Abstract
Objective
The purpose of this study was to determine the efficacy of bone cement-augmented short segment fixation using percutaneous screws for thoracolumbar burst fractures in a background of severe osteoporosis.
Methods
Sixteen patients with a single-level thoracolumbar burst fracture (T11-L2) accompanying severe osteoporosis treated from January 2008 to November 2009 were prospectively analyzed. Surgical procedures included postural reduction for 3 days and bone cement augmented percutaneous screw fixation at the fracture level and at adjacent levels without bone fusion. Due to the possibility of implant failure, patients underwent implant removal 12 months after screw fixation. Imaging and clinical findings, including involved vertebral levels, local kyphosis, canal encroachment, and complications were analyzed.
Results
Prior to surgery, mean pain score (visual analogue scale) was 8.2 and this decreased to a mean of 2.2 at 12 months after screw fixation. None of the patients complained of pain worsening during the 6 months following implant removal. The percentage of canal compromise at the fractured level improved from a mean of 41.0% to 18.4% at 12 months after surgery. Mean kyphotic angle was improved significantly from 19.8° before surgery to 7.8 at 12 months after screw fixation. Canal compromise and kyphotic angle improvements were maintained at 6 months after implant removal. No significant neurological deterioration or complications occurred after screw removal in any patient.
Conclusion
Bone cement augmented short segment fixation using a percutaneous system can be an alternative to the traditional open technique for the management of selected thoracolumbar burst fractures accompanied by severe osteoporosis.
Keywords: Burst fracture, Fusion, Percutaneous
INTRODUCTION
Thoracolumbar burst fractures are common spinal injuries caused by vertical loading, and affect at least two columns of the spine predominantly in younger patients, whereas thoracolumbar burst fractures accompanied by osteoporosis increase with age5). The goals of surgical treatment for thoracolumbar burst fractures are to restore stability of the vertebral column and to decompress the spinal canal, which when achieved, lead to early mobilization. Despite general agreement regarding the goals of surgical treatment, the management of thoracolumbar burst fractures accompanying osteoporosis without neurological deficit remains controversial. The traditional procedures for treating thoracolumbar burst fractures in patients with osteoporosis entail bone fusion with supplemental long-level instrumentation. However, these surgeries have distinct disadvantages. Extensive dissection of paraspinous muscles may be associated with massive blood loss and lead to persisting sequelae, such as, muscular denervation, atrophy, and pain. On the other hand, recent reports on burst fractures have demonstrated the efficacy of bone cement augmented short segment fixation in terms of preventing implant failure1,3). Furthermore, percutaneous screw fixation has been proposed and applied to minimize the negative consequences of traditional open surgery, which include muscular denervation and atrophy6,8). However, no prospective study has been conducted on the clinical outcomes of short segment fixation by percutaneous screw insertion without bone fusion for burst fractures in a background of osteoporosis. Accordingly, we designed this prospective study to evaluate the clinical outcomes of short segment fixation without bone fusion of thoracolumbar burst fractures in osteoporotic patients. We also examined whether implant removal aggravates kyphotic deformities and adversely affects clinical outcomes. The hypothesis of this study was that screw removal would not affect spinal stability.
MATERIALS AND METHODS
This study included 16 patients (5 males, 11 females) with a thoracolumbar burst fracture. The inclusion criteria were limited to : 1) neurologically intact patients with a single level thoracolumbar burst fracture (canal compromise of >30%); 2) kyphotic angle of >20° and anterior vertebral height loss of >40%; 3) intact bilateral pedicles, enabling screw insertion at the fractured vertebra; and 4) an osteoporotic spine (T-score by bone mineral densitometry of <-3.0). Patients with conditions requiring anterior decompression for neurologic deficits, or conditions preventing screw insertion at the fracture level were excluded. However, patients with a posterior column fracture were not excluded (Table 1). All patients underwent implant removal at 12 months after screw fixation due to possibility of implant failure (the need for this procedure was fully explained before surgery). After postural reduction for 3 days using a soft roll under the collapsed vertebra in the supine position, bone cement augmented, percutaneous screw fixation confined to adjacent levels (one above and one below the injured vertebra and including the fractured vertebra) was performed. Bone cement augmentation was achieved using polymethylmethacrylate (PMMA), which was injected under C-arm guidance through a vertebroplasty needle and allowed to localize in the vertebral body area. Approximately 2 cc of PMMA was injected through the vertebroplasty needle - a total of 4 cc per vertebra. A transpedicular screw system with a detachable screw extender, Apollon® Solco Medical Korea (Fig. 1) was used to insert screws. Intraoperatively, following the induction of general or spinal anesthesia, patients were placed in the prone position with cushions under the iliac crests and thorax to maintain a hyperextended spine.
