of 500μsec (A-M system isolated pulse stimulator Model 12100) using 0–1 contact of the Medtronic 3389 lead. To test the effects of stimulation intensity, 4 pigs from the STN DBS group and 3 pigs from the GPi DBS group were randomly selected to receive biphasic 2V pulses at 130Hz and pulse widths of 500μsec followed by a ~10min rest after the first fMRI scan. For the single subject in which SN was the target, stimulation parameters of biphasic 300μA pulses at 60Hz, and pulse widths of 2 ms were applied.
Anatomical Confirmation of the DBS Lead Location
Upon completion of the experimental fMRI DBS procedure, subjects were deeply anesthetized with intravenous sodium pentobarbital (100mg/kg) and euthanized. The brain was extracted and kept in 10% formalin for two weeks. The brain was then sectioned at 250μm in the coronal plane by a vibratome (VT 1000s, Leica) to confirm the DBS lead location by visual inspection of the DBS lead track. The electrode position was marked in the pig brain atlas as shown in Figure 1B.
Data Processing and Analysis
The fMRI data were converted into BrainVoyager data format. A standard sequence of pre-processing steps, including 3D motion correction and temporal filtering (Gaussian filter; FWHM 3 data points), was implemented in the BrainVoyager QX software and applied to each data set. Functional activation was analyzed by correlating the observed signal intensity changes in each voxel with the given stimulus protocol. Based on the results of this procedure, an appropriate activation map was generated for each subject.
To account for hemodynamic delay, the stimulus representing the block design was convolved with a double-gamma hemodynamic response function (onset 0 s, time to response peak 5 s, time to undershoot peak 15 s). To correct for multiple comparisons and exclude false positive voxels, we considered only voxels with a significance level less than the False Discovery Rate (FDR) < 0.001 to represent sites of activation.
To visualize the group activation pattern during each of the five stimulation blocks, each fMRI dataset was normalized to a 3D ultra-high resolution pig brain MRI atlas (Saikali et al., 2010). Using the 2D FSE anatomical image and the first volume of the fMRI data, a manual skull and muscle stripping was performed on both 2-dimensional image leaving only the brain by Analyzer 10.0 software (Mayo Clinic) and then the image was used for a full affine (12 parameters) normalization to the 3D atlas by BrainVoyager QX.
Event-related BOLD responses were calculated by measuring the signal intensities that began 10 volumes before the stimulus onset and continued for 25 volumes after the stimulus ended. The averaged signal intensity within the appropriate area in the first 10 volumes was set to 100% signal intensity as a baseline, and post-stimulus signal variation was calculated relative to it. These datasets were then further analyzed using linear regression analysis with the general linear model (GLM) and multi-subject analysis, as implemented in BrainVoyager QX software.
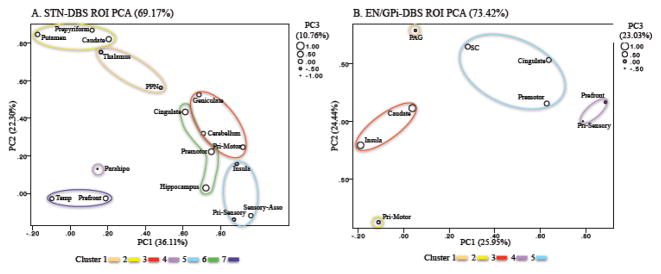
To investigate the pattern of relationships among the activated brain areas, regions of interest (ROI) were selected based on clusters of functional activation identified from the normalized averaged group data for each target. Pearson correlation was performed to compare the maximum signal intensity of each ROI (See supplementary data Figure S3). Factor analysis based on principal component analysis (PCA) with varimax rotation of the correlation matrix was then performed to identify patterns among the ROIs, and was followed by k-means clustering of the three-dimensional Eigen plot (Dunteman, 1989; Mardia et al., 1979). Agglomerative hierarchical clustering was also used to verify the number of clusters by the elbow rule (Anderberg, 1973) (Statistical Package for the Social Sciences, version 20, IBM).
Results
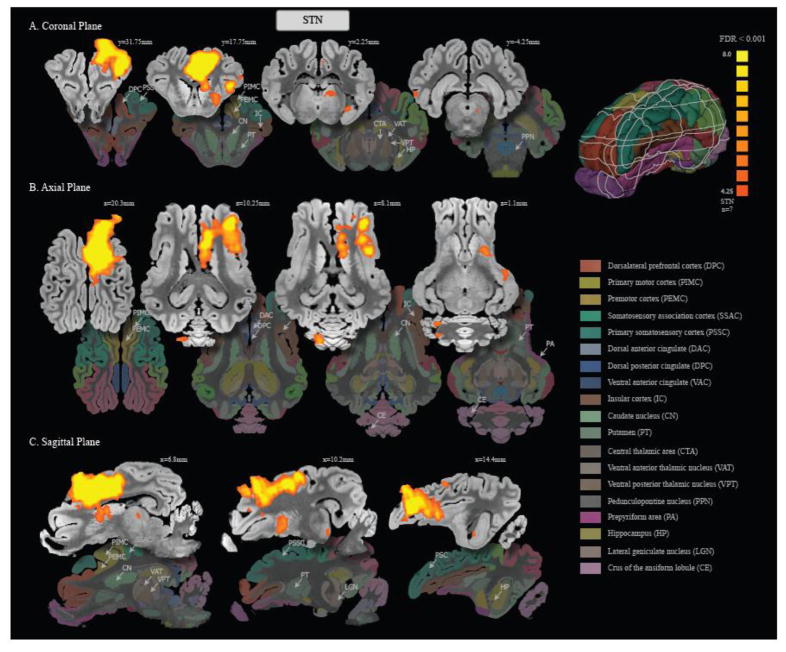
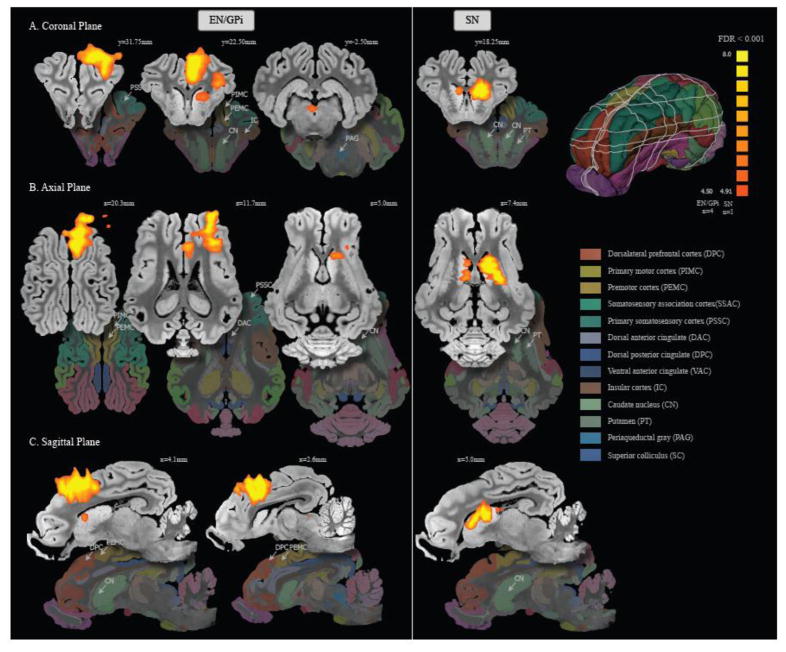
Stimulation of both STN (Table 1 and Figure 2) and EN/GPi DBS (Table 1 and Figure 3 ) significantly increased the BOLD signal in the ipsilateral sensorimotor network, including the premotor cortex, primary motor cortex, and primary somatosensory cortex (FDR < 0.001). Group comparisons showed that there were large areas of overlap in the regions activated by these two targets. Additional areas of activation for both target sites were the ipsilateral dorsolateral prefrontal cortex, caudate nucleus, anterior cingulate cortex, and the anterior part of the insular cortex. The largest and most significant clusters of activation were detected in the sensorimotor cortex for both STN and EN/GPi DBS (Table 1).
Table 1.
