Abstract
Dental disease is largely preventable. Many older adults, however, experience poor oral health.
National data for older adults show racial/ethnic and income disparities in untreated dental disease and oral health–related quality of life. Persons reporting poor versus good health also report lower oral health–related quality of life.
On the basis of these findings, suggested public health priorities include better integrating oral health into medical care, implementing community programs to promote healthy behaviors and improve access to preventive services, developing a comprehensive strategy to address the oral health needs of the homebound and long-term-care residents, and assessing the feasibility of ensuring a safety net that covers preventive and basic restorative services to eliminate pain and infection.
Oral health is vital to the general health and well-being of all Americans.1 The mouth reflects a person's health and well-being throughout life. Oral diseases can have an impact on many aspects of general health and health conditions can in turn have an impact on oral health. Oral and other diseases also share common risk factors. Because the risk of chronic conditions increases with age, it is important to examine the interplay of these diseases with oral disease, and their combined impact on overall health among older adults.
We describe the scope of the problem of dental and periodontal diseases among older adults and how they can profoundly diminish quality of life and have an adverse impact on general health. Next, we characterize the burden of oral diseases with current national data and published studies. Finally, we explore roles for the public health system in improving the oral health of older US adults. Although oral cancer disproportionately affects older adults and has a high burden,2 it is excluded because of space constraints.
POOR ORAL HEALTH AND QUALITY OF LIFE AND GENERAL HEALTH
Poor oral health can limit food choices and diminish the pleasures of eating.1 Studies indicate that extensive tooth loss impairs chewing efficiency.3,4 Because having 20 teeth is considered necessary for functional dentition5 and chewing with removable dentures is at least 30% to 40% less efficient than chewing with natural teeth,6 persons with extensive or complete tooth loss are more likely to substitute easier-to-chew foods such as those rich in saturated fats and cholesterol for foods high in carotenes, vitamin C, and fiber.7,8 Among older persons, tooth loss has been shown to be associated with both weight loss9 and obesity.10
Extensive and complete tooth loss may also restrict social contact and inhibit intimacy.1 Tooth loss can affect speech, which in turn limits social interaction,11 detracts from physical appearance,12 and lowers self-esteem.13
Untreated oral diseases will not resolve if left untreated and can profoundly impact quality of life. Pain from untreated oral diseases can restrict normal activities of daily life and disturb sleep.1 In advanced states, caries involves the pulp of the tooth and destroy tooth structure leaving only root fragments that can lead to ulcerations and abscesses.14 Periodontitis can destroy the supporting tissues of the teeth and also lead to abscesses that result in swelling, bleeding, and pain.15 Untreated, caries and periodontitis ultimately lead to tooth loss.16
Failure to prevent or control the progression of oral disease may increase the risk of adverse health outcomes. A recent Cochrane systematic review found evidence that the treatment of periodontal disease improved metabolic control among persons with type 2 diabetes.17 Another recent study found that invasive dental procedures (periodontal therapy and tooth extraction), likely avoidable with early treatment and prevention, increased the incidence of ischemic stroke and myocardial infarctions.18
Studies have demonstrated a similar association between oral hygiene and positive health outcomes. Two systematic reviews19,20 found that enhanced oral hygiene care can prevent respiratory infections and death from pneumonia in elderly people in hospitals and nursing homes. Another recent study found that frequent toothbrushing was associated with lower levels of cardiovascular disease.21
Preventing Poor Oral Health
Poor oral health is largely preventable.1 A meta-analysis found that fluorides, whether self-applied (i.e., toothpaste), professionally applied, or delivered through community water systems, reduce coronal caries incidence in adults by about 25%.22 Fluorides22 and antimicrobial varnish (i.e., chlorhexidine-thymol)23 are also effective in reducing root caries incidence. Effective interventions to prevent and control periodontal disease include scaling and root planing24 and oral health education on self-care.25 Increased exposure to fluorides has been a major factor contributing to the decline in edentulism (i.e., total tooth loss) over the past 50 years.26 By 2004, the prevalence of complete tooth loss among those aged 75 years and older had dropped to less than half the 1957 rate—68% versus 31%.16,27
Untreated Dental Disease and Limited Access to Care
The presence of extensive tooth loss, untreated caries, and untreated periodontal disease among older adults27 indicates that a sizable number may not have access to interventions effective in preventing and controlling oral disease. In 2008, almost half of older community-dwelling dentate adults reported no past-year dental visit.28 There is also evidence that those in highest need are the least likely to receive care. Among dentate adults aged 65 years and older, racial/ethnic minorities were about half as likely to report a past-year dental visit28 and about twice as likely to have at least 1 tooth with a cavity in need of a restoration than were their nonminority counterparts—37% and 41%, respectively, for non-Hispanic Blacks and Mexican Americans versus 16% for non-Hispanic Whites.27
Older adults may have more difficulty accessing effective interventions to prevent and control oral disease than do younger adults. One major barrier is lack of insurance. Medicare only covers narrowly defined medically necessary procedures and many state Medicaid programs do not cover dental services for adults. This results in adults paying an increasing portion of their dental expenditures out of pocket as they age. National data indicate that the percentage of dental expenditures paid by private dental insurance decreased with age from 50% for dentate persons aged 55 to 64 years, to 22% for dentate persons aged 65 to 74 years, and to 14% for dentate persons aged 75 years and older.28 This lack of dental insurance coverage may affect treatment choices. Mean dental expenditures were lower among persons aged 75 years and older compared with persons aged 55 to 74 years,29 suggesting that these persons may have selected no treatment or lower cost options such as tooth extraction instead of more expensive endodontic and prosthetic treatment.
