Abstract
Medication adherence is critical to the efficacy of available treatment for depression in primary care settings. This review identifies factors associated with adherence and what is known about the effectiveness of adherence-enhancement programmes. A comprehensive systematic review of English language publications from January 2002 to October 2011 was conducted using the following databases: PUBMED/MEDLINE, PsycINFO and the Cochrane database. Twenty-one studies met the inclusion criteria for adherence-enhancement evaluations. Eleven of the studies evaluated demonstrated significantly positive effects on adherence; the remaining 10 reported mixed or no effects. Similar to previous literature reviews, factors shown to be associated with adherence were multifactorial and in this analysis were grouped as patient, condition and comorbidities, therapy or treatment, patient–provider relationship and healthcare system level. Adherence improved most notably in studies that included sustainable system and patient-targeted changes. Evaluating adherence-enhancement interventions is key to promoting successful approaches; however, a number of gaps exist between intervention and implementation: (1) the cost in resources and time to implement and sustain these programmes is unknown, (2) specific details about which subgroups of patients are best helped with such programmes is not clear, and (3) what specific processes or content are critical to programme success is still to be identified. There are sufficient data supporting the substantial need for planning and implementing adherence interventions despite reported mixed results. Primary care providers are often positioned to impact patients' adherence; however, practice constraints can limit their implementation.
Keywords: adherence-enhancement programmes, antidepressant adherence/non-adherence, associated factors
Introduction
Antidepressants are a standard approach to treating primary care patients in the acute phase of depression. With over 20 antidepressant medications (ADMs) currently available worldwide, these medications can, singularly or in combination with other antidepressants, bring relief to many suffering the disabling effects of depression. However, reported levels of non-adherence have been consistently high and this remains a serious concern.1–3 Patients who only partially follow or discontinue their antidepressant regimen for any reason have been found to act without physician consultation.4 This failure to follow medical advice has resulted in suboptimal treatment, risk of relapse and poor quality of life. More common than full discontinuation, partial non-adherence can also be detrimental to efficacious treatment, but not always resulting in ill effects.5
The World Health Organization (WHO) defines adherence as ‘the extent to which a person's behaviour – taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider’.6
The desired outcome of adherence is a therapeutic result based upon patient–provider agreed upon treatment goals and medical approach (referred to as concordance). Concordance implies a partnership between patient and provider with shared decision making.7,8 Adherence refers to patients taking their medications as prescribed with respect to timing, dosage and frequency. Finally, the term persistence is the extent to which patients continue to take a prescribed medication to achieve therapeutic outcomes. Thus, adherence or compliance refers to the intensity of drug use during the duration of therapy, whereas persistence refers to the overall duration of drug therapy.8,9
Many factors have been examined for their association with adherence/non-adherence and are generally grouped in categories. The WHO has categorised these factors into five broad groupings: patient, condition, therapy, socioeconomic and health system related.6 The purpose of this review is twofold: (1) to summarise studies examining factors associated with adherence/non-adherence to ADMs, and (2) to determine the state of the science regarding the impact of intervention-enhancement programmes.
Previous literature reviews on the treatment of depression in primary care settings have been informative, but not always helpful. Earlier reviews might not be depression specific, e.g. those that included affective disorders as a whole.10,11 Further, isolating key strategies that seemed to be successful was not always easy when analysing study reports. This was a problem early on in the ADM adherence literature. Pampallona and colleagues12 summarised the early literature to say that although patient education and medication clinics were most commonly tested for their impact on adherence, studies did not show consistent indications of which specific interventions were associated with adherence and would be effective if targeted in adherence-enhancement programmes.
More recent reviews on ADM adherence explored the effectiveness of multifaceted adherence-enhancement programmes with careful attention to what appeared to be the components of successful multifaceted programmes. Williams et al13 reported on programmes in the literature from 1966 to February 2006. These authors concluded that there was strong support for short-term care-management programmes; however, to be successful, these programmes required either staff reassignment or additional resources that were not always available. A more recent review by Chong and colleagues14 examined ADM adherence intervention choosing only randomised controlled trials (RCTs). Of the 28 programmes identified, only 16 (57%) reported better adherence. Although RCT studies promise high quality, relying only on RCTs may restrict data otherwise available. Our review includes RCTs but also pilot studies, intervention trials and quasi-experimental designs. Additionally, unlike previous reviews, we used the WHO categories of reasons for non-adherence to organise our discussion of factors associated with adherence.
Methods
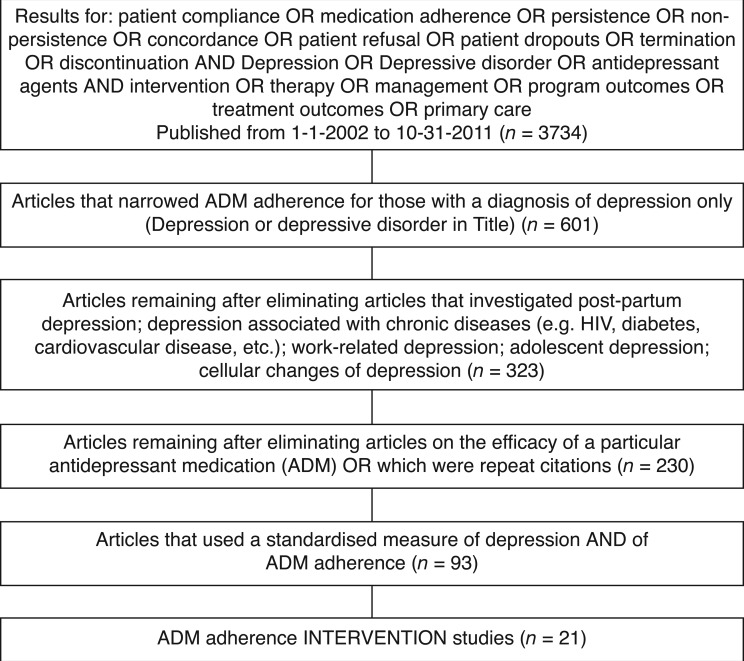
A comprehensive literature review was conducted using PUBMED/MEDLINE, PsycINFO and the Cochrane electronic database. The search was limited to English language articles published in peer-reviewed journals between January 2002 and October 2011. Keywords were: ‘Medication adherence or non-compliance or patient compliance or medication compliance or treatment refusal or dropout’ and ‘depression or depressive’. Recognising the growing importance of the concept of ‘concordance’, we expanded the initial review to include this term. We also included articles listed in authors' reference lists and those listed in other systematic reviews. Two researchers scanned the retrieved studies using both title and abstract, refining the list by eliminating irrelevant studies and duplications. Full articles were reviewed on those studies deemed relevant and screened on inclusion criteria. Both researchers evaluated included and excluded studies on the basis of relevancy and resolved differences of opinion by extensive discussions if needed.
