Abstract
Background and Objectives
Youth with type 1 diabetes do not count carbohydrates (CHOs) accurately, yet it is an important strategy in blood glucose control. The study objective was to determine whether a nutrition education intervention would improve CHO counting accuracy and glycemic control.
Design
Randomized, controlled, nutrition intervention trial recruited February 2009 to February 2010.
Participants and Methods
Youth (12-18 years, n=101) with type 1 diabetes were screened to identify those with poor CHO counting accuracy, using a previously developed CHO counting accuracy test covering commonly consumed foods and beverage items presented in six mixed meals and two snacks. All participants (n=66, age=15 ± 3 yrs, 41 male, diabetes duration=6 ± 4 yrs, HbA1c=8.3 ± 1.1%) were randomized to the control or intervention group at the baseline visit. The intervention group attended a 90 minute class with a RD/CDE and twice kept three-day food records, which were used to review CHO counting progress.
Main Outcome Measures
CHO counting accuracy (measured as described above) and HbA1c were evaluated at baseline and three months to determine the effectiveness of the intervention.
Statistical Analyses
T-tests, Spearman correlations, and repeated measures models were used.
Results
At baseline, CHO content was over and underestimated in 16 and five of 29 food items, respectively. When foods were presented as mixed meals, participants either significantly over or underestimated 10 of the nine meals and four snacks. After three months of follow-up, HbA1c decreased in both the intervention and control groups by −0.19 ± 0.12% (p=0.12) and −0.08 ± 0.11% (p=0.51) respectively; however, the overall intervention effect was not statistically significant for change in HbA1c or CHO counting accuracy.
Conclusions
More intensive intervention may be required to improve adolescents’ CHO counting accuracy and nutrition management of type 1 diabetes. Further research is needed to translate nutrition education into improved health outcomes.
Keywords: Type 1 Diabetes, Carbohydrate Counting, Nutrition Education, Randomized Clinical Trial
Introduction
The primary goal in management of type 1 diabetes is to maintain blood glucose close to normal levels. Many patients with type 1 diabetes have HbA1c values that exceed American Diabetes Association (ADA) goals (<7.5% for 13-19 years old and <8% for 6-12 years old)1 and elevated postprandial glucose levels contribute to the failure to attain optimal glycemic control 2 . The total amount of carbohydrates (CHOs) consumed strongly predicts glycemic response; therefore, monitoring total CHOs by either exchanges or CHO counting to appropriately dose rapid acting insulin is critical to lower average glycemia (HbA1c) and to reduce glucose variability3-7.
Little data exist on accuracy of CHO counting in youth with type 1 diabetes, yet it is a recommended part of their daily care 5, 8-13. Using continuous subcutaneous insulin infusion (CSII) and multiple daily insulin injections (MDI) require patient (or parent) assessment of CHO amount in order to determine proper bolus insulin dosing 5,9. Thus, accurate estimation of total CHO to be consumed is critical to achieving glycemic control 3,4. CHO counting in treatment of youth with type 1 diabetes is not a new approach; however the adjustment of pre-meal doses based on the CHO content of meals has become more standard since the introduction of rapid acting insulin analogs, CSII and MDI 5.
There is very little research specifically providing evidence for the accuracy of CHO counting in youth with diabetes 8,10,13 and no standardized approach to assessing the accuracy of CHO counting is available. Koontz et al developed a pediatric questionnaire that evaluates knowledge about CHOs and insulin dosing calculations, but does not assess all aspects of CHO counting 14. While one study found 102 children and adolescents estimated CHO within 10-15 gm of the actual amount for 73% of 17 meals and snacks 13, this group has reported in a previous study that adolescents with type 1 diabetes do not count CHOs accurately and commonly either over or under estimate CHOs in a given meal. Only 11 of 48 (23%) adolescents estimated daily CHO within 10 grams of the true amount despite selection of common meals and only 15 (31%) estimated accurately within 20 g/day 8. The dose adjustment for normal eating (DAFNE) randomized controlled trial in the United Kingdom found that adult patients with type 1 diabetes, who were taught how to use flexible intensive insulin treatment with CHO-to-insulin ratios, improved HbA1c by 1% after six months and reported improved quality of life 15. In addition, a recent study conducted in Italy found that adults with type 1 diabetes, who attended a 4 week nutrition education program focusing on CHO counting, led to a significant decrease in HbA1c and fewer hypoglycemic events 16. However, no research exists on whether a nutrition education intervention focusing on CHO counting can improve adolescents’ ability to count CHOs and if such an improvement translates into better glycemic control.
There are two hypotheses for this study. The first hypothesis is that CHO counting is not practiced accurately among adolescents with type 1 diabetes. The second hypothesis is that a nutrition intervention conducted by a Registered Dietitian/Certified Diabetes Educator (RD/CDE) and aimed at improving CHO counting accuracy will result in improved CHO counting accuracy and as a result improved glycemic control in the intervention group compared to the control group. Therefore, the aim of this study was to evaluate CHO counting accuracy in adolescents with type 1 diabetes and to determine if a nutrition education intervention with a RD/CDE for those who do not count CHOs accurately, could improve CHO counting accuracy and as a result improved glycemic control. This study reports the results of a randomized, controlled, nutrition intervention trial.
Methods
Eligibility Criteria
Adolescents aged 12-18 years with type 1 diabetes (defined by American Diabetes Association criteria)17 for one year or more, seen at the Barbara Davis Center for Childhood Diabetes (BDC) and using insulin-to-CHO ratios for at least one meal a day were eligible for the study. Patients with celiac disease, type 1 diabetes with less than one-year duration, HbA1c>10% (at most recent clinic appointment) or non-English speaking were excluded.
