Abstract
Objective
To investigate death rates in schizophrenia and related psychoses.
Design
Data from two epidemiologically complete cohorts of patients presenting for the first time to mental health services in North Wales for whom there are at least 1, and up to 10-year follow-up data have been used to calculate survival rates and standardised death rates for schizophrenia and related psychoses.
Setting
The North Wales Asylum Denbigh (archived patient case notes) and the North West Wales District General Hospital psychiatric unit.
Population
Cohort 1: The North Wales Asylum Denbigh (archived patient case notes). Of 3168 patients admitted to the North Wales Asylum Denbigh 1875–1924, 1074 had a schizophrenic or related psychosis. Cohort 2: Patients admitted between 1994 and 2010 to the North West Wales District General Hospital psychiatric unit, of whom 355 had first admissions for schizophrenia or related psychoses.
Results
We found a 10-year survival probability of 75% in the historical cohort and a 90% survival probability in the contemporary cohort with a fourfold increase in standardised death rates in schizophrenia and related psychoses in both historical and contemporary periods. Suicide is the commonest cause of death in schizophrenia in the contemporary period (SMR 35), while tuberculosis was the commonest cause historically (SMR 9). In the contemporary data, deaths from cardiovascular causes arise in the elderly and deaths from suicide in the young.
Conclusions
Contemporary death rates in schizophrenia and related psychoses are high but there are particular hazards and windows of risk that enable interventions. The data point to possible interventions in the incident year of treatment that could give patients with schizophrenia a normal life expectancy.
Article summary.
Article focus
-
▪
The question of possible increases in mortality in psychosis is a current issue of concern, with both suicide and increased cardiovascular risk noted. It is known that the initial year after a diagnosis of schizophrenia is a point of high risk.
Key messages
-
▪
In North Wales, access to two epidemiologically complete case registers makes it possible to demonstrate that suicide is not inherent in schizophrenia and that cardiovascular deaths are confined to elderly patients, who typically do not have a schizophrenia diagnosis.
-
▪
Tackling the problem of suicides in the first year of schizophrenia has the potential to restore life expectancy to normal in this illness.
Strengths and limitations of this study
-
▪
This study has unique access to a large and complete cohort of unmedicated psychotic patients, which makes it possible to separate the contributions of the illness and its treatments to mortality.
-
▪
The study also offers a first rigorous estimate of historical mortality in serious mental illness. The cohort design of the study highlights factors that cross-sectional studies miss.
-
▪
The size of the contemporary cohort, duration of follow-up and number of deaths preclude definitive statements about mortality.
Introduction
There is growing interest in outcomes for schizophrenia and related psychoses, fuelled by consistent reports of an apparent doubling or tripling of death rates, along with significant reductions in life expectancy.1–11 A double or tripling of death rates, equates in the case of schizophrenia to a loss of approximately 15 years of life expectancy.11 As reported, mortality stems variously from natural causes, especially cardiovascular disorders2 7 10 and from unnatural causes in particular suicide.1 3 11
After their introduction in the 1950s, the antipsychotic drugs were seen as having a beneficial effect on death rates in psychosis.12 13 However, death rates now appear to be increasing10 14 and this has led to concerns that antipsychotics with adverse cardiovascular profiles could aggravate this trend, with particular concerns for the elderly.15 16
The majority of studies have been cross-sectional in design. They also lack data on patients not treated with antipsychotic medication. These factors make it difficult to pinpoint the effects of treatment and hinder efforts to devise interventions for risks that may arise at different stages of an illness. Owing to the geographical and economic constraints imposed by North-West Wales, we have been able to design a study that addresses some of these issues, and overcomes selection biases. We have logged all admissions for schizophrenia and related non-affective psychoses from 1994 to 2010, and followed up all admissions during this period. We also have a database of all admissions to the North Wales asylum in Denbigh between 1875 and 1924 complete with subsequent clinical records and thus have data on causes of mortality in an untreated cohort of psychotic patients. Finally we have separated delusional disorder, acute and transient psychoses and schizophrenia in both historical and contemporary databases in an effort to link specific hazards to clinical syndromes. The resulting databases allow different perspectives to be brought to bear on the data arising from other studies.
Method
We have used two datasets to look at outcome data for schizophrenia and other non-affective psychoses drawn from the periods 1875–1924 and 1994–2010. The methods used for case definition are described in detail in an accompanying article on the incidence of psychoses during these two periods.17
Patients in both historical and contemporary cohorts were allocated to five diagnostic groups: schizophrenia (F20), schizoaffective disorder (F25), delusional disorder (F22), acute and transient psychoses (F23) and other patients who were difficult to classify, coded as unspecified non-organic psychosis (F29). One co-author (SCL) reviewed all affective and non-affective diagnoses covering eight randomly picked years from the 1875 to 1924 period. The agreement concerning the schizophrenic diagnoses (F20) between the initial rater and SCL was 96.5%. To take account of the number of agreements expected by chance, we used Cohen's κ-coefficient, a statistical measure of inter-rater agreement for categorical items.18 The κ-coefficient (781 cases, two raters, for schizophrenia versus all other diagnoses) was 86%.
Deaths
In the historical cohort, all deaths in hospital (N=764) were recorded in the patients’ medical records. Of these, 58% had recorded postmortems. In addition there were 10 patients who were discharged gravely ill to die at home. We have counted these patients as deaths in the year of discharge and assigned a cause of death consistent with the clinical picture outlined in the records. There were 300 patients (28%) who were discharged recovered and healthy within the 10 years from the date of first admission, on whom there is no further data.
We followed up contemporary patients, using their National Health Service number, even when they had moved out of area. All deaths were established through coroner's records, along with contacts with the patient's general practitioner and treating team. The contemporary database was updated at regular 3-monthly intervals, and accordingly all deaths were investigated and confirmed the year they happened. No patients were lost to follow-up.