Inclusion criteria
The following inclusion criteria for selecting studies were used: (1) of varying methodologies (case reports, clinical trials (I–V), comparative studies, controlled clinical trials and randomised controlled trials); (2) must target adult patients, 18 years and older with primary diagnoses of depression (unipolar or major depressive disorder), excluding those with bipolar, personality and psychotic disorders; (3) diagnosis of depression must be made on the basis of a standard measure of occurrence or severity (e.g. DSM-IV criteria, Hopkins' Symptom Checklist, Beck Depression Inventory, PHQ-9); (4) must include patients currently prescribed or starting on at least one antidepressant; (5) the outcome measure, adherence, should be defined by one or more standard methods of calculating adherence level (e.g. pharmacy refill data, pill count, electronic refill data record); and (6) assessed potential predictors of ADM adherence. The process of selecting studies meeting criteria for inclusion is described in Figure 1.
Figure 1.
Review of multimodal intervention research to promote ADM adherence
Results
We used the WHO categories to organise our discussion of factors with the exception of creating a new category, patient–provider relationship, and subsuming socioeconomic factors under patient level factors. We examined the following categories of reasons for non-adherence: (1) patient, (2) condition and comorbidities, (3) therapy or treatment, (4) patient–provider relationship and (5) health system level.
Patient factors
Patients' perceptions of ADMs have been associated with adherence and persistence in a number of ADM adherence studies. In a prospective naturalistic cohort study of 269 patients with a new diagnosis of depression, patients with negative attitudes about ADMs at entry tended to terminate ADMs in the acute phase more often than patients with positive or neutral attitudes.15 However, this finding was only marginally significant. Those with negative attitudes at 18 months also reported more non-adherence than patients with positive or neutral attitudes.
In a prospective cohort study examining the impact of patients' ADM concerns, treatment preferences and perceptions of their illness only 19% of the initial 147 participants completed their 6-month therapy.16 Concerns about ADM side-effects and general worry about taking antidepressants were independent predictors of antidepressant non-adherence. Preference for different treatment/uncertainty about preferred treatment was also a strong predictor.
Patient scepticism at baseline predicted discontinuance of ADMs in a prospective naturalistic evaluation of the clinical response to SSRIs of 573 patients with depression.17 In a separate, but related, study reporting attitudes of 81 primary care patients in the maintenance phase of antidepressant therapy, perceptions of harmfulness relative to the perceived necessity of taking ADMs was associated with adherence.18
In a multivariate context, beliefs, in combination with other patient characteristics, were found to be significant for various kinds of adherence behaviours. Positive ADM attitudes emerged as the most important factor for correct intake; whereas, those with a negative drug attitude or those who reported no social support were more likely to take a drug holiday.19 Finally, the role of patient social support, attitudes and adherence appeared complex. Whereas a 6-month prospective cohort study established that drug holidays were predicted by less social support and negative drug attitudes,20 another study examined the complexity of perceived locus of control in relationship to social support and adherence. In this study, greater social support was associated with greater adherence only among patients with a high locus of control.21 Familismo (family) was reported to assert strong influence among Latinos on ADM adherence either positively or negatively depending on family views of depression.22
Patient demographic characteristics associated with adherence were explored less often and included age, gender, ethnicity and educational level. In a latent class analysis of 228 enrolled participants, ethnicity and marital status were associated with adherence behaviours.23 There were no associations between age, gender, education level, depression status, cognitive status or medical comorbidity and class of adherence.
Patient condition and comorbidity factors
Patient physiological and psychological conditions along with other medical comorbidities can cause non-adherence to ADMs. This is particularly the case if severity of symptoms or other conditions significantly impact cognitive status. In a 12-month observational study of 192 family practice patients, severity of depressive symptoms and specific concerns about ADMs were the only variables associated with self-reported medication adherence; however, these variables explained only 13% of the variance in adherence behaviours, suggesting that other unaccounted for factors are more important.24
Alcohol or substance abuse, and comorbid conditions (cardiovascular/metabolic conditions) were explored in a retrospective observational study of 4312 patients continuously enrolled in a large health plan.1 Comorbid alcohol or substance abuse, comorbid cardiovascular/metabolic conditions, use of older generation ADMs, younger age and residence in low-income residential areas were associated with lower acute-phase ADM adherence.
Patient–provider relationship
Numerous studies examined aspects of the patient–provider relationship or collaboration with the health-care provider team. In a retrospective observational study of over 4000 patients continuously enrolled in a major health plan, patients were more likely to be adherent if they were seen by a psychiatrist during the 16-week observational period. Shared decision making appeared important in a cross-sectional study of 241 general practitioner (GP) patients.25 In a 12-month observational study of the impact of better communication and education (flow sheet supported by physician instruction, patient education and diligent follow-up), adherence was found to be improved. Of the 61 patients enrolled, 66% were adherent for at least 9 months.
The patient–physician partnership was shown to be associated with antidepressant concerns.16 Preference for different treatment and uncertainty about preferred treatment was a strong predictor of adherence. Otherwise, a mismatch between patients' preferred and physician prescribed treatment can serve as a significant barrier to ongoing adherence.
Therapy or treatment
The most commonly studied factors in this group were side-effect profiles and treatment complexity. ADMs class and their potential for side-effects were explored either independently or in conjunction with other variables.24–27 Some studies focused primarily on medication use and medication side effects. Previous use of ADMs was found to be a potential predictor in a large study of 211 565 out-patients.28 Median time to discontinuance in those who had not previously been dispensed an ADM was 67 days compared with 184 days in those who had a history of ADM use. Those who lacked a history of ADM use were more likely to discontinue ADMs in the first 30 days of treatment.
Specific side effects were examined for their relationship to non-adherence in a descriptive study of both inpatients (n = 198) and outpatients (n = 208).26 One in four patients discontinued their index ADM. Experiencing one or more ‘extremely bother-some’ side-effects more than doubled the risk of discontinuation.
Healthcare system level
The healthcare system category includes a broad range of factors impacting access to care and quality of care, e.g. extending care options, outreach, co-ordination of care and continuity of care. These factors have been shown to have either positive or no effects upon adherence. For example, the inclusion of pharmacists to enhance adherence outcomes was shown not to significantly impact adherence in primary care settings.29 This programme included three pharmacist contacts which took the form of selected educational messages about ADMs and a take-home educational video on depression, treatment and the importance of adherence. While this study indicated that there were no associations between adding a pharmacist to the treatment team, a pharmacist-guided education and monitoring programme (PGEM) did have a positive effect on adherence behaviours.30
Other studies found significant positive effects with the use of primary care-based interventions or collaborative care models. Lin31 and Ludman32 reported the effect of a primary care-based intervention on processes and outcomes (n = 386). The programme was multifaceted incorporating evidence-based practice for relapse prevention and cognitive-behavioural and motivational interviewing strategies. Depression relapse specialists received a 60-paged training manual and participated in two half-day training sessions with a psychiatrist. In sum, the organisation of health systems such as when usual care practices are supplemented or extended might have an impact on adherence.