Sample Selection
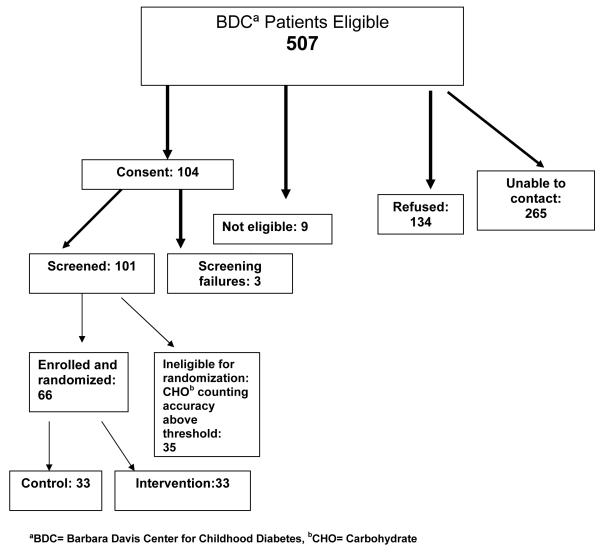
Patients coming to the BDC for their routine follow-up visit between February 2009 and February 2010 were contacted to see if they would be interested in participating in the study. A CHO counting accuracy test (as described below) was given based on a previously published method 8 and participants were included if they counted CHOs inaccurately. The a priori accuracy cut point was defined as participant’s CHO count for a meal within 10 gm CHO of the true CHO value for four out of six meals. A total of 104 individuals provided consent (three were screening failures, four intervention participants withdrew after the baseline visit); therefore, baseline data were analyzed for 101 participants and complete data were analyzed from 97 participants (Figure 1). Screening failures included two participants who were not CHO counting for at least one meal per day and one who had a developmental disorder. Sixty-six of the 101 eligible participants screened qualified for the intervention by scoring below the CHO counting accuracy cut point and were randomized into the intervention or control group (33 in each group).
Figure 1.
Flow Chart of recruitment and enrollment of participants in the Carbohydrate Counting in Adolescents with Type 1 Diabetes Study: Is More Intensive Education Needed?
Informed Consent
All participants provided written informed consent and/or assent and the study was approved by the Colorado Multiple Institutional Review Board.
Study Design
At the baseline visit 101 participants completed a CHO accuracy test 8 which involved assessing the CHO content (grams) for 29 food items (e.g., apple [snack] and cereal with milk and banana [breakfast]) presented as typical breakfasts, lunches, dinners, and snacks (six mixed meals, two snacks) commonly consumed by youth. Participants recorded their estimate of portion size, CHO content, and their frequency of consumption (from “<1/month” to “almost everyday”) for each individual food item presented in the six mixed meals and two snacks. The total meal CHO (grams) estimate of the six mixed meals was used for scoring the CHO counting accuracy test at the baseline visit. In order to assess how well participants estimate CHOs when evaluating a whole meal rather than individual foods, they were also asked to record their estimate of total meal CHO (grams) for an additional three meals and two snacks. All food items were selected as common by RDs after a review of diet records at the BDC and of dietary data collected from youth with diabetes in the SEARCH for Diabetes in Youth Study 18. Food items were presented either as food models or as real food, with some items presented as standard serving sizes and some self-portioned by the study participant. Packaged real food items were presented to participants with the food labels and participants were allowed to use these food labels in their estimations if they wanted. Study staff recorded the use of nutrition labels by participants during the study visit (for foods that were presented with a nutrition label). For self-portioned foods, the actual weight of the food served was recorded out of sight of the participant. The amount of CHO in each food was determined by either the nutrition label for the real food that came in packaging; by the Nasco Food Replica Nutrition Guide (based on USDA Standard Reference for Nutrient Composition) for all food models or the Nutrient Data System for Research (NDSR)(Version 2007, Nutrition Coordinating Center (NCC), University of Minnesota, Minneapolis, MN) for real foods that were self-portioned by the study participant. Participants were also given a sheet with two labels with Nutrition Facts and asked to calculate CHO grams for a given serving.
Data Collection
At baseline an interviewer-administered questionnaire assessed CHO counting education received from a RD, duration of CHO counting, family/friend support for CHO counting, and pattern of CHO counting (at which meals and snacks they count CHOs and how often). Participants also completed a self-administered questionnaire of parental support (collaborative scale) of their diabetes management 19,20. This questionnaire was completed by the participant only without input from the parent.
A demographic/medical history questionnaire was also completed, which included information such as date of birth, ethnicity, and routine clinical data such as height, weight, Body Mass Index (BMI) (kg/m2), and insulin dosing (Table 1). As part of the participant’s clinical visit concurrent with the study visit (baseline and final visit), HbA1c was measured by blood sample on a Bayer DCA 2000+ (Siemens/Bayer, Deerfield, IL) and BMI was calculated by a computer program after obtaining height on a wall-mounted stadiometer (Seca, Hamburg, Germany) and weight on a clinic electronic scale (Detecto,Webb City, MO). Height and weight were measured in duplicate to 0.1 cm and 0.1 kg increments respectively.
Table 1.