Areas of Significant Brain Activation
| Location | Size (mm3) | Coordinates (x, y, z) | Max z-Score | Possible circuits involved | |
|---|---|---|---|---|---|
| STN | Primary motor cortex (I) | 859 | 5.7, 18.00, 18.9 | 18.73 | BGTC loop (Indirect pathway), Antidormic STN-Cortex, DS of CST in IC |
| Premotor cortex (I) | 1836 | 2.9, 18.00, 18.1 | 20.40 | BGTC loop (Indirect pathway), Antidormic STN-Cortex, DS of CST in IC | |
| Primary somatosensory cortex (I) | 915 | 7.6, 30.25, 18.0 | 12.61 | BGTC loop (Indirect pathway), Antidormic STN-Cortex, DS of CST in IC | |
| Somatosensory association cortex (I) | 227 | 7.7, 14.50, 18.9 | 12.70 | BGTC loop (Indirect pathway), Antidormic STN-Cortex, DS of CST in IC | |
| Dorsalateral prefrontal cortex (I) | 197 | 4.3, 27.50, 18.0 | 13.20 | Associative territory of STN | |
| Anterior Cingulate cortex (I) | 634 | 2.9, 16.25, 14.9 | 17.02 | Limbic territory of STN | |
| Insular cortex (I) | 916 | 15.3, 30.25, 10.7 | 14.10 | Limbic territory of STN | |
| Caudate nucleus (I) | 142 | 4.5, 16.75, 7.5 | 7.01 | STN-SNc, DS of SN, DS of NSF, PPN-SNc | |
| Putamen (I) | 152 | 8.8, 20.75, −0.7 | 6.04 | STN-SNc DS of SN, DS of NSF, PPN-SNc | |
| Thalamus (I) | 12 | 5.4, 1.75, 5.4 | 4.83 | BGTC loop (Indirect pathway), Antidormic STN-CmPf, DS of thalamus | |
| Pedunculopontine nucleus (I) | 1 | 4.8, −4.25, −2.3 | 4.53 | STN-PPN | |
| Prepyriform area (I) | 51 | 18.4, 5.75, 0.2 | 5.07 | Limbic territory of STN | |
| Hippocampus (I) | 9 | 13.3, 1.75, −2.8 | 4.86 | Limbic territory of STN | |
| Lateral geniculate nucleus (I) | 25 | 10.9, −225, −1.4 | 5.56 | Associative territory of STN, DS of oculomotor fiber | |
| Cerebellum (C) | 183 | −5.9, −23.00, 8.3 | 6.81 | Motor Cortex-Cerebellum connection, DS of Cerebello-thalamic fibers | |
| Temporal cortex (C) | 13 | −24.2, −4.25, 5.0 | 4.78 | N/A | |
| Parahippocampal gyrus (C) | 29 | −21.0, 4.50, −3.7 | 5.20 | N/A | |
| EN/GPi | Primary motor corteex (I) | 188 | 9.4, 26.5, 17.4 | 9.56 | BGTC loop (Indirect pathway), DS of CST in IC |
| Premotor cortex (I) | 759 | 4.3, 25.50, 21.0 | 11.04 | BGTC loop (Indirect pathway), DS of CST in IC | |
| Primary somatosensory cortex (I) | 1175 | 12.7, 35.25, 14.5 | 11.34 | BGTC loop (Indirect pathway), DS of CST in IC | |
| Dorsalateral prefrontal cortex (I) | 220 | 5.7, 29.25, 18.1 | 10.11 | Associative territory of EN/GPi | |
| Anterior Cingulate cortex (I) | 158 | 2.7, 19.50, 14.8 | 10.20 | Limbic territory of EN/GPi | |
| Insular cortex (I) | 356 | 14.0, 25.50, 10.1 | 10.47 | Limbic territory of EN/GPi | |
| Caudate (I) | 62 | 7.0, 24.00, 4.3 | 621 | Antidonmic EN/GPi-Caudate | |
| Periaqueductal gray (C) | 32 | −1.0, −2.00, 0.9 | 5.72 | N/A | |
| Superior colluculus (I) | 1 | 2.8, −3.75, 3.4 | 4.64 | DS of optic tract |
Coordinates (mm): x = mediolateral, y = rostrocaudal, and z = dorsoventral. Abbreviations: BGTC, Basal ganglia-thalamocortical; C, Contralateral; CmPf, Centromedian and parafascicular nuclei of the thalamus; CST, Corticospinal tract; DS, Direct stimulation through electric spread; EN, Entopeduncular nucleus; GPi, Globus pellidus interna; I, Ipsilateral; IC, Internal capsule; NSF, Nigrostriatal fiber; PPN, Pedunculopontine nucleus; SNc, Substantia Nigra pars compacta; STN, Subthalamic nucleus
Figure 2.
Areas of activation with STN stimulation at 1V 130Hz 0.5ms, normalized to a 3D pig brain template(Saikali et al., 2010). Significant activation (FDR < 0.001) was observed in the ipsilateral premotor cortex, primary motor cortex, primary somatosensory cortex, dorsolateral prefrontal cortex, caudate nucleus, putamen, anterior cingulate cortex, insular cortex, thalamus (central, ventral anterior and ventral posterior areas), prepyriform area, hippocampus, lateral geniculate nucleus, pedunculopontine nucleus, and the contralateral cerebellum.
Figure 3.
Areas of activation with EN/GPi stimulation at 1V 130Hz 0.5ms (left) and SN stimulation at 300mA 60Hz 2ms (right), normalized to a 3D pig brain template (left)(Saikali et al., 2010). With EN/GPi stimulation, significant activation (FDR < 0.001) was observed in the ipsilateral premotor cortex, primary motor cortex, primary somatosensory cortex, dorsolateral prefrontal cortex, caudate nucleus, anterior cingulate cortex, insular cortex, and contralateral periaqueductal gray. SN stimulation activated ipsilateral and contralateral caudate nucleus and ipsilateral putamen.
There were also target-specific results. STN DBS was uniquely associated with activation in the ipsilateral thalamus (ventral anterior/posterior areas), the somatosensory association cortex, prepyriform area, hippocampus, lateral geniculate nuclei, pedunculopontine nucleus (PPN), the contralateral temporal cortex, parahippocampal gyrus, and cerebellum (Table 1). EN/GPi DBS was uniquely associated with periaqueductal gray and superior colliculus activation (Table 1). In the single subject experiment testing SN stimulation, DBS activated bilateral caudate nuclei, including activation of the putamen, with a stronger ipsilateral than contralateral activation. There were no regions of negative BOLD signal induced by DBS in any group. The time course representing percent change in the BOLD signal versus time demonstrated clear increases that were time-locked with each of the five blocks of stimulation pulses in each ROI (Figure S2).
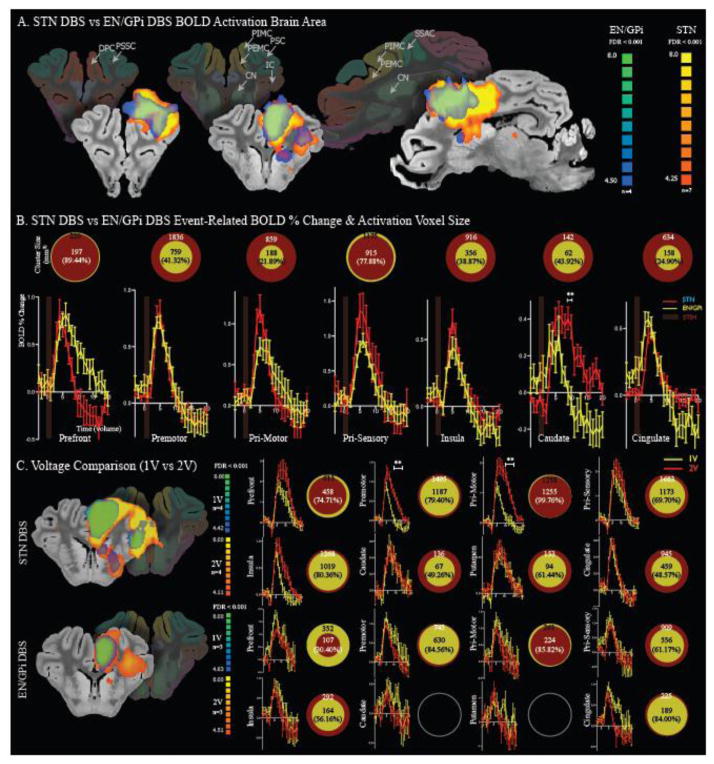
Figure 4, A and B, shows a comparison between ROI cluster sizes and the event-related time course of percent change in the BOLD signal of STN versus EN/GPi stimulation. STN stimulation resulted in larger cluster size, >30% increase than EN/GPi, which included premotor cortex, primary motor cortex, insular cortex, caudate nucleus and anterior cingulate cortex. STN stimulation also induced higher BOLD% change in the caudate than did EN/GPi (p<0.001, t-test).
Figure 4.
A) The fMRI activation map of STN (red scale) and EN/GPi (blue scale) DBS fMRI activation map. Areas of overlap include dorsolateral prefrontal cortex, premotor cortex, primary motor cortex, primary somatosensory cortex, insula cortex, caudate and anterior cingulate cortex. B) Region of interest cluster sizes (top) and event-related time course of percent change in BOLD signal from baseline (bottom) with STN stimulation (red) versus EN/GPi stimulation (yellow). STN stimulation resulted in greater area of activation of premotor cortex, primary motor cortex, insular cortex, caudate and anterior cingulate cortex than EN/GPi stimuation. STN also showed higher BOLD activation in the Caudate (p<0.001, t-test). C) Voltage comparison showing fMRI activation map of 1V (blue scale) and 2V (red scale) of each group. Region of interest cluster sizes and event-related time course of percent change in BOLD signal have been compared (1V-yellow vs 2V-red).
Abbreviations: BOLD, blood oxygenation level-dependent; Caudate, Caudate nucleus; Cingulate, Anterior cingulate cortex; CN, Caudate nucleus; DBS, Deep brain stimulation; DPC, Dorsalateral prefrontal cortex; EN, Entopeduncular nucleus; FDR, False discovery rate; GPi, Globus pallidus interna; IC, Insular cortex; Insula, Insular cortex; PIMC, Primary motor cortex; PEMC, Premotor cortex; Premotor, Premotor cortex; Prefront, Dorsalateral prefrontal cortex; Pri-Motor, Primary motor cortex; Pri-sensory, Primary Somatosensory cortex PSSC, Primary Somatosensory cortex; SSAC, Somatosensory association cortex; STIM, DBS stimulation; STN, Subthalamic nucleus
Figure 4C, shows the effects of varying stimulus intensity (1 V vs 2 V) within each group (STN DBS(n=4) and EN/GPi DBS(n=3)). The results showed that the size of the activated areas of the brain increased as intensity increased with STN DBS. Stimulation at 2 V (vs 1 V) generated a >30% increase in the size of the activated area, including primary somatosensory cortex, cingulate cortex, caudate, and putamen and showed a higher BOLD% change in the premotor cortex and primary motor cortex (p<0.001, t-test). A similar comparison with EN/GPi DBS, showed increased area of activation in primary somatosensory cortex, insula cortex and a decreased area of activation in prefrontal cortex. In addition, there was no significant difference in BOLD % change with EN/GPi DBS.