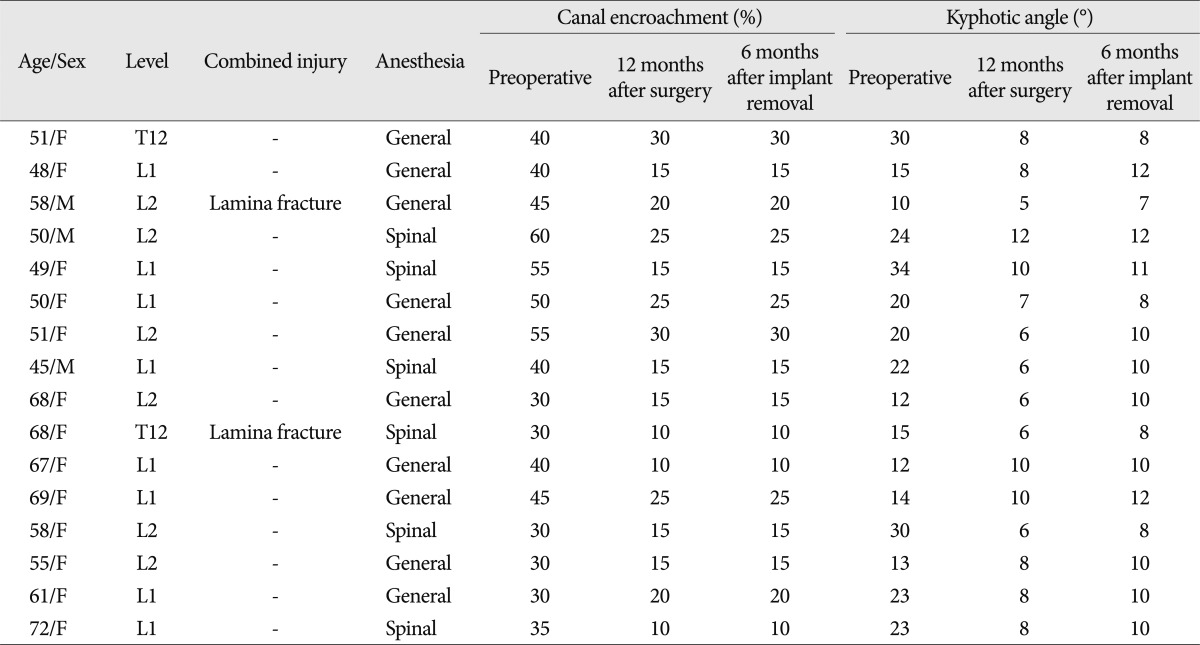
Table 1.
Clinical and radiological data of the patients included in this series
Fig. 1.
Changes in kyphotic angles.
Lateral plain radiography, computed tomography (CT), and magnetic resonance imaging were performed at three time points, that is, 1) preoperatively, 2) at 12 months after surgery, just before implant removal, 3) at six months after implant removal. The axial CT images showing greatest canal encroachment by retropulsed bone fragments were selected to measure canal compromise. Kyphotic angle was measured by making a straight line from the superior endplate of the vertebra one level above the fractured body and a straight line from the inferior endplate of the vertebra one level below the fractured body. Imaging and clinical findings, including involved vertebral level, vertebral height restoration, local kyphosis, clinical outcomes, and complications were analyzed.