Survival analysis
To account for the different lengths of follow-up, primarily in the contemporary cohort, we have undertaken survival analyses on both historical and contemporary cohorts.19In the case of the historical cohort, a survival analysis gives patients discharged healthy and lost to follow-up the same rate of death as is found in the observed cohort. Because death from tuberculosis in particular was much commoner in hospital, this underestimates the survival probability in discharged patients. We have therefore undertaken a further analysis in the historical cohort that assumes no recovered patients died within the 10-year timeframe (best case scenario). The true result is likely to lie somewhat closer to the best case than to the observed outcomes.
Death rates
We have used mortality data from 1900 to 1910 for England and Wales on which to base our calculations of standardised mortality ratios (SMRs) for 1875–1924, as data before 1900 and for the period surrounding the Great War are not available.20 For the historical sample we took the mean value of the years from 1901 to 1910 for each age and sex grouping. Given a decline in death rates from 1875 to 1900 and greater mortality between 1914 and 1920 linked to the Great War and the influenza epidemic of 1918–1920, the 1901–1910 group is likely to lead to higher SMRs in the historical sample than is warranted.
For the contemporary data we worked from available mortality data from 1994 to 2010.21 In the case of contemporary suicides we have standardised deaths by suicide in all psychoses and for schizophrenia by age, sex and year against the deaths from suicide in Wales alone rather than deaths from suicide in England and Wales. Annual suicide statistics in both Wales and England include a proportion of open verdict deaths. We have taken this into account in calculating suicide-specific SMRs.
When computing standardised death rates for successive years, we removed all patients who died the previous year and have not included patients for whom we do not have full follow-up data. This gives contemporary cohorts of 337 at year 2, 322 at year 3, 313 at year 4 and 288 at year 5. We have then used person years at risk when calculating SMRs.
For the purposes of accounting for possible deaths in our recovered discharges from the historical cohort, we have calculated two sets of SMRs. A best-case scenario assumes that patients discharged in apparent good health survived the remainder of the period of observation. A worst-case scenario assumes that these recovered and healthy patients died at the same rate in subsequent years as those remaining in hospital. This procedure seems likely to overestimate the rate of death in the historical cohort.
Years of life lost
In both historical and contemporary cohorts we have calculated years of life lost. In the historical cohort we have taken life expectancy in the period 1901–1910 as the basis of our calculations. For patients admitted up to the age of 44 this has meant a projected life expectancy for men of 62 years and for women of 65 years; for men and women between 45 and over the figures were 68 and 71 years, respectively. In the historical cohort the analysis is based on known age of death.
In the contemporary cohort we have observed years of life lost in the cohort of patients who have completed 10 years. Our sample size and the nature of the cohort do not permit a trend analysis across ages to establish projected life expectancies.
Results
This study is linked to a study looking at the incidence of admissions for schizophrenia and related psychoses that identified 1074 cases in the historical period and 355 cases in the contemporary period. We found an increase in the admission incidence for schizophrenia between 1875 and 1900 when standardised against population norms, a drop in admission incidence for schizophrenia between 2005 and 2010, and a switch in gender ratios from an equal rate of male and female admissions in the 19th century to a rate of two males for each female admission in the contemporary sample.17
Cause of death
Causes of death by diagnosis after 1, 5 and 10 years from first admission in the contemporary and historical samples are laid out in tables 1 and 2.
Table 1.
Contemporary sample: cause of death by diagnosis
| Schizophrenia (F20/F25) N=227 |
Delusional disorder (F22) N=48 |
Acute and transient psychosis (F23) N=66 |
Other psychoses (F29) N=14 |
All psychoses N=355 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cause of death | 1 year | 5 year | 10 year | 1 year | 5 year | 10 year | 1 year | 5 year | 10 year | 1 year | 5 year | 10 year | 1 year | 5 year | 10 year |
| Suicide/open | 7 | 10 | 12 | 0 | 0 | 1 | 1 | 2 | 2 | 0 | 1 | 1 | 8 | 13 | 16 |
| Cardiovascular | 0 | 0 | 0 | 0 | 2 | 3 | 0 | 3 | 4 | 1 | 1 | 1 | 1 | 6 | 8 |
| Respiratory | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| Cancer | 0 | 0 | 0 | 0 | 1 | 2 | 1 | 2 | 2 | 0 | 1 | 1 | 1 | 4 | 5 |
| Other | 0 | 1 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 3 |
| All causes | 7 | 11 | 13 | 0 | 4 | 9 | 2 | 7 | 8 | 1 | 3 | 3 | 10 | 25 | 33 |
| Average age of death | 29.5 | 31.3 | 31.6 | – | 78.6 | 72.7 | 54.7 | 60.3 | 60.9 | 39.5 | 45.9 | 45.9 | 35.6 | 48.7 | 51.2 |
Table 2.