PCA was performed comparing each of seventeen STN ROI and nine EN/GPi ROI, defined functionally by the group analysis results in order to identify correlation patterns of the BOLD percent change in each group (Figure 5 and Figure S3). The PCA and subsequent cluster analysis revealed seven distinct clusters associated with STN (p<0.001). Cluster 1 consisted of the thalamus and PPN. Cluster 2 consisted of the caudate nucleus, putamen, and prepyriform area. Cluster 3 consisted of primary motor cortex, lateral geniculate nuclei, and cerebellum. Cluster 4 consisted of parahippocampal gyrus. Cluster 5 consisted of primary somatosensory cortex, somatosensory association cortex, and insular cortex. Cluster 6 consisted of premotor cortex, anterior cingulate cortex and the hippocampus. Cluster 7 consisted of dorsolateral prefrontal cortex and temporal cortex (Figure 5A).
Figure 5.
Principal component analysis between functionally-defined regions of interest for STN (A) and EN/GPi (B) DBS. Additional cluster analysis revealed seven groups for STN DBS and five groups for EN/GPI, which are outlined in circles. For STN DBS clusters 1 and 2 consist of brain areas that represent the basal ganglia-thalamocortical network. Clusters 3 and 5 consist of brain areas representing the sensorimotor network. Clusters 4, 6, and 7 consist of brain areas representing the cognitive/emotional network. EN/GPi DBS pattern that emerged did not share characteristics with any known neural-network pattern.
Abbreviations: BOLD, blood oxygenation level-dependent; Caudate, Caudate nucleus; Cingulate, Anterior cingulate cortex; DBS, Deep brain stimulation; EN, Entopeduncular nucleus; Geniculate, Lateral geniculate nucleus; GPi, Globus pallidus interna; Insula, Insular cortex; PAG, Periaqueductal gray; Parahipo, Parahippocampal gyrus; PC, Principal component; PCA, Principal component analysis; PPN, Pedunculopontine nucleus; Premotor, Premotor cortex; Prefront, Dorsalateral prefrontal cortex; Prepyriform, Prepyriform area; Pri-Motor, Primary motor cortex; Pri-sensory, Primary Somatosensory cortex; ROI, Region of Interest, SC, Superior colluculus; Sensory-Asso, Somatosensory association cortex; STN, Subthalamic nucleus Temp, Temporal nucleus
EN/GPi DBS PCA revealed five clusters (p<0.05). Clusters 1 and 2, with one component each, consisted of periaqueductal gray and primary motor cortex, respectively. Cluster 3 consisted of caudate and insular cortex. Cluster 4 consisted of primary sensory cortex and dorsolateral prefrontal cortex. Cluster 5 consisted of premotor cortex, anterior cingulate cortex, and superior colliculus (Figure 5B).
Discussion
Our results show significant activation in the ipsilateral premotor cortex, primary motor cortex, primary somatosensory cortex, dorsolateral prefrontal cortex, head of the caudate, anterior cingulate cortex, and insular cortex with both STN and EN/GPi stimulation. Combined with previous findings, our data support the theory that DBS has a neuromodulatory effect, which facilitates the basal ganglia-thalamocortical loop complex in modulating global neural activity in both motor and non-motor circuits (Grill et al., 2004; Kringelbach et al., 2007; McIntyre et al., 2004a; McIntyre et al., 2004b; Vitek, 2002b) (See Table 2).
Table 2.
Anatomical connections of STN and EN/GPi
| Category | Locations | Structures | Connections | Functions / Adverse Event (DBS) | |
|---|---|---|---|---|---|
| STN | Substructures | Dorsolateral | Motor area | A: Motor & Premotor cortices (Glu) A: Gpe (GABA) E: GPi, Gpe, and SNr (Glu) |
F: ‘indirect’ pathway of BGTC projection F: ‘indirect’ pathway of BGTC projection F: ‘indirect’ pathway of BGTC projection |
| Ventromedial | Associative area | A: Dorsolateral prefrontal cortex A; Frontal eye field E: SNr |
F: Oculometer control and cognitive aspects of motor behavior F: Oculometer control and cognitive aspects of motor behavior F: Oculometer control and cognitive aspects of motor behavior |
||
| Medial | Limbic area | A: Medial Prefrontal cortex A: Anterior cingulate cortex E: Ventral and medial pallidum |
F: Motivational and emotional aspects of motor behavior F: Motivational and emotional aspects of motor behavior F: Motivational and emotional aspects of motor behavior |
||
| Other connections | A: CmPf (Glu) R: PPN (A: Glu & Cho, E:Glu) R: SNc |
F: Controlling motor patttern generators (Gait) | |||
| Surrounding structures | osterior-medial and dors | Thalamus & medial leminiscus | AE: Persistent dyesthesias | ||
| Lateral and anterior | IC (corticobulbar fibre) | AE: Dysarthria/dysphagia | |||
| IC (corticobulbar fibre) | AE: Tonic muscle contractions | ||||
| Ventral | SN | AE: Acute depression | |||
| Dorsal | ZI and the H2 FF (includes MFB) | ||||
| Medial and ventral | Oculomotor fibres | AE: Diplopia/eye deviations | |||
| Cerebello-thalamic fibres | AE: Antaxia | ||||
| Posteromedial | Red nucleus | ||||
| EN/GPi | Substructures | Posteroventral | Sensorimotor area | A: GPe (GABA) A: STN (Glu) VA nucleus of the thalamus (GABA) VL nucleus of the thalamus (GABA) |
|
| Dorsal | Associative area | AE: Relief of akinesia but no relief of dyskinesia | |||
| Ventomedial | Limbic area | AE: Relief of dyskinesia and rigidity but worse akinesia | |||
| Other connections | E: CmPf (GABA) E: Lateral habenular nucleus (GABA) E: PPN |
||||
| Surrounding structures | Anterior | Anterior commissure | |||
| Ventral | Optic tract | AE: Visual phenomena | |||
| Medial and posterior | IC (corticobulbar fiber) | AE: Dysarthria | |||
| IC (corticospinal fiber) | AE: Tonic muscle contraction |
Abbrevations: A, Afferent connection; AE; Adverse Event; BGTC, Basal ganglia-thalamocortical; Cho, Cholinergic; CmPf, Centromedian and parafascicular nuclei of the thalamus; E, Efferent connection; EN, Entopeduncular nucleus; F, Functions; FF, Field of forel; GABA, γ-Aminobutyric acid; Glu, Glutamatergic; Gpe, Globus pallidus externa; Gpi, Globus pallidus interna; IC, Internal capsule; MFB, Medial forebrain bundle; PPN, Pedunculopontine nucleus; R, Reciprocal connection; SN, Substantia Nigra; SNc, Substantia Nigra pars compacta; SNr, Substantia Nigras pars reticulata; STN, Subthalamic nucleus; VA, Ventral anterior; VL, Ventral lateral; ZI, Zona incerta(Tarsy, 2008; Benarroch, 2008)
The activation of premotor, primary motor and sensory cortices by both STN and EN/GPi DBS supports the sensorimotor network as the basis for the common therapeutic effect of these two targets in the treatment of PD. Compared to EN/GPi DBS, STN DBS was shown on fMRI to recruit a larger area of the motor network. This finding is in concert with the suggestion that STN DBS is a superior target for improving motor performance scores (DBS-study-group, 2001). Of note, our study was not a within-subject design, and the group comparison results may have been affected by the unequal number of subjects per group (4 vs 7). However, our data shows that activation patterns in individual subjects conform well to the group data. The difference in activation found between STN and GPi DBS may be related in part to the physical size difference of GPi compared to STN. The anatomical size of GPi is larger than STN, and the use of an identical stimulation parameter could thus have induced greater electrical stimulation effects for STN DBS compared to GPi DBS. Our voltage comparison results (Figure 4C) suggest that STN is more sensitive than EN/GPi to stimulation intensity. This discrepancy has been demonstrated in the clinical setting in which GPi DBS requires a higher charged density parameter (higher voltage) than does STN-DBS to produce the same therapeutic outcome(Anderson et al., 2005; Okun and Foote, 2005). However, because the outcome can be optimized by changing stimulation contacts and/or stimulation parameters, both STN and GPi are considered appropriate therapeutic targets for DBS, as shown recently in a randomized clinical study on the motor symptoms associated with PD (Anderson et al., 2005).
Of note, although the pig brain is closer in volume and structure to the human brain than the rodent brain, there are marked differences between pigs and humans in the volume of both STN and GPi/EN. The volume of STN is 0.8±0.1 mm3 in the rat, 50±7 mm3 in the pig, 34±6 mm3 in the Macaque monkey, and 240±23mm3 in the human. The volume of EN/GPi is 2.2±0.7mm3 in the rat, ~180mm3 in the pig, 127±26mm3 in the Macaque, and 957±209mm3 in the human (Felix et al., 1999; Hardman et al., 2002; Saikali et al., 2010; Shon et al., 2010). We took several steps to accommodate these volumetric differences. We used a human DBS electrode with low voltage (1V) and long pulse duration (500μsec) in an effort to increase current density while containing the spread of the electrical field. Each DBS electrode has four contact points. The Medtronic 3389 DBS electrode used in this study has smaller gap (0.5mm) between contact points than the Medtronic 3387 electrode, which has a gap of 1.5 mm and is commonly used for human DBS surgery in North America. In addition, we stimulated only the 0–1 contact.