As older adults age they may experience difficulties brushing their teeth, which has been shown to be effective in preventing oral disease,30 and in seeking effective clinical care.29 For example, institutionalized and homebound elderly for whom self-care may be especially difficult have poorer oral health than active elderly.31–33
Low utilization of dental care may also be attributable to lack of perceived need. Among adults with similar clinical dental health status, older adults report less need for dental care than do younger adults. Perceived need is an important predictor of dental utilization—a multivariate analysis found the best predictor of dental utilization by older adults to be perceived importance of dental care followed by perceived need and number of teeth remaining.34 The disadvantaged and ethnic minorities are also more likely to report lower perceived need than other older adults with similar clinical status.
EPIDEMIOLOGY AND BURDEN
Both caries and periodontal disease share common risk factors with other chronic diseases. These risk factors include poverty,29 poor diet,30 and tobacco use.29 Tobacco use accounts for more than half of periodontitis cases among US adults.35
Factors associated with aging can also increase the risk of dental caries. For example, chronic conditions and medications taken to treat them increase the likelihood of dry mouth. Commonly used drugs that can induce dry mouth include tricyclic antidepressants, antipsychotics, atropinics, β-blockers, and antihistamines.36 Saliva protects teeth against dental caries by lubricating the mouth and gums, which in turn reduces bacteria growth, and provides minerals, such as calcium, phosphate, and fluoride needed to remineralize tooth surfaces where tooth decay is just beginning. Receding gums, associated with periodontal diseases, are more common in older adults and expose root surfaces to decay-causing bacteria.
The National Health and Nutrition Examination Survey (NHANES) is a program of studies designed to assess the health and nutritional status of adults and children in the United States. The cross-sectional survey is unique in that it combines interviews and physical examinations. We used data from NHANES 2005 through 200837 to estimate dentate status and prevalence of untreated dental disease (Figures 1 and 2) by age (50–64 years, 65–74 years, and ≥ 75 years) and selected characteristics, including persons reporting fair or poor general health (hereafter referred to as poor general health), chronic disease status (see Appendix A, available as a supplement to the online version of this article at http://www.ajph.org), race/ethnicity (non-Hispanic Whites, non-Hispanic Blacks, and Hispanics), and income (≤ 200% and > 200% federal poverty level). NHANES 2003 through 200838 includes oral health quality of life–related questions (Table 1; distribution of responses to question in Appendix B, available as a supplement to the online version of this article at http://www.ajph.org). Because NHANES only samples noninstitutionalized persons, data from 2 state surveys39,40 conducted since 2000 provided statewide estimates of long-term-care (LTC) residents’ oral health status. Because of the paucity of data for LTC residents, these findings may not be generalizable to other states. Four major themes emerged from the analyses of these data.
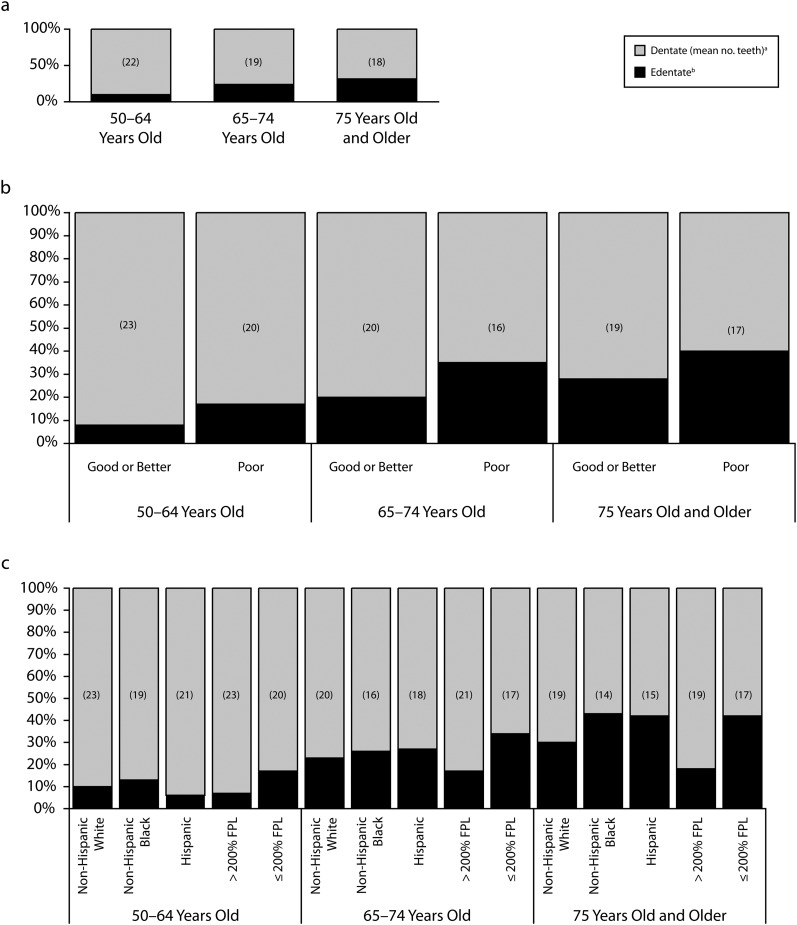
FIGURE 1—
Tooth loss among US adults aged 50 years and older by (a) age, (b) age and general health status, and (c) age, race/ethnicity, and income: NHANES 2005-2008.