Historical sample: cause of death by diagnosis
| Schizophrenia F20/F25 N=605 |
Delusional disorder F22 N=143 |
Acute and transient psychosis F23 N=143 |
Other psychoses F29 N=135 |
Catatonia F06.1/F20.2 N=48 |
All psychoses N=1074 |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cause of death | 1 year | 5 year | 10 year | 1 year | 5 year | 10 year | 1 year | 5 year | 10 year | 1 year | 5 year | 10 year | 1 year | 5 year | 10 year | 1 year | 5 year | 10 year |
| Suicide | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
| Cardiovascular | 0 | 1 | 17 | 1 | 7 | 12 | 0 | 0 | 1 | 2 | 6 | 9 | 1 | 3 | 5 | 4 | 17 | 44 |
| Respiratory | 5 | 14 | 20 | 1 | 5 | 9 | 2 | 4 | 4 | 1 | 2 | 6 | 3 | 5 | 6 | 12 | 30 | 45 |
| Cancer | 0 | 0 | 0 | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 1 | 3 | 4 |
| Tuberculosis | 6 | 51 | 82 | 0 | 4 | 8 | 2 | 2 | 2 | 1 | 5 | 6 | 1 | 5 | 5 | 10 | 67 | 103 |
| Dysentery | 1 | 4 | 8 | 0 | 1 | 1 | 0 | 0 | 1 | 2 | 2 | 2 | 3 | 3 | 3 | 6 | 10 | 15 |
| Other | 2 | 10 | 24 | 1 | 5 | 8 | 3 | 3 | 3 | 3 | 6 | 8 | 7 | 9 | 10 | 16 | 33 | 53 |
| All causes | 15 | 81 | 153 | 4 | 23 | 40 | 7 | 9 | 11 | 9 | 23 | 33 | 15 | 25 | 29 | 50 | 161 | 266 |
| Average age of death | 40.4 | 37.0 | 45.6 | 49.5 | 55.6 | 58.4 | 40.5 | 43.3 | 46.2 | 48.2 | 51.2 | 56.6 | 45.7 | 43.3 | 44.7 | 44.9 | 46.1 | 50.3 |
‘Other’ causes of death in the historical sample include ‘exhaustion’, septicaemia, kidney disease and erysipelas.
There is a clear difference in age of death in those dying from suicide compared with deaths from cardiovascular causes and a clear difference in age of death for those diagnosed with schizophrenia compared with the ages of death for those other psychotic diagnoses in the contemporary cohort. There are differences between age of death from tuberculosis and cancer in the historical cohort. To explore the interaction between age, diagnosis and cause of death we have laid out the mean age of death by specific causes in both contemporary and historical samples in table 3A,B.
Table 3B.
Other psychoses: Causes of and age at death—contemporary and historical samples
| Contemporary sample |
Historical sample |
||||||
|---|---|---|---|---|---|---|---|
| Age group | Cause of death | Year 1 (n=128) | Years 2–5 (n=104)* | Total 5 years (n=104)* | Year 1 (n=421) | Years 2–5 (n=421) | Total 5 years (n=421) |
| 15–44 | Tuberculosis | – | – | – | 3 | 4 | 7 |
| Respiratory | – | – | – | 3 | 1 | 4 | |
| Cardiovascular | 1 | 1 | 2 | – | 1 | 1 | |
| Cancer | – | – | – | – | – | – | |
| Other | – | – | – | 2 | 1 | 3 | |
| Suicide | 1 | 1 | 2 | – | – | – | |
| 45–74 | Tuberculosis | – | – | – | – | 4 | 4 |
| Respiratory | – | – | – | 1 | 6 | 7 | |
| Cardiovascular | – | 2 | 2 | 3 | 9 | 12 | |
| Cancer | 1 | 3 | 4 | 1 | 2 | 3 | |
| Other | – | – | – | 7 | 7 | 14 | |
| Suicide | – | 1 | 1 | – | – | – | |
| 75+ | Tuberculosis | – | – | – | – | – | |
| Respiratory | – | 1 | 1 | – | – | – | |
| Cardiovascular | – | 2 | 2 | – | – | – | |
| Cancer | – | – | – | – | – | – | |
| Other | – | – | – | – | – | – | |
| Suicide | – | – | – | – | – | – | |
| All ages | All deaths | 3 | 11 | 14 | 20 | 35 | 55 |
| All deaths (excl tuberculosis, %) | 3 (2.34) | 11 (10.57) | 14 (13.46) | 17 (4.03) | 27 (6.41) | 44 (10.45) | |
Figures exclude patients with incomplete 5-year histories.
Table 3A.
Schizophrenia: Causes of and age at death—contemporary and historical samples
| Contemporary sample |
Historical sample |
||||||
|---|---|---|---|---|---|---|---|
| Age group | Cause of death | Year 1 (n=227) | Years 2–5 (n=203)* | Total 5 years (n=203)* | Year 1 (n=653) | Years 2–5 (n=653) | Total 5 years (n=653) |
| 15–44 | Tuberculosis | – | – | – | 6 | 42 | 48 |
| Respiratory | – | – | – | 5 | 7 | 12 | |
| Cardiovascular | – | – | – | – | – | – | |
| Cancer | – | – | – | – | – | – | |
| Other | – | 1 | 1 | 4 | 10 | 14 | |
| Suicide | 6 | 2 | 8 | 1 | – | 1 | |
| 45–74 | Tuberculosis | – | – | – | 1 | 7 | 8 |
| Respiratory | – | – | – | 3 | 4 | 7 | |
| Cardiovascular | – | – | – | 1 | 3 | 4 | |
| Cancer | – | – | – | – | – | – | |
| Other | – | – | – | 9 | 3 | 12 | |
| Suicide | 1 | 1 | 2 | – | – | – | |
| 75+ | Tuberculosis | – | – | – | – | – | – |
| Respiratory | – | – | – | – | – | – | |
| Cardiovascular | – | – | – | – | – | – | |
| Cancer | – | – | – | – | – | – | |
| Other | – | – | – | – | – | – | |
| Suicide | - | – | – | – | – | – | |
| All ages | All deaths | 7 | 4 | 11 | 30 | 76 | 106 |
| All deaths (excl tuberculosis, %) | 7 (3.08) | 4 (1.97) | 11 (5.41) | 24 (3.68) | 34 (5.21) | 58 (8.88) | |
In the case of contemporary suicides, the 16 deaths comprised of 12 suicide, 3 open verdicts and 1 death by misadventure. The open verdicts were regarded by the treating teams as suicides. The death by misadventure involved an overdose on psychotropic drugs. We have accordingly classified these deaths with suicide rather than under the heading of ‘other’. Only one open verdict happened within the first year of admission, in a patient with schizophrenia.
In the historical cohort, many patients with schizophrenia spent their life in the hospital, so that we know the nature of their final illnesses. In total, 32 psychotic patients (25 with schizophrenia) died in hospital from cancer. Of these 32 deaths, 28 involved cancer of the gastrointestinal tract. There was one breast cancer and no lung cancers.
