Abstract
The Family Van mobile health clinic uses a “Knowledgeable Neighbor” model to deliver cost-effective screening and prevention activities in underserved neighborhoods in Boston, MA. We have described the Knowledgeable Neighbor model and used operational data collected from 2006 to 2009 to evaluate the service. The Family Van successfully reached mainly minority low-income men and women. Of the clients screened, 60% had previously undetected elevated blood pressure, 14% had previously undetected elevated blood glucose, and 38% had previously undetected elevated total cholesterol. This represents an important model for reaching underserved communities to deliver proven cost-effective prevention activities, both to help control health care costs and to reduce health disparities.
KEY FINDINGS
▪The Family Van mobile health clinic succeeded in reaching mainly minority low-income clients by using a community-based “Knowledgeable Neighbor” model.
▪Of the clients screened, 60% had previously undetected elevated blood pressure, 14% had previously undetected elevated blood glucose, and 38% had previously undetected elevated total cholesterol.
▪Male clients were almost as common as female clients. Men were more likely to be uninsured and had higher rates of previously undiagnosed elevated blood pressure and blood glucose.
▪Most clients had health insurance, suggesting that this service addresses barriers to health care beyond lack of insurance.
▪Mobile health clinics are a promising tool to deliver proven cost-effective chronic disease prevention interventions in underserved areas and to meet the dual imperatives of controlling health care costs and reducing health disparities.
New solutions are needed to deliver cost-effective preventive interventions for chronic conditions in low-income minority communities across the United States, both to reduce health disparities and to control the nation's rising health care costs.1–4 The National Commission on Prevention Priorities has identified the top 25 cost-effective preventive interventions, including hypertension, diabetes, and hypercholesterolemia screening.5 However, as highlighted in the National Healthcare Disparities Report, low-income minority communities have poor access to these services.2 They experience poorer client-provider communication and lower client trust and health literacy.1,2,6 In addition, financial and logistical barriers include lack of insurance, out-of-pocket medical expenses, distance to services, appointment scarcity, and the complexities of navigating the system with public or no insurance.1,2,6–8
Created to overcome barriers to health care, mobile health clinics have operated in the United States for many years, and an estimated 2000 currently operate.9,10 Despite the mobile health clinic sector's size, it has low visibility within the health care system perhaps because of its positioning in the nonprofit sector and its relative lack of rigorous formal evaluation. The aims of this study were to describe the model used by one mobile health clinic and to evaluate the rates of previously undetected elevated blood pressure, blood glucose, and total serum cholesterol levels yielded from screening. This study used anonymous information collected for operational purposes.
THE FAMILY VAN
The Family Van, a Harvard Medical School affiliate founded in 1992, uses the Knowledgeable Neighbor model to reach underserved communities5 (Box on p. e3; Figure 1; Figure 2).2 A recent study on the causes for delays in treatment after the first signs of stroke found that 75% of African Americans called a friend or relative first, and only 12% called 911 first.11 This inclination to reach out to a trusted friend when in medical need was the basis for the creation of the Knowledgeable Neighbor model. Knowledgeable Neighbor is the role played by all Family Van staff: a friend who helps you learn about and access local resources and who willingly takes the time to listen to your story but to whom you do not relinquish control over your health.12
FIGURE 1—
The Family Van parked at one of its regular sites in Boston, MA.
FIGURE 2—
Rainelle Walker-White, Manager of Direct Service, Family Van, with Santos, a Family Van client.
Health educators, dieticians, and counselors provide screening followed by health education, health coaching, referrals, and navigational support. No diagnoses or treatments are provided on the Family Van. Blood pressure is measured with a manual sphygmomanometer to screen for hypertension. A Cholestech LDX (Alere San Diego, Inc, San Diego, CA) machine is used to measure total serum cholesterol levels to screen for hypercholesterolemia. Fasting or nonfasting elevated blood glucose level is measured with the Ascensia Breeze glucometer (Bayer Corporation, Mishawaka, IN) to screen for diabetes. All clients with elevated screening levels and no previous diagnosis of the relevant condition are referred to a local community health center or their primary care physician for diagnosis and follow-up. Additional navigational support is provided as needed, including assistance with acquiring health insurance, making appointments, health coaching, and follow-up to ensure attendance. Clients are given cards with their screening results and encouraged to drop in regularly for ongoing health coaching and monitoring.