Safety and outcome evaluation
Visual analogue scale pain scores were evaluated at the above-mentioned time points. At six months after implant removal, the patients were evaluated according to a modified version of MacNab's criteria for characterizing clinical outcomes after spinal surgery.
Statistics
Statistical analysis was performed using SAS software version 6.12 (SAS Institute, Inc., Cary, NC, USA). Comparisons at different time points were conducted using the paired Student's t-test. Results are presented as mean values and standard deviations, and differences were considered statistically significant for p values of <0.05.
RESULTS
With respect to the anatomic distribution of fractures, T12 (n=2), L1 (n=8), and L2 (n=6) were involved in the present study. Mean operation time was 66.5±30.5 minutes and mean blood loss was 63.1±45.0 mL.
Overall reduction of kyphotic deformity
Intraoperative correction of kyphotic deformities by longitudinal distraction was possible. Mean kyphotic angle improved significantly from 19.8±8.2° (range : 10-34°) before surgery to 7.8° (range : 6-12°) at 12 months after surgery.
At six months after implant removal, the average amount of correction loss of kyphotic deformities was 2.0°, which represented a 10° change in angulation from the original position (p<0.01) (Fig. 1).
Proportion of canal compromise
Mean preoperative canal compromise, due to retropulsed bone fragments, was 41.0%. CT at 1 year after surgery and just before implant removal, revealed an improvement in canal compromise to 18.4%. Furthermore, this improvement was maintained on CT scans at 6 months after implant removal (Fig. 2), and was statistically significant (p<0.001). No patient experienced neurological deterioration due to a retropulsed bony fragment after implant removal.
Fig. 2.
Fraction of canal compromise.
Clinical outcomes
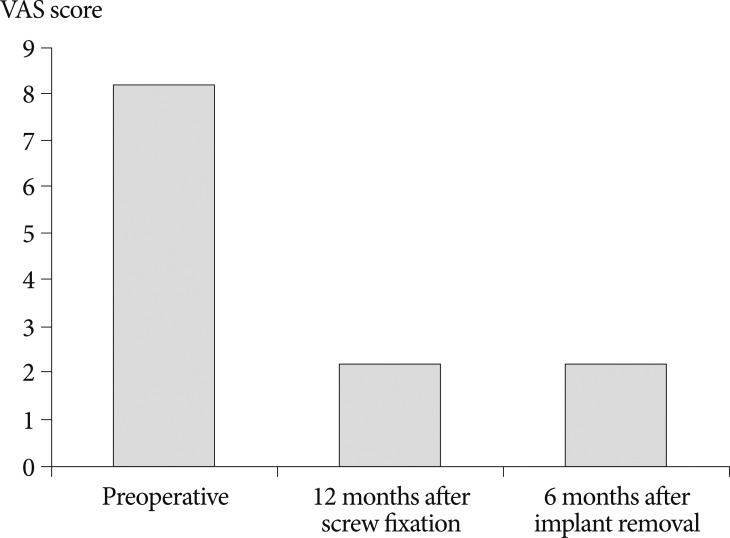
No patient needed a drainage catheter and all 16 patients were able to ambulate at 24 hours after surgery wearing a thoraco-lumbo-sacral-orthosis. At 6 months after implant removal, all patients achieved an excellent or good outcome (excellent in 14 patients and good in 2). Prior to surgery, mean pain score was 8.2 and this decreased to 2.2 at 12 months after surgery and maintained at 6 months after implant removal (Fig. 3). No significant complications or neurological deterioration occurred after screw removal in any patient (Fig. 4, 5).
Fig. 3.
Pain score improvement. VAS : visual analogue scale.