Tuberculosis was the greatest hazard for patients admitted to the asylum, especially for younger patients, who show a spike in deaths from this cause 3–5 years after admission. The drop in mean age of death at year 5 in table 2 reflects this. Table 3 shows a full break-down of deaths by diagnosis and age.
Survival analysis
A survival analysis of the contemporary cohort for all psychoses shows a cumulative 10-year survival probability of 90% (90% CI 0.86 to 0.92, figure 1A). For schizophrenia, the 10-year cumulative survival probability is 94% (90% CI 0.91 to 0.96, figure 1B). For other psychoses the 10-year cumulative survival probability is 81% (90% CI 0.74 to 0.87, figure 1C).
Figure 1.
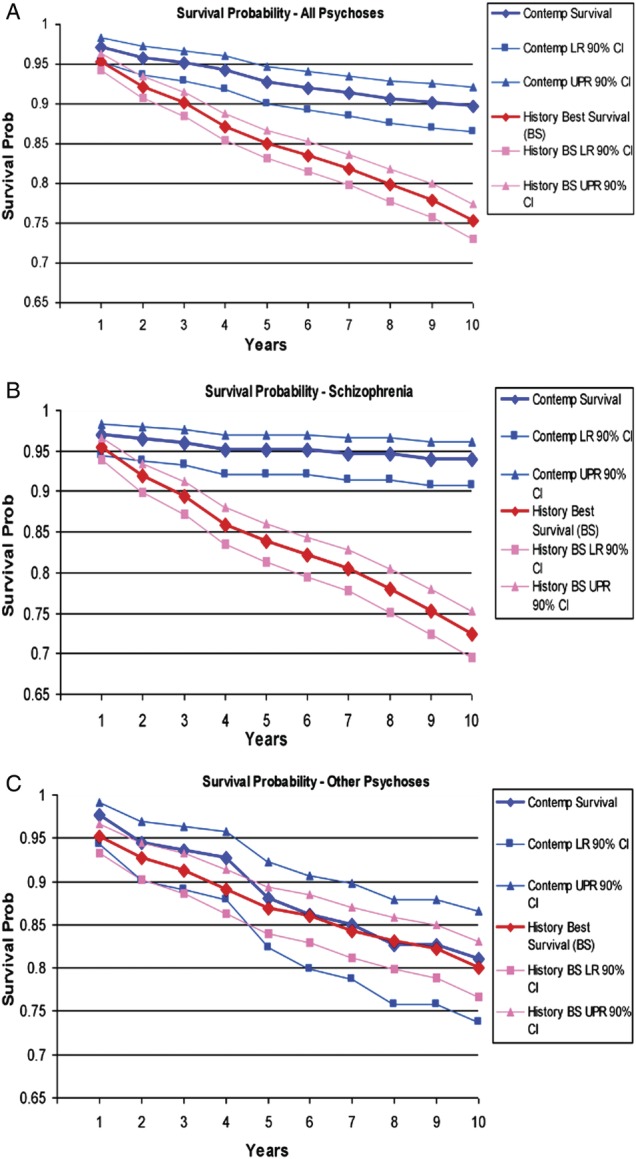
(A) Survival probabilities in all psychose in contemporary and historical cohorts. (B) Survival probabilities in schizophrenia (F20, 25 and 061) in contemporary and historical cohorts. (C) Survival probabilities in other psychoses (F22, 23 and 29) in contemporary and historical cohorts.
In the historical cohort, analysing all discharges as dying at the same rate as those left in hospital produces 10-year cumulative survival probabilities for all psychoses of 69% (90% CI 0.66 to 0.71); for schizophrenia of 69% (90% CI 0.66 to 0.72) and for other psychoses of 63% (90% CI 0.57 to 0.69). Analysing observed deaths as though they were all deaths (best case scenario) produces 10-year cumulative survival probabilities for all psychoses of 75% (90% CI 0.73 to 0.77); for schizophrenia of 72% (90% CI 0.70 to 0.75); and for other psychoses of 80% (90% CI 0.77 to 0.83).
Standardised mortality rates
We have calculated SMRs for contemporary (see table 4) and historical cohorts (tables 5 and 6) for 1, 2, 3, 4 and 5 years from first admission. The contemporary SMRs show a marked increase over population norms in the first year of admission. The rates thereafter remain elevated compared with population norms but fall towards rates reported by other studies. Contemporary death rates are as high as those found in the historical cohort.
Table 4.
Standardised mortality ratios (SMRs) contemporary sample
| SMR year 1 | SMR year 2 | SMR year 3 | SMR year 4 | SMR year 5 | Average 5-year SMR | |
|---|---|---|---|---|---|---|
| Male | ||||||
| All psychosis | 11.1 (CI 4.4 to 23.0) N=218 |
1.0 (CI 1.6 to 6.6) N=208 |
3.5 (CI 0.3 to 13.0) N=203 |
3.8 (CI 0.4 to 13.9) N=197 |
5.9 (CI 1.1 to 17.2) N=180 |
4.9 (CI 0.85 to 15.2) |
| Schizophrenia | 28.6 (CI 7.4 to 73.9) N=150 |
1.0 (CI 7.4 to 30.2) N=144 |
7.9 (CI 0.003 to 45.1) N=143 |
16.7 (CI 1.6 to 61.3) N=139 |
1.0 (CI 8.7 to 35.6) N=127 |
11.2 (CI 0.3 to 51.0) |
| Female | ||||||
| All psychosis | 4.3 (CI 0.8 to 12.7) N=136 |
7.4 (CI 2.3 to 17.3) N=129 |
1.0 (CI 1.6 to 6.5) N=119 |
1.7 (CI 0.001 to 9.8) N=116 |
3.5 (CI 0.3 to 12.9) N=108 |
3.5 (CI 0.4 to 12.2) |
| Schizophrenia | 44.8 (CI 8.1 to 126.9) N=76 |
16.7 (CI 0.01 to 95.5) N=73 |
1.0 (CI 16.0 to 65.3) N=70 |
1.0 (CI 16.0 to 65.3) N=69 |
1.0 (CI 18.5 to 75.4) N=65 |
13.2 (CI 0.1 to 89.2) |
| Total | ||||||
| All psychosis | 7.5 (CI 3.6 to 13.9) N=355 |
3.9 (CI 1.2 to 9.3) N=337 |
1.7 (CI 0.2 to 6.3) N=322 |
2.7 (CI 0.5 to 8.0) N=313 |
4.6 (CI 1.5 to 10.9) N=288 |
4.2 (CI 1.3 to 9.9) |
| Schizophrenia | 33.3 (CI 13.2 to 69.1) N=227 |
5.3 (CI 0.002 to 30.2) N=217 |
5.4 (CI 0.002 to 30.7) N=213 |
11.1 (CI 1.0 to 40.9) N=208 |
1.0 (CI 5.9 to 24.2) N=192 |
11.8 (CI 1.4 to 41.3) |
Table 5.