In summary, the studies reviewed reported a number of potential reasons for adherence and non-adherence across five categories. Several important factors emerged and included patient factors, patient-provider relationship and healthcare system. However, conclusions about reasons for non-adherence are limited by significant study methodological differences. The most obvious differences include the wide variation in how depression and ADM adherence were defined and measured. For example, measures of depression included the PRIME-MD for DSM-IV symptoms. However, other studies used the simple prescription of an ADM or a diagnosis of depressive symptoms with a new prescription of an ADM as a measure of depression. The same level of variability was found in measures of ADM adherence. The most frequently used approach was patient self-report (interview or questionnaire), either as the only measure or in conjunction with other measures such as pharmacy refill records, pill count, MEMS and/or clinician rating.
Studies examining the effectiveness of adherence-enhancement programmes
Our second objective was to examine the effectiveness of adherence-enhancement programmes. It would logically follow that reasons for ADM adherence/non-adherence would inform programmes about directions for designing and implementing adherence-enhancement programmes. In the review of literature spanning January 2002 to October 2011, 21 studies were identified and tabled as those showing positive effects (Table 1) and those showing mixed or no effects (Table 2). The studies were not restricted to RCTs; nor were they required to report clinical outcomes. They could include pilot, pre-liminary or quality improvement studies, intervention trials or quasi-experimental designs.
Table 1.
Literature review: adherence-enhancement programmes with positive effects, beginning with the most recent (n = 11)
| Intervention | Author (year) [country] | Study design | Types of medication | Population/sample characteristics | Measures of adherence outcomes | Main findings for changes in adherence and/or depression |
|---|---|---|---|---|---|---|
| Online care management messaging follow-up programme | Simon et al (2011)39 [USA] | RCT pilot study | ADM categories not reported | 208 patients starting ADM, recruited from clinics using the Epic Electronic Medical Record System Intervention group = 106 Usual care = 102 |
Prescription refill data assessing total days dispensed and receipt of second antidepressant, indicating medication switch or combination |
Adherence: intervention patients had higher rates of adherence after 3 months Symptom severity: lower SCL scores after 5 months Satisfaction with treatment: greater satisfaction with treatment |
| Improve health e-Health intervention (improve.eu.) e-Health service to support collaborative depression care | Meglic et al (2010)37 [Slovenia] | Pilot study | ADM categories not reported | Pilot of 46 patients enrolled by seven physicians Intervention group = 21 Usual care = 25 |
Self-report questionnaire |
Adherence: in the control group, 3 of 9 patients were adherent to ADMs compared with 10 of 12 in the intervention group Symptom severity: significant within-group reduction in BDI II score fromtime 0 to time 1 Patient perceptions of care: no significant differences in perception of care accessibility or quality |
| Psychosocial intervention Treatment Initiation and Participation programme (TIP) |
Sirey et al (2010)42 [USA] | RCT pilot study | ADM categories not reported | 70 patients from geriatric and mixed aged primary care site Intervention group = 33 Usual care = 37 |
Self-report (medication and non-medication treatment compliance data form) with chart verification |
Adherence: TIP patients significantly more adherent at 6, 12 and 24 weeks Depressive symptoms: greater crease in depressive symptoms |
| Primary care practice-based healthcare assistant case management programme | Gensichen et al(2009)38 [Germany] | Clustered RCT | ADM categories not reported | 626 patients in small primary care practices, stratified by urban and rural practices Intervention group = 310 Usual care = 316 |
Patient self-report modified Morisky Adherence Scale |
Adherence: increased treatment adherence Symptom severity: lower mean scores on PHQ 9 values for depression symptoms Patient assessments of care: more favourable |
| Depression treatment intervention to reduce negative beliefs about antidepressants | Edlund et al (2008)36 [USA] | RCT | ADM categories not reported | 395 primary care patients in VA healthcare system Intervention group = 177 Usual care = 218 |
Self-report and electronic record monitoring whether > 80% dosages taken in prior month |
Adherence: beliefs generally not associated with taking medication. Summary measure of beliefs did predict initiating and adhering to ADMs Clinical response: not associated with clinical response Beliefs about ADMs: few effects on beliefs and were not in expected direction |
| Telemedicine-based collaborative care model | Fortney et al (2007)28 [USA] | Randomised intervention trial | ADM categories not reported | 395 primary care patients with PHQ 9 depression severity scores, 12 followed for 12 months Intervention group = 117 Usual care = 218 |
Self-report and pharmacy data, 80% prescriptions taken as prescribed in previous month at 6 and 12 months |
Adherence: intervention patients more likely to be adherent at both 6 and 12 months Respond/remit: intervention patients more likely to respond by 6 months and remit by 12 months |
| Depression disease self-management programme | Aubert et al (2003)34 [USA] | Longitudinal cohort observational study | ADM categories not reported | Members with new or recurrent episode of depression Three groups: Intervention = 505 Control = 3744 (Minimal intervention = 1375) |
Pharmacy claims data where acute phase adherence was a minimum of 84 days on therapy in a 114-day period; continuation phase adherence was 180 days of therapy in 231-day period |
Adherence: significantly more likely to adhere during acute phase and continuation phase. Also more likely refill prescription on more timely basis Therapy continuation: more likely to continue psychotherapy after 7 months Satisfaction with programme: over 90% felt mailings helpful, 98.7% calls helped answer questions, 81.7% helped take medications as recommended |
| Pharmacist collaborative care model | Finley et al (2002)35 [USA] | Intervention trial | Start or maintenance dose of fluoxetine, paroxetine, or other antidepressant | Cohort of primary care providers asked to refer patients to staffmodel HMO immediately after starting ADM Intervention group = 91 Control group = 129 |
Computerised prescription refill data |
Adherence: intent to treat analysis showed adherence significantly higher in intervention group Primary care provider visits: greater decline of primary care provider visits for intervention patients |
| Mail-based physician and HMO member educational intervention | Hoffman et al (2003)40 [USA] | Randomised controlled prospective design | Drug categories: SSRIs, TCAs and atypical agents | 9564 patients from a large IPA-model HMO newly enrolled and 7021 physicians included with cohort Intervention arm = 4899 patients and 3474 physicians Control group = 4665 patients and 3547 physicians |
Medication possession relative to refill data as specified by HEDIS | Adherence: significantly greater adherence at 90 and 180 days |
| Biopsychosocial intervention on depression relapse and antidepressant adherence/primary care-based depression programme | Lin et al (2003)31 [USA] Ludman et al (2003)32 [USA] |
Randomised intervention trial | ADM categories not fully reported (fluoxetine used with some patients) | 386 enrolled primary care patients at high risk for depression relapse from four large primary care clinics of group health cooperative Intervention group = 194 Control group = 192 |
Self-report data correlated highly with automated pharmacy refill records |
Adherence: increased favourable attitudes to ADM treatment and confidence in managing ADM side-effects, which were found to be significant predictors of adherence to maintenance pharmacotherapy Self-efficacy/managing depression: increased confidence in managing side-effects, depressive symptom monitoring, checking for early warning signs, and ‘planful coping’ at 3, 6, 9 and 12 months |
| Innovative approach through monitoring HEDIS standards | Roberts et al (2002)41 [USA] | Quality improvement multiphase design | ADM categories not reported | Members of major HMO with potential valid depression diagnosis Confirmed cohort of 6045 patients No control group |
% who received continuous trial of ADMs for 84 days (12 weeks) and no more than a 30-day gap allowed | Adherence: within the first year ADM compliance rates improved by more than 10% |
Table 2.