EVALUATION
During 2006 to 2009, 13 272 clients visited the Family Van: 5898 first-time clients and 7374 returning clients. During visits, the team collected anonymous data on paper forms, which were later entered into a Microsoft Access database. Because of the anonymity, it was impossible to link clients’ records over time, so only information from the first visits was analyzed. The Family Van predominantly served minorities: 65% Black, 15% Hispanic, 15% White, and 5% other. Overall, 28% did not speak English as their primary language (Spanish 14%, Haitian Creole 6%, and Cape Verdean Creole 5%). Most (82%) had health insurance, but only 27% had private insurance, suggesting that most were low-income clients. Of the 2762 clients who had their body mass index (BMI, defined as weight in kilograms divided by the square of height in meters) measured, 33% were overweight (BMI = 25–29), and 30% were obese (BMI ≥ 30). Visitors were primarily adults (1% younger than 18 years; 50% aged 35–64 years). Male clients (45%) were almost as common as female clients (55%), and men were more likely to be uninsured (proportion uninsured = 23% of men vs 14% of women; Pearson C2 test = 71; P < .01).
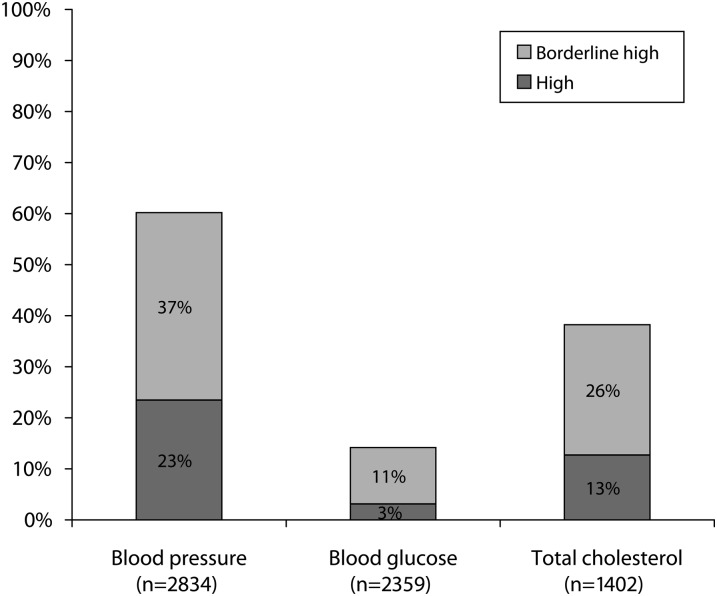
Of those who had their blood pressure measured, 33% reported a history of hypertension or prehypertension; of the remaining 2834 clients screened, 23% had high blood pressure (systolic ≥ 140 mm Hg; diastolic ≥ 90 mm Hg), and 37% had borderline high blood pressure (systolic = 120–139 mm Hg; diastolic = 80–89 mm Hg). Of those who had their blood glucose measured, 18% reported a history of diabetes or prediabetes; of the remaining 2359 clients screened, 3% had levels indicative of diabetes (fasting ≥ 126 mg/dL; nonfasting ≥ 200 mg/dL), and 11% had levels indicative of prediabetes (fasting = 110–126 mg/dL; nonfasting = 140–200 mg/dL). Of those who had their cholesterol level measured, 17% reported a history of hypercholesterolemia or borderline hypercholesterolemia; of the remaining 1402 clients screened, 13% had high total serum cholesterol value (3 240 mg/dL), and 26% had borderline high total serum cholesterol value (200–239 mg/dL; Figure 3).
FIGURE 3—
Results from screening for previously undetected elevated blood pressure, total serum cholesterol, and blood glucose levels in first-time Family Van clients: Boston, MA, 2006–2009.
Note. Screening included only first-time clients who did not already have the diagnosis of the condition and who opted for screening. Thresholds were as per national guidelines (blood pressure—high: diastolic ≥ 90 mm Hg or systolic ≥ 140 mm Hg; borderline high: diastolic = 80–89 mm Hg or systolic = 120–139 mm Hg; blood glucose—high: fasting ≥ 126 mg/dL, nonfasting ≥ 200 mg/dL; borderline high: fasting = 110–126mg/dL; nonfasting = 140–200 mg/dL; total serum cholesterol—high ≥ 240 mg/dL; borderline high = 200–239 mg/dL).