Baseline characteristics of the participants who qualified versus those who did not qualify for the study and those in the intervention group versus control group in the Carbohydrate Counting in Adolescents with Type 1 Diabetes Study: Is More Intensive Education Needed?
| Qualifiers (n=66) |
Non- qualifiers (n=35) |
Intervention
(n= 33) |
Control
(n= 33) |
|||
|---|---|---|---|---|---|---|
| mean±SD | mean±SD | p a | mean±SD | mean±SD | p a | |
| Age, years | 15.1± 2.8 | 14.8 ± 3.5 | 0.58 | 15.7± 3.4 | 14.5 ± 1.8 | 0.083 |
| Diabetes duration, years |
5.5 ± 3.5 | 6.9 ± 3.5 | 0.064 | 5.5 ± 3.5 | 5.6 ± 3.4 | 0.83 |
| BMIc, kg/m2 | 22.1 ± 3.8 | 20.7 ± 2.6 | 0.057 | 22.3 ± 3.7 | 21.9 ± 3.8 | 0.63 |
| HbA1c, % | 8.33 ± 1.09 | 8.10 ± 0.92 | 0.29 | 8.41 ± 1.04 | 8.25 ± 1.14 | 0.54 |
| Blood glucose | 190.3 ± 70.6 | 206.1± 61.9 | 0.27 | 193.8 ± 79.6 | 186.8 ± 61.4 | 0.69 |
| Insulin total | 56.8 ± 26.5 | 48.7 ± 14.7 | 0.10 | 59.5 ± 17.0 | 54.2 ± 33.3 | 0.42 |
| Basal % | 47.2 ± 12.8 | 45.1 ± 10.1 | 0.43 | 47.4 ± 10.9 | 47.1 ± 14.5 | 0.93 |
| Bolus % | 52.8 ± 12.8 | 54.9 ± 10.0 | 0.44 | 52.6 ± 10.9 | 52.9 ± 14.5 | 0.93 |
| Number of boluses per day |
5.8 ± 2.2 | 7.3 ± 2.8 | 0.009 | 6.0 ± 1.7 | 5.6 ± 2.6 | 0.59 |
| n(%) | n(%) | p b | n(%) | n(%) | p b | |
| Gender | ||||||
| Female | 25(38) | 18(51) | 8(24) | 17(52) | ||
| Male | 41(62) | 17(49) | 0.21 | 25(76) | 16(48) | 0.041 |
| Ethnicity | ||||||
| Non-Hispanic | ||||||
| whites | 60(91) | 33(94) | 30(91) | 30(91) | 1.0 | |
| Other | 6(9) | 2(6) | 0.71 | 3(9) | 3(9) | |
| Parent education | ||||||
| Associate degree and higher |
51(77) | 21(60) | 22(67) | 29(88) | ||
| Less than associate degree |
15(23) | 14(40) | 0.10 | 11(33) | 4(12) | 0.076 |
| Family income, US dollars 50, 000 and more |
46(78) | 28(90) | 20(71) | 26(84) | ||
| Less than 50,000 |
13(22) | 3(10) | 0.25 | 8(29) | 5(16) | 0.35 |
| Insulin mode | ||||||
| Injections | 13(20) | 5(14) | 7(21) | 6(18) | ||
| Pump | 53(80) | 30(86) | 0.59 | 26(79) | 27(82) | 1.0 |
Pooled t-test;
Fisher exact two-sided test,
BMI= Body Mass Index
At their three to four month follow-up (routine clinic visit/final visit), all participants repeated the CHO counting accuracy test conducted to determine if their accuracy had improved. The CHO counting questionnaire, demographic/medical history questionnaire and parental support questionnaire were also repeated at this visit.
Usual Practice
Usual CHO counting education for patients at the BDC includes meeting with a RD/CDE for 60 minutes at diagnosis, attending a 120 minute class at one week after diagnosis and an individual visit with a RD/CDE at one month after diagnosis. All pump patients also attend a 60 minute class on CHO counting and complete food records for evaluation of CHO counting accuracy and insulin-to-CHO ratio dosing adjustments prior to pump initiation. All patients can meet with a RD at each quarterly visit if needed, but the frequency of those visits varies widely. Patients at the BDC are taught to match insulin dose to the total amount of CHO grams they are eating. In addition, food records are evaluated periodically for CHO counting accuracy and insulin-to-CHO ratio dosing adjustments. All participants received this education as part of their routine care.
Randomized Controlled Trial /Nutrition Education Intervention
Participants were randomly assigned to the nutrition intervention group or the control group using a computer generated scheme developed by our staff biostatistician.
Control
Participants randomized to the control group received a handout with the CHO content of commonly eaten foods and a list of CHO counting resources. RDs or a study staff member with a master’s degree in nutrition briefly (5 minutes) reviewed the handouts and discussed the importance of CHO counting and gave the participant the phone number of the staff RD to call with questions.
Intervention
In addition to the above, the intervention group attended a CHO counting class and completed two sets of three day food records as described below.
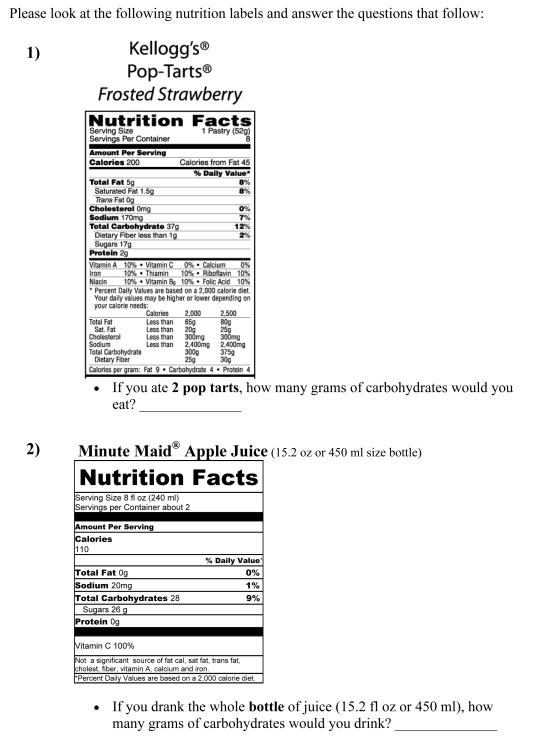
Carbohydrate Counting Class
The intervention targeted the adolescent and was designed by RDs/CDEs to improve CHO counting accuracy and insulin dosing. This was an interactive 90 minute class, taught by the same RD, CDE following a planned curriculum with hands on activities and time for discussion. The class applied knowledge gained by RDs from previous studies conducted by this research group about areas of deficiency that this population encounters when estimating CHO content of foods 8. RDs adapted the current nutrition education program, used as part of standard clinical care at the BDC, to better address performance deficits in CHO counting in this patient population. Targeted review areas included calculating CHOs from food labels, estimating portions accurately when eating out or at home with no label available, reviewing CHO content of foods that most patients eat often, determining CHO content of restaurant meals, and calculating insulin doses using an insulin-to-CHO ratio and blood glucose correction factor. To help participants estimate portions, real foods including pasta, chips, cereal, juice and milk were used along with food models. Participants portioned out the amounts of foods that they usually eat and then used measuring cups to determine what portion size and CHO content the food contained.