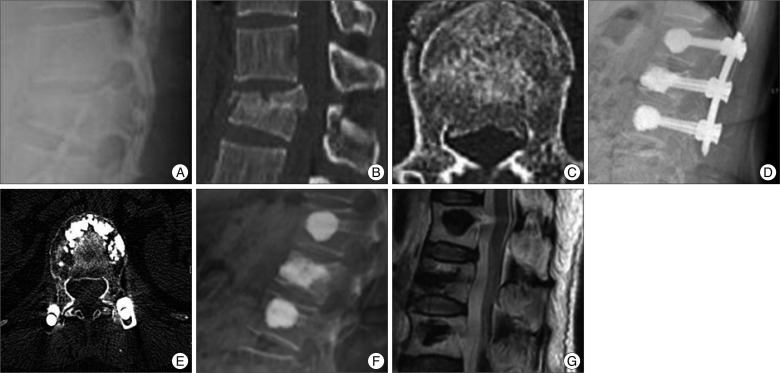
Fig. 4.
The case of a neurologically intact 58-year-old woman with an L2 bursting fracture. A, B and C : Preoperative simple radiograph and computed tomography scans show about 45% height loss and 45% canal compromise. Posterior element fracture is also seen. D and E : Simple radiograph and a computed tomography scan taken at 12 months after screw fixation show restored vertebral height and improved kyphotic deformity. F and G : Simple radiograph and a magnetic resonance image taken at 6 months after implant removal reveal a well maintained kyphotic angle and much reduced canal compromise.
Fig. 5.
The case of neurologically intact 45-year-old man with an L1 bursting fracture. A, B and C : Preoperative simple radiograph, computed tomography scan and magnetic resonance image show about 50% height loss and 40% canal compromise. D and E : Simple radiograph and a computed tomography scan taken at 12 months after screw fixation show a restored vertebral height and improved kyphotic deformity. F and G : Simple radiograph and a magnetic resonance image taken at 6 months after implant removal reveal a well maintained kyphotic angle and much reduced canal compromise.
DISCUSSION
The goals of the surgical treatment of thoracolumbar burst fractures are; to restore vertebral column stability, to decompress the spinal canal, and to facilitate early ambulation. Stabilization by open surgery continues to be widely used to treat thoracolumbar burst fractures, but traditional open surgery is highly invasive and requires a long skin incision. Furthermore, when performed anteriorly, it requires significant invasion of the retroperitoneal space or thoracic cavity and a wide dissection margin2,9). Therefore, when there is no need to decompress neural elements, multi-segment fixation using a posterior approach is usually performed. However, this also requires extensive dissection of the paraspinal muscles of the back and resection of the posterior elements of the spine, which makes it difficult to preserve motion segments15). Due to several problems associated with extensive long level fusion, posterior short-segment fusion is now preferred for the treatment of thoracolumbar burst fractures13). The main advantage of short-segment fixation is that it preserves motion segments more so than long-level fixation. However, failure to restore anterior column support can lead to secondary kyphosis, which primarily depends on the residual load transfer capacity of the fractured vertebral body. To date, the results of short-segment fixation have not been good, and implant failure rates of 10 to 30% have been reported7,10,16). Moreover, in severe osteoporotic patients, the anchoring effect that holds screws in place is diminished, and the probability of hardware failure is high, and thus, the risk of non-union is increased17). In 2006, Wang et al.18) reported satisfactory results for short-segment fixation without fusion in surgically-treated burst fractures of the thoracolumbar spine, and found that for surgically treated burst fractures, clinical results were similar for those treated with or without bone fusion. The advantages of instrumentation without fusion are the elimination of donor site complications, the preservation of motion segments, reduced blood loss, and a shorter operation time. More recently, some investigators have reported successful surgical outcomes for percutaneous non-fusion short-segment fixation6,8). The preservation of the segmental stability obtained by posterior screw fixation is not easily achieved before the fusion of fractured vertebra, and screw loosening or vertebral collapse may occur more frequently after percutaneous screwing procedures. In addition, these problems may be more significant in patients with severe osteoporosis. To overcome these limitations, we attempted bone cement augmentation at adjacent