Literature review: adherence-enhancement programmes with mixed or no effects, beginning with the most recent (n = 10)
| Intervention | Author (year) [country] | Study design | Types of medication | Population/sample characteristics | Measures of adherence outcomes | Main findings for changes in adherence and/or depression |
|---|---|---|---|---|---|---|
| Pharmacy based intervention to improve adherence | Bosmans et al (2007)29 [The Netherlands] | RCT | Non-tricyclic ADMs | 151 adult primary care patients treated with new prescription for a non-tricyclic ADM Education and coaching by the pharmacist group = 70 Usual care = 81 |
Electronic pill container (eDEM); records of precise time container opened |
Adherence: no significant differences at 6 months Depressive symptoms: no significant improvements in the SCL depression mean item score Costs: no significant differences over 6 months |
| Depression education for primary care patients and providers | Azocar and Branstrom (2006)33 [Australia] | Experimental cohort design | ADM categories not reported | State employees or spouses recruited receiving first ADM Intervention group = 460 Control group = 512 |
Pharmacy claims data: how consistently medications refilled over 1 year with acute phase the first 6 months and continuance phase the second 6-month period |
Adherence: consistency of ADM use over 12 months was not significantly different between groups; the intervention group had fewer gaps in coverage between prescriptions and gaps were shorter Psychotherapy and combination treatment: significant increase in the use of therapy; neither had hospitalisations during the 12-month study period Duration of treatment and therapies: those in the second full course of ADM therapy and psychotherapy were more likely to receive the full course of therapy |
| Community pharmacists manage depression | Crockett et al (2006)45 [Australia] | Parallel groups design with intervention and control groups | ADM categories not reported | 106 patients recruited by 32 community pharmacists in rural and remote areas of New South Wales, Australia Intervention group = 46 Control group = 60 |
Persistence in taking medications at 1 and 2 months |
Adherence: high in both groups; no between-group differences, still taking medication at 1 or 2 months Well-being: improvement in well-being in both groups Drug attitudes: improvement in attitudes in both groups with no significant differences between groups |
| Pharmacist-guided education and monitoring programme (PGEM) | Rickles et al (2005)30 [USA] | Randomised control unblinded, mixed experimental design | ADM categories not reported | 63 patients presenting for new ADM prescription at their community pharmacies Intervention group = 28 Usual care = 32 |
Pharmacy refill data missed doses per day by number of days late between refills and multiplying by 100 for % missed doses |
Adherence: no significant group differences. PGEM patients missed fewer doses than the usual care group at 6 months Patient knowledge/beliefs: PGEM significant and positive effect on patient feedback, knowledge, medication beliefs and perceptions of progress Symptoms: no significant difference in symptoms observed at 3 months |
| Pharmacist interventions to improve depression care and outcomes in primary care | Capoccia et al (2004)44 [USA] | Intervention trial | ADM categories not reported | Primary care patients with new episode of depression and started on ADM Intervention group = 41 Control group = 33 |
Self-report, number days took medication in past month |
Adherence: no significant differences between groups at 3, 6, 9 or 12 months Symptoms and quality-of-life: no significant differences in depressive symptoms or quality of life Patient satisfaction and number of provider visits: no significant differences |
| Remote treatment of depression through tele-psychiatry | Ruskin et al (2004)48 [USA] | RCT | ADM categories not reported | Interested patients referred from outpatient VA mental health clinics Intervention remote group = 59 In-person group = 60 |
Pill count; those who took at least 70% of their medications were deemed adherent |
Adherence: no difference in percentage of patients adherent Patient satisfaction with programme: no difference in satisfaction at visits at 4, 6 or 8 months. Satisfaction with psychiatrist higher in patients treated in person Resource consumption/cost: estimated marginal costs to institution higher with remote programme; however, when cost of psychiatrist travel factored in for remote patients, costs were equal |
| Depression care programme (including education, social support and homework assignments) OPtimind | Vergouwen et al (2005)51 [The Netherlands] | RCT | Selective serotonin reuptake inhibitors | 30 GPs and 211 patients randomised Intervention group = 101 Systematic follow-up group = 110 |
Adherence evaluated at 2, 6, 10, 14, 18, 22 and 26 weeks with pill count | Adherence: no significant differences in adherence at week 10 or week 26 |
| Educational compliance enhancement programme using (RHYTHMS) by Pfizer Pharmaceuticals and managed by GP | Akerblad et al (2003)49 [Sweden] | Randomised controlled design | Sertraline treatment | Patients on sertaline therapy were recruited through mail to GPs Intervention group = 326 Control group = 339 |
Based upon four approaches: 1. Questions at visits at 4, 12 and 24 weeks 2. Measurable serum levels 3. Appointments kept at 4, 12 and 24 weeks 4. Composite index (items 1–3) |
Adherence: no significant between-group differences Remission rates: significantly more patients in intervention group responded at 24 weeks |
| Telephone disease management programme | Datto et al (2003)47 [USA] | Intervention pilot | ADM categories not reported | 35 primary care practices in university health system Intervention group = 78 Control group = 123 |
Assessed as single measure: follow clinician treatment recommendations with respect to initiating treatment, taking medications and increasing doses as recommended |
Adherence: no significant effect on improving patient adherence to clinician recommendations. Intervention patients improved significantly more over time Depression symptoms: both groups showed significant changes in CES D scale scores |
| Information and ongoing interactive programme (RHYTHMS) by Pfizer Pharmaceuticals | Kutcher et al (2002)50 [USA] | Randomised blinded, parallel group, controlled trial | Sertraline treatment | 269 primary care patients from five Canadian maritime provinces receiving sertraline therapy Intervention group = 85 Non-intervention group = 79 |
Pill count: proportion of pills not returned and presumed taken to pills dispensed (PNR/PD) |
Adherence: no significant between-group differences Remission rates: no significant differences in remission rates, or mean Hamilton Depression Rating Scale scores Satisfaction with treatment: greater satisfaction with information and treatment received |
Data extraction and analysis
Data extracted from each study reviewed included: adherence intervention identified, author and date, as well as country where the study was conducted, setting/population/sample, type of ADM, measure of adherence, study findings of changes in adherence and/or treatment satisfaction and clinical outcomes.