Note. FPL = federal poverty level.
aDifference in mean number of teeth between persons aged 50–64 years and ≥ 75 years was significant at P < .05. Difference in mean number of teeth by general health status was significant at P < .05 for all ages. Difference in mean number of teeth between Non-Hispanic White and Non-Hispanic Black and Non-Hispanic White and Hispanic was significant at P < .05 for all ages. Difference in mean number of teeth by income was significant at P < .05 for all ages.
bDifference in edentulism between persons aged 50–64 years and ≥ 75 years was significant at P < .05. Difference by general health status was significant at P < .05 for all ages. Difference between Non-Hispanic White and Non-Hispanic Black and Non-Hispanic White and Hispanic was significant at P < .05 only for persons aged ≥ 75 years. Difference by income status was significant at P < .05 for all ages.
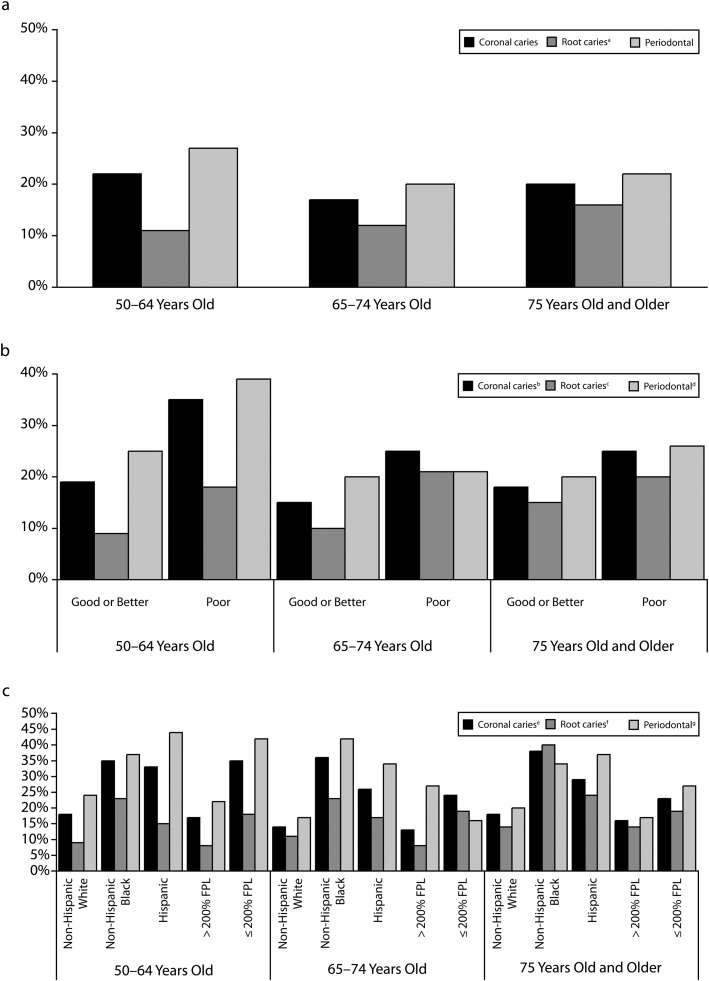
FIGURE 2—
Untreated dental disease among US adults aged 50 years and older by (a) age, (b) age and general health status, and (c) age, race/ethnicity, and income: NHANES 2005-2008.
Note. FPL = federal poverty level.
aDifference between persons aged 50–64 years and ≥ 75 years was significant at P < .01.
bDifference by general health status was significant at P < .05 for all ages.
cDifference by general health status was significant at P < .05 for persons aged 50–74 years.
dDifference by general health status was significant at P < .05 for persons aged 50–64 years.
eDifference between Non-Hispanic White and Non-Hispanic Black was significant at P < .05 for all ages. Difference between Non-Hispanic White and Hispanic was significant at P < .05 for persons aged 50–74 years. Difference by income significant at P < .05 for all ages.
fDifference between Non-Hispanic White and Non-Hispanic Black and Non-Hispanic White and Hispanic was significant at P < .05 for all ages. Difference by income was significant at P < .05 for persons aged 50–74 years.
gDifference between Non-Hispanic White and Non-Hispanic Black and Non-Hispanic White and Hispanic was significant at P < .05 for all ages. Difference by income was significant at P < .05 for all ages.