vertebrae. In addition, the insertion of bone cement-augmented pedicle screws at fracture levels resulting in segmental constructs with improved biomechanical stability due to the protection afforded fractured vertebral bodies and indirect support of the anterior column11,12). Furthermore, the insertion of bone cement-augmented pedicle screws can significantly reduce pedicle screw bending and increase initial stiffness in the flexion-extension plane. In a previous study, it was found that PMMA can increase pull-out strength from 96 to 262% and transverse bending stiffness by up to 153%19). In addition, spontaneous remodeling of the spinal canal was shown to occur after a burst fracture, regardless of the treatment modality used. Scapinelli and Candiotto14) concluded that rhythmic respiratory oscillations in cerebrospinal fluid pressure and loss of mechanical loading are important components of bone remodeling. de Klerk et al.4) reported that the process of remodeling mainly takes place during the first year after injury, and that subsequently, little remodeling takes place, which is why, we removed implants at 1 year after screw fixation. Furthermore, after bone cement-augmented short segment fixation without bone fusion, early ambulation was possible and motion segments were preserved by screw removal, which contrasts to that observed after long level instrumentation and fusion. The advantages of short segment fixation without bone fusion also include immediate pain relief due to the elimination of donor site pain, reduced blood loss, and a short operative time. The present study demonstrates the efficacy of short segment fixation without fusion in patients with a thoracolumbar burst fracture but without neurologic deficit, but this method is by no means indicated in all patients with a thoracolumbar burst fracture, and in particular, may be contraindicated in patients with a highly unstable fracture and severe neurologic injury. In the present study, we addressed the question as to whether simultaneous fusion is necessary when treating a thoracolumbar burst fracture by percutaneous short-segment fixation rather than addressing controversial issues related to the indications for operative or nonoperative treatment. Furthermore, we acknowledge that some of the patients in the present series might also have been appropriate candidates for balloon kyphoplasty. In fact, we know that nonoperative treatment is also safe and effective for selected patients with an osteoporotic thoracolumbar burst fracture, as demonstrated by improvements in pain and work status. Randomized, comparative, clinical trials in larger populations are required in the near future.
CONCLUSION
Bone cement augmented, percutaneous short segment fixation following postural reduction without fusion might be an alternative to traditional long level fusion for the management of patients with a thoracolumbar burst fracture accompanied by severe osteoporosis but without neurologic deficit. In the present study, this technique was found to reduce the number of screw fixation levels, preserve motion segments, and correct kyphotic deformities. Furthermore, improved canal compromise and kyphotic deformity were maintained during follow-up after screw removal.
References
- 1.Acosta FL, Jr, Aryan HE, Taylor WR, Ames CP. Kyphoplasty-augmented short-segment pedicle screw fixation of traumatic lumbar burst fractures : initial clinical experience and literature review. Neurosurg Focus. 2005;18:e9. doi: 10.3171/foc.2005.18.3.10. [DOI] [PubMed] [Google Scholar]
- 2.Arrington ED, Smith WJ, Chambers HG, Bucknell AL, Davino NA. Complications of iliac crest bone graft harvesting. Clin Orthop Relat Res. 1996:300–309. doi: 10.1097/00003086-199608000-00037. [DOI] [PubMed] [Google Scholar]