KNOWLEDGEABLE NEIGHBOR MODEL
| Step 1: Reaching Clients Through Creating a Community Hub of Wellness |
| A. Building trust on the Family Van |
| 1. Service is led by health educators, dietitians, and HIV counselors, many of whom are from the community. |
| 2. Inclusive relationships are created through interpersonal informality in a safe, nonhierarchical, nontraditional health care environment. |
| 3. Clients control the encounter, deciding when to come, what screenings to receive, and when and how to act on the information they receive. |
| 4. Staff receives cultural competence training to ensure that they have the skills to learn each client's unique social and economic context, cultural beliefs, and behaviors. |
| B. Building trust in the community |
| 1. Long-term weekly presence in neighborhoods (established 1992) |
| 2. Strong collaborations with community health centers, hospitals, churches, and others |
| 3. Continual outreach through participation in community events and street outreach |
| C. Reducing financial barriers: no charge to clients |
| D. Reducing logistical barriers: drop-in service in the neighborhood (no appointments, no waiting, no eligibility requirements, no distance to travel) |
| Step 2: Empowering Clients to Access Care and Improve Their Health |
| 1. Screening for several chronic conditions, including hypertension, diabetes, and hypercholesterolemia, so that clients can learn about their health |
| 2. Culturally competent health literacy and motivational interviewing: to educate clients about their health and help them develop appropriate wellness strategies |
| 3. Creating a bridge into care: through referral to community neighborhood health centers and social services, with additional advocacy and navigational support |
Note. The Family Van Mobile Health Clinic's Knowledgeable Neighbor Model: Boston, MA, 2006–2009
By multivariate logistic regression, male clients had higher odds than female clients of previously undiagnosed elevated blood pressure and blood glucose levels (blood pressure = 64% for men vs 53% for women; adjusted odds ratio [AOR] = 1.4; 95% confidence interval [CI] = 1.2, 1.7; P < .01; blood glucose = 17% for men vs 12% for women; AOR = 1.8; 95% CI = 1.0, 3.1; P = .02). Other factors associated with higher odds of elevated screening levels were being Black, older, and obese.
CONCLUSIONS
We found that the Family Van was successful at reaching individuals at high risk for chronic disease and yielding a high rate of previously undetected elevated blood pressure, blood glucose, and total serum cholesterol levels. The population served was largely low-income minority groups who experience the greatest disparities in health.2–4 The rates of previously undiagnosed high blood pressure (23%) and total serum cholesterol (13%) among Family Van clients were considerably higher than the age-adjusted prevalence of undiagnosed hypertension and hypercholesterolemia among adults nationally measured through the National Health and Nutrition Examination Survey (NHANES), suggesting that this intervention was successfully addressing a large unmet need (Table 113). The rate of previously undiagnosed high blood glucose level (3%) was equal to the age-adjusted prevalence of undiagnosed diabetes nationally.13 The Family Van rate may be relatively low because diabetes screening services are more readily available in this community or because the Family Van glucose screening protocol has reduced sensitivity as a result of the inclusion of nonfasting glucose readings.
TABLE 1—
Comparison of National Prevalence of Undiagnosed Chronic Conditions: National Health and Nutrition Examination Survey (NHANES), 1999–2006, and Family Van Screening Rates, 2006–2009
| Total Sample, % | Non-Hispanic Black, % | Mexican American/ Latino,a % | Non-Hispanic White, % | |
| NHANES | ||||
| Hypertensio8 | 9 | 8 | 8 | |
| Diabetes | 3 | 3 | 3 | 3 |
| Hypercholesterolemia | 8 | 8 | 8 | 9 |
| Family Van screening | ||||
| High blood pressure | 23 | 26 | 19 | 18 |
| High blood glucose | 3 | 3 | 2 | 4 |
| High total cholesterol | 13 | 10 | 15 | 14 |
Source. Fryar et al.13
Mexican American used in NHANES; Latino used in Family Van screening.