TABLE 1—
US Adults and Select Groups Aged 50 Years and Older Responding Positively to Oral Health–Related Quality of Life Indicators: National Health and Nutrition Examination Survey, 2003–2008
| Painful Aching Anywhere in Mouth, % (SE) |
Avoided Particular Foods Because of Problems With Teeth, Mouth, or Dentures, % (SE) |
Self-Conscious or Embarrassed Because of Teeth, Mouth, or Dentures, % (SE) |
Life Less Satisfying Because of Problems With Teeth, Mouth, or Dentures, % (SE) |
|||||||||
| Group | 50–64 Years | 65–74 Years | ≥ 75 Years | 50–64 Years | 65–74 Years | ≥ 75 Years | 50–64 Years | 65–74 Years | ≥ 75 Years | 50–64 Years | 65–74 Years | ≥ 75 Years |
| All persons | 20.44 (0.90) | 13.70 (0.99) | 12.37 (0.74) | 19.75 (0.85) | 14.92 (0.99) | 18.01 (1.06) | 16.21 (0.57) | 10.42 (0.69) | 10.25 (0.61) | 12.69 (0.70) | 8.61 (0.59) | 9.84 (0.78) |
| General health | ||||||||||||
| Good or better | 17.28 (0.99) | 11.57 (0.99) | 9.64 (0.70) | 15.49 (0.71) | 12.67 (0.99) | 14.89 (1.29) | 13.13 (0.62) | 8.44 (0.70) | 8.42 (0.59) | 9.12 (0.62) | 6.93 (0.78) | 6.62 (0.82) |
| Fair or poor | 32.03 (1.87) | 20.50 (2.07) | 18.61 (1.51) | 35.34 (2.01) | 22.06 (2.53) | 24.95 (1.71) | 27.54 (1.33) | 16.75 (1.68) | 14.52 (1.51) | 25.81 (1.39) | 13.96 (1.79) | 17.21 (1.56) |
| Income | ||||||||||||
| ≤ 200% FPL | 26.96 (1.74) | 16.08 (1.35) | 13.09 (0.90) | 29.14 (1.36) | 18.78 (1.48) | 20.70 (1.67) | 25.26 (1.47) | 14.16 (1.20) | 11.35 (0.97) | 21.51 (1.33) | 11.75 (1.14) | 10.91 (1.09) |
| > 200% FPL | 17.92 (0.82) | 12.14 (1.23) | 11.49 (1.25) | 16.11 (0.98) | 12.37 (1.05) | 14.76 (1.25) | 12.72 (0.70) | 7.96 (1.00) | 8.92 (1.02) | 9.28 (0.72) | 6.56 (0.88) | 8.56 (0.95) |
| Race/ethnicity | ||||||||||||
| Non-Hispanic White | 19.08 (0.98) | 12.58 (1.04) | 11.30 (0.79) | 18.36 (1.06) | 13.50 (1.14) | 17.54 (1.16) | 14.62 (0.74) | 8.92 (0.80) | 9.85 (0.70) | 10.82 (0.87) | 7.40 (0.70) | 9.31 (0.81) |
| Non-Hispanic Black | 27.22 (1.62) | 17.91 (1.92) | 17.70 (2.41) | 23.84 (1.66) | 19.45 (1.64) | 20.02 (2.53) | 22.77 (1.39) | 18.96 (2.57) | 12.29 (2.35) | 20.32 (1.58) | 15.08 (2.07) | 11.46 (2.11) |
| Hispanic | 21.33 (1.62) | 17.85 (1.96) | 12.15 (2.04) | 20.20 (1.60) | 20.94 (2.61) | 20.86 (3.13) | 21.42 (1.82) | 15.90 (2.15) | 13.21 (2.23) | 17.66 (1.47) | 14.41 (1.89) | 14.32 (2.63) |
Notes. FPL = federal poverty level. Positive response = answered very or fairly often or occasionally in past year. We do not report findings for 1 question on impact of oral health on ability to perform job or attend school because it likely did not apply to some of our study population, 1 question on the impact of oral health on ability to eat that was highly correlated to the question on food avoidance, and 1 question on impact of oral health on taste because of space constraints.
Risk of Tooth Loss Among Older Persons
Age per se was not a risk factor for tooth loss. Among the same age cohorts, edentulism rates vary by country and have decreased significantly over time in the United States.16 A major factor in the decline in tooth loss is better prevention and control of its 2 major causes—dental caries and periodontal infections.16 Among the current cohort of older adults (NHANES 1999–2004), however, tooth loss was highest among persons aged 75 years and older (Figure 1). Compared with persons aged 50 to 64 years, persons aged 75 years and older were 3 times more likely to be edentulous (32% vs 10%) and, among the dentate, persons aged 75 years and older had 4 fewer teeth on average (18 vs 22).
A significant number of older adults had untreated dental disease. About 20% had untreated dental caries in a coronal surface and a similar number needed periodontal treatment (Figure 2). Persons in the oldest age group were about 50% more likely to have untreated root caries than persons aged 50 to 64 years (16% vs 11%).
Poor Oral Health and Poor General Health
The NHANES data confirm findings of previous studies—there is a strong association between poor general health and poor oral health. Edentulism was about 10% points higher among persons reporting poor general health compared with those reporting good or better general health (Figure 1). Dentate persons reporting poor general health also had from about 2 (aged ≥ 75 years) to 4 (aged 65–74) fewer teeth than persons reporting good or better general health. Of note is that the mean number of teeth in persons aged 50 years and older reporting poor general health was below the threshold for functional dentition (Figure 1; mean number for those aged 50–64 years was 19.7). Rates of complete and partial tooth loss were higher among older persons with arthritis, cardiovascular disease, chronic obstructive pulmonary disease, diabetes, and low vision/blindness compared with persons without these conditions (Appendix C available as a supplement to the online version of this article at http://www.ajph.org).
