Abstract
Background and purpose
Primary spontaneous osteonecrosis of the knee is a painful lesion in the elderly without any known cause. The onset of pain is usually acute. The prognosis is poor with high frequency of osteoarthritis, joint surface collapse, and subsequent knee surgery. In the present study, we determined whether bisphosphonates can prevent the joint surface collapse by delaying the post-necrotic remodeling.
Patients and methods
Between 2006 and 2009, 17 consecutive patients (mean age 68 years) with clinical and radiographic signs of knee osteonecrosis were identified and given alendronate, 70 mg perorally, once a week for a minimum of 6 months. The patients were followed clinically, radiographically, and by MRI.
Results
10 of the 17 patients did not develop osteoarthritis (group A), 4 patients developed mild osteoarthritis but no knee joint surface collapse (group B), and 3 patients had a joint surface collapse (group C). 2 of the 3 patients in group C—as compared to none in the other groups—stopped medication prematurely, due to side effects.
Interpretation
Compared to a previous, untreated series of osteonecrosis patients at our hospital, the clinical results in the present series appeared better. 59% of the patients had a complete radiographic recovery, as compared to 25% in the original study. 12% were failures regarding need to undergo surgery when bisphosphonates were given, as compared to 32% in the previous untreated series. An anticatabolic drug delaying the remodeling might be an effective treatment in osteonecrosis of the knee but further (preferably randomized) studies are necessary.
The prognosis for spontaneous osteonecrosis in the medial or lateral femoral condyle is poor. It is associated with a high frequency of osteoarthritis and often leads to subsequent knee surgery (Lotke et al. 1982). 20 years ago, 40 patients with scintigraphic and/or radiographic signs of osteonecrosis in either one of the femoral condyles were followed for 1–7 years at our hospital (Al-Rowaih et al. 1991). 29 patients developed osteoarthritis, 8 of whom were operated with a knee arthroplasty, 4 with a proximal tibial osteotomy, and 1 with arthrotomy and drilling. The size of the lesion was found to be prognostic of the outcome (Al-Rowaih et al. 1993).
Bisphosphonates are a group of drugs that are in clinical use for treatment of osteoporosis and bone malignancies. Circulating bisphosphonates bind to bone mineral and, as the bone is resorbed by osteoclasts, bisphosphonates are internalized and interfere with cell metabolism—leading to apoptosis of the osteoclast (Rogers 2003). Systemic treatment with bisphosphonates can postpone the resorption of a bone graft (Åstrand and Aspenberg 2002, Tägil et al. 2004). In osteonecrosis, bisphosphonates have been shown to delay the resorption of revascularizing dead bone, both experimentally (Little et al. 2003, Kim et al. 2005) and in clinical series (Nishii et al. 2006, Ramachandran et al. 2007). In a randomized human study, bisphosphonates were found to substantially reduce the risk of secondary osteoarthritis in patients with femoral head osteonecrosis (Lai et al. 2005), with only 2 of 29 collapsing in the treated group compared to 19 of 25 in the placebo group. We wanted to determine whether it is also possible to prevent joint surface collapse in spontaneous osteonecrosis of the knee by using a bisphosphonate.
Patients and methods
Patients
At our department, 17 consecutive patients (mean age 68 (48–82) years), 9 of who were women, were diagnosed between 2006 and 2009 as having primary osteonecrosis of the knee. In 14 patients, the lesion was located in the medial femoral condyle and in 3 patients it was located in the lateral condyle. The duration of symptoms was 5 (1–15) months. The inclusion criteria were typical osteonecrotic changes on MRI scan and sudden onset of pain without significant preceding trauma. No time limit from debut of symptoms or diagnosis and start of treatment was used. The exclusion criteria were known bisphosphonate allergy, kidney or dental problems, known secondary etiology of osteonecrosis, and manifest osteoartrithis of Ahlbäck grade > 1 at onset of symptoms.