Procedures to table adherence-enhancement studies included grouping articles where possible when studies originated from a certain category (e.g. pharmacist interventions) or by widely known intervention (e.g. TIPS, STAR-D* or RHYTHMS). This enabled us to present key studies by category making it more meaningful for readers to follow evaluations of programmes over time by the same or similar research teams. Studies reporting positive results are presented, followed by those with mixed or no significant effects.
Results
Studies reporting positive effects
Eleven of the 21 studies reviewed showed significantly positive effects on adherence. Rarely is the provision of education materials alone productive in promoting adherence. However, Azocar and Branstrom,33 using an experimental cohort study design, did find a moderate impact on consistency of ADM use and on the use of psychotherapy in combination with ADMs. Educational flyers were mailed to participants following prescription of an ADM and their corresponding treating physicians were alerted to the study. The intervention group had fewer gaps in ADM coverage between prescriptions and these gaps were shorter over the 12-month study period.
Multiple pharmacy based intervention studies were found in the literature, with several showing positive effects. Using a longitudinal cohort observation study, Aubert and colleagues34 evaluated the impact of a pharmacy benefit management programme.
Programme patients received three additional nurse-delivered telephone counselling calls and five educational mailings. Intervention patients were significantly more likely to adhere in either the acute or continuation phases. Using a pharmacist collaborative care model, Finley35 conducted an intervention trial to examine the effect of a collaborative pharmacy practice model among patients after starting a dose of fluoxetine, paroxetine or other ADM in a large health maintenance organisation (HMO). The cohort of primary care providers was asked to refer patients to the staff-model HMO immediately after starting ADMs. They found slightly higher rates of adherence.
Significant positive effects on adherence were found with the use of primary care-based interventions or collaborative care models. In reports stemming from a study by Lin31 and Ludman,32 386 patients at high risk for relapse were randomly assigned to the care as usual or intervention trial. Participants engaged in specialty trained staff enhanced self-management behaviours such as monitoring depression symptoms and scheduling pleasant activities. They were significantly more likely to refill ADM prescriptions and to receive adequate ADM dosages compared to controls during the 1-year follow-up.
Edlund and colleagues36 reported that patients in a telemedicine-based collaborative care model were twice as likely to be adherent at both 6 and 12 months, more likely to respond by 6 months and remit by 12 months. The intervention included initial encounters with a case manager with follow-up as needed. Researchers determined that the active intervention component was telephone-based supervised nurse case management. They concluded that outcomes can be modestly improved by implementing a nurse case-management system without elaborate and expensive interactive video equipment or reorganising care to duplicate a team-based environment.
Meglic and colleagues37 found initial positive effects with their pilot programme of e-Health to support collaborative depression care. This pilot study tested the impact of a web-based information and technology system, ‘the ICT system’, designed to support collaborative care management and patient engagement in their care. Active patient involvement was achieved through online and phone-based care management support performed by programme psychologists. Risks for non-adherence were identified automatically and included poor or missing treatment response, unwanted side-effects and ADM non-adherence. Care managers were available during service hours and email replies occurred within two working days. Participants reported feeling actively engaged and in control of their disease.
Finally, in an additional four studies evidence of improvements were shown.38–41 Gensichen et al.38 conducted a clustered RCT with patients in small primary care practices from rural and urban settings. This primary care case-management programme was reported to increase treatment adherence. In a most recent report of a pilot study, Simon and colleagues39 tested an online care management messaging follow-up programme using the Epic Electronic Medical System. Recognising the relative expense of telephone management in depression care, these researchers examined the impact of their programme on 208 patients in nine primary care clinics in an integrated health system. Each participant was given three online care management contacts with a trained psychiatric nurse. These contacts included a structured assessment (severity of depression, medication adherence, side-effects), algorithm-based feed-back to the patient and corresponding physician, and facilitation of follow-up care when needed. Significant improvements in adherence were observed after 3 months.
Hoffman et al.40 conducted a randomised prospective design in a major HMO by implementing a mail-based physician and patient educational intervention to improve adherence among patients newly prescribed ADMs. The programme not only educated both providers and patients, but also tracked adherence levels and informed both patients and physicians when adherence dipped. Alerting patients and providers simultaneously was felt to have a stronger impact on patient–provider interaction.
Finally, Roberts41 led a team to evaluate the effectiveness of a depression management programme within a major HMO using HEDIS standards. Intervention patients participated in a four-phase programme to ensure proper diagnosis and monitor a full course of treatment. With only the first 6 months of data available, a significant increase in adherence measured by the percentage of patients in a continuous trial of ADMs for a minimum of 12 weeks was demonstrated.
In conclusion, slightly over half of the studies found reported positive effects on adherence. In four of the studies reporting positive effects significant reductions in depressive symptomatology or respond and remit rates were also favourable.28,37–39,42
Studies reporting mixed or no effects
While 11 of the 21 studies reported positive effects, the remaining 10 reported mixed or no effects. In a randomised controlled pilot study, Sirey and colleagues42 tested the impact of a psychosocial intervention to improve depression in a sample of geriatric and mixed age primary care patients prescribed ADMs by their primary care provider. The extensively structured programme, the Treatment Initiation and Participation (TIP), consisted of a brief intervention of three initial meetings during the first 6 weeks, followed by two telephone calls at 8 and 10 weeks. The researchers emphasised the aspect of a patient–TIP counsellor alliance to work together on barriers to adherence. The content of the intervention included information about depression and treatment, barriers to adherence, defining a personal goal that could be achieved with adherence, importance of collaboration to address barriers, and empowering patients to have direct communication with the primary care provider about the treatment. A ‘contact list’ that listed barriers served to organise sessions and record interventions administered.
Of equal attention to detail and what accounted for half the studies reporting mixed or no effects were those examining the impact of pharmacist intervention models. Rickles et al.30 in a study of a PGEM reported no significant group differences in adherence, but at 6 months PGEM patients missed fewer doses than usual care patients. In an RCT conducted by van Dulmen et al.43 to test the effects of a pharmacy based intervention in a primary care setting, no significant differences in adherence were found at 6 months. No significant between-group differences were reported in a trial conducted by Capoccia et al.44 This programme was designed as a pharmacist intervention to improve both depression care and outcomes in primary care. No differences were found in patients' self-reports of the number of medications in the past month, at 3, 6, 9 or 12 months.