Persons reporting poor health also had higher levels of untreated dental disease (Figure 2) and were more likely to report painful aching in their mouth—32% of persons aged 50 to 64 years with poor health (Table 1). Specific conditions that increased the likelihood of reporting pain include arthritis, chronic obstructive pulmonary disease, cardiovascular disease, diabetes, and low or no vision (Appendix D, available as a supplement to the online version of this article at http://www.ajph.org). About 22% of adults aged 65 to 74 years and 35% of adults aged 50 to 64 years reporting poor general health also reported avoiding particular foods because of poor oral health (problems with their teeth, dentures, or mouth; Table 1).
Poor oral health profoundly diminishes quality of life among persons with poor general health—persons aged 50 to 64 years reporting poor health were almost 3 times as likely to report that their life was less satisfying because of poor oral health whereas persons in the other age groups were about twice as likely (Table 1).
Disparities in Oral Health by Race/Ethnicity and Income
Disparities in percentage dentate by race/ethnicity and income increased with age (Figure 1). The percentage dentate was similar by race/ethnicity among those aged 50 to 74 years, but ranged from about 57% for non-Hispanic Blacks and Hispanics to 70% for non-Hispanic Whites among persons aged 75 years and older. Among persons aged 50 to 64 years there was a 10% point difference by income; among those aged 75 years and older, the difference was 24% points. Non-Hispanic Whites aged 75 years and older had about 4 more teeth than non-Hispanic Blacks or Hispanics (19 compared with about 15 teeth). Higher-income adults had 2 to 3 more teeth than lower-income adults depending on age group (Figure 1).
Disparities in untreated dental disease for the 2 primary causes of tooth loss—caries and periodontal disease—however, were typically highest in persons aged 50 to 64 years (Figure 2). Poor persons in this age group were about twice as likely to have a cavity that needs treatment (35% vs 17%), have untreated root caries (18% vs 8%), or need periodontal treatment (42% vs 22%) as were their higher income counterparts. The prevalence of untreated root caries, however, was especially striking for older non-Hispanic Blacks—more than 40% (Figure 2).
Disparities in untreated dental disease may contribute to disparities in oral health–related quality of life. Persons aged 50 to 64 years, racial/ethnic minorities, and the poor were more likely to report oral pain, food avoidance, and self-consciousness or embarrassment because of their mouth, teeth, or dentures (Table 1). They were also about twice as likely to report that poor oral health diminishes their satisfaction with life (Table 1).
Vulnerable Elderly and Noninstitutionalized Counterparts
Data from Massachusetts (2009)39 and Kentucky (2002–2005)40 indicate that the vulnerable elderly (residents of LTC facilities and homebound) have high levels of untreated dental disease (Appendix E, available as a supplement to the online version of this article at http://www.ajph.org). In Massachusetts, almost 60% of dentate LTC residents have untreated cavities; among these persons, 58% have major or urgent treatment needs. Almost 75% of LTC residents have gingivitis, an important marker of poor oral hygiene among elders that may indicate a need for assistance with oral hygiene. In Kentucky, only 48% of LTC residents are classified as having good or better oral health by a dentist. This value decreases to 40% for homebound elderly. Among edentulous persons, 81% of residents in LTC facilities in Massachusetts have no or inadequate dentures. In Kentucky these values for mandibular dentures are 30% for LTC residents and 46% for homebound elderly. Overall, the oral health (e.g., dentate status and untreated dental disease) of LTC residents and the homebound is markedly worse than that of the younger elderly living independently (Appendix E, available as a supplement to the online version of this article at http://www.ajph.org).
The vulnerable elderly confront barriers in accessing clinical care. More than 59% of nursing home directors in Massachusetts39 report cost as a barrier to providing dental care to their residents and 69% of the homebound elderly in Kentucky report that cost, lack of transportation, and limited mobility restrict their access to dental clinical care.40 Utilization of dental care among the vulnerable elderly is also low—55% of the homebound elderly in Kentucky report not having visited the dentist within 5 years.40
Surveyed adults in Kentucky aged 65 years and older (64% were either residents of LTC or homebound) reported that poor oral health has a significant impact on their quality of life: 19% reported aching in their mouth, teeth, or jaws; 22% reported dissatisfaction with their ability to chew; and 23% reported dissatisfaction with the appearance of their teeth or dentures.40
ROLES AND PRIORITIES FOR PUBLIC HEALTH SYSTEM
NHANES data confirm that, compared with the general elderly population, untreated dental disease is higher among persons reporting poor general health, racial/ethnic minorities, and persons living in low-income families. These same groups are also more likely to report oral pain; food avoidance; self-consciousness or embarrassment because of their mouth, teeth, or dentures; and that life is less satisfying because of poor oral health. These impacts tend to be higher among persons aged 50 to 64 years compared with the older age groups.
Our finding that persons reporting poor general health have higher levels of untreated dental disease that diminishes their oral health–related quality of life suggests that oral health should be better integrated into medical care. Because persons reporting poor health are more likely to visit a physician than a dentist,41 it is important that primary care providers and geriatricians be educated on common oral conditions, risk factors, and healthy behaviors along with the medical, functional, emotional, and social consequences of poor oral health. It is also important that new integrated care models (e.g., health homes) incorporate oral health expertise into a comprehensive set of services, especially because persons reporting poor health are significantly more likely to have multiple chronic conditions.42 Finally, the finding that more than 35% of the youngest elderly group who reported poor health also reported avoiding certain foods suggests that educating clinicians to recognize common oral conditions and to refer for subsequent treatment would not only enhance quality of life but also encourage healthier eating patterns that could result in improved long-term health.