Nonetheless, given the small size of the swine STN and EN/GPi, it is likely that we activated the entire STN and EN/GPi and partly surrounding areas in the pig brain. However, as Figure 5 shows, the activated areas for each target revealed a specific correlation pattern, which suggests a distinct set of network connections.
Other sources of variance in this study include consistency of targeting and the influence of the stimulation block-design. As is true of any electrode implantation study, anatomic variations across subjects can translate into small variations in the precise position of the stimulating electrode. In addition, while stimulations within a stimulation-block may have been independent, it may also have influenced the succeeding stimulations (See supplementary data Figure S2). This potential composite stimulation effect could cause fluctuations in the brain areas that are activated. These inter- and intra-subject sources of variance make the resulting correlations among activated areas seen in Figure 5 and the consistent, integrated networks they appear to define for each target all the more notable.
Obtaining optimal clinical benefit from DBS requires maximal coverage of the targeted subcortical region by the stimulation fields while minimizing current spread to adjacent structures that may induce adverse side-effects (Kringelbach et al., 2007; Montgomery and Gale, 2008). Thus, it is of note that, despite some current spread, we nonetheless found differential, target-specific non-motor network effects. The PCA analysis for STN revealed distinct correlation patterns, each comprising functional connectivity between ROI. Clusters 1 and 2 consisted of brain areas that may represent the basal ganglia-thalamocortical network, including the putamen, caudate nucleus, and thalamus. Clusters 3 and 5 consisted of brain areas representing the sensorimotor network, including primary motor cortex, cerebellum, primary somatosensory cortex, and sensory association cortex. Clusters 4, 6, and 7 consisted of brain areas representing the cognitive/emotional network, including the anterior cingulate cortex, hippocampus, dorsolateral prefrontal cortex and temporal cortex. Although our results also revealed clustering of EN/GPi DBS brain areas, the pattern that emerged did not share characteristics with any known neural-network pattern.
The regional connections found in this study may also shed light on the growing body of evidence that suggests DBS for PD can induce psychiatric complications. Among the known adverse effects, which can include suicide (Appleby et al., 2007; Funkiewiez et al., 2004), are depression(Bejjani et al., 1999; Berney et al., 2002; Doshi et al., 2002; Houeto et al., 2002), hypomania, euphoria, impulsivity and hypersexuality (Burn and Troster, 2004; Chopra et al., 2011; Frank et al., 2007; Herzog et al., 2003; Krack et al., 2001; Kulisevsky et al., 2002; Romito et al., 2002; Witt et al., 2008). These complications are most often associated with STN (versus GPi) DBS (Anderson and Mullins, 2003; Burn and Troster, 2004; Fields et al., 1999; Herzog et al., 2003; Kulisevsky et al., 2002; Miyawaki et al., 2000; Saint-Cyr et al., 2000; Tarsy, 2008; Trepanier et al., 2000; Vingerhoets et al., 1999; Vitek, 2002a; Voon et al., 2006).
Functional neuroimaging studies have shed light on the involvement of non-motor circuits in the cognitive effects and pathophysiology of PD. Metabolic decrease in the left orbitofrontal cortex and dorsal anterior cingulate, for example, has been associated with a decline in verbal learning. Decreased verbal fluency associated with FDG uptake in the left dorsolateral prefrontal cortex and right dorsal anterior cingulate following STN DBS has also been reported (Kalbe et al., 2009). Reduced gray matter density in the insular cortex and cingulate has been linked to apathy in PD (Reijnders et al., 2010). Finally, white matter loss in the cingulate and orbitofrontal cortex is associated with depression in PD (Kostic et al., 2010).
An early human fMRI DBS case study with fMRI results similar to our STN results, reported both mood and motor responses induced by STN DBS. In a patient with PD, left DBS improved motor symptoms. However, unexpectedly, right DBS elicited several reproducible episodes of acute depressive dysphoria. The fMRI data revealed that left DBS primarily affected motor regions, which included increased activation of premotor and motor cortex, ventrolateral thalamus, putamen, and cerebellum, as well as decreased activation of sensorimotor/supplementary motor cortex. Right DBS showed similar but less extensive changes in motor regions. More prominent were the unique increases in the superior prefrontal cortex, anterior cingulate, anterior thalamus, caudate, and brainstem, with marked and widespread decreases in medial prefrontal cortex activation (Stefurak et al., 2003).
A PET study of two patients with PD who underwent DBS surgery revealed additional non-motor effects of STN stimulation (Mallet et al., 2007). Selective stimulation of subterritories of the STN with simultaneous PET assessment of cortical activation showed that with a target localized in the anteromedial STN, stimulation of the anteromedial contact and the contact immediately dorsal to it led to a reduction in motor symptoms, but also consistently produced a hypomanic state. This state was likely mediated by the activation of limbic and association cortex, including areas of the anterior cingulate gyrus and ventral anterior nucleus of the thalamus (Benarroch, 2008; Mallet et al., 2007).
A recent clinical report showed that using model-based optimization of DBS stimulation parameters to avoid current spread to non-motor areas reduced cognitive and cognitive-motor impairments while maintaining therapeutic motor benefit (Frankemolle et al., 2010). Our data suggest that anatomical target placement decisions during human DBS surgery could be augmented by consideration of the functional consequences of STN stimulation on non-motor cortical areas, which, from our results, appear to be part of an electrically influenced STN neural network.
In our study, STN stimulation induced greater activation in the caudate and putamen than EN/GPi. This finding may help to explain why more patients have been able to reduce medication dosage following STN DBS than following GPi DBS (Benabid et al., 1994; DBS-study-group, 2001; Kumar et al., 1998). In previous studies we have shown that electrical stimulation of the STN in the rat induces excitatory postsynaptic potentials in substantia nigra pars compacta (SNc) dopaminergic neurons in vitro (Lee et al., 2004; Lee et al., 2003) and increased striatal dopamine release in vivo (Lee et al., 2006). We have also found that STN DBS in pigs evokes intensity- and frequency-dependent striatal dopamine release (Shon et al., 2010). While it appears that both medication reduction and improved motor performance are consistent with STN DBS in humans, it may be that increased dopamine release produces dopaminergic-related behavioral complications such as impulse control disorders (Broen et al., 2011).
It is well-known that the STN has reciprocal interactions with the dopaminergic neurons of the SNc. The STN, both directly and indirectly, via the PPN conveys excitatory influence from prefrontal cortex to these dopaminergic neurons, which is critical for their reward-related activity (Benarroch, 2008) (See Table 2). For example, a case report of a patient with PD found that ventral STN DBS induced manic symptoms which resolved with dorsolateral STN stimulation (Ulla et al., 2006). The report suggested that the patient’s mania was induced by dopaminergic circuit stimulation. We, too, have reported on a patient with PD in whom STN DBS generated a voltage-dependent mania, possibly due to electrical spread (Chopra et al., 2011). However, a series of [C-11] raclopride PET studies in PD patients failed to demonstrate any changes in synaptic dopamine release induced by DBS (Abosch et al., 2003; Hilker et al., 2003; Strafella et al., 2003). Thus the role of dopamine in DBS remains unclear and warrants further study.
Current postoperative DBS pulse generator programming decisions are based on and limited by the subjective judgments of the patient and the stimulus programmer. It has been reported that more than one-third of patients referred to two specialized movement disorder centers for “DBS failures” were not properly programmed (Okun et al., 2005). Given the potential for fMRI to reveal distal activation from DBS, we envision it could be a useful adjunct for objectively determining and evaluating programming parameters after DBS surgery (Kringelbach et al., 2007). We also recognize that it is important to keep in mind safety precautions when using fMRI with DBS, predominant among which is the increase in temperature near the electrode tips from the scanner RF field focusing (Baker et al., 2007; Carmichael et al., 2007; Phillips et al., 2006; Pictet et al., 2002; Rezai et al., 2005; Rezai et al., 2002).
We recognize several limitations of the present study. In our data,the frontal sinus of the pig brain is thought to cause a geometric distortion in the EPI image, which is limited to rostral part of the prefrontal cortex and anterior part of the primary somatosensory cortex. Thus, some activated brain regions in the frontal cortex were outside of the atlas borders. However, although this MRI distortion could have caused an error in the voxel-based analysis, especially in prefrontal cortex, it is of note that it is limited to the tissue-air interfaces and thus unlikely to affect other brain areas (Jezzard and Clare, 1999).
We also recognize that our STN DBS vs GPi DBS comparison is not a within-subject design using within-scan comparison. Therefore more sophisticated fMRI experiments would be needed in the future to further evaluate the question of clinical therapeutic effects vs side effects of STN vs GPi DBS. This question remains a matter of considerable debate (Green et al., 2006; Moum et al., 2012; Okun and Foote, 2005; Weaver et al., 2012).
In addition, to better accommodate the small size of the pig STN and EN/GPi, rather than using a hum an DBS electrode, we plan to use miniaturized DBS leads (Miocinovic et al., 2007). We also envision that a more sophisticated lead design (Chaturvedi et al., 2012; Martens et al., 2011)} and a selective neuronal activation method, such as optogenetic stimulation (Kravitz et al., 2010; Lee, 2012), which can be combined with neuroimaging would allow enhanced discrimination of the global neuromodulary network effects of neural stimulation.
Functional neuroimaging is extremely difficult in the conscious animal. Although awake fMRI might yield different results from those in the anesthetized state, our use of sedation and muscle relaxant was based on previous animal fMRI studies which showed robust visual and electrical stimulation-dependent BOLD responses and electrophysiological responses in the anesthetized state (Angenstein et al., 2009; Angenstein et al., 2010; Jin and Kim, 2008; Masamoto et al., 2007).