In an extensive study by Crockett et al,45 patients were recruited from 32 community pharmacies in both rural and remote areas of New South Wales, Australia. Patients along with their corresponding local pharmacists who were trained on the nature and management of depression were paired to receive education about depression management. Participating pharmacists were given videoconference training by a psychiatrist, psychologist and GP and asked to dispense antidepressants with extra advice and support from the programme. Differences between groups did not emerge because adherence was high in both treatment and control patients. Also, both groups improved significantly in terms of well-being; no significant change was detected in attitude toward ADMs.
Finally, a pharmacist intervention to improve adherence was tested by Bosmans et al.46 No significant differences were shown at 6 months. These researchers wanted to create a minimal intervention that was easy to implement without too much interruption in the pharmacist's daily routine, but suggested that the intervention might not have been sufficiently intense to establish change differences.
The following studies reported on programmes aiming to control costs and retain effectiveness. Datto et al.47 conducted a pilot study using a telephone disease-management programme (TDM) with patients in the acute phase of depression recruited from 35 separate primary care practices in a university health system. All patients received baseline and 16-month follow-up telephone calls; however, the TDM group received calls every 3 weeks with formal evaluations at 6 and 12 weeks. Patient and clinician follow-up calls were designed to facilitate adherence to the Agency for Health Research and Quality (AHRQ) treatment algorithm. The improvement in depression was associated with clinician adherence to the algorithms; however, the TDM pilot programme did not show a significant effecton adherence improvement.
A telepsychiatry programme was compared with an in-person treatment of depression approach in a study reported by Ruskin and colleagues.48 The purpose was to judge the relative efficacy of tele-psychiatry over in-person treatment with remotely located veteran outpatients. Participants used personal computer-based videoconferencing which included eight 20-minute sessions with a psychiatrist over a 6-month period. These sessions addressed ADM management, psychoeducation and a brief supportive counselling. There were no between-group differences; these groups had equivalent levels of patient adherence, patient satisfaction and healthcare costs. The researchers stressed the ability to treat hard-to-reach patients remotely, thus expanding healthcare access without reducing patient satisfaction or patient ADM adherence.
Finally, in an additional three studies, no significant changes were observed. Akerblad49 and Kutcher50 reported separate information on an ongoing interactive programme with patients in primary care practices in five maritime provinces in Canada. The RHYTHMS programme by Pfizer pharmaceuticals was implemented and tested for its impact on adherence. Both researchers found no significant between-group differences in adherence.
Vergouwen51 conducted a randomised trial with patients receiving selective serotonin reuptake inhibitors (SSRIs; OPtimid#TM). Depression care included education, social support and homework assignments. There were no significant between-group differences in adherence either at 10 or 26 weeks. The depression care programme was shown not to be superior to the systematic follow-up programme.
Discussion
Despite a full range of effective ADM options, poor adherence to these regimens continues to threaten their therapeutic value. A substantial number of studies exploring potential reasons for ADM adherence/non-adherence were found in our initial review.
In keeping with other published reviews we also found evidence for the complexity of adherence and that the reasons for non-adherence are multifaceted. Several important factors surfaced. There was strong support for certain patient characteristics, namely patient beliefs, mistrust, fear of ADMs and adherence. Patient-held beliefs or fears of ADMs were found to be associated with non-adherence, particularly negative attitudes at entry,15 treatment preferences and perception of harmfulness of ADMs relative to perceived necessity16 and scepticism about ADM treatment.17 Quality patient-provider relationships and communications had a positive effect upon adherence behaviours, and the patient-provider partnership was central in exploring adherence concerns.16 Healthcare system level factors also surfaced as important and worthy of future research.
Our second objective was to update and evaluate the state of the science on adherence-enhancement programmes. Twenty-one articles reported on the effectiveness of ADM adherence-enhancement programmes and met our criteria. The number of studies having positive or no effects were split evenly. Programmes targeting patient, patient–provider and system factors were evident and a number were found to be effective. Being less restrictive than some previous reviews made it possible to evaluate the evidence of new approaches and technological supports to improve adherence37,39 that might not otherwise be included in a systematic review of RCTs only. Our evaluation of the adherence-enhancement programme literature indicated that, although there has been further progress, more needs to be known about what specific elements work most effectively, with which patient groups and at what costs. Seldom were these issues raised and addressed in sufficient detail. In only two programmes were data on costs analysed and reported.29,48 Yet, some researchers were specifically motivated to find effective methods at the same or lesser costs.
Taken as a whole, there was support for a complex interaction between patient-provider and system approaches. However, in keeping with Williams,13, these approaches might require a reconfiguration in patient-provider relationships with additional resources or role reassignments not always available in primary care or primary care-linked settings.
The role of concordance in achieving and maintaining adherence needs further study. However, concordance currently lacks measurability.7 Concordance levels change over time and can differ significantly in the acute, continuation and maintenance phases of depression treatment. As Garfield et al.52 noted, a symptom of depression is impaired decision making. This makes it improbable that all patients will be capable of shared decision making and at all times. Patients' preferences for involvement vary: ‘Healthcare professionals therefore need to create opportunities for identifying changes in preferences for involvement during the process, to enable them to form truly concordant relationships with their patients’ (p. 246).
Generalisations of these findings are bound by the criteria used to select studies. We focused on patients with depressive disorders. Articles directed at treatment of other psychiatric illnesses (e.g. schizophrenia, bipolar disorder, obsessive compulsive disorder (OCD), post-traumatic stress disorder (PTSD) and panic disorders) or medical illnesses (e.g. HIV/AIDS, diabetes, hypertension, chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), stroke and cardiac rehabilitation and cancers) were excluded. These exclusions limit the generalisability of our findings for other patient populations.
The results of this systematic review indicate some deficits in study designs not always addressed in evaluation studies. The lack of uniformity in measures of depression and adherence are important. Additionally, few studies seemed to be guided by explicitly stated theoretical frameworks. A number of frameworks address the process of treatment adherence in other chronic illnesses, e.g. cardiovascular and HIV/AIDS. There are adherence-enhancement programmes that are effective with or without theoretical models, but these theories need to be assessed more thoroughly for their ability to inform efficacious interventions.43
Conclusions
Primary care providers are often the first to identify depression and are the most likely to monitor patient's adherence to ADMs and the efficacy of drug treatment. Optimal treatment includes not only prescribing ADMs but monitoring, adjusting and if possible, implementing adherence-enhancement programmes.
Explorations of the impact of adherence-enhancement programmes are beginning to be reported, but more needs to be known. Of particular promise are programmes that address patient-provider relationships and care management systems that support medication adherence over time. Current research is not sufficient to support a particular programme for all patients, thus the need to be specific and precise about what works and with whom.