Drug treatment
Alendronate (Fosamax(R), 70 mg, was prescribed once a week perorally for a minimum of 6 months (Lai et al. 2005) or until the lesion (centrally) started to regain bone density by MRI or radiography, i.e. until calcification of the central healing tissue had started (Figures 1 and 2).
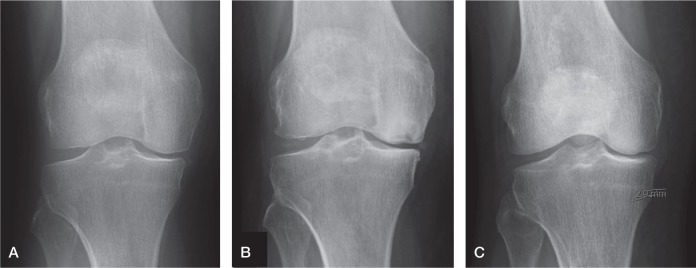
Figure 1.
A. A 59-year-old man had sudden onset of knee pain and was diagnosed with osteonecrosis by MRI. B. There were no or discrete signs of osteonecrosis in the plain radiographs. Alendronate was given for 6 months and the pain disappeared. C. Radiograph after 1 year. Radiographically, no signs of osteonecrosis ever appeared.
Figure 2.
A. An 82-year-old women suddenly noticed pain in her right knee. A mild osteoarthritis was seen and regarded as the cause of the symptoms. No treatment was given. (This radiograph was taken 1 month after start of symptoms). B. One year after start of symptoms, the symptoms were the same and a visible osteonecrosis was now seen with a Lotke index of 33%. The patient was referred to our department. C. The patient was treated for 13 months. Radiograph taken at follow-up 2 years after the start of treatment. The ostenecrosis had healed completely but the patient had developed mild osteoarthritis of Ahlbäck grade 1.
Outcome
The patients were followed with clinical examination, radiographs, and MRI initially and after one year. In 2010, all the patients were reviewed again using the same protocol, to determine whether a late collapse had occurred. To determine the size of the osteonecrosis, the Lotke index was used (Lotke et al. 1982). The ratio, expressed as percent of the joint surface affected by the osteonecrosis, was measured and related to the total joint surface of the affected medial or lateral condyle. Although the Lotke index was originally described in radiographs, the size of the lesion was measured both by radiography and MRI. Based on the radiographic outcome, the patients were divided into 3 groups: (A) those who did not develop osteoarthritis, (B) those who developed mild osteoarthritis but no collapse, and (C) those who developed a joint surface collapse.
Results
Based on the radiographic outcome (Table), 10 of the 17 patients did not develop osteoarthritis (group A) (Figure 1), 4 patients developed mild osteoarthritis but never had collapse (group B) (Figure 2), and 3 had a knee joint surface collapse (group C) (Figure 3). 2 of the patients with joint surface collapse underwent knee arthroplasty and 1 did not. The first patient stopped medication after the first drug dose due to gastrointestinal side effects and had core decompression at another hospital after another 2 weeks. The size of the osteonecrosis successively increased to a Lotke index of 50, and the joint surface collapsed in the 2 months that followed. He was subsequently operated with a knee arthroplasty. The second patient stopped treatment after 3 months due to side effects, and a large part of the joint line collapsed in the 6 months that followed (Figure 3). This patient was operated with a knee arthroplasty 2.5 years after symptoms started. The third patient rapidly developed a joint line collapse and osteoarthritis (Ahlbäck grade 3) during bisphosphonate treatment (at 6 months), but has not been operated due to mild symptoms.
Radiographic outcome and the size of the lesion (Lotke index)
| Group A | Group B | Group C | |
|---|---|---|---|
| Present study (bisphosphonate treatment) | |||
| No. of patients | 10 | 4 | 3 |
| Lotke at debut (radiography) | 17 | 14 | 6 |
| Lotke at debut (MRI) | 35 | 23 | 26 |
| Max. Lotke (radiography) | 25 | 30 | 35 |
| Natural course (no treatment) a | |||
| No. of patients | 10 | 8 | 22 |
| Max. Lotke (radiography) | 22 | 28 | 39 |
Group A: good—no OA and no joint collapse;
Group B: intermediate—OA but no joint collapse;
Group C: poor—OA and/or joint collapse.
a In the study by al Rowaih et al. (1991)
Figure 3.