In the present study, we used an acute protocol in a non-PD animal model, which enabled both proof of principle and an investigation of the effects of neural network electrical stimulation on the normally functioning swine brain model. We have recently confirmed our MR image-guided targeting system and fMRI group analysis method in Yucatan minipigs (data not included) for which there is a PD model available (Bjarkam et al., 2008; Nielsen et al., 2009). The work reported here, thus sets the stage for future investigations that combine functional neuroimaging with electrical stimulation in a chronic MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) PD model.
Conclusions
Our findings suggest that DBS at both targets increased BOLD activation at a number of subcortical and cortical projection areas within the basal ganglia-thalamocortical network. The activated brain areas shown in our data reflect an effect of electrical stimulation spreading via orthodromic and/or antidromic activation for each DBS target. While STN and EN/GPi stimulation showed common sensorimotor network activation, our correlation data suggest that each target also activates a distinctive neural network. Taken together our results support the differences and similarities between STN and GPi noted in clinical reports comparing the two targets. The results also suggest that that the swine model for DBS fMRI, which conforms to human implanted DBS electrode configurations and human neuroanatomy, may be a useful platform for translational studies investigating the global neuromodulatory effects of DBS.
Supplementary Material
Highlights.
First report to set up a fMRI group analysis method for pigs.
STN vs EN/GPi stimulation shown common sensorimotor network activation.
PCA data also show that each target activates a distinctive neural network.
Swine model may be a useful platform for global neuromodulatory DBS studies.
Acknowledgments
This work was supported by The Grainger Foundation, and by the National Institutes of Health (K08 NS 52232 and R01 NS 70872 to KHL). The authors are grateful to Penelope Duffy, Ph.D. for her editorial contributions and review. We thank Dr. Stephan Saikali and Dr. Charles Henri Malbert for their public release of their 3D ultra-high resolution pig brain atlas. We also thank Osama Abulseoud, M.D. for his assistance with the psychiatric portions of the Discussion and the Center for Advanced Imaging Research, Opus Building, Mayo Clinic for their support.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abosch A, Kapur S, Lang AE, Hussey D, Sime E, Miyasaki J, Houle S, Lozano AM. Stimulation of the subthalamic nucleus in Parkinson’s disease does not produce striatal dopamine release. Neurosurgery. 2003;53:1095–1102. doi: 10.1227/01.neu.0000088662.69419.1b. discussion 1102–1095. [DOI] [PubMed] [Google Scholar]
- Alexander GE, DeLong MR, Strick PL. Parallel organization of functionally segregated circuits linking basal ganglia and cortex. Annual review of neuroscience. 1986;9:357–381. doi: 10.1146/annurev.ne.09.030186.002041. [DOI] [PubMed] [Google Scholar]
- Anderberg MR. Cluster analysis for applications. Academic Press; New York: 1973. [Google Scholar]
- Anderson KE, Mullins J. Behavioral changes associated with deep brain stimulation surgery for Parkinson’s disease. Current neurology and neuroscience reports. 2003;3:306–313. doi: 10.1007/s11910-003-0007-z. [DOI] [PubMed] [Google Scholar]
- Anderson VC, Burchiel KJ, Hogarth P, Favre J, Hammerstad JP. Pallidal vs subthalamic nucleus deep brain stimulation in Parkinson disease. Archives of neurology. 2005;62:554–560. doi: 10.1001/archneur.62.4.554. [DOI] [PubMed] [Google Scholar]
- Angenstein F, Kammerer E, Scheich H. The BOLD response in the rat hippocampus depends rather on local processing of signals than on the input or output activity. A combined functional MRI and electrophysiological study. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2009;29:2428–2439. doi: 10.1523/JNEUROSCI.5015-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angenstein F, Krautwald K, Scheich H. The current functional state of local neuronal circuits controls the magnitude of a BOLD response to incoming stimuli. NeuroImage. 2010;50:1364–1375. doi: 10.1016/j.neuroimage.2010.01.070. [DOI] [PubMed] [Google Scholar]
- Appleby BS, Duggan PS, Regenberg A, Rabins PV. Psychiatric and neuropsychiatric adverse events associated with deep brain stimulation: A meta-analysis of ten years’ experience. Movement disorders : official journal of the Movement Disorder Society. 2007;22:1722–1728. doi: 10.1002/mds.21551. [DOI] [PubMed] [Google Scholar]
- Baker KB, Kopell BH, Malone D, Horenstein C, Lowe M, Phillips MD, Rezai AR. Deep brain stimulation for obsessive-compulsive disorder: using functional magnetic resonance imaging and electrophysiological techniques: technical case report. Neurosurgery. 2007;61:E367–368. doi: 10.1227/01.neu.0000303995.66902.36. discussion E368. [DOI] [PubMed] [Google Scholar]
- Bejjani BP, Damier P, Arnulf I, Thivard L, Bonnet AM, Dormont D, Cornu P, Pidoux B, Samson Y, Agid Y. Transient acute depression induced by high-frequency deep-brain stimulation. The New England journal of medicine. 1999;340:1476–1480. doi: 10.1056/NEJM199905133401905. [DOI] [PubMed] [Google Scholar]
- Benabid AL. Deep brain stimulation for Parkinson’s disease. Current opinion in neurobiology. 2003;13:696–706. doi: 10.1016/j.conb.2003.11.001. [DOI] [PubMed] [Google Scholar]
- Benabid AL, Benazzouz A, Hoffmann D, Limousin P, Krack P, Pollak P. Long-term electrical inhibition of deep brain targets in movement disorders. Movement disorders : official journal of the Movement Disorder Society. 1998;13(Suppl 3):119–125. doi: 10.1002/mds.870131321. [DOI] [PubMed] [Google Scholar]
- Benabid AL, Pollak P, Gross C, Hoffmann D, Benazzouz A, Gao DM, Laurent A, Gentil M, Perret J. Acute and long-term effects of subthalamic nucleus stimulation in Parkinson’s disease. Stereotactic and functional neurosurgery. 1994;62:76–84. doi: 10.1159/000098600. [DOI] [PubMed] [Google Scholar]
- Benabid AL, Pollak P, Seigneuret E, Hoffmann D, Gay E, Perret J. Chronic VIM thalamic stimulation in Parkinson’s disease, essential tremor and extra-pyramidal dyskinesias. Acta Neurochir Suppl (Wien) 1993;58:39–44. doi: 10.1007/978-3-7091-9297-9_8. [DOI] [PubMed] [Google Scholar]
- Benarroch EE. Subthalamic nucleus and its connections: Anatomic substrate for the network effects of deep brain stimulation. Neurology. 2008;70:1991–1995. doi: 10.1212/01.wnl.0000313022.39329.65. [DOI] [PubMed] [Google Scholar]
- Berney A, Vingerhoets F, Perrin A, Guex P, Villemure JG, Burkhard PR, Benkelfat C, Ghika J. Effect on mood of subthalamic DBS for Parkinson’s disease: a consecutive series of 24 patients. Neurology. 2002;59:1427–1429. doi: 10.1212/01.wnl.0000032756.14298.18. [DOI] [PubMed] [Google Scholar]
- Bjarkam CR, Nielsen MS, Glud AN, Rosendal F, Mogensen P, Bender D, Doudet D, Moller A, Sorensen JC. Neuromodulation in a minipig MPTP model of Parkinson disease. British journal of neurosurgery. 2008;22(Suppl 1):S9–12. doi: 10.1080/02688690802448285. [DOI] [PubMed] [Google Scholar]
- Broen M, Duits A, Visser-Vandewalle V, Temel Y, Winogrodzka A. Impulse control and related disorders in Parkinson’s disease patients treated with bilateral subthalamic nucleus stimulation: a review. Parkinsonism & related disorders. 2011;17:413–417. doi: 10.1016/j.parkreldis.2011.02.013. [DOI] [PubMed] [Google Scholar]
- Brown RG, Dowsey PL, Brown P, Jahanshahi M, Pollak P, Benabid AL, Rodriguez-Oroz MC, Obeso J, Rothwell JC. Impact of deep brain stimulation on upper limb akinesia in Parkinson’s disease. Annals of neurology. 1999;45:473–488. doi: 10.1002/1531-8249(199904)45:4<473::aid-ana9>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- Burchiel KJ, Anderson VC, Favre J, Hammerstad JP. Comparison of pallidal and subthalamic nucleus deep brain stimulation for advanced Parkinson’s disease: results of a randomized, blinded pilot study. Neurosurgery. 1999;45:1375–1382. doi: 10.1097/00006123-199912000-00024. discussion 1382–1374. [DOI] [PubMed] [Google Scholar]
- Burn DJ, Troster AI. Neuropsychiatric complications of medical and surgical therapies for Parkinson’s disease. Journal of geriatric psychiatry and neurology. 2004;17:172–180. doi: 10.1177/0891988704267466. [DOI] [PubMed] [Google Scholar]