Standardised mortality ratios (SMRs) history sample—observed deaths
| SMR year 1 | SMR year 2 | SMR year 3 | SMR year 4 | SMR year 5 | Average 5-year SMR | |
|---|---|---|---|---|---|---|
| Male | ||||||
| All psychosis | 2.9 (CI 1.7 to 4.6) N=516 |
2.8 (CI 1.5 to 5.0) N=385 |
1.9 (CI 0.7 to 3.8) N=354 |
3.5 (CI 1.9 to 6.0) N=337 |
3.6 (CI 1.8 to 6.2) N=313 |
2.9 (CI 2.2 to 3.7) |
| Schizophrenia | 2.1 (CI 0.7 to 4.9) N=301 |
2.8 (CI 1.0 to 6.2) N=273 |
3.0 (CI 1.1 to 6.5) N=258 |
4.1 (CI 1.8 to 8.1) N=246 |
3.7 (CI 1.5 to 7.7) N=234 |
3.1 (CI 2.1 to 4.4) |
| Female | ||||||
| All psychosis | 5.5 (CI 3.8 to 7.8) N=558 |
5.3 (CI 3.3 to 8.0) N=410 |
4.1 (CI 2.3 to 6.8) N=366 |
5.6 (CI 3.4 to 8.7) N=340 |
3.7 (CI 1.8 to 6.6) N=306 |
5.0 (CI 4.0 to 6.0) |
| Schizophrenia | 4.3 (CI 2.0 to 7.9) N=304 |
5.7 (CI 2.9 to 10.0) N=274 |
3.7 (CI 1.5 to 7.6) N=253 |
7.0 (CI 3.7 to 12.1) N=242 |
4.1 (CI 1.6 to 8.5) N=222 |
4.9 (CI 3.7 to 6.5) |
| Total | ||||||
| All psychosis | 4.2 (CI 3.1 to 5.5) N=1074 |
4.1 (CI 2.8 to 5.7) N=795 |
3.0 (CI 1.9 to 4.5) N=720 |
4.5 (CI 3.1 to 6.4) N=677 |
3.6 (CI 2.3 to 5.4) N=619 |
3.9 (CI 3.3 to 4.6) |
| Schizophrenia | 3.2 (CI 1.8 to 5.2) N=605 |
4.3 (CI 2.5 to 6.8) N=547 |
3.3 (CI 1.8 to 5.7) N=511 |
5.5 (CI 3.4 to 8.5) N=488 |
3.9 (CI 2.1 to 6.6) N=456 |
4.0 (CI 3.5 to 5.0) |
Table 6.
Standardised mortality ratios (SMRs) history sample—observed and inferred deaths
| SMR year 1 | SMR year 2 | SMR year 3 | SMR year 4 | SMR year 5 | Average 5-year SMR | |
|---|---|---|---|---|---|---|
| Male | ||||||
| All psychosis | 3.6 (CI 2.2 to 5.4) N=516 |
3.8 (CI 2.1 to 6.1) N=385 |
2.6 (CI 1.3 to 4.9) N=354 |
5.2 (CI 3.1 to 8.1) N=337 |
5.3 (CI 3.2 to 8.5) N=313 |
4.0 (CI 3.2 to 5.0) |
| Schizophrenia | 2.5 (CI 0.9 to 5.5) N=301 |
3.3 (CI 1.3 to 6.8) N=273 |
3.5 (CI 1.4 to 7.2) N=258 |
4.6 (CI 2.1 to 8.8) N=246 |
4.2 (CI 1.8 to 8.4) N=234 |
3.6 (CI 2.5 to 4.9) |
| Female | ||||||
| All psychosis | 6.7 (CI 4.8 to 9.2) N=558 |
7.0 (CI 4.7 to 10.1) N=410 |
5.7 (CI 3.6 to 8.8) N=366 |
8.2 (CI 5.5 to 11.9) N=340 |
5.7 (CI 3.3 to 9.2) N=306 |
6.7 (CI 5.6 to 8.0) |
| Schizophrenia | 4.7 (CI 2.3 to 8.4) N=304 |
6.2 (CI 3.3 to 10.6) N=274 |
4.2 (CI 1.8 to 8.3) N=253 |
8.1 (CI 4.5 to 13.4) N=242 |
4.7 (CI 2.0 to 9.3) N=222 |
5.6 (CI 4.2 to 7.2) |
| Total | ||||||
| All psychosis | 5.1 (CI 3.9 to 6.6) N=1074 |
5.4 (CI 3.9 to 7.2) N=795 |
4.2 (CI 2.8 to 5.9) N=720 |
6.6 (CI 4.9 to 8.8) N=677 |
5.5 (CI 3.8 to 7.7) N=619 |
5.3 (CI 4.6 to 6.1) |
| Schizophrenia | 3.6 (CI 2.1 to 5.7) N=605 |
4.7 (CI 2.9 to 7.3) N=547 |
3.8 (CI 2.1 to 6.3) N=511 |
6.3 (CI 4.0 to 9.4) N=488 |
4.5 (CI 2.5 to 7.2) N=456 |
4.5 (CI 3.7 to 5.6) |
The suicide-specific SMR in the contemporary cohort for year 1 for all psychoses is 133 (95% CI 58 to 263) and for schizophrenia is 168 (95% CI 67 to 346). The suicide-specific SMR for years 1–5 combined for all psychosis is 47 (95% CI 25 to 81), and for schizophrenia is 51.5 (95% CI 25 to 95).The suicide-specific SMR for all psychoses for years 1–10 combined is 34 (95% CI 19 to 55), and for schizophrenia is 35 (95% CI 18 to 61).