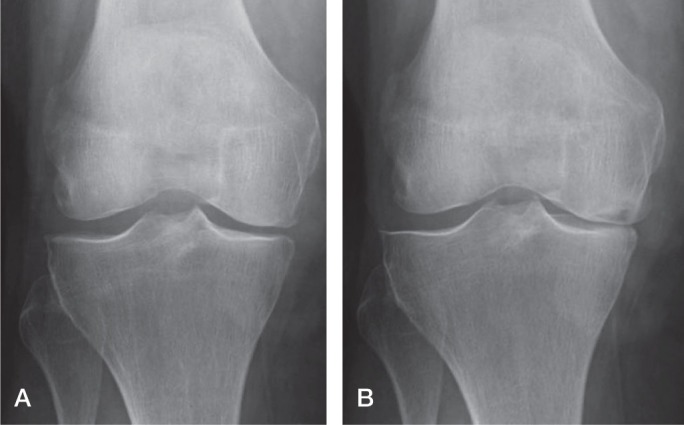
A. A 83-year-old woman at symptom start. Bisphosphonate treatment was initiated within 3 months after symptom debut. B. The patient used the drug for three months but had unwanted side effects and stopped the medication. The pain persisted and osteoarthritis gradually developed (Ahlbäck 4) and 2 years later, the patient had a joint replacement.
The 15 unoperated patients were treated with bisphosphonates for mean 11 (6–21) months until the defect in the center of the lesion was considered to increase in density and medication was stopped. In 1 patient, a subchondral fracture was seen in the osteonecrotic lesion before treatment started. In this patient, the joint surface did not collapse and the lesion eventually healed with Ahlbäck grade 1 osteoarthritis and minor symptoms (Figure 2).
In the 10 patients who never developed osteoarthritis, the mean Lotke index in plain radiographs at the first visit was 17% (0–60) and in MRI it was 35% (16–58). The lesions gradually increased during treatment and Lotke index peaked in the plain radiographs at a mean of 25% (0–58) before gradually decreasing. The 4 patients who developed osteoarthritis (Ahlbäck grade 1–2) but no collapse had a mean Lotke index in plain radiographs of 14% (0–33) and 23% (19–27) by MRI; it reached a maximum radiographic Lotke index of 30% (21–33). The 3 knees that collapsed had a mean Lotke index at the first visit of 10% (0–18) on plain radiographs and 26% (21–30) by MRI. The maximum Lotke index peaked at 35% (23–50).
In 7 patients, the necrosis was first diagnosed by MRI without there being any radiographic changes. 5 of these patients gradually developed radiographic signs of osteonecrosis during treatment, whereas 2 patients never did. All these patients healed without collapse, and with only mild or no development of osteoarthritis. The mean time from start of symptoms to diagnosis and start of treatment was 4 (1–8) months in the patients who were diagnosed by MRI only and 7 (1–15) in patients who had radiographic lesions at diagnosis. The mean time from start of symptoms to diagnosis was 5 (1–15) months in the whole group and 2 (1–3) months in the patients who were subsequently operated.
Discussion
By definition, osteonecrosis means in situ death of bone cells, osteocytes, and hematopoietic and fatty marrow precursor cells, and it is most often thought to be due to bone marrow pressure (Kantor et al.1987) or an occult subchondral fracture (Yamamoto and Bullough 2000). Although the cells in the necrotic lesion die, the inorganic bone matrix is primarily unaffected and the bone will initially retain its load-bearing capacity (Parks and Engh 1997). Regardless of cause, ingrowing blood vessels invade the necrotic bone from the surrounding living bone, and osteoclasts are brought into the lesion to resorb the necrotic bone matrix. A remodeling process starts, with simultaneous coupling of bone resorption and formation. The mechanical strength of the remodeling bone might be temporarily reduced, either due to the resorption of necrotic bone or to a fatigue stress fracture in necrotic bone that has not yet become revitalized. If the necrosis occurs in subchondral load-bearing bone, partial joint collapse and secondary osteoarthritis might be the final result (Tägil et al. 2004, Lai et al. 2005).