- Carmichael DW, Pinto S, Limousin-Dowsey P, Thobois S, Allen PJ, Lemieux L, Yousry T, Thornton JS. Functional MRI with active, fully implanted, deep brain stimulation systems: safety and experimental confounds. NeuroImage. 2007;37:508–517. doi: 10.1016/j.neuroimage.2007.04.058. [DOI] [PubMed] [Google Scholar]
- Ceballos-Baumann AO, Boecker H, Bartenstein P, von Falkenhayn I, Riescher H, Conrad B, Moringlane JR, Alesch F. A positron emission tomographic study of subthalamic nucleus stimulation in Parkinson disease: enhanced movement-related activity of motor-association cortex and decreased motor cortex resting activity. Archives of neurology. 1999;56:997–1003. doi: 10.1001/archneur.56.8.997. [DOI] [PubMed] [Google Scholar]
- Ceballos-Baumann AO, Boecker H, Fogel W, Alesch F, Bartenstein P, Conrad B, Diederich N, von Falkenhayn I, Moringlane JR, Schwaiger M, Tronnier VM. Thalamic stimulation for essential tremor activates motor and deactivates vestibular cortex. Neurology. 2001;56:1347–1354. doi: 10.1212/wnl.56.10.1347. [DOI] [PubMed] [Google Scholar]
- Chaturvedi A, Foutz TJ, McIntyre CC. Current steering to activate targeted neural pathways during deep brain stimulation of the subthalamic region. Brain stimulation. 2012;5:369–377. doi: 10.1016/j.brs.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho ZH, Min HK, Oh SH, Han JY, Park CW, Chi JG, Kim YB, Paek SH, Lozano AM, Lee KH. Direct visualization of deep brain stimulation targets in Parkinson disease with the use of 7-tesla magnetic resonance imaging. Journal of neurosurgery. 2010;113:639–647. doi: 10.3171/2010.3.JNS091385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chopra A, Tye SJ, Lee KH, Matsumoto J, Klassen B, Adams AC, Stead M, Sampson S, Kall BA, Frye MA. Voltage-dependent mania after subthalamic nucleus deep brain stimulation in Parkinson’s disease: a case report. Biological psychiatry. 2011;70:e5–7. doi: 10.1016/j.biopsych.2010.12.035. [DOI] [PubMed] [Google Scholar]
- Davis KD, Taub E, Duffner F, Lozano AM, Tasker RR, Houle S, Dostrovsky JO. Activation of the anterior cingulate cortex by thalamic stimulation in patients with chronic pain: a positron emission tomography study. Journal of neurosurgery. 2000;92:64–69. doi: 10.3171/jns.2000.92.1.0064. [DOI] [PubMed] [Google Scholar]
- DBS-study-group. Deep-brain stimulation of the subthalamic nucleus or the pars interna of the globus pallidus in Parkinson’s disease. The New England journal of medicine. 2001;345:956–963. doi: 10.1056/NEJMoa000827. [DOI] [PubMed] [Google Scholar]
- Deiber MP, Pollak P, Passingham R, Landais P, Gervason C, Cinotti L, Friston K, Frackowiak R, Mauguiere F, Benabid AL. Thalamic stimulation and suppression of parkinsonian tremor. Evidence of a cerebellar deactivation using positron emission tomography. Brain : a journal of neurology. 1993;116 ( Pt 1):267–279. doi: 10.1093/brain/116.1.267. [DOI] [PubMed] [Google Scholar]
- Deuschl G, Schade-Brittinger C, Krack P, Volkmann J, Schafer H, Botzel K, Daniels C, Deutschlander A, Dillmann U, Eisner W, Gruber D, Hamel W, Herzog J, Hilker R, Klebe S, Kloss M, Koy J, Krause M, Kupsch A, Lorenz D, Lorenzl S, Mehdorn HM, Moringlane JR, Oertel W, Pinsker MO, Reichmann H, Reuss A, Schneider GH, Schnitzler A, Steude U, Sturm V, Timmermann L, Tronnier V, Trottenberg T, Wojtecki L, Wolf E, Poewe W, Voges J. A randomized trial of deep-brain stimulation for Parkinson’s disease. The New England journal of medicine. 2006;355:896–908. doi: 10.1056/NEJMoa060281. [DOI] [PubMed] [Google Scholar]
- Doshi PK, Chhaya N, Bhatt MH. Depression leading to attempted suicide after bilateral subthalamic nucleus stimulation for Parkinson’s disease. Movement disorders : official journal of the Movement Disorder Society. 2002;17:1084–1085. doi: 10.1002/mds.10198. [DOI] [PubMed] [Google Scholar]
- Dunteman GH. Principal components analysis. Sage Publications; Newbury Park: 1989. [Google Scholar]
- Felix B, Leger ME, Albe-Fessard D, Marcilloux JC, Rampin O, Laplace JP. Stereotaxic atlas of the pig brain. Brain research bulletin. 1999;49:1–137. doi: 10.1016/s0361-9230(99)00012-x. [DOI] [PubMed] [Google Scholar]
- Fields JA, Troster AI, Wilkinson SB, Pahwa R, Koller WC. Cognitive outcome following staged bilateral pallidal stimulation for the treatment of Parkinson’s disease. Clinical neurology and neurosurgery. 1999;101:182–188. doi: 10.1016/s0303-8467(99)00044-x. [DOI] [PubMed] [Google Scholar]
- Frank MJ, Samanta J, Moustafa AA, Sherman SJ. Hold your horses: impulsivity, deep brain stimulation, and medication in parkinsonism. Science. 2007;318:1309–1312. doi: 10.1126/science.1146157. [DOI] [PubMed] [Google Scholar]
- Frankemolle AM, Wu J, Noecker AM, Voelcker-Rehage C, Ho JC, Vitek JL, McIntyre CC, Alberts JL. Reversing cognitive-motor impairments in Parkinson’s disease patients using a computational modelling approach to deep brain stimulation programming. Brain : a journal of neurology. 2010;133:746–761. doi: 10.1093/brain/awp315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funkiewiez A, Ardouin C, Caputo E, Krack P, Fraix V, Klinger H, Chabardes S, Foote K, Benabid AL, Pollak P. Long term effects of bilateral subthalamic nucleus stimulation on cognitive function, mood, and behaviour in Parkinson’s disease. Journal of neurology, neurosurgery, and psychiatry. 2004;75:834–839. doi: 10.1136/jnnp.2002.009803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghika J, Villemure JG, Fankhauser H, Favre J, Assal G, Ghika-Schmid F. Efficiency and safety of bilateral contemporaneous pallidal stimulation (deep brain stimulation) in levodopa-responsive patients with Parkinson’s disease with severe motor fluctuations: a 2-year follow-up review. Journal of neurosurgery. 1998;89:713–718. doi: 10.3171/jns.1998.89.5.0713. [DOI] [PubMed] [Google Scholar]
- Grafton ST, DeLong M. Tracing the brain’s circuitry with functional imaging. Nature medicine. 1997;3:602–603. doi: 10.1038/nm0697-602. [DOI] [PubMed] [Google Scholar]
- Green AL, Bittar RG, Bain P, Scott RB, Joint C, Gregory R, Aziz TZ. STN vs. Pallidal Stimulation in Parkinson Disease: Improvement With Experience and Better Patient Selection. Neuromodulation : journal of the International Neuromodulation Society. 2006;9:21–27. doi: 10.1111/j.1525-1403.2006.00038.x. [DOI] [PubMed] [Google Scholar]
- Greene P. Deep-brain stimulation for generalized dystonia. The New England journal of medicine. 2005;352:498–500. doi: 10.1056/NEJMe048333. [DOI] [PubMed] [Google Scholar]
- Grill WM, Snyder AN, Miocinovic S. Deep brain stimulation creates an informational lesion of the stimulated nucleus. Neuroreport. 2004;15:1137–1140. doi: 10.1097/00001756-200405190-00011. [DOI] [PubMed] [Google Scholar]
- Hardman CD, Henderson JM, Finkelstein DI, Horne MK, Paxinos G, Halliday GM. Comparison of the basal ganglia in rats, marmosets, macaques, baboons, and humans: volume and neuronal number for the output, internal relay, and striatal modulating nuclei. The Journal of comparative neurology. 2002;445:238–255. doi: 10.1002/cne.10165. [DOI] [PubMed] [Google Scholar]
- Haslinger B, Boecker H, Buchel C, Vesper J, Tronnier VM, Pfister R, Alesch F, Moringlane JR, Krauss JK, Conrad B, Schwaiger M, Ceballos-Baumann AO. Differential modulation of subcortical target and cortex during deep brain stimulation. NeuroImage. 2003;18:517–524. doi: 10.1016/s1053-8119(02)00043-5. [DOI] [PubMed] [Google Scholar]
- Herzog J, Reiff J, Krack P, Witt K, Schrader B, Muller D, Deuschl G. Manic episode with psychotic symptoms induced by subthalamic nucleus stimulation in a patient with Parkinson’s disease. Movement disorders : official journal of the Movement Disorder Society. 2003;18:1382–1384. doi: 10.1002/mds.10530. [DOI] [PubMed] [Google Scholar]
- Hilker R, Voges J, Ghaemi M, Lehrke R, Rudolf J, Koulousakis A, Herholz K, Wienhard K, Sturm V, Heiss WD. Deep brain stimulation of the subthalamic nucleus does not increase the striatal dopamine concentration in parkinsonian humans. Movement disorders : official journal of the Movement Disorder Society. 2003;18:41–48. doi: 10.1002/mds.10297. [DOI] [PubMed] [Google Scholar]