Evaluation Limitations
Rates of elevated blood pressure, total serum cholesterol, and blood glucose levels measured through the Family Van are not directly comparable with diagnosis rates of hypertension, hypercholesterolemia, and diabetes measured through NHANES because the Family Van screening techniques have lower specificity and sensitivity than do the NHANES diagnostic methods and because the Family Van rates depend on clients’ self-report of prior diagnosis. The age distribution also may be different. More importantly, although the Family Van provides additional advocacy and navigational support to clients who screen positive to ensure that they see a physician, the proportion of clients that are successfully referred is unknown. An important aim of the clinic is to help clients manage their health over time through health coaching and monitoring. Improvements in clients’ health over time could not be analyzed because of the anonymity of the data.
Supporting Evidence
This article joins a small but consistent body of literature indicating that mobile health clinics facilitate access to health care.14–17 Significant supportive evidence suggests that the Family Van's Knowledgeable Neighbor model contributed to its success. Many successful mobile health clinics cite their ability to foster trusting relationships.14–21 Qualitative research in such mobile health clinics has found that people value the informal, familiar environment in a convenient location, with staff who “are easy to talk to,” and that the staff's “marriage of professional and personal discourses” provides individuals the space to disclose information themselves.18,20,21 A communications academic argued that mobile health clinics’ unique use of space is important in facilitating these relationships; mobile health clinics park in spaces such as shopping centers, which gives a community atmosphere, and the constrained space inside renders the internal space a social as well as a health care space.21 More broadly, the Knowledgeable Neighbor model incorporates several recommendations from the Institute of Medicine's Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care,1 including
community health workers,
client-centered care focusing on client education and empowerment,
cultural competence training for staff,
stability and consistency of service provision within communities, and
staff diversity.
All of these have been shown to overcome barriers resulting from poor client-provider communication, mistrust, and disempowerment in minority communities.1,22–26 In addition, the Family Van removes financial barriers to accessing services, including the need for health insurance and copayments and logistical constraints, such as long journeys, difficulties making appointments, long waiting times, or complex administrative processes.1,2,6–8 That most clients were insured is evidence that lack of insurance is not the only factor promoting clients’ attendance and that mobile health clinics may continue to provide an important service even when health insurance coverage is high. It is notable that the intervention successfully attracted men, who have poorer health-seeking behavior.27
Acknowledgments
We would like to thank the Family Van team, clients, and funders and particularly Santos for agreeing to appear in the photograph and Mim Akins and Trishan Panch, the photographers.
Human Participant Protection
The Harvard Medical School institutional review board found this analysis of anonymous operational data exempt from review (CHS Study M19481-101). Individuals who appear in the figures consented to be photographed for Family Van marketing. They are not research subjects.
References
- 1.Institute of Medicine Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care: Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003 [PubMed] [Google Scholar]
- 2.US Department of Health and Human Services, Agency for Healthcare Research and Quality. National healthcare disparities report. 2010. Available at: http://www.ahrq.gov/qual/nhdr10/nhdr10.pdf. Accessed September 10, 2011 [Google Scholar]
- 3.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–1241 [DOI] [PubMed] [Google Scholar]
- 4.US Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2020: Disparities. Available at: http://healthypeople.gov/2020/about/disparitiesAbout.aspx. Accessed April 6, 2011
- 5.Maciosek MV, Coffield AB, Edwards NM, Flottemesch TJ, Goodman MJ, Solberg LI. Priorities among effective clinical preventive services: results of a systematic review and analysis. Am J Prev Med. 2006;31:52–61 [DOI] [PubMed] [Google Scholar]
- 6.Maxwell J, Cortes DE, Schneider KL, Graves A, Rosman B. Massachusetts’ health care reform increased access to care for Hispanics, but disparities remain. Health Aff (Millwood). 2011;30:1451–1460 [DOI] [PubMed] [Google Scholar]
- 7.Long SK, Masi PB. Access and affordability: an update on health reform in Massachusetts, fall 2008. Health Aff (Millwood). 2009;28:w578–w587 [DOI] [PubMed] [Google Scholar]
- 8.Clark CR, Soukup J, Govindarajulu U, Riden HE, Tovar DA, Johnson PA. Lack of access due to costs remains a problem for some in Massachusetts despite the state's health reforms. Health Aff (Millwood). 2011;30:247–255 [DOI] [PubMed] [Google Scholar]
- 9.James JJ. Survey of Mobile Health Units: Academy of Health Sciences (Army) Fort Sam Houston: Texas Health Care Studies Division; 1974 [Google Scholar]
- 10. Oriol NE, Vavasis A, Bennet J, Cote P, DeLorenzo D, Brownstein J. Putting mobile on the map, mapping the impact of this non-traditional health service delivery system. Paper presented at: APHA 138th Annual Meeting and Expo; November 9, 2010; Denver, CO.