In the previous study of 40 patients at our hospital (Al-Rowaih et al. 1991) with a similar but untreated series of knee osteonecrosis, patients with higher Lotke indices had worse outcome with a high frequency of joint surface collapse and subsequent surgery than those in the present, treated series. Only 10 of 40 patients had a good outcome in the original study with complete radiographical recovery, as compared to 10 of 17 in the present series (p = 0.03, Fisher’s exact test). 8 of 40 patients were considered intermediate due to development of osteoarthritis, but with minor symptoms compared to the present study where 4 of 17 of the bisphosphonate-treated patients developed mild osteoarthritis.
The incidence of secondary surgery appears to be less when bisphosphonates are given. In the original series, 22 of 40 patients were considered failures due to osteoarthritis and major symptoms. Of these patients, 13 underwent surgery with osteotomy, decompression, or prosthesis. In the present series, 2 of the 17 patents were failures because they needed surgery (p = 0.2, Fisher’s exact test). It is notable that none of these patients were able to complete the planned minimum 6 months of bisphosphonate treatment and they were the only patients not to do so. Although not operated, another patient in the bisphosphonate-treated group was considered a failure, as he developed severe osteoarthritis (Ahlbäck grade 3) and collapse of the joint surface. In the original series, the size of the lesion was found to be associated with an inferior outcome but in the present series no such association was found. In our series, lesions larger than the cutoff at Lotke index 30% healed without osteoarthritis, but lesions smaller in size also collapsed. In addition, time from the start of symptoms to start of treatment appeared to be unrelated to outcome.
In the only randomized trial using bisphosphonates in osteonecrosis (of the hip) (Lai et al. 2005), a fixed treatment time of 6 months was set. In our study, treatment was continued until the central region started to increase in radiographic density, indicating osteoblast activity in the center and a hypothetically regained mechanical strength. It is not known how long treatment should last.
In conclusion, the outcome for our patients in the present series appears to have been better than in the previous, untreated series (al Rowai 1991), and calls for a prospective randomized study to determine whether bisphosphonates are capable of changing the outcome. Perhaps a prolonged period of partial weight bearing would be as effective, or maybe both are needed. In the future, other drugs might also be used—such as RANK-ligand antibodies—which besides being more short-acting, have been shown to be more effective than bisphosphonates in experimentally induced osteonecrosis (Kim et al. 2006).
Acknowledgments
JJ: planning, collection and interpretation of data, statistics, and writing of the article. AL: project setup, collection and interpretation of data, and revision of the manuscript. MG: evaluation of imaging studies, interpretation of data, and revision of the manuscript. DR: collection and interpretation of data and revision of the manuscript. MT: project setup, planning, collection and interpretation of data, statistics, and writing of the article.
The project was supported by the Swedish Research Council (project 2031), the Greta and Johan Kock Foundation, the Alfred Österlund Foundation, the Maggie Stephens Foundation, the Thure Carlsson Foundation, and the Medical Faculty of Lund. The study was performed without support from the manufacturers of the drug.
No competing interests declared.