- Houeto JL, Mesnage V, Mallet L, Pillon B, Gargiulo M, du Moncel ST, Bonnet AM, Pidoux B, Dormont D, Cornu P, Agid Y. Behavioural disorders, Parkinson’s disease and subthalamic stimulation. Journal of neurology, neurosurgery, and psychiatry. 2002;72:701–707. doi: 10.1136/jnnp.72.6.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jech R, Urgosik D, Tintera J, Nebuzelsky A, Krasensky J, Liscak R, Roth J, Ruzicka E. Functional magnetic resonance imaging during deep brain stimulation: a pilot study in four patients with Parkinson’s disease. Movement disorders : official journal of the Movement Disorder Society. 2001;16:1126–1132. doi: 10.1002/mds.1217. [DOI] [PubMed] [Google Scholar]
- Jezzard P, Clare S. Sources of distortion in functional MRI data. Human brain mapping. 1999;8:80–85. doi: 10.1002/(SICI)1097-0193(1999)8:2/3<80::AID-HBM2>3.0.CO;2-C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin T, Kim SG. Cortical layer-dependent dynamic blood oxygenation, cerebral blood flow and cerebral blood volume responses during visual stimulation. NeuroImage. 2008;43:1–9. doi: 10.1016/j.neuroimage.2008.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalbe E, Voges J, Weber T, Haarer M, Baudrexel S, Klein JC, Kessler J, Sturm V, Heiss WD, Hilker R. Frontal FDG-PET activity correlates with cognitive outcome after STN-DBS in Parkinson disease. Neurology. 2009;72:42–49. doi: 10.1212/01.wnl.0000338536.31388.f0. [DOI] [PubMed] [Google Scholar]
- Kostic VS, Agosta F, Petrovic I, Galantucci S, Spica V, Jecmenica-Lukic M, Filippi M. Regional patterns of brain tissue loss associated with depression in Parkinson disease. Neurology. 2010;75:857–863. doi: 10.1212/WNL.0b013e3181f11c1d. [DOI] [PubMed] [Google Scholar]
- Krack P, Benazzouz A, Pollak P, Limousin P, Piallat B, Hoffmann D, Xie J, Benabid AL. Treatment of tremor in Parkinson’s disease by subthalamic nucleus stimulation. Movement disorders : official journal of the Movement Disorder Society. 1998;13:907–914. doi: 10.1002/mds.870130608. [DOI] [PubMed] [Google Scholar]
- Krack P, Hamel W, Mehdorn HM, Deuschl G. Surgical treatment of Parkinson’s disease. Current opinion in neurology. 1999;12:417–425. doi: 10.1097/00019052-199908000-00008. [DOI] [PubMed] [Google Scholar]
- Krack P, Kumar R, Ardouin C, Dowsey PL, McVicker JM, Benabid AL, Pollak P. Mirthful laughter induced by subthalamic nucleus stimulation. Movement disorders : official journal of the Movement Disorder Society. 2001;16:867–875. doi: 10.1002/mds.1174. [DOI] [PubMed] [Google Scholar]
- Kravitz AV, Freeze BS, Parker PR, Kay K, Thwin MT, Deisseroth K, Kreitzer AC. Regulation of parkinsonian motor behaviours by optogenetic control of basal ganglia circuitry. Nature. 2010;466:622–626. doi: 10.1038/nature09159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kringelbach ML, Jenkinson N, Owen SL, Aziz TZ. Translational principles of deep brain stimulation. Nat Rev Neurosci. 2007;8:623–635. doi: 10.1038/nrn2196. [DOI] [PubMed] [Google Scholar]
- Kulisevsky J, Berthier ML, Gironell A, Pascual-Sedano B, Molet J, Pares P. Mania following deep brain stimulation for Parkinson’s disease. Neurology. 2002;59:1421–1424. doi: 10.1212/wnl.59.9.1421. [DOI] [PubMed] [Google Scholar]
- Kumar R, Lozano AM, Montgomery E, Lang AE. Pallidotomy and deep brain stimulation of the pallidum and subthalamic nucleus in advanced Parkinson’s disease. Movement disorders : official journal of the Movement Disorder Society. 1998;13(Suppl 1):73–82. [PubMed] [Google Scholar]
- Lee JH. Informing brain connectivity with optogenetic functional magnetic resonance imaging. NeuroImage. 2012 doi: 10.1016/j.neuroimage.2012.01.116. [DOI] [PubMed] [Google Scholar]
- Lee KH, Blaha CD, Harris BT, Cooper S, Hitti FL, Leiter JC, Roberts DW, Kim U. Dopamine efflux in the rat striatum evoked by electrical stimulation of the subthalamic nucleus: potential mechanism of action in Parkinson’s disease. The European journal of neuroscience. 2006;23:1005–1014. doi: 10.1111/j.1460-9568.2006.04638.x. [DOI] [PubMed] [Google Scholar]
- Lee KH, Chang SY, Roberts DW, Kim U. Neurotransmitter release from high-frequency stimulation of the subthalamic nucleus. Journal of neurosurgery. 2004;101:511–517. doi: 10.3171/jns.2004.101.3.0511. [DOI] [PubMed] [Google Scholar]
- Lee KH, Roberts DW, Kim U. Effect of high-frequency stimulation of the subthalamic nucleus on subthalamic neurons: an intracellular study. Stereotactic and functional neurosurgery. 2003;80:32–36. doi: 10.1159/000075157. [DOI] [PubMed] [Google Scholar]
- Limousin P, Krack P, Pollak P, Benazzouz A, Ardouin C, Hoffmann D, Benabid AL. Electrical stimulation of the subthalamic nucleus in advanced Parkinson’s disease. The New England journal of medicine. 1998;339:1105–1111. doi: 10.1056/NEJM199810153391603. [DOI] [PubMed] [Google Scholar]
- Mallet L, Schupbach M, N’Diaye K, Remy P, Bardinet E, Czernecki V, Welter ML, Pelissolo A, Ruberg M, Agid Y, Yelnik J. Stimulation of subterritories of the subthalamic nucleus reveals its role in the integration of the emotional and motor aspects of behavior. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:10661–10666. doi: 10.1073/pnas.0610849104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mardia KV, Kent JT, Bibby JM. Multivariate analysis. Academic Press; London ; New York: 1979. [Google Scholar]
- Martens HC, Toader E, Decre MM, Anderson DJ, Vetter R, Kipke DR, Baker KB, Johnson MD, Vitek JL. Spatial steering of deep brain stimulation volumes using a novel lead design. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology. 2011;122:558–566. doi: 10.1016/j.clinph.2010.07.026. [DOI] [PubMed] [Google Scholar]
- Masamoto K, Kim T, Fukuda M, Wang P, Kim SG. Relationship between neural, vascular, and BOLD signals in isoflurane-anesthetized rat somatosensory cortex. Cerebral cortex. 2007;17:942–950. doi: 10.1093/cercor/bhl005. [DOI] [PubMed] [Google Scholar]
- McIntyre CC, Grill WM, Sherman DL, Thakor NV. Cellular effects of deep brain stimulation: model-based analysis of activation and inhibition. Journal of neurophysiology. 2004a;91:1457–1469. doi: 10.1152/jn.00989.2003. [DOI] [PubMed] [Google Scholar]
- McIntyre CC, Hahn PJ. Network perspectives on the mechanisms of deep brain stimulation. Neurobiology of disease. 2010;38:329–337. doi: 10.1016/j.nbd.2009.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre CC, Mori S, Sherman DL, Thakor NV, Vitek JL. Electric field and stimulating influence generated by deep brain stimulation of the subthalamic nucleus. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology. 2004b;115:589–595. doi: 10.1016/j.clinph.2003.10.033. [DOI] [PubMed] [Google Scholar]
- Miocinovic S, Zhang J, Xu W, Russo GS, Vitek JL, McIntyre CC. Stereotactic neurosurgical planning, recording, and visualization for deep brain stimulation in non-human primates. Journal of neuroscience methods. 2007;162:32–41. doi: 10.1016/j.jneumeth.2006.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyawaki E, Perlmutter JS, Troster AI, Videen TO, Koller WC. The behavioral complications of pallidal stimulation: a case report. Brain and cognition. 2000;42:417–434. doi: 10.1006/brcg.1999.1113. [DOI] [PubMed] [Google Scholar]
- Montgomery EB, Jr, Gale JT. Mechanisms of action of deep brain stimulation(DBS) Neuroscience and biobehavioral reviews. 2008;32:388–407. doi: 10.1016/j.neubiorev.2007.06.003. [DOI] [PubMed] [Google Scholar]
- Moum SJ, Price CC, Limotai N, Oyama G, Ward H, Jacobson C, Foote KD, Okun MS. Effects of STN and GPi deep brain stimulation on impulse control disorders and dopamine dysregulation syndrome. PloS one. 2012;7:e29768. doi: 10.1371/journal.pone.0029768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen MS, Sorensen JC, Bjarkam CR. The substantia nigra pars compacta of the Gottingen minipig: an anatomical and stereological study. Brain structure & function. 2009;213:481–488. doi: 10.1007/s00429-009-0217-5. [DOI] [PubMed] [Google Scholar]
- Okun MS, Foote KD. Subthalamic nucleus vs globus pallidus interna deep brain stimulation, the rematch: will pallidal deep brain stimulation make a triumphant return? Archives of neurology. 2005;62:533–536. doi: 10.1001/archneur.62.4.533. [DOI] [PubMed] [Google Scholar]
- Okun MS, Tagliati M, Pourfar M, Fernandez HH, Rodriguez RL, Alterman RL, Foote KD. Management of referred deep brain stimulation failures: a retrospective analysis from 2 movement disorders centers. Archives of neurology. 2005;62:1250–1255. doi: 10.1001/archneur.62.8.noc40425. [DOI] [PubMed] [Google Scholar]