- 3.Cho DY, Lee WY, Sheu PC. Treatment of thoracolumbar burst fractures with polymethyl methacrylate vertebroplasty and short-segment pedicle screw fixation. Neurosurgery. 2003;53:1354–1360. doi: 10.1227/01.neu.0000093200.74828.2f. discussion 1360-1361. [DOI] [PubMed] [Google Scholar]
- 4.de Klerk LW, Fontijne WP, Stijnen T, Braakman R, Tanghe HL, van Linge B. Spontaneous remodeling of the spinal canal after conservative management of thoracolumbar burst fractures. Spine (Phila Pa 1976) 1998;23:1057–1060. doi: 10.1097/00007632-199805010-00018. [DOI] [PubMed] [Google Scholar]
- 5.Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 1983;8:817–831. doi: 10.1097/00007632-198311000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Gahr RH, Strasser S, Strasser E, Schmidt OI. Percutaneous internal fixation of thoracolumbar spine fractures. Top Spinal Cord Inj Rehabil. 2006;12:45–54. [Google Scholar]
- 7.Hakalo J, Wroński J. [Complications of a transpedicular stabilization of thoraco-lumbar burst fractures] Neurol Neurochir Pol. 2006;40:134–139. [PubMed] [Google Scholar]
- 8.Huang QS, Chi YL, Wang XY, Mao FM, Lin Y, Ni WF, et al. [Comparative percutaneous with open pedicle screw fixation in the treatment of thoracolumbar burst fractures without neurological deficit] Zhonghua Wai Ke Za Zhi. 2008;46:112–114. [PubMed] [Google Scholar]
- 9.Kaneda K, Taneichi H, Abumi K, Hashimoto T, Satoh S, Fujiya M. Anterior decompression and stabilization with the Kaneda device for thoracolumbar burst fractures associated with neurological deficits. J Bone Joint Surg Am. 1997;79:69–83. doi: 10.2106/00004623-199701000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Lee YS, Sung JK. Long-term follow-up results of short-segment posterior screw fixation for thoracolumbar burst fractures. J Korean Neurosurg Soc. 2005;37:416–421. [Google Scholar]
- 11.Lü FX, Huang Y, Zhang Q, Shi FL, Zhao DS, Hu Q. Pedicle screw fixation against burst fracture of thoracolumbar vertebrae. Chin J Traumatol. 2007;10:349–352. [PubMed] [Google Scholar]
- 12.Mahar A, Kim C, Wedemeyer M, Mitsunaga L, Odell T, Johnson B, et al. Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine (Phila Pa 1976) 2007;32:1503–1507. doi: 10.1097/BRS.0b013e318067dd24. [DOI] [PubMed] [Google Scholar]
- 13.Parker JW, Lane JR, Karaikovic EE, Gaines RW. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures : a consecutive 41/2-year series. Spine (Phila Pa 1976) 2000;25:1157–1170. doi: 10.1097/00007632-200005010-00018. [DOI] [PubMed] [Google Scholar]
- 14.Scapinelli R, Candiotto S. Spontaneous remodeling of the spinal canal after burst fractures of the low thoracic and lumbar region. J Spinal Disord. 1995;8:486–493. [PubMed] [Google Scholar]
- 15.Sihvonen T, Herno A, Paljärvi L, Airaksinen O, Partanen J, Tapaninaho A. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine (Phila Pa 1976) 1993;18:575–581. doi: 10.1097/00007632-199304000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Son BG, Bae KJ, Jung ES, Choi ES, Shin JH, Kim MJ, et al. Results of posterior short segment fixation cases which are more than 65% canal compromise of thoracolumbar burst fractures (Minimum 3 years follow-up) Korean J Spine. 2007;4:199–204. [Google Scholar]
- 17.Soshi S, Shiba R, Kondo H, Murota K. An experimental study on transpedicular screw fixation in relation to osteoporosis of the lumbar spine. Spine (Phila Pa 1976) 1991;16:1335–1341. doi: 10.1097/00007632-199111000-00015. [DOI] [PubMed] [Google Scholar]
- 18.Wang ST, Ma HL, Liu CL, Yu WK, Chang MC, Chen TH. Is fusion necessary for surgically treated burst fractures of the thoracolumbar and lumbar spine?: a prospective, randomized study. Spine (Phila Pa 1976) 2006;31:2646–2652. doi: 10.1097/01.brs.0000244555.28310.40. discussion 2653. [DOI] [PubMed] [Google Scholar]
- 19.Wittenberg RH, Lee KS, Shea M, White AA, 3rd, Hayes WC. Effect of screw diameter, insertion technique, and bone cement augmentation of pedicular screw fixation strength. Clin Orthop Relat Res. 1993:278–287. [PubMed] [Google Scholar]