Participants randomized to the intervention group were scheduled for a class while at the baseline study visit, if possible. The classes were offered weekly and were attended by 1-2 study participants. The original intention was to have a larger, group class, but because of difficulty scheduling within the protocol’s timeframe (1-2 weeks after baseline visit) and the participants’ schedules, this was not possible. Family members were also offered the opportunity to attend and a total of seventeen family members attended, usually being one parent with the participant. Participants were given measuring cups, a food scale and The Calorie King Calorie, Fat and Carbohydrate Counter book 21 to keep for home use and to help with ease and accuracy of CHO counting. Participants were instructed by the RD/CDE at the end of the class on how to complete food record forms.
Completion of Food Records and Follow-Up with Registered Dietitians
As part of the intervention, participants completed the three day food record form at approximately two weeks and eight weeks after the Carbohydrate Counting class for review of CHO counting accuracy. The RD called all participants one week in advance to remind them to complete the food records. The RD followed-up with the participant or parent (whomever completed the forms) by phone to review the food records and gave feedback on CHO counting, correcting any inaccuracies in CHO content estimation and adjusting insulin doses including insulin-to-CHO ratios or basal insulin based on blood glucose results taken before and two hours after meals and recorded in the records. Records indicating topic and problem areas discussed were kept for each phone consult. Other topics discussed included adjustments for high fat meals using extra insulin or extended boluses, bolusing before eating, checking blood glucose more frequently, restaurant eating, treatment of hypoglycemia and whether participants weighed and measured foods for the records.
Statistical Methods
Frequencies, means and standard deviations were calculated as descriptive statistics. nQuery Advisor (version 4.0, 2000, Statistical Solutions, Los Angeles, CA) was used to calculate power for the difference in mean differences in CHO estimates versus actual and HbA1c. A total of 29 participants in each arm provided 80% power to detect a 0.75 difference in HbA1c between the intervention and control groups assuming a standard deviation of 1.0%. Sixty six participants were recruited to account for potential drop outs. Accuracy of CHO counting was determined as a difference between actual and participant-estimated CHO content (in grams) for each food and meal. T-tests were used to assess the significance of over or underestimation of CHO content. The effect of the intervention on the outcome variable was assessed by fitting the repeated measurements model using SAS MIXED procedure. Spearman rank correlation was used to test the associations when the normality assumption was violated. All analyses were performed using SAS (version 9.2, 2010, SAS Institute Inc., Cary, NC). A p-value <0.05 was considered statistically significant.
Results
Table 1 describes the baseline characteristics of the 101 adolescents screened for this study and the 66 who were randomized into the control and intervention groups. There were significantly more boys (25) than girls (eight) who were randomized to the intervention group (p=0.041) (Table 1). Those who did not qualify were similar to those who qualified in most characteristics including age and HbA1c, except that non-qualifiers on pumps bolused significantly more frequently (p=0.009) had diabetes for a slightly longer duration (not significant, p=0.064), and had a slightly lower BMI (not significant, p=0.057). Participants who were below the CHO counting accuracy cut point (n=66) at baseline significantly overestimated CHO amounts in many individual foods including milk, syrup, orange juice, chips, peanut butter, jelly, carrots, broccoli, chicken nuggets, cheese, hamburger, spaghetti, Goldfish® crackers, and waffles (Table 2). They underestimated CHO amounts in some individual foods as well, including cereal, banana, fries, barbecue sauce and regular soda. When evaluating accuracy when foods were presented as meals, participants significantly under or overestimated CHO amounts in 10 of the nine meals and four snacks (Table 3).
Table 2.