Several factors highlight the importance of developing community programs to prevent and control oral disease among the elderly. First, demographic trends coupled with the fact that current and future cohorts of older adults are more likely than previous cohorts to retain their natural teeth indicate a future increase in the number of elderly at risk for oral disease. Second, the high levels of untreated dental disease among certain segments of the elderly, especially those aged 50 to 64 years, as well as the potential future shortage of dentists (the number of persons per dentist is expected to increase from 1712 in the mid-1990s to 1898 by 2020)43 suggest that future dental treatment needs will remain at their current levels or increase. Finally, leaving oral disease untreated not only diminishes quality of life but also may place the elderly at higher risk for other adverse health outcomes.17–21
To successfully implement and effectively target such programs, systematic collection of data on the oral health status of the elderly will be required. The Association of State and Territorial Dental Directors has developed and validated a simple population-based screening tool that can be performed by trained nondentists to provide key information to assess dental care needs44 comparable to data previously obtained in Kentucky and Massachusetts.39,40 Congregate meal settings are 1 of the 2 recommended data collection sites because they serve higher risk community-dwelling older adults and have a set location and times when multiple adults can be surveyed. The second recommended data collection site is LTC facilities.
Important components of community programs would include education and improved access to effective preventive services. Through partnerships with the aging services network and organizations addressing aging issues, messages on older adults’ need for and the effectiveness of fluorides in preventing oral disease could be more widely disseminated to elders, their caregivers, health care providers, and policymakers. Innovative strategies to increase access to preventive care through medical settings and community programs should be explored. Approaches such as replicating the North Carolina experiment of using physician offices to screen for oral disease and deliver fluoride varnish to very young children45 should be implemented and evaluated for older adults. In a similar way, providing fluoride varnish in pharmacy settings, which have been shown to be effective in increasing influenza vaccine coverage among older adults,46 could be piloted. For the vulnerable (homebound and LTC residents) elderly, the effectiveness of alternative modes of fluoride delivery, such as dietary prescription supplements, for persons who cannot brush their teeth, and partnering with associations that serve the homebound elderly to deliver fluoride, should be explored.16
A comprehensive strategy to address the oral health needs of the vulnerable elderly is also needed. Valid and reliable data on oral health status as well as accountability for LTC facilities to provide adequate daily oral hygiene care and access to regular preventive dental care are especially important for this group of older adults—at present, there are few incentives to provide such care.47 In addition, LTC residents and the homebound elderly are likely in poorer states of health than the elderly in the general population. Poor self-reported health is associated with cognitive and physical limitations48 that hinder the ability to adequately articulate dental needs, perform daily oral hygiene, or access necessary care.
An essential element of this strategy would be to implement and evaluate different approaches to ensure that more homebound seniors and LTC residents benefit from daily self-care procedures, receive oral assessments as the basis for individualized care plans that address provision of preventive care by trained personnel, and have access to restorative services when appropriate. To ensure adequate access for persons with limited mobility, the feasibility of different models to provide dental care onsite at LTC facilities (e.g., staffing and equipping dental operatories49 or contracting with mobile dental clinics) should be evaluated. Two possible approaches to increase LTC staff knowledge about oral health include having dental hygienists provide standardized trainings to existing LTC staff and creating a new LTC staff position for a geriatric dental practitioner (e.g., create a geriatric advanced practice dental hygienist similar to nurse practitioners).49
Finally, because of the high levels of untreated disease among the poor and vulnerable elderly, the feasibility of ensuring a safety net that covers basic preventive care and restorative services to eliminate pain and infections should be examined. At present, about half of the states provide no or minimal dental benefits for adults enrolled in Medicaid.50 A first step would be to document the costs and consequences of leaving dental disease untreated. These findings could then be used to support coverage of select groups of elders. It has been suggested that a possible funding mechanism could be to add adult dental coverage to the Medicaid “aged, blind, and disabled” provisions.49
Good oral health is essential to healthy aging. Because effective interventions to prevent and control oral disease exist, good oral health can be achieved by older adults. The public health system can play a vital role in ensuring that this occurs.
Acknowledgments
This article was prepared for the CDC series on aging and the roles of public health.
Funding was received from the National Institutes of Health (J. A. J.; grant K24DE018211/DE/NIDCR NIH HHS/United States).
The authors would like to thank Laurie Barker for her assistance in determining the best way to visually display the data in the figures contained in the article.
Human Participant Protection
Because the data used in this analysis are publicly available and not identifiable, institutional review board approval was not required.