There was one open verdict in the year 1 figures, which is more likely than not to have been included in national figures as a suicide. In the case of the 10-year figures, there were in total four open verdicts. Excluding all of these would give a 10-year suicide-specific SMR for all psychoses of 25 (95% CI 13 to 44) and for schizophrenia of 23 (95% CI 10 and 46).
On the basis of number of patient exposure years, the SMR for death from cancer in the historical cohort was 3.49 (95% CI 2.25 to 5.15)-fold higher than the population norm at the time. Calculating an SMR for deaths from tuberculosis based on years exposure and deaths within the first 10 years of admission gives an SMR of 9.37 (95% CI 7.64 to 11.4) compared with the population in general, with the figures being twice as bad for women as for men.
Years of life lost
In the historical cohort the confirmed deaths allow estimates of years of life lost. For all psychoses years of life lost range from 9.8 years per patient in the confirmed death group to a possible 5.9 years per patient if those discharged died at the same rate as the rest of the population. For schizophrenia in the historical cohort, the years of life lost range from 10.8 in the confirmed death group to 8.0 when discharged patients are included in the analysis. For other psychoses, the years of life lost range from 6.8in the confirmed dead group to 2.5 when extrapolated to include discharged patients.
In the contemporary cohort with complete 10-year follow-up (N=210), we have data on 143 patients with schizophrenia, and 67 with other psychoses. Patients with all psychoses lost 999 years between them. Patients with schizophrenia lost 613 or 4.3 years each. Patients with other psychoses lost 5.8 years on average.
Discussion
This is the first attempt to calculate survival curves and standardised death rates for schizophrenia and related psychoses in an epidemiologically complete cohort of admissions from the late 19th and early 20th centuries. It enables us to explore contemporary causes of mortality in a way not possible for other studies, and to assess whether death rates in schizophrenia are getting worse over time.
The survival analysis shows the absolute mortality in the historical period was higher than today, but historical SMRs overlap the SMRs for patients reported in recent studies. The actual years of life lost in our historical cohort are less than those lost now.5 11 The main hazard of asylum care for younger people, particularly women, a century ago lay in the risk of contracting tuberculosis. Another hazard was lethal catatonia which seems likely to have accounted for most deaths from exhaustion.22
The SMR we report for schizophrenia at the end of the first year of admission is higher than the SMR from the historical cohort but is consistent with reports showing increased death rates for patients with psychotic disorders in the first year of admission today,23 and reports indicating this stems primarily from suicide.1 6 11 Our contemporary SMR at 5 years for all psychoses moreover overlaps rates reported in other studies.10
This combination of findings brings out the value of a cohort study and the importance of diagnosis. When the data are examined by diagnosis and time from first admission, the findings reveal patterns not apparent in cross-sectional studies. Cross-sectional studies miss the impact of first admissions which account for less than 15% of admissions for psychosis.
The data on suicide in the historical and contemporary samples are strikingly different. In the historical records, it was mandatory for the admitting clinician to record suicide risk and 25% of the historical patients at admission had threatened or attempted suicide. The lack of subsequent suicides raises a number of questions. Was there a bias against a diagnosis of suicide? In the case of historical patients admitted for severe depressive disorders, a number are clearly recorded as dying from suicide and as attempting suicide both in the asylum and soon after discharge so that there was no reticence about recording such verdicts for other patients at this time.24 Furthermore, the case notes of patients dying from tuberculosis and other causes contain clinical details consistent with these diagnoses. A bias against recording suicide verdicts in the schizophrenia group can probably be ruled out.
To suicide you need to have opportunity to commit suicide. The registration of suicidal tendencies in the historic cohort meant that patients were monitored. Both schizophrenic and affective disorder patients were monitored, but affective disorder patients went on to commit suicide at expected rates whereas the schizophrenic patients did not. In addition, the monitoring of patients in the asylum was by the same methods used today. There was not an undue restriction of liberty by today's standards. Historical patients with schizophrenia spent 99% of their time at liberty working on the hospital farm, in the knitting rooms or kitchens, with ample opportunity to commit suicide.
A second issue is whether patients today are more severely ill than a century ago. This seems unlikely for a number of reasons. First, the more malignant psychoses (hebephrenic and catatonic schizophrenia) were present in the historical cohort but have close to disappeared now. Second, historical patients were detained compulsorily whereas many patients today are voluntary admissions; it is therefore easier for less severely ill patients to get admitted now. Third, patients today have immediate access to medication that for many can be expected to mitigate the most distressing aspects of their disorder. In the case of catatonic syndromes, benzodiazepines eliminate the disorder now, while a higher proportion of these patients died in hospital historically than for any other form of psychosis (60%, see table 2).