Carbohydrate counting accuracy of control and intervention participants at baseline and follow-up, by individual foods
| Qualifiers | CHOa estimate accuracy,gb | |||||
|---|---|---|---|---|---|---|
| Food | Average CHO, g |
group | Baseline | Follow-up | p- valuec |
p-valued |
| Cereale | 41.6 | control | −3.7 | −3.7 | 1.00 | 0.90 |
| intervention | −6.0 | −5.5 | 0.86 | |||
| Milk (with cereal) e | 7.9 | control | 5.7 | 6.0 | 0.71 | 0.19 |
| intervention | 4.9 | 3.4 | 0.15 | |||
| Banana | 27.0 | control | −4.4 | −2.6 | 0.22 | 0.41 |
| intervention | −8.3 | −4.6 | 0.023 | |||
| Mac’n’cheese | 45.7 | control | 0.7 | 1.3 | 0.82 | 0.98 |
| intervention | −9.4 | −8.7 | 0.80 | |||
| Carrots | 4.9 | control | 4.1 | 3.6 | 0.71 | 0.28 |
| intervention | 3.3 | 4.8 | 0.25 | |||
| Snack milke | 11.4 | control | 5.0 | 4.3 | 0.65 | 0.38 |
| intervention | 3.1 | 4.4 | 0.44 | |||
| Cookiese | 30.0 | control | 0.6 | 1.1 | 0.81 | 0.58 |
| intervention | 0.4 | −0.7 | 0.58 | |||
| Chicken nuggetse | 16.0 | control | 5.3 | 5.4 | 0.95 | 0.77 |
| intervention | 3.8 | 3.2 | 0.74 | |||
| Friese | 48.0 | control | −2.9 | −4.4 | 0.49 | 0.11 |
| intervention | −6.3 | −2.7 | 0.11 | |||
| Barbeque sauce | 12.0 | control | −1.6 | −2.6 | 0.41 | 0.19 |
| intervention | −3.4 | −2.1 | 0.31 | |||
| Soda | 86.0 | control | −11.2 | −8.6 | 0.60 | 0.47 |
| intervention | −12.8 | −15.2 | 0.62 | |||
| Goldfish® crackerse | 20.5 | control | 3.1 | −1.1 | 0.032 | 0.45 |
| intervention | 3.2 | 1.1 | 0.29 | |||
| String cheese | 0.0 | control | 5.3 | 4.1 | 0.15 | 0.64 |
| intervention | 4.7 | 3.0 | 0.042 | |||
| Eggos® | 27.0 | control | 8.1 | 5.4 | 0.24 | 0.29 |
| intervention | 6.7 | 7.5 | 0.74 | |||
| Syrupe | 12.6 | control | 12.4 | 12.7 | 0.93 | 0.62 |
| intervention | 13.6 | 12.2 | 0.55 | |||
| Orange juicee | 23.8 | control | 5.2 | 3.4 | 0.41 | 0.60 |
| intervention | 3.1 | 2.9 | 0.94 | |||
| Burger | 0.0 | control | 2.7 | 3.1 | 0.59 | 0.040 |
| intervention | 4.3 | 2.8 | 0.021 | |||
| Bun | 26.1 | control | −0.7 | −3.4 | 0.085 | 0.75 |
| intervention | −0.7 | −2.7 | 0.21 | |||
| Chipse | 16.1 | control | 6.8 | 6.0 | 0.63 | 0.29 |
| intervention | 4.7 | 6.4 | 0.32 | |||
| Milke | 11.9 | control | 3.8 | 3.0 | 0.54 | 0.96 |
| intervention | 2.2 | 1.5 | 0.61 | |||
| Spaghetti | 35.8 | control | 9.1 | 12.5 | 0.32 | 0.54 |
| intervention | 3.3 | 9.8 | 0.075 | |||
| Marinara | 11.7 | control | 1.6 | 1.5 | 0.95 | 0.68 |
| intervention | −1.9 | −1.0 | 0.61 | |||
| Broccoli | 2.9 | control | 4.1 | 3.4 | 0.37 | 0.014 |
| intervention | 2.9 | 5.0 | 0.011 | |||
| Snapple®e | 2.0 | control | 0.9 | 0.9 | 0.99 | 0.79 |
| intervention | 0.1 | −0.2 | 0.70 | |||
| Bread | 30.0 | control | −0.9 | −2.0 | 0.38 | 0.40 |
| intervention | −3.1 | −2.7 | 0.76 | |||
| Peanut butter | 7.0 | control | 4.0 | 3.7 | 0.83 | 0.31 |
| intervention | 2.0 | 3.3 | 0.23 | |||
| Jelly | 13.0 | control | 4.2 | 4.3 | 0.94 | 0.77 |
| intervention | 3.8 | 4.6 | 0.63 | |||
| Apple | 21.8 | control | 0.2 | 1.2 | 0.36 | 0.81 |
| intervention | −1.4 | −0.8 | 0.59 | |||
| Browniee | 40.0 | control | 4.8 | 2.3 | 0.39 | 0.11 |
| intervention | −0.9 | 3.4 | 0.17 | |||
CHO = carbohydrate;
accuracy was defined as a difference between actual and estimated CHO;
significance of change between baseline and follow-up accuracy within the group, adjusted for age, gender, and diabetes duration;
significance of the overall intervention effect;
Foods presented with nutrition labels in study visit
Table 3.
Carbohydrate counting accuracy at baseline and follow-up, by meals
| Qualifiers | CHOa estimate accuracy, gb |
||||||
|---|---|---|---|---|---|---|---|
| Meal | Average CHO, g |
Group | Baseline | Follow-up | p- valuec |
p- valued |
|
| Day 1 | breakfast | 52.3 | control | −8.1 | −6.2 | 0.39 | 0.91 |
| intervention | −12.3 | −10.7 | 0.50 | ||||
| lunch | 83.4 | control | −14.9 | −15.5 | 0.86 | 0.29 | |
| intervention | −18.5 | −13.8 | 0.19 | ||||
| dinner | 48.9 | control | 9.2 | 7.9 | 0.70 | 0.036 | |
| intervention | 1.8 | 10.7 | 0.012 | ||||
| snack | 66.0 | control | 7.7 | 6.3 | 0.65 | 0.32 | |
| intervention | 2.2 | 5.1 | 0.35 | ||||
| Day 2 | breakfast | 76.6 | control | −2.4 | −0.3 | 0.54 | 0.92 |
| intervention | −9.2 | −6.5 | 0.46 | ||||
| lunch | 92.0 | control | 10.2 | 10.3 | 0.99 | 0.71 | |
| intervention | −2.4 | 0.2 | 0.59 | ||||
| dinner | 162.0 | control | −10.5 | −10.7 | 0.97 | 0.82 | |
| intervention | −18.2 | −16.5 | 0.78 | ||||
| snack | 20.5 | control | 8.3 | 3.0 | 0.014 | 0.62 | |
| intervention | 8.1 | 4.3 | 0.085 | ||||
| Day 3 | breakfast | 63.4 | control | 25.7 | 21.5 | 0.35 | 0.60 |
| intervention | 23.3 | 22.4 | 0.85 | ||||
| lunch | 54.0 | control | 12.6 | 8.5 | 0.15 | 0.67 | |
| intervention | 10.6 | 8.2 | 0.43 | ||||
| dinner | 52.4 | control | 15.6 | 18.3 | 0.52 | 0.29 | |
| intervention | 4.3 | 13.5 | 0.040 | ||||
| snack | 71.8 | control | 7.4 | 7.3 | 0.97 | 0.51 | |
| intervention | 1.3 | 4.1 | 0.38 | ||||
CHO = carbohydrate;
accuracy was defined as a difference between actual and estimated CHO;
significance of change between baseline and follow-up accuracy within the group, adjusted for age, gender,and diabetes duration;
significance of the overall intervention effect.