References
- 1.Oral Health in America: A Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000 [Google Scholar]
- 2.Centers for Disease Control and Prevention, Division of Oral Health Oral cancer. Available at http://www.cdc.gov/oralhealth/topics/cancer.htm. Accessed December 7, 2010
- 3.Rosenoer LM, Sheiham A. Dental impacts on daily life and satisfaction with teeth in relation to dental status in adults. J Oral Rehabil. 1995;22(7):469–480 [DOI] [PubMed] [Google Scholar]
- 4.Sarita PT, Witter DJ, Kreulen CM, Van't Hof MA, Creugers NH. Chewing ability of subjects with shortened dental arches. Community Dent Oral Epidemiol. 2003;31(5):328–334 [DOI] [PubMed] [Google Scholar]
- 5.Recent Advances in Oral Health. Geneva, Switzerland: World Health Organization; 1992:16–17 WHO Technical Report Series No. 826 [Google Scholar]
- 6.Idowu AT, Handelman SL, Graser GN. Effect of denture stability, retention, and tooth form on masticatory function in the elderly. Gerodontics. 1987;3(4):161–164 [PubMed] [Google Scholar]
- 7.Walls AWG, Steele JG, Sheiham A, Marcenes W, Moynihan PJ. Oral health and nutrition in older people. J Public Health Dent. 2000;60(4):304–307 [DOI] [PubMed] [Google Scholar]
- 8.Ervin RB, Dye BA. The effect of functional dentition on Healthy Eating Index scores and nutrient intakes in a nationally representative sample of older adults. J Public Health Dent. 2009;69(4):207–216 [DOI] [PubMed] [Google Scholar]
- 9.Ritchie CS, Joshipura K, Silliman RA, Miller B, Douglas CW. Oral health problems and significant weight loss among community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2000;55(7):M366–M371 [DOI] [PubMed] [Google Scholar]
- 10.Sheiham A, Steele JG, Marcenes W, Finch S, Walls AW. The relationship between oral health status and body mass index among older people: a national survey of older people in Great Britain. Br Dent J. 2002;192(12):703–706 [DOI] [PubMed] [Google Scholar]
- 11.Smith JM, Sheiham A. How dental conditions handicap the elderly. Community Dent Oral Epidemiol. 1979;7(6):305–310 [DOI] [PubMed] [Google Scholar]
- 12.Eli I, Bar-Tal Y, Kostovetzki I. At first glance: social meanings of dental appearance. J Public Health Dent. 2001;61(3):150–154 [DOI] [PubMed] [Google Scholar]
- 13.Starr JM, Hall R. Predictors and correlates of of edentulism in the healthy older people. Curr Opin Clin Nutr Metab Care. 2010;13(1):19–23 [DOI] [PubMed] [Google Scholar]
- 14.Monse B, Heinrich-Weltzien R, Benzian H, Holmgren C, van Palenstein Helderman W. PUFA—An index of clinical consequences of untreated dental caries. Community Dent Oral Epidemiol. 2010;38(1):77–82 [DOI] [PubMed] [Google Scholar]
- 15.Herrera D, Roldán S, González I, Sanz M. The periodontal abscess (I). Clinical and microbiological findings. J Clin Periodontol. 2000;27(6):387–394 [DOI] [PubMed] [Google Scholar]
- 16.Burt BA, Eklund SA. Dentistry, Dental Practice, and the Community. St. Louis, MO: Elsevier Saunders; 2005:224 [Google Scholar]
- 17.Simpson TC, Needleman I, Wild SH, Moles DR, Mills EJ. Treatment of periodontal disease for glycaemic control in people with diabetes. Cochrane Database Syst Rev. 2010;12(5):CD004714. [DOI] [PubMed] [Google Scholar]
- 18.Minassian C, D'Aiuto F, Hingorani AD, Smeeth L. Invasive dental treatment and risk for vascular events a self-controlled case series. Ann Intern Med. 2010;153(8):499–506 [DOI] [PubMed] [Google Scholar]
- 19.Sjögren P, Nilsson E, Forsell M, Johansson O, Hoogstraate J. A systematic review of the preventive effect of oral hygiene on pneumonia and respiratory tract infection in elderly people in hospitals and nursing homes: effect estimates and methodological quality of randomized controlled trials. J Am Geriatr Soc. 2008;56(11):2124–2130 [DOI] [PubMed] [Google Scholar]
- 20.Pace CC, McCullough GH. The association between oral microorganisms and aspiration pneumonia in the institutionalized elderly: review and recommendations. Dysphagia. 2010;25(4):307–322 [DOI] [PubMed] [Google Scholar]
- 21.de Oliveira C, Watt R, Hamer M. Toothbrushing, inflammation, and risk of cardiovascular disease: results from Scottish Health Survey. BMJ. 2010;340c2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Griffin SO, Regnier E, Griffin PM, Huntley V. Effectiveness of fluoride in preventing caries in adults. J Dent Res. 2007;86(5):410–415 [DOI] [PubMed] [Google Scholar]
- 23.Tan HP, Lo EC, Dyson JE, Luo Y, Corbet EF. A randomized trial on root caries prevention in elders. J Dent Res. 2010;89(10):1086–1090 [DOI] [PubMed] [Google Scholar]
- 24.Heitz-Mayfield LJ, Trombelli L, Heitz F, Needleman I, Moles D. A systematic review of the effect of surgical debridement vs non-surgical debridement for the treatment of chronic periodontitis. J Clin Periodontol. 2002;29(Suppl 3):92–102 [DOI] [PubMed] [Google Scholar]
- 25.Little SJ, Hollis JF, Stevens VJ, Mount K, Mullooly JP, Johnson BD. Effective group behavioral intervention for older periodontal patients. J Periodontal Res. 1997;32(3):315–325 [DOI] [PubMed] [Google Scholar]