The importance of the historical cohort in this study is that it demonstrates that suicide is not an inherent risk of schizophrenia. The historical data suggest that there is something about the modern delivery of care that contributes to suicide as an outcome. If suicide risk is not inherent in the illness, another possibility lies in deinstitutionalisation. As in our data, Mortensen and Juel1 flagged up the incident year of a schizophrenic illness as problematic. They suggest the high rates of suicide at this time might stem from deinstitutionalisation. However, more recent Nordic data argue against deinstitutionalisation as the cause of the problem, as life expectancies have slightly increased (or at least not fallen further) as deinstitutionalisation has progressed,11 and suicide rates have fallen rather than got worse.25 Moreover, contemporary patients with schizophrenia had a mean duration of admission lasting weeks rather than months and hence institutionalisation cannot have set in.
Patients who have schizophrenia are also subjected to stigma, and lack of family support. It has also been argued that antipsychotics can restore insight and this might lead to suicide. It would clearly be difficult to discount these possibilities if the suicides were happening 5 or 10 years into the illness. But the fact that suicides happen in the first year, before stigma has set in, or supports have been lost, make such factors less likely to be sole determinants of suicides.
Men are in general more likely to commit suicide than women, and in the contemporary schizophrenia sample there was a twofold greater rate of male admissions than in the historical cohort, but the increased suicide rate in the contemporary sample does not stem from this source in that in the contemporary schizophrenia sample there was a greater proportion of female than male suicides.
Suicide in schizophrenia is likely to be multifactorial in origin. One contributory factor may be treatment. A high rate of suicide in the first year of treatment, across diagnostic groups, is consistent with an initial exposure of vulnerable individuals to the dysphoric effects of antipsychotics. The elimination of individuals at risk to such effects would produce precisely the drop in SMR over time found in our study. The antipsychotics are in fact the only element of the picture to have been shown in placebo-controlled trials to be linked to an excess of suicides in psychosis, although the data are of poor quality.26 A recent observational study has also linked benzodiazepine usage to suicidal deaths in psychotic patients.27
Wahlbeck et al11 report SMRs for suicide from national cohorts of patients recruited in Denmark, Finland and Sweden of 20.6 for men and 36.6 for women. These figures map on to the suicide-specific SMR for schizophrenia reported here for years 1–10 of follow-up (35). Removing all suicides from the contemporary cohort gives an SMR for schizophrenia of 1.1 (95% CI 0.01 to 6.4), and of 1.9 (95% CI 1.0 to 3.4) for all psychoses.
An SMR of 1.9 maps onto figures cited for mortality in schizophrenia drawn from samples that contain subjects later in the trajectory of their illness. The deaths in these other studies have been linked to an increase in risk from cardiovascular causes. Our data support this. We have found high death rates in the contemporary patients with acute and transient psychoses (F23) (table 1). Our data are consistent with other studies.2 23 In this group over half the mortality stems from cardiovascular causes (table 3B).
Two observations stem from this. First, patients with acute and transient psychoses often get diagnoses of schizophrenia. Studies that do not distinguish between these two groups will lead to increased estimates of cardiovascular risk in schizophrenia. Second, it is older patients in our acute and transient cohort who died from cardiovascular causes. Their average age of death was 63 years. Consistent with this, cardiovascular deaths also featured prominently in the contemporary cohort in patients with delusional disorders (F22), where the average age at death was 74 years. Age is therefore a significant contributor to cardiovascular deaths.
Placebo-controlled trials of antipsychotics in the elderly show an excess of mortality primarily from cardiovascular causes in those on active treatment.15 16 The debate about using antipsychotics in the elderly has focused primarily on their use in dementia patients but our figures suggest the risk may apply in all older subjects.
These data have implications for projected years of life lost in patients with schizophrenia. Our data open up the possibility that estimates based on diagnoses that fail to distinguish between schizophrenia and acute and transient psychoses or delusional disorders may substantially overestimate the years of life lost in schizophrenia proper. For instance all cancers in the contemporary cohort came from the delusional disorder or acute and transient psychosis group. This raises the possibility that these cancers antedated and contributed to the development of rather than stemmed from these mental disorders or their treatment.
While data from the contemporary cohort offer no support for psychosis or its treatment as a cause of cancer, the incidence of gastrointestinal cancers is a striking feature of the historical data. There was only one breast cancer and no lung cancers, while 28 of the 32 cancers were related to the gastrointestinal tract. The official mortality figures for 1910 do not categorise mortality in terms of specific cancers to the extent that would permit a conclusive analysis of these data but it is worth noting that in 1910 the commonest cancers in England and Wales were of the mouth, gut and abdominal organs. Ovarian and breast cancers were commoner than found in our sample. Cancers of other bodily systems were filed under other, and were comparatively rare.
A majority of hospitalised patients with suspected cancers had postmortems and it is possible that a proportion of the increased frequency of cancer diagnosis is an artefact of postmortems. There was, however, concern about food adulteration in the 19th and early 20th centuries raising questions about possible links between this and gastrointestinal cancer as an outcome.
In summary, this study reports elevations in SMRs in schizophrenia and related psychoses over a century with the modern data in some respects worse than the historical data. While it is fashionable to look at mortality as an outcome, it must be emphasised that patients today live outside the asylum. When the antipsychotics were introduced, the benefits of recovery and discharge were widely viewed as warranting a potential reduction in life expectancy.28
Other studies have suggested that patients with schizophrenia are dying prematurely because of lifestyle factors and lack of access to healthcare resources, leading to calls for interventions in these domains. In contrast, the current data point to different hazards arising at different periods of risk, allowing differential interventions. The most striking figure in this study is that eliminating suicide in schizophrenia would restore life expectancy to normal. Checking for dysphoric responses to medication, and being willing to change medication if indicated, is worth pursuing as it might offer one of the greatest possible public health gains in any area of medicine at minimal cost.