There was no association between previous reported CHO education, receiving help while counting CHO, duration of CHO counting and CHO counting accuracy. The mean length of time that participants reported they had been CHO counting was 45 ± 28 months (6-108 months) with no significant difference between the groups. At baseline, 40 of the participants reported not having received CHO counting education from a RD for over one year with no significant difference between groups. Fifty-five of 66 participants reported receiving help with CHO counting from their mother with dinner being the most frequent meal for which they reported receiving help. There was no significant difference between groups in these areas and the distribution of parents helping across the groups was similar. There was a statistically significant negative correlation between HbA1c and the collaborative scale, such that adolescents who collaborated more with their parents had lower HbA1c (r=-0.264, p=0.008). There was also a negative correlation between frequency of eating a food and accurate estimates of CHO in milk, string cheese, waffles and apple. When evaluating use of labels and its correlation with accuracy of CHO estimates, accuracy was significantly better for some foods when using labels (crackers, nuggets, fries, Snapple®), but not for others.
HbA1c for the intervention and control groups were similar at baseline (8.41 ± 0.19%, 8.25 ± 0.19%, respectively). After three months of follow-up, HbA1c decreased to 8.22 ± 0.18 (−0.19 ± 0.12% (p=0.12)) in the intervention group and to 8.17 ± 0.18% (−0.08 ± 0.11% (p=0.51)) for the control group and the overall intervention effect was not statistically significant (p=0.49).
At the three month follow-up visit 29 of the 33 control participants and 26 of the 29 intervention participants continued to be below the CHO counting accuracy cut point. There were limited statistically significant improvements in CHO counting accuracy on the CHO counting test from baseline to final visit in the intervention or control group (Table 2 and 3).
Discussion
The findings in this study demonstrate that adolescents with type 1 diabetes do not accurately count CHOs and commonly either over or under estimate CHO grams in a given meal. A previous study conducted at the Barbara Davis Center found similar results to the current study in the same age group 8. Smart et al assessed CHO counting accuracy in eight to 18 year olds in Australia and the United Kingdom and found that for 73% of the meals, youth estimated CHOs within 10-15 gm of the actual CHO and concluded that they CHO count reasonably accurately 13. By the accuracy definition used in this study, many of those participants would not be considered accurate. Another study evaluating CHO counting accuracy and precision in youth looked at parents of four to12 years olds using diet recalls and found that on average, parent estimates of CHO intake were 120% of nutrition database calculation and greater precision (consistency), but not accuracy was associated with lower HbA1c 10. Perhaps this indicates that if patients consistently overestimate or underestimate the CHO content of foods, their insulin dose is adjusted accordingly and this type of inaccuracy does not affect blood glucose control adversely as expected. A limitation of this study may be that accuracy was assessed on 24 hour dietary recalls of parents rather than actual intake over several days.
While it was expected that participants’ CHO estimates for foods eaten more frequently would be more accurate, that was not the case for all foods. A possible explanation is that some foods are easier to memorize or are more standard than others. Smart et al found that foods in labeled packages were estimated most accurately 13. But in this study, participants who used labels to estimate CHO were not more accurate than those who did not use labels for many of the foods, and that may point to the difficulty that adolescents have in estimating portion size. Therefore, RDs need to continually focus on helping adolescents estimate portions using real food and food models and encourage them to check the serving sizes of foods they are eating by measuring portions regularly. This study found that there was no association between duration of CHO counting and accuracy, while Smart et al found that adolescents who were CHO counting for the longest duration were the least accurate 13. The assumption in clinical care is that the longer patients count CHOs, the more accurate they would be. Because this does not appear to be the case, RDs need to meet with patients regularly for reeducation. Parental support as measured on the collaborative scale was associated with better HbA1c, supporting the idea that adolescents do better when their parents continue to be involved in their diabetes care and this needs to be encouraged in the clinical setting.
Intervention studies conducted on patients with type 1 diabetes have only included adults and were comprised of four to five sessions of education that resulted in reductions in HbA1c15,16. But those participants had no experience with CHO counting or adjusting insulin for CHOs prior to the study. The participants in this study were already adjusting insulin for CHOs and had previous education on CHO counting. Baseline HbA1c levels (Table 1) for both the control and intervention groups were higher than the ADA goal of <7.5%11 for this age group, confirming that some type of intervention was needed to help optimize their control. A limitation of this study was the lack of an evidence based model to inform development of an intervention for this specific population.