The design and evaluation of adherence-enhancement programmes should flow logically from the factors that are associated with reasons for nonadherence. The realities of research heterogeneity, study designs, purpose, populations studied, settings and adherence measurements might differ, raise the need for unity in measurement approaches and careful description of the active elements of enhancement programmes so that data across studies can be compared and insight into what works with whom can be better synthesised. While findings from RCTs provide important results, findings from intervention trials, quality improvement projects and evaluation studies provide a window to what is possible and might be worth further exploration particularly as they include new informational technology.
ACKNOWLEDGEMENTS
We thank Betsy S Hopkins, BS, MSL, Life Science Librarian, Harold B Lee Library for assisting in the literature search. Laura Boone, research assistant is acknowledged for her efforts in data retrieval.
Contributor Information
Gwen van Servellen, Professor Emerita, School of Nursing, University of California, Los Angeles and Visiting Professor, College of Nursing, Brigham Young University, Provo, UT, USA.
Barbara A Heise, Assistant Professor.
Robin Ellis, Research Assistant, College of Nursing, Brigham Young University, Provo, UT, USA.
REFERENCES
- 1.Akincigil A, Bowblis J, Levin C, Walkup J, Jan S, Crystal S. Adherence to antidepressant treatment among privately insured patients diagnosed with depression. Medical Care 2007;45(4):363–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cantrell CR, Eaddy MT, Shah MB, Regan TS, Sokol MC. Methods for evaluating patient adherence to antidepressant therapy: a real-world comparison of adherence and economic outcomes. Medical Care 2006;44(4):300–3 [DOI] [PubMed] [Google Scholar]
- 3.Demyttenaere K, Enzlin P, Dewe W, et al. Compliance with antidepressants in a primary care setting 1: beyond lack of efficacy and adverse events. Journal of Clinical Psychiatry 2001;62(22):30–3 [PubMed] [Google Scholar]
- 4.Sawada N, Uchida H, Suzuki T, et al. Persistence and compliance to antidepressant treatment in patients with depression: a chart review. BMC Psychiatry 2009;9–38 doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mitchell A. Understanding medication discontinuation in depression. Psychiatric Times 2007;34 Available at: www.lexisnexis.com/Inacui2api/delivery/PrintDoc.do?jobHandle=2825%3A31832 (accessed 16 November 2011). [Google Scholar]
- 6.World Health Organization Adherence to Long-Term Therapies: evidence for action. Geneva, Switzerland: World Health Organization, 2003 [Google Scholar]
- 7.De las Cuevas C. Towards a clarification of terminology in medicine taking behavior: compliance, adherence and concordance are related although different terms with different uses. Current Clinical Pharmacology 2011;6:74–7 [DOI] [PubMed] [Google Scholar]
- 8.Liu X, Chen Y, Faries DE. Adherence and persistence with branded antidepressants and generic SSRIs among managed care patients with major depressive disorder. Clinicoecononomics and Outcomes Research 2011;3:63–72 (Epub 15 March 2011) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: terminology and definitions. Value Health 2008;11(1):44–7 [DOI] [PubMed] [Google Scholar]
- 10.Lingam R, Scott J. Treatment non-adherence in affective disorders. Acta Psychiatrica Scandinavica 2002;105:164–72 [DOI] [PubMed] [Google Scholar]
- 11.Vergouwen AC, Bakker A, Katon WJ, Verheij TJ, Koerselman F. Improving adherence to antidepressants: a systematic review of interventions. Journal of Clinical Psychiatry 2003;64(12):1415–20 [DOI] [PubMed] [Google Scholar]
- 12.Pampallona S, Bollini P, Tibaldi G, et al. Patient adherence in the treatment of depression. British Journal of Psychiatry 2002;180:104–9 [DOI] [PubMed] [Google Scholar]
- 13.Williams JW, Jr, Gerrity M, Holsinger T, et al. Systematic review of multifaceted interventions to improve depression care. General Hospital Psychiatry 2007;29:91–116 [DOI] [PubMed] [Google Scholar]
- 14.Chong WW, Aslani P, Chen TF. Effectiveness of interventions to improve antidepressant medication adherence: a systematic review. International Journal of Clinical Practice 2011;65(9):954–75 [DOI] [PubMed] [Google Scholar]
- 15.Melartin TK, Rytsälä HJ, Leskelä US, et al. Continuity is the main challenge in treating major depressive disorder in psychiatric care. Journal of Clinical Psychiatry 2005;66(2):220–7 [DOI] [PubMed] [Google Scholar]
- 16.Hunot VM, Horne R, Leese MN, Churchill RC. A cohort study of adherence to antidepressants in primary care: the influence of antidepressant concerns and treatment preferences. Primary Care Companion Journal of Clinical Psychiatry 2007;9(2):91–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aikens JE, Kroenke K, Swindle RW, Eckert GJ. Nine-month predictors and outcomes of SSRI anti-depressant continuation in primary care. General Hospital Psychiatry 2005;27(4):467–77 [DOI] [PubMed] [Google Scholar]
- 18.Aikens JE, Nease DE, Nau DP, Klinklman MS, Schwenk TL. Adherence to maintenance-phase anti-depressant medication as a function of patient beliefs about medication. Annals of FamilyMedicine 2005;3(1):23–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brook O, van Hout H, Stalman W, de Haan M. Nontricyclic antidepressants: predictors of nonadherence. Journal of Clinical Psychopharmacology 2006;26(6):643–7 [DOI] [PubMed] [Google Scholar]
- 20.Brook OH, van Hout H, Stalman W, et al. A pharmacy-based coaching program to improve adherence to antidepressant treatment among primary care patients. Psychiatric Services 2005;56(4):487–9 [DOI] [PubMed] [Google Scholar]
- 21.Voils C, Steffens D, Flint E, Bosworth H. Social support and locus of control as predictors of adherence to antidepressant medication in an elderly populations. American Journal of Geriatric Psychiatry 2005;13(2):157–65 [DOI] [PubMed] [Google Scholar]
- 22.Interian A, Martinez I, Rios L, et al. Adaptation of a motivational interviewing intervention to improve antidepressant adherence among Latinos. Cultural Diversity in Mental Health 2010;16(2):215–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bogner HR, de Vries HF. Integration of depression and hypertension treatment: a pilot, randomized controlled trial. Annals of Family Medicine 2008;6(4):295–301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brown C, Battista D, Bruehlman R, Sereika S, Thase M, Dunbar-Jacob J. Beliefs about antidepressant medications in primary care patients: relationship to self-reported adherence. Medical Care 2005;43(12):1203–7 [DOI] [PubMed] [Google Scholar]