- 11.Hsia AW, Castle A, Wing JJet al. Understanding reasons for delay in seeking acute stroke care in an underserved urban population. Stroke. 2011;42:1697–1701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Oriol NE. The Black community: taking control of our health. Presented at: Commonwealth of Massachusetts, Executive Office of Health and Human Services, Office of Minority Health Conference; 1999; Boston, MA.
- 13.Fryar CD, Hirsch R, Eberhardt MS, Yoon SS, Wright JD. Hypertension, high serum total cholesterol, and diabetes: racial and ethnic prevalence differences in U.S. adults, 1999-2006. NCHS Data Brief, No. 36 Hyattsville, MD: National Center for Health Statistics; 2010 [PubMed] [Google Scholar]
- 14.Nuttbrock L, McQuistion H, Rosenblum A, Magura S. Broadening perspectives on mobile medical outreach to homeless people. J Health Care Poor Underserved. 2003;14:5–16 [PubMed] [Google Scholar]
- 15.Mayernik D, Resick LK, Skomo ML, Mandock K. Parish nurse-initiated interdisciplinary mobile health care delivery project. J Obstet Gynecol Neonatal Nurs. 2010;39:227–234 [DOI] [PubMed] [Google Scholar]
- 16.Edgerley LP, El-Sayed YY, Druzin ML, Kiernan M, Daniels KI. Use of a community mobile health van to increase early access to prenatal care. Matern Child Health J. 2007;11:235–239 [DOI] [PubMed] [Google Scholar]
- 17.Diaz-Perez Mde J, Farley T, Cabanis CM. A program to improve access to health care among Mexican immigrants in rural Colorado. J Rural Health. 2004;20:258–264 [DOI] [PubMed] [Google Scholar]
- 18.Rodriguez KL, Appelt CJ, Young AJ, Fox AR. African American veterans’ experiences with mobile geriatric care. J Health Care Poor Underserved. 2007;18:44–53 [DOI] [PubMed] [Google Scholar]
- 19.Kahn RH, Moseley KE, Thilges JN, Johnson G, Farley TA. Community-based screening and treatment for STDs: results from a mobile clinic initiative. Sex Transm Dis. 2003;30:654–658 [DOI] [PubMed] [Google Scholar]
- 20.Guruge S, Hunter J, Barker K, McNally MJ, Magalhães L. Immigrant women's experiences of receiving care in a mobile health clinic. J Adv Nurs. 2010;66:350–359 [DOI] [PubMed] [Google Scholar]
- 21.Carmack HJ. "What happens on the van, stays on the van": the (re)structuring of privacy and disclosure scripts on an Appalachian mobile health clinic. Qual Health Res. 2010;20:1393–1405 [DOI] [PubMed] [Google Scholar]
- 22.Viswanathan M, Kraschnewski JL, Nishikawa Bet al. Outcomes and costs of community health worker interventions: a systematic review. Med Care. 2010;48:792–808 [DOI] [PubMed] [Google Scholar]
- 23.Scisney-Matlock M, Bosworth HB, Giger JNet al. Strategies for implementing and sustaining therapeutic lifestyle changes as part of hypertension management in African Americans. Postgrad Med. 2009;121:147–159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brach C, Fraser I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med Care Res Rev. 2000;57(suppl 1):181–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bloch MJ, Betancourt J, Green A. Overcoming racial and ethnic disparities in blood pressure control: a patient-centered approach to cross-cultural communication. J Clin Hypertens (Greenwich). 2008;10:589–591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Normand J. Culturally competent healthcare systems: a systematic review. Am J Prev Med. 2003;24(suppl 3):68–79 [DOI] [PubMed] [Google Scholar]
- 27.Viera AJ, Thorpe JM, Garrett JM. Effects of sex, age, and visits on receipt of preventive healthcare services: a secondary analysis of national data. BMC Health Serv Res. 2006;6:15. [DOI] [PMC free article] [PubMed] [Google Scholar]