Comparing the intervention and control groups, there was no statistically significant difference in CHO counting accuracy or HbA1c after three months of intervention and follow-up. These negative outcomes may be due to several reasons including limitations in the study. First, perhaps a one time class with phone feedback on two sets of three day food records from a RD/CDE is not intensive enough education to improve knowledge, CHO estimation and accuracy skills. Second, participants may not have measured portions as directed when completing food records and for some participants, parents were completing the records and still doing much of the CHO counting, so the child may not have learned as much. Third, the CHO counting test used may not have reflected the actual foods that the participants eat frequently and their true ability to estimate CHOs at home. Additionally, although this method has been used previously to evaluate CHO counting skills 8, it may lack sufficient resolution to capture changes. Fourth, many variables affect HbA1c and glycemic control including illness, puberty, change in activity levels and stress. These factors could not be controlled and were not measured in this study. While CHO counting is the most commonly used method for determining the insulin bolus dose for meals and snacks, other methodologies have been proposed that also account for fat and protein 22,23. However, these methods add complexity to the bolus dose decision and may prove to be too complex for some families. Additional data on these methods is required to determine their affect on glycemic control. Missed meal or snack boluses and timing of meal doses are also important factors affecting postprandial hyperglycemia and HbA1c. Missed or late boluses commonly occur in adolescents and may also explain some of the challenge in effecting change in glycemic control in this group compared to adults 24. Though these factors were not tracked in this study, it would not be expected that missed doses or late bolusing would have occurred disproportionately in the two groups. It is also possible that continuous glucose monitoring may have detected differences in post-prandial glycemia, but any such possible differences were insufficient to have a significant effect on HbA1c between the two groups. Finally, there were several intervention participants who did not follow recommendations given by the RD/CDE to adjust insulin doses. Of the 101 participants screened for the randomized study, 70% of the boys qualified compared to 58% of the girls and more boys than girls were allocated to the intervention arm. Also, although a larger study population may have resulted in a statistically significant difference between the two groups, the magnitude of the difference in HbA1c at 3 months (0.11 ± 0.16%) would not be considered clinically important since a decrease of 0.3% to 0.5% would need to be achieved to have been clinically meaningful.
Conclusions
Bolusing rapid-acting insulin for meals (CHOs) is a cornerstone of current management of type 1 diabetes; however, this study demonstrates that adolescents do not count CHOs accurately. Little data exist on how health-care providers can optimize advice on this important aspect of diabetes care performed multiple times daily and educating adolescents with type 1 diabetes on CHO counting is a stepping stone to improving glycemic control. In addition, educating adolescents and helping them make changes in their diabetes care has its unique challenges as compared to adults.
This study found that improvements in CHO counting accuracy are difficult to achieve with one class and phone feedback on two sets of three day food records by a RD/CDE. Parental support was found to be associated with better HbA1c, therefore clinicians need to assess this aspect of diabetes care and encourage more involvement in their care and education, if found to be inadequate. Also, continued emphasis by RDs on estimating portions and measuring foods may be helpful. Further research is needed to identify cost effective approaches to improve this skill which may include multiple classes, including parents in the intervention more actively and using media. Until full development of a closed-loop artificial pancreas, insulin dosing decisions will continue to be an everyday challenge for patients with type 1 diabetes and their parents. Therefore, these data can serve to inform future studies designed to improve dietary management of type 1 diabetes.
Figure 2.
Label Reading Activity
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Gail Spiegel, Barbara Davis Center for Childhood Diabetes, Department of Pediatrics University of Colorado Denver, 1775 Aurora Court, MS A140, PO Box 6511, Aurora, CO 80045.
Andrey Bortsov, Department of Anesthesiology, The University of North Carolina at Chapel Hill N2201 UNC Hospitals CB 7010, Chapel Hill, NC 27599-7010 Phone: 919.843.5353 Fax: 919.966.7193 abortsov@aims.unc.edu; Center for Research in Nutrition and Health Disparities University of South Carolina, Columbia, SC 29208.
Franziska K. Bishop, Barbara Davis Center for Childhood Diabetes, Department of Pediatrics University of Colorado Denver, 1775 Aurora Court, MS A140, PO Box 6511 Aurora, CO 80045 Phone: 303.724.6764 Fax: 303.724.6779 franziska.bishop@ucdenver.edu.
Darcy Owen, Barbara Davis Center for Childhood Diabetes, Department of Pediatrics University of Colorado Denver, 1775 Aurora Court, MS A140, PO Box 6511 Aurora, CO 80045 Phone: 303.724.6702 Fax: 303.724.6779 Darcy.owen@ucdenver.edu.
Georgeanna J. Klingensmith, Barbara Davis Center for Childhood Diabetes, Department of Pediatrics University of Colorado Denver, 1775 Aurora Court, MS A140, PO Box 6511 Aurora, CO 80045 Phone: 303.724.6717 Fax: 303.724.6779 georgeanna.klingensmith@ucdenver.edu.
Elizabeth J. Mayer-Davis, Departments of Nutrition and Medicine School of Public Health and School of Medicine 2211 McGavran-Greenberg Hall CB 7461 University of North Carolina at Chapel Hill, Chapel Hill, NC 27599-7461 Phone: 919.966.1991 Fax: 919.966.7216 ejmayer_davis@unc.edu.
David M. Maahs, Barbara Davis Center for Childhood Diabetes, Department of Pediatrics University of Colorado Denver, 1775 Aurora Court, MS A140, PO Box 6511, Aurora, CO 80045 Phone: 303.724.6706 Fax: 303.724.6779 david.maahs@ucdenver.edu.