- 25.Byng R, Bury C, Weaver L. Patients' experiences of consultations for depression and predictors of adherence to antidepressants. Primary Care Community Psychiatry 2007;12(3):109–15 [Google Scholar]
- 26.Goethe J, Wooley S, Cardoni A, Woznicki B, Piez D. Selective serotonin reuptake inhibitor discontinuation: side effects and other factors that influence medication adherence. Journal of Clinical Psychopharmacology 2007;27(5):451–8 [DOI] [PubMed] [Google Scholar]
- 27.Melartin TK, Rytsälä HJ, Leskelä US, Lestelä-Mielonen PS, Sokero TP, Isometsä ET. Continuity is the main challenge in treating major depressive disorder in psychiatric care. Journal of Clinical Psychiatry 2005;66(2):220–7 [DOI] [PubMed] [Google Scholar]
- 28.Vanelli Fortney J, Pyne J, Edlund M, et al. A randomized trial of telemedicine-based collaborative care for depression. Journal of General Internal Medicine 2007;22:1086–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bosmans J, Brook O, van Hout H, et al. Cost effectiveness of a pharmacy-based coaching programme to improve adherence to antidepressants. Pharm-ocoEconomics 2007;25(1):25–37 [DOI] [PubMed] [Google Scholar]
- 30.Rickles NM, Svarstad BL, Statz-Paynter JL, Taylor LV, Kobak KA. Pharmacist telemonitoring of anti-depressant use: effects on pharmacist–patient collaboration. Journal of the American Pharmacists Association 2005;45(3):344–53 [DOI] [PubMed] [Google Scholar]
- 31.Lin E, Von Koreff M, Ludman EJ, et al. Enhancing adherence to prevent depression relapse in primary care. General Hospital Psychiatry 2003;25(5):303–10 [DOI] [PubMed] [Google Scholar]
- 32.Ludman E, Katon W, Bush T, et al. Behavioural factors associated with symptom outcomes in a primary care-based depression prevention intervention trial. Psychological Medicine 2003;33(6):1061–70 [DOI] [PubMed] [Google Scholar]
- 33.Azocar F, Branstrom RB. Use of depression education materials to improve treatment compliance of primary care patients. Journal of Behavioral Health Services and Research 2006;33(3):347–53 [DOI] [PubMed] [Google Scholar]
- 34.Aubert RE, Fulop G, Fang X, Thiel M, Maldonato D, Woo C. Evaluation of a depression health management program to improve outcomes in first and recurrent episodic depression. American Journal of Managed Care 2003;9(5):374–80 [PubMed] [Google Scholar]
- 35.Finley P, Rens H, Pont J, et al. Impact of collaborative pharmacy practice model on the treatment of depression in primary care. American Journal of Health-System Pharmacy 2002;59:1518–26 [DOI] [PubMed] [Google Scholar]
- 36.Edlund M, Fortney J, Reaves C, Pyne J, Mittal D. Beliefs about depression and depression treatment among depressed veterans. Medical Care 2008;46(6):581–9 [DOI] [PubMed] [Google Scholar]
- 37.Meglic M, Furlan M, Kuzmanic M, et al. Feasibility of an e-Health service to support collaborative depression care: results of a pilot study. Journal of Medical Internet Research 2010;12(5):e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gensichen J, von Korff M, Peitz M, et al. Case management for depression by health care assistants in small primary care practices: a cluster randomized trial. Annals of Internal Medicine 2009;151:369–78 [DOI] [PubMed] [Google Scholar]
- 39.Simon G, Ralston J, Savarino J, Pabiniak C, Wentzel C, Operskalski B. Randomized trial of depression follow-up care by online messaging. Journal of General Internal Medicine 2011;26(7):698–704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hoffman L, Enders J, Luo J, et al. Impact of an antidepressant management program on medication adherence. American Journal of Managed Care 2003;9(1):70–80 [PubMed] [Google Scholar]
- 41.Roberts K, Cockerham TR, Waugh WJ. An innovative approach to managing depression: focus on HEDIS standards. Journal for Healthcare Quality 2002;24:11–17 [DOI] [PubMed] [Google Scholar]
- 42.Sirey JA, Bruce ML, Kales HC. Improving anti-depressant adherence and depression outcomes in primary care: the treatment initiation and participation (TIP) program. American Journal of Geriatric Psychiatry 2010;18(6):554–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.van Dulmen S, Sluijs E, van Dijk L, de Ridder D, Heerdink R, Bensing J. Patient adherence to medical treatment: a review of reviews. BMC Health Services Research 2007;7(5):1–13 Available at: www.biomedcentral.com/1472–6963/7/55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Capoccia KL, Boudreau DM, Blough DK, et al. Randomized trial of pharmacist interventions to improve depression care and outcomes in primary care. American Journal of Health-System Pharmacy 2004;61:364–72 [DOI] [PubMed] [Google Scholar]
- 45.Crockett J, Taylor S, Grabham A, Standford P. Patient outcomes following an intervention involving community pharmacists in the management of depression. Australian Journal of Rural Health 2006;14:263–9 [DOI] [PubMed] [Google Scholar]
- 46.Bosmans Aikens JE, Kroenke K, Swindle RW, Eckert GJ. Nine-month predictors and outcomes of SSRI antidepressant continuation in primary care. General Hospital Psychiatry 2005;27(4):467–77 [DOI] [PubMed] [Google Scholar]
- 47.Datto CJ, Thompson R, Horowitz D, Disbot M, Oslin DW. The pilot study of a telephone disease management program for depression. General Hospital Psychiatry 2003;25:169–77 [DOI] [PubMed] [Google Scholar]
- 48.Ruskin P, Silver-Aylaian M, Kling M, et al. Treatment outcomes in depression: comparison of remote treatment through telepsychiatry to in-person treatment. American Journal of Psychiatry 2004;161:1471–6 [DOI] [PubMed] [Google Scholar]
- 49.Akerblad AC, Bengtsson F, Ekselius L, von Knorring L. Effects of an educational compliance enhancement programme and therapeutic drug monitoring on treatment adherence in depressed patients managed by general practitioners. International Clinical Psychopharmacology 2003;18:347–54 [DOI] [PubMed] [Google Scholar]
- 50.Kutcher S, Leblanc J, Maclaren C, Hadrava V. A randomized trial of a specific adherence enhancement program in sertraline-treated adults with major depressive disorder in a primary care setting. Progress in Neuro-Psychopharmacology and Biological Psychiatry 2002;26:591–6 [DOI] [PubMed] [Google Scholar]
- 51.Vergouwen A, Bakker A, Burger H, Verheij T, Koerselman F. A cluster randomized trial comparing two interventions to improve treatment of major depression in primary care. Psychological Medicine 2005;35:25–33 [DOI] [PubMed] [Google Scholar]
- 52.Garfield GS, Francis SA, Smith FJ. Building concordant relationships with patients starting antidepressant medication. Patient Educcation and Counseling 2004;55(2):241–6 [DOI] [PubMed] [Google Scholar]
CONFLICTS OF INTEREST
The authors report no financial or other relationships relevant to the subject.