Abstract
Objective
To investigate the longer-term cost-effectiveness of a nurse-coordinated preventive cardiology programme for primary prevention of cardiovascular disease (CVD) compared to routine practice from a health service perspective.
Design
A matched, paired cluster-randomised controlled trial.
Setting
Six pairs of general practices in six countries.
Participants
1019 patients were randomised to the EUROACTION intervention programme and 1005 patients to usual care (UC) and who completed the 1-year follow-up.
Outcome measures
Evidence on health outcomes and costs was based on patient-level data from the study, which had a 1-year follow-up period. Future risk of CVD events was modelled, using published risk models based on patient characteristics. An individual-level Markov model for each patient was used to extrapolate beyond the end of the trial, which was populated with data from published sources. We used an 11-year time horizon and investigated the impact on the cost-effectiveness of varying the duration of the effect of the intervention beyond the end of the trial. Results are expressed as incremental cost per quality-adjusted life-year gained.
Results
Unadjusted results found the intervention to be more costly and also more effective than UC. However, after adjusting for differences in age, gender, country and baseline risk factors, the intervention was dominated by UC, but this analysis was not able to take into account the lifestyle changes in terms of diet and physical activity.
Conclusions
Although the EUROACTION study achieved healthier lifestyle changes and improvements in management of blood pressure and lipids for patients at high risk of CVD, compared to UC, it was not possible to show, using available risk equations which do not incorporate diet and physical activity, that the intervention reduced longer-term cardiovascular risk cost-effectively. Whether or not an intervention such as that offered by EUROACTION is cost-effective requires a longer-term trial with major cardiovascular events as the outcome.
Trial Registration number
ISRCTN 71715857.
Keywords: Health Economics, Cardiology, Primary Care
Article summary.
Article focus
To investigate the longer-term cost-effectiveness of a nurse-coordinated preventive cardiology programme for primary prevention of cardiovascular disease compared to routine practice.
Key messages
The EUROACTION study achieved healthier lifestyle changes and improvements in management of blood pressure and lipids for patients at high risk of CVD, compared to usual care (UC).
The unadjusted results of the cost-effectiveness analysis found the intervention to be more effective than UC but also more costly. However, the adjusted results showed that the intervention was dominated by UC.
The published cardiovascular risk equations do not take account of lifestyle changes in terms of diet and physical activity and therefore may be inadequate for the evaluation of whether or not a lifestyle intervention to prevent cardiovascular disease is cost-effective.
Strengths and limitations of the study
This is the first study assessing the cost-effectiveness of the EUROACTION programme.
The available cardiovascular risk modelling is based on a limited number of risk factors, which do not include measures of diet or physical activity, and a healthier lifestyle was the most important outcome of the EUROACTION trial.
Introduction
Evidence has shown that individuals with increased risk of cardiovascular disease (CVD) can reduce their risk of cardiovascular morbidity and mortality by stopping smoking, changing their diet, engaging in physical activity, achieving a healthy body weight and controlling their blood pressure, cholesterol and diabetes.1 However, not all patients at high risk of developing CVD manage to achieve these recommended lifestyle and risk factor goals and there remains considerable potential to reduce CVD risk in these patients.2 The EUROACTION study was designed to address the need for preventive cardiology care in everyday clinical practice.3
The EUROACTION study was a matched, paired cluster-randomised controlled trial, across eight countries and 24 hospitals and general practices. The project evaluated the impact of a nurse-coordinated, multidisciplinary preventive cardiology programme for coronary patients in hospital and high-risk individuals in general practice. It aimed to help all these high-risk patients and their families to achieve recommended lifestyle and risk factor targets for CVD prevention in everyday clinical practice over 1 year. The principal results concluded that the EUROACTION programme achieved healthier lifestyle changes and improvements in risk factor management for patients with coronary heart disease (CHD) and those at high risk of CVD, together with their partners, compared to usual care (UC).4
While there is evidence that the EUROACTION programme is effective in terms of modifying lifestyle and some CVD risk factors, there is no evidence as to its cost-effectiveness. Therefore, this paper aims to model the long-term cost-effectiveness of the EUROACTION programme in comparison with UC within the primary care setting.
Methods
Patients
The EUROACTION primary care study took place in Denmark, Italy, Netherlands, Poland, Spain and UK, where a matched pair of general practices was identified, and then randomised to either the EUROACTION programme or to UC. General practioners (GPs) prospectively identified the study population. The comparison was restricted to patients and did not include partners. Eligibility criteria for patients have previously been published.4
All intervention patients were assessed at baseline and at 1 year. These assessments focused on smoking habits, diet and physical activity, measurement of body mass index, blood pressure, cholesterol and glucose levels, and cardiac medications were also recorded. The programme was delivered by specialist nurses, working with GPs, and supported by software programs, educational materials and group workshops to achieve individual goals. Each person was given a personal record card to record lifestyle and risk factor goals, medications and appointments. To avoid the possibility that undergoing baseline assessments might affect outcomes, only a random sub-sample (∼25%) of UC patients were seen at baseline and then all UC patients were invited for assessment at 1 year. In the UC arm, patients did not receive any form of special care.
Model structure
We adopted a health service perspective to measure costs and outcomes. Each cycle in the model is of 1 year's duration. All patients were CVD-free on entering the model. In each subsequent cycle, patients may remain CVD event free, they may have a fatal or non-fatal CVD event, or they may die from non-CVD causes. Once the patient has had an initial CVD event, then in subsequent cycles they move to the post-CVD event states and they may move between different CVD states and/or die from CVD or non-CVD causes.
The CVD event states are: non-fatal myocardial infarction (MI), stable angina, unstable angina, CHD death, transient ischaemic attack (TIA), stroke, CVD death and non-CVD death.
Measuring initial CVD risk
To estimate the risk of an initial CVD event in a subsequent year, we used the D'Agostino et al5 CVD risk function, derived from the Framingham Heart Study. This calculates individual sex-specific risks for future cardiovascular events (in patients initially free of CVD). These CVD risk equations incorporate as risk factors the natural logarithms of age, total and high-density lipoprotein (HDL) cholesterol, systolic blood pressure (SBP) if treated with or without antihypertensive medications, smoking and diabetes. We used the published calibration factors to focus on the CHD and stroke event states.
Ten-year risks were estimated from the equations and adjusted to 1-year values.6 One-year CVD risk beyond the end of the trial was calculated based on both (a) baseline patient characteristics (adjusted for age) for intervention patients only; and (b) 1-year follow-up characteristics for both groups, in order to evaluate any changes to CVD risk factors as a result of the EUROACTION programme.
Validating the appropriateness of the risk functions of the model
We tested the validity of applying the D'Agostino et al5 risk equations to the study population, by comparing the observed number of CHD cases with the number predicted at 1 year. Because stroke and TIA incidence data were not collected in the study we converted the CVD risk equations to CHD risks using the recommended calibration factors.5 We present the results of the comparison for both groups.
Transition probabilities
We disaggregated the overall risk of a CVD event into rates for specific events by age and gender, using UK relative incidence rates based on published literature7–9 and expert opinion, as previously used in Ward et al.10 These event rates were applied to individual annual CVD risks to calculate individual transition probabilities for moving from the CVD free state to the initial CVD event states. Also, individual patients could die from non-vascular causes, depending on their age and gender. The non-CVD death transition probabilities were taken from Briggs et al.11