- Phillips MD, Baker KB, Lowe MJ, Tkach JA, Cooper SE, Kopell BH, Rezai AR. Parkinson disease: pattern of functional MR imaging activation during deep brain stimulation of subthalamic nucleus--initial experience. Radiology. 2006;239:209–216. doi: 10.1148/radiol.2391041990. [DOI] [PubMed] [Google Scholar]
- Pictet J, Meuli R, Wicky S, van der Klink JJ. Radiofrequency heating effects around resonant lengths of wire in MRI. Physics in medicine and biology. 2002;47:2973–2985. doi: 10.1088/0031-9155/47/16/312. [DOI] [PubMed] [Google Scholar]
- Pour-El I. Animals in Translation: Using the Mysteries of Autism To Decode Animal Behavior. Library Journal. 2006;131:119–119. [Google Scholar]
- Reijnders JS, Scholtissen B, Weber WE, Aalten P, Verhey FR, Leentjens AF. Neuroanatomical correlates of apathy in Parkinson’s disease: A magnetic resonance imaging study using voxel-based morphometry. Movement disorders : official journal of the Movement Disorder Society. 2010;25:2318–2325. doi: 10.1002/mds.23268. [DOI] [PubMed] [Google Scholar]
- Rezai AR, Baker KB, Tkach JA, Phillips M, Hrdlicka G, Sharan AD, Nyenhuis J, Ruggieri P, Shellock FG, Henderson J. Is magnetic resonance imaging safe for patients with neurostimulation systems used for deep brain stimulation? Neurosurgery. 2005;57:1056–1062. doi: 10.1227/01.neu.0000186935.87971.2a. discussion 1056–1062. [DOI] [PubMed] [Google Scholar]
- Rezai AR, Finelli D, Nyenhuis JA, Hrdlicka G, Tkach J, Sharan A, Rugieri P, Stypulkowski PH, Shellock FG. Neurostimulation systems for deep brain stimulation: in vitro evaluation of magnetic resonance imaging-related heating at 1.5 tesla. Journal of magnetic resonance imaging : JMRI. 2002;15:241–250. doi: 10.1002/jmri.10069. [DOI] [PubMed] [Google Scholar]
- Rezai AR, Lozano AM, Crawley AP, Joy ML, Davis KD, Kwan CL, Dostrovsky JO, Tasker RR, Mikulis DJ. Thalamic stimulation and functional magnetic resonance imaging: localization of cortical and subcortical activation with implanted electrodes. Technical note. Journal of neurosurgery. 1999;90:583–590. doi: 10.3171/jns.1999.90.3.0583. [DOI] [PubMed] [Google Scholar]
- Romito LM, Raja M, Daniele A, Contarino MF, Bentivoglio AR, Barbier A, Scerrati M, Albanese A. Transient mania with hypersexuality after surgery for high frequency stimulation of the subthalamic nucleus in Parkinson’s disease. Movement disorders : official journal of the Movement Disorder Society. 2002;17:1371–1374. doi: 10.1002/mds.10265. [DOI] [PubMed] [Google Scholar]
- Saikali S, Meurice P, Sauleau P, Eliat PA, Bellaud P, Randuineau G, Verin M, Malbert CH. A three-dimensional digital segmented and deformable brain atlas of the domestic pig. Journal of neuroscience methods. 2010;192:102–109. doi: 10.1016/j.jneumeth.2010.07.041. [DOI] [PubMed] [Google Scholar]
- Saint-Cyr JA, Trepanier LL, Kumar R, Lozano AM, Lang AE. Neuropsychological consequences of chronic bilateral stimulation of the subthalamic nucleus in Parkinson’s disease. Brain : a journal of neurology. 2000;123 ( Pt 10):2091–2108. doi: 10.1093/brain/123.10.2091. [DOI] [PubMed] [Google Scholar]
- Shon YM, Lee KH, Goerss SJ, Kim IY, Kimble C, Van Gompel JJ, Bennet K, Blaha CD, Chang SY. High frequency stimulation of the subthalamic nucleus evokes striatal dopamine release in a large animal model of human DBS neurosurgery. Neuroscience letters. 2010;475:136–140. doi: 10.1016/j.neulet.2010.03.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SM, Jenkinson M, Woolrich MW, Beckmann CF, Behrens TE, Johansen-Berg H, Bannister PR, De Luca M, Drobnjak I, Flitney DE, Niazy RK, Saunders J, Vickers J, Zhang Y, De Stefano N, Brady JM, Matthews PM. Advances in functional and structural MR image analysis and implementation as FSL. NeuroImage. 2004;23(Suppl 1):S208–219. doi: 10.1016/j.neuroimage.2004.07.051. [DOI] [PubMed] [Google Scholar]
- Starr PA, Christine CW, Theodosopoulos PV, Lindsey N, Byrd D, Mosley A, Marks WJ., Jr Implantation of deep brain stimulators into the subthalamic nucleus: technical approach and magnetic resonance imaging-verified lead locations. Journal of neurosurgery. 2002;97:370–387. doi: 10.3171/jns.2002.97.2.0370. [DOI] [PubMed] [Google Scholar]
- Stefurak T, Mikulis D, Mayberg H, Lang AE, Hevenor S, Pahapill P, Saint-Cyr J, Lozano A. Deep brain stimulation for Parkinson’s disease dissociates mood and motor circuits: a functional MRI case study. Movement disorders : official journal of the Movement Disorder Society. 2003;18:1508–1516. doi: 10.1002/mds.10593. [DOI] [PubMed] [Google Scholar]
- Strafella AP, Sadikot AF, Dagher A. Subthalamic deep brain stimulation does not induce striatal dopamine release in Parkinson’s disease. Neuroreport. 2003;14:1287–1289. doi: 10.1097/00001756-200307010-00020. [DOI] [PubMed] [Google Scholar]
- Tarsy D. Deep brain stimulation in neurological and psychiatric disorders. Humana Press; Totowa, NJ: 2008. [Google Scholar]
- Trepanier LL, Kumar R, Lozano AM, Lang AE, Saint-Cyr JA. Neuropsychological outcome of GPi pallidotomy and GPi or STN deep brain stimulation in Parkinson’s disease. Brain and cognition. 2000;42:324–347. doi: 10.1006/brcg.1999.1108. [DOI] [PubMed] [Google Scholar]
- Ulla M, Thobois S, Lemaire JJ, Schmitt A, Derost P, Broussolle E, Llorca PM, Durif F. Manic behaviour induced by deep-brain stimulation in Parkinson’s disease: evidence of substantia nigra implication? Journal of neurology, neurosurgery, and psychiatry. 2006;77:1363–1366. doi: 10.1136/jnnp.2006.096628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Gompel JJ, Bower MR, Worrell GA, Stead M, Meier TR, Goerss SJ, Chang SY, Kim I, Meyer FB, Richard Marsh W, Marsh MP, Lee KH. Swine model for translational research of invasive intracranial monitoring. Epilepsia. 2011;52:e49–53. doi: 10.1111/j.1528-1167.2011.03096.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vingerhoets G, van der Linden C, Lannoo E, Vandewalle V, Caemaert J, Wolters M, Van den Abbeele D. Cognitive outcome after unilateral pallidal stimulation in Parkinson’s disease. Journal of neurology, neurosurgery, and psychiatry. 1999;66:297–304. doi: 10.1136/jnnp.66.3.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitek JL. Deep brain stimulation for Parkinson’s disease. A critical re-evaluation of STN versus GPi DBS. Stereotactic and functional neurosurgery. 2002a;78:119–131. doi: 10.1159/000068959. [DOI] [PubMed] [Google Scholar]
- Vitek JL. Mechanisms of deep brain stimulation: excitation or inhibition. Movement disorders : official journal of the Movement Disorder Society. 2002b;17(Suppl 3):S69–72. doi: 10.1002/mds.10144. [DOI] [PubMed] [Google Scholar]
- Voon V, Kubu C, Krack P, Houeto JL, Troster AI. Deep brain stimulation: neuropsychological and neuropsychiatric issues. Movement disorders : official journal of the Movement Disorder Society. 2006;21(Suppl 14):S305–327. doi: 10.1002/mds.20963. [DOI] [PubMed] [Google Scholar]
- Wakeman DR, Crain AM, Snyder EY. Large animal models are critical for rationally advancing regenerative therapies. Regenerative medicine. 2006;1:405–413. doi: 10.2217/17460751.1.4.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver FM, Follett KA, Stern M, Luo P, Harris CL, Hur K, Marks WJ, Jr, Rothlind J, Sagher O, Moy C, Pahwa R, Burchiel K, Hogarth P, Lai EC, Duda JE, Holloway K, Samii A, Horn S, Bronstein JM, Stoner G, Starr PA, Simpson R, Baltuch G, De Salles A, Huang GD, Reda DJ. Randomized trial of deep brain stimulation for Parkinson disease: Thirty-six-month outcomes. Neurology. 2012;79:55–65. doi: 10.1212/WNL.0b013e31825dcdc1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witt K, Daniels C, Reiff J, Krack P, Volkmann J, Pinsker MO, Krause M, Tronnier V, Kloss M, Schnitzler A, Wojtecki L, Botzel K, Danek A, Hilker R, Sturm V, Kupsch A, Karner E, Deuschl G. Neuropsychological and psychiatric changes after deep brain stimulation for Parkinson’s disease: a randomised, multicentre study. Lancet neurology. 2008;7:605–614. doi: 10.1016/S1474-4422(08)70114-5. [DOI] [PubMed] [Google Scholar]
- Wu YR, Levy R, Ashby P, Tasker RR, Dostrovsky JO. Does stimulation of the GPi control dyskinesia by activating inhibitory axons? Movement disorders : official journal of the Movement Disorder Society. 2001;16:208–216. doi: 10.1002/mds.1046. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.