References
- 1.Danne T, Mortensen HB, Hougaard P, et al. Persistent differences among centers over 3 years in glycemic control and hypoglycemia in a study of 3,805 children and adolescents with type 1 diabetes from the Hvidore Study Group. Diabetes Care. 2001;24(8):1342–1347. doi: 10.2337/diacare.24.8.1342. [DOI] [PubMed] [Google Scholar]
- 2.Postprandial blood glucose. American Diabetes Association. Diabetes Care. 2001;24(4):775–778. doi: 10.2337/diacare.24.4.775. [DOI] [PubMed] [Google Scholar]
- 3.Sheard NF, Clark NG, Brand-Miller JC, et al. Dietary carbohydrate (amount and type) in the prevention and management of diabetes: a statement by the american diabetes association. Diabetes Care. 2004;27(9):2266–2271. doi: 10.2337/diacare.27.9.2266. [DOI] [PubMed] [Google Scholar]
- 4.Rabasa-Lhoret R, Garon J, Langelier H, Poisson D, Chiasson JL. Effects of meal carbohydrate content on insulin requirements in type 1 diabetic patients treated intensively with the basal-bolus (ultralente-regular) insulin regimen. Diabetes Care. 1999;22(5):667–673. doi: 10.2337/diacare.22.5.667. [DOI] [PubMed] [Google Scholar]
- 5.Bantle JP, Wylie-Rosett J, Albright AL, et al. Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2008;31(Suppl 1):S61–S78. doi: 10.2337/dc08-S061. [DOI] [PubMed] [Google Scholar]
- 6.Delahanty LM, Halford BN. The role of diet behaviors in achieving improved glycemic control in intensively treated patients in the Diabetes Control and Complications Trial. Diabetes Care. 1993;16(11):1453–1458. doi: 10.2337/diacare.16.11.1453. [DOI] [PubMed] [Google Scholar]
- 7.Gillespie SJ, Kulkarni KD, Daly AE. Using carbohydrate counting in diabetes clinical practice. J Am Diet Assoc. 1998;98(8):897–905. doi: 10.1016/S0002-8223(98)00206-5. [DOI] [PubMed] [Google Scholar]
- 8.Bishop FK, Maahs DM, Spiegel G, et al. The carbohydrate counting in adolescents with type 1 diabetes (CCAT) study. Diabetes Spectrum. 2010;22(1):56–62. [Google Scholar]
- 9.Kawamura T. The importance of carbohydrate counting in the treatment of children with diabetes. Pediatr Diabetes. 2007;8(Suppl 6):57–62. doi: 10.1111/j.1399-5448.2007.00287.x. [DOI] [PubMed] [Google Scholar]
- 10.Mehta SN, Quinn N, Volkening LK, Laffel LM. Impact of carbohydrate counting on glycemic control in children with type 1 diabetes. Diabetes Care. 2009;32(6):1014–1016. doi: 10.2337/dc08-2068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Silverstein J, Klingensmith G, Copeland K, et al. Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care. 2005;28(1):186–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- 12.Smart C, slander-van VE, Waldron S. Nutritional management in children and adolescents with diabetes. Pediatr Diabetes. 2009;10(Suppl 12):100–117. doi: 10.1111/j.1399-5448.2009.00572.x. [DOI] [PubMed] [Google Scholar]
- 13.Smart CE, Ross K, Edge JA, King BR, McElduff P, Collins CE. Can children with Type 1 diabetes and their caregivers estimate the carbohydrate content of meals and snacks? Diabet Med. 2010;27(3):348–353. doi: 10.1111/j.1464-5491.2010.02945.x. [DOI] [PubMed] [Google Scholar]
- 14.Koontz MB, Cuttler L, Palmert MR, et al. Development and validation of a questionnaire to assess carbohydrate and insulin-dosing knowledge in youth with type 1 diabetes. Diabetes Care. 2010;33(3):457–462. doi: 10.2337/dc09-0390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating (DAFNE) randomised controlled trial. BMJ. 2002;325(7367):746–751. doi: 10.1136/bmj.325.7367.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scavone G, Manto A, Pitocco D, et al. Effect of carbohydrate counting and medical nutritional therapy on glycaemic control in Type 1 diabetic subjects: a pilot study. Diabet Med. 2010;27(4):477–479. doi: 10.1111/j.1464-5491.2010.02963.x. [DOI] [PubMed] [Google Scholar]
- 17.Summary of Revisions for the 2002 Clinical Practice Recommendations. Diabetes Care. 2002;25(Suppl 1):3S. [PubMed] [Google Scholar]
- 18.Mayer-Davis EJ, Nichols M, Liese AD, et al. Dietary intake among youth with diabetes: the SEARCH for Diabetes in Youth Study. J Am Diet Assoc. 2006;106(5):689–697. doi: 10.1016/j.jada.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 19.Nansel TR, Rovner AJ, Haynie D, et al. Development and validation of the collaborative parent involvement scale for youths with type 1 diabetes. J Pediatr Psychol. 2009;34(1):30–40. doi: 10.1093/jpepsy/jsn058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wysocki T, Nansel TR, Holmbeck GN, et al. Collaborative involvement of primary and secondary caregivers: associations with youths’ diabetes outcomes. J Pediatr Psychol. 2009;34(8):869–881. doi: 10.1093/jpepsy/jsn136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Borushek A. The CalorieKing® Calorie Fat & Carbohydrate Counter 2009. 2009 ed Family Health Publications; 2010. [Google Scholar]
- 22.Kordonouri O, Hartmann R, Remus K, et al. Supplementary fat plus protein (cfp) counting for insulin bolus calculation in children with pump therapy is superior to conventional carbohydrate (carb) counting. (Abstract) Diabetes. 2010;59(Suppl 1):A81. [Google Scholar]
- 23.Pankowska E, Szypowska A, Lipka M, Szpotanska M, Blazik M, Groele L. Application of novel dual wave meal bolus and its impact on glycated hemoglobin A1c level in children with type 1 diabetes. Pediatr Diabetes. 2009;10(5):298–303. doi: 10.1111/j.1399-5448.2008.00471.x. [DOI] [PubMed] [Google Scholar]
- 24.Burdick J, Chase HP, Slover RH, et al. Missed insulin meal boluses and elevated hemoglobin A1c levels in children receiving insulin pump therapy. Pediatrics. 2004;113(3 Pt 1):e221–e224. doi: 10.1542/peds.113.3.e221. [DOI] [PubMed] [Google Scholar]