References
- Al-Rowaih A, Lindstrand A, Björkengren A, Wingstrand H, Thorngren KG. Osteonecrosis of the knee. Diagnosis and outcome in 40 patients. Acta Orthop Scand. 1991;62(1):19–23. doi: 10.3109/17453679108993085. [DOI] [PubMed] [Google Scholar]
- Al-Rowaih A, Björkengren A, Egund N, Lindstrand A, Wingstrand H, Thorngren KG. Size of osteonecrosis of the knee. Clin Orthop. 1993;(287):68–75. [PubMed] [Google Scholar]
- Kantor H. Bone marrow pressure in osteonecrosis of the femoral condyle (Ahlbäck’s disease) Arch Orthop Trauma Surg. 1987;106(6):349–52. doi: 10.1007/BF00456868. [DOI] [PubMed] [Google Scholar]
- Kim HK, Randall TS, Bian H, Jenkins J, Garces A, Bauss F. Ibandronate for prevention of femoral head deformity after ischemic necrosis of the capital femoral epiphysis in immature pigs. J Bone Joint Surg (Am) 2005;87(3):550–7. doi: 10.2106/JBJS.D.02192. [DOI] [PubMed] [Google Scholar]
- Kim HK, Morgan-Bagley S, Kostenuik P. RANKL inhibition: a novel strategy to decrease femoral head deformity after ischemic osteonecrosis. J Bone Miner Res. 2006;21(12):1946–54. doi: 10.1359/jbmr.060905. [DOI] [PubMed] [Google Scholar]
- Lai KA, Shen WJ, Yang CY, Shao CJ, Hsu JT, Lin RM. The use of alendronate to prevent early collapse of the femoral head in patients with nontraumatic osteonecrosis. A randomized clinical study. J Bone Joint Surg (Am) 2005:2155–9. doi: 10.2106/JBJS.D.02959. [DOI] [PubMed] [Google Scholar]
- Little DG, Peat RA, Mcevoy A, Williams PR, Smith EJ, Baldock PA. Zoledronic acid treatment results in retention of femoral head structure after traumatic osteonecrosis in young Wistar rats. J Bone Miner Res. 2003;18(11):2016–22. doi: 10.1359/jbmr.2003.18.11.2016. [DOI] [PubMed] [Google Scholar]
- Lotke PA, Abend JA, Ecker ML. The treatment of osteonecrosis of the medial femoral condyle. Clin Orthop. 1982;(171):109–16. [PubMed] [Google Scholar]
- Nishii T, Sugano N, Miki H, Hashimoto J, Yoshikawa H. Does alendronate prevent collapse in osteonecrosis of the femoral head? Clin Orthop. 2006;443:273–9. doi: 10.1097/01.blo.0000194078.32776.31. [DOI] [PubMed] [Google Scholar]
- Parks NL, Engh GA. Histology of nine structural bone grafts used in total knee artroplasty. Clin Orthop. 1997;(345):17–23. [PubMed] [Google Scholar]
- Ramachandran M, Ward K, Brown RR, Munns CF, Cowell CT, Little DG. Intravenous bisphosphonate therapy for traumatic osteonecrosis of the femoral head in adolescents. J Bone Joint Surg (Am) 2007;89(8):1727–34. doi: 10.2106/JBJS.F.00964. [DOI] [PubMed] [Google Scholar]
- Rogers MJ. New insights into the molecular mechanisms of action of bisphosphonates. Curr Pharm Des. 2003;9(32):2643–58. doi: 10.2174/1381612033453640. Review. [DOI] [PubMed] [Google Scholar]
- Tägil M, Astrand J, Westman L, Aspenberg P. Alendronate prevents collapse in mechanically loaded osteochondral grafts: a bone chamber study in rats. Acta Orthop Scand. 2004;75(6):756–61. doi: 10.1080/00016470410004157. [DOI] [PubMed] [Google Scholar]
- Yamamoto T, Bullough PG. Spontaneous osteonecrosis of the knee: the result of subchondral insufficiency fracture. J Bone Joint Surg (Am) 2000;82(6):858–66. doi: 10.2106/00004623-200006000-00013. [DOI] [PubMed] [Google Scholar]
- Åstrand J, Aspenberg P. Systemic alendronate prevents resorption of necrotic bone during revascularization. A bone chamber study in rats. BMC Musculoskelet Disord. 2002;3:19. doi: 10.1186/1471-2474-3-19. [DOI] [PMC free article] [PubMed] [Google Scholar]