Supplementary Material
Footnotes
Contributors: All authors have been involved in this piece of research in terms of contributing to the design, data acquisition, analysis/interpretation along with drafting/revising the manuscript in preparation for the final publication; DH: principal investigator and primary author; JLN: data collection, analysis, study write-up and review; MH: data collection, analysis, study write-up and review; MB: data analysis, study write-up and review; SL: data analysis, study write-up and review; CW: principal statistician; LZ: statistician; APR: study write-up and review.
Competing interests: None.
Ethics approval: This study was approved by the North West Wales NHS Trust ethics committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Extra data can be accessed via the Dryad data repository at http://datadryad.org/ with the doi:10.5061/dryad.b6t13.
References
- 1.Mortensen P, Juel N. Mortality and causes of death in first admitted schizophrenic patients. Br J Psychiatry 1993;163:183–9 [DOI] [PubMed] [Google Scholar]
- 2.Harris EC, Barraclough B. Suicide as an outcome for mental disorders: a meta-analysis. Br J Psychiatry 1997;170:205–28 [DOI] [PubMed] [Google Scholar]
- 3.Brown S, Inskip H, Barraclough B. Causes of the excess mortality of schizophrenia. Br J Psychiatry 2000;177:212–17 [DOI] [PubMed] [Google Scholar]
- 4.Joukamaa M, Heliövaara M, Knekt P, et al. Schizophrenia, neuroleptic medication and mortality. Br J Psychiatry 2006;188:122–7 [DOI] [PubMed] [Google Scholar]
- 5.Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis 2006;3:0180. http://www.cdc.gov/pcd/issues/2006/apr/05_0180.htm [PMC free article] [PubMed] [Google Scholar]
- 6.Bertelsen M, Jeppesen P, Petersen L, et al. Suicidal behaviour and mortality in first-episode psychosis: the OPUS trial. Br J Psychiatry 2007;191(Suppl 51):140–6 [DOI] [PubMed] [Google Scholar]
- 7.Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia. Arch Gen Psychiatry 2007;64:1123–31 [DOI] [PubMed] [Google Scholar]
- 8.Osborn DJ, Levy G, Nazareth Z, et al. Relative risk of cardiovascular and cancer mortality in people with serious mental illness from the United Kingdom's General Practice Research Database. Arch Gen Psychiatry 2007;64:242–9 [DOI] [PubMed] [Google Scholar]
- 9.Tiihonen J, Lönnqvist J, Wahlbeck K, et al. 11 year follow up of mortality in patients with schizophrenia: a population based cohort study. Lancet 2009;374:620–7 [DOI] [PubMed] [Google Scholar]
- 10.Hoang U, Stewart R, Goldacre MJ. Mortality after hospital discharge for people with schizophrenia or bipolar disorder: retrospective study of linked English hospital episode statistics, 1999–2006. BMJ 2011;343:d5422 doi:10.1136/bmjd5422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wahlbeck K, Westman J, Nordentoft M, et al. Outcomes of Nordic mental health systems: life expectancy of patients with mental disorders. Br J Psychiatry 2011;199:453–8 [DOI] [PubMed] [Google Scholar]
- 12.Ban TA. Schizophrenia. p psychopharmacological approach. Springfield, IL: Charles C Thomas, 1972:41–2 [Google Scholar]
- 13.Healy D. The creation of psychopharmacology. Cambridge, MA: Harvard University Press, 2002 [DOI] [PubMed] [Google Scholar]
- 14.Osby U, Correia N, Brandt L, et al. Time trends in schizophrenia mortality in Stockholm County, Sweden: a cohort study. BMJ 2000;321:483–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo controlled trials. JAMA 2005;294:1934–43 [DOI] [PubMed] [Google Scholar]
- 16.Baillard C, Howard R. Neuroleptic drugs in dementia: benefits and harms. Nat Rev Neurosci 2006;7:492–500 [DOI] [PubMed] [Google Scholar]
- 17.Healy D, Le Noury J, Linden S, et al. The incidence of admissions for schizophrenia and related psychoses in two cohorts: 1875–1924 and 1994–2010. BMJ Open 2012;2:e000447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas 1960;20:37–46 [Google Scholar]
- 19.Rothman KJ. Estimation of confidence limits for the cumulative probability of survival in life table analysis. J Chron Dis 1978;31:557–60 [DOI] [PubMed] [Google Scholar]
- 20.Office of National Statistics Twentieth century mortality. One hundred years of mortality data from England and Wales by age, sex, year and underlying causes ONS, 2010 [Google Scholar]
- 21.Office of National Statistics Twenty first century mortality data. ONS, 2010 [Google Scholar]
- 22.Shorter E. What historians and clinicians can learn from the history of medicine; the example of fatal catatonia. Medicina&Storia 2011;21:5–17 [Google Scholar]
- 23.Harris EC, Barraclough B. Excess mortality of mental disorder. Br J Psychiatry 1998;173:11–53 [DOI] [PubMed] [Google Scholar]
- 24.Healy D, Harris M, Tranter R, et al. Lifetime suicide rates in treated schizophrenia: 1875–1924 and 1994–1998 cohorts compared. Br J Psychiatry 2006;188:223–8 [DOI] [PubMed] [Google Scholar]
- 25.Nordentoft M, Laursen TM, Agerbo E, et al. Change in suicide rates for patients with schizophrenia in Denmark, 1981–97: nested case-control study. BMJ 2004;329:261–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Healy D. Shaping the Intimate. Influences on the experience of everyday nerves. Soc Stud Sci 2004;34:219–45 [DOI] [PubMed] [Google Scholar]
- 27.Tiihonen J, Suokas JT, Suvisaari JM, et al. Polypharmacy with antipsychotics, antidepressants, or benzodiazepines and mortality in schizophrenia. Arch Gen Psychiatry 2012;69:476–83 [DOI] [PubMed] [Google Scholar]
- 28.Healy D. Neuroleptics and mortality: a 50-year cycle. Br J Psychiatry 2006;188:128. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