- 26.[No authors listed.] Recommendations for using fluoride to prevent and control dental caries in the United States. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2001;50(RR-14):1–42 [PubMed] [Google Scholar]
- 27.Dye BA, Tan S, Smith Vet al. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital Health Stat 11. 2007;11(248):1–92 [PubMed] [Google Scholar]
- 28.Agency for Healthcare Research and Quality Medical Expenditure Survey 2008 [data were generated using the Dental, Oral and Craniofacial Data Resource Center's Data Query System]. Available at: http://drc.hhs.gov. Accessed October 15, 2010
- 29.Vehkalahti MM, Paunio IK. Occurrence of root caries in relation to dental health behavior. J Dent Res. 1988;67(6):911–914 [DOI] [PubMed] [Google Scholar]
- 30.Beck J. The epidemiology of root surface caries. J Dent Res. 1990;69(5):1216–1221 [DOI] [PubMed] [Google Scholar]
- 31.Pajukoski H, Meurman JH, Snellman-Grohn S, Sulkava R. Oral health in hospitalized and nonhospitalized community-dwelling elderly patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88(4):437–443 [DOI] [PubMed] [Google Scholar]
- 32.Martin KU, Martin JO. Meeting the oral health needs of institutionalized elderly. Dysphagia. 1992;7(2):73–80 [DOI] [PubMed] [Google Scholar]
- 33.Strayer MS. Dental health among homebound elderly. J Public Health Dent. 1993;53(1):12–16 [DOI] [PubMed] [Google Scholar]
- 34.Kiyak HA. An explanatory model of older persons’ use of dental services: implications for health policy. Med Care. 1987;25(10):936–952 [DOI] [PubMed] [Google Scholar]
- 35.Tomar SL, Asma S. Smoking attributable periodontitis in the United States: findings from NHANES III. National Health and Nutrition Examination Survey. J Periodontol. 2000;71(5):743–751 [DOI] [PubMed] [Google Scholar]
- 36.Petersen PE, Yamamoto T. Improving the oral health of older people: the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2005;33(2):81–92 [DOI] [PubMed] [Google Scholar]
- 37.National Center for Health Statistics National Health and Nutrition Examination Survey Data [2005–2008]. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Control and Prevention; Available at: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm. Accessed January 11, 2010 [Google Scholar]
- 38.National Center for Health Statistics National Health and Nutrition Examination Survey Data [2003–2008]. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Control and Prevention; Available at: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm. Accessed January 11, 2010 [Google Scholar]
- 39.The Commonwealth's high-risk senior population results and recommendations from 2009 statewide oral health assessment. Boston, MA: Massachusetts Department of Public Health, Office of Oral Health; 2010. Available at: http://www.mass.gov/eohhs/docs/dph/com-health/oral-health/senior-oral-health-assessment-report.pdf [Google Scholar]
- 40.Bush HM, Dickens NE, Henry RGet al. Oral health status of older adults in Kentucky: results from the Kentucky elder oral health survey. Spec Care Dentist. 2010;30(5):185–192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.2009: With Special Feature on Medical Technology. Hyattsville, MD: National Center for Health Statistics; 2010 [PubMed] [Google Scholar]
- 42.Chen H-Y, Baumgardner DJ, Rice JP. Health-related quality of life among adults with multiple chronic conditions in the United States, Behavioral Risk Factor Surveillance System, 2007. Prev Chronic Dis. 2011;8(1):A09 Available at: http://www.cdc.gov/pcd/issues/2011/jan/09_0234.htm. Accessed May 1, 2011 [PMC free article] [PubMed] [Google Scholar]
- 43.Mertz E, O'Neil E. The growing challenge of providing oral health care services to all Americans. Health Aff (Millwood). 2002;21(5)2:66–77 [DOI] [PubMed] [Google Scholar]
- 44.ASTDD Basic Screening Survey for Older Adults Planning and Implementation Package. Available at: http://www.astdd.org/basic-screening-survey-tool. Accessed August 18, 2010
- 45.Rozier RG, Sutton BK, Bawden JW, Haupt K, Slade GD, King RS. Prevention of early childhood caries in North Carolina medical practices: implications for research and practice. J Dent Educ. 2003;67(8):876–885 [PubMed] [Google Scholar]
- 46.Grabenstein JD, Guess HA, Hartzema AG, Koch GG, Konrad TR. Effect of vaccination by community pharmacists among adult prescription recipients. Med Care. 2001;39(4):340–348 [DOI] [PubMed] [Google Scholar]
- 47.Katz RV, Smith BJ, Berkey DB, Guset A, O'Connor MP. Defining oral neglect in institutionalized elderly: a consensus definition for the protection of vulnerable elderly people. J Am Dent Assoc. 2010;141(4):433–440 [DOI] [PubMed] [Google Scholar]
- 48.Idler EL, Kasl SV. Self-ratings of health—do they also predict change in functional ability? J Gerontol B Psychol Sci Soc Sci. 1995;50(6):S344–S353 [DOI] [PubMed] [Google Scholar]
- 49.The Elders’ Oral Health Summit Proceedings. Boston, Massachusetts, 13–14 September 2004. J Dent Educ. 2005;69(9):956–1063 [PubMed] [Google Scholar]
- 50.Ku L. Medical and dental care utilization and expenditures under Medicaid and private health insurance. Med Care Res Rev. 2009;66(4):456–471 [DOI] [PubMed] [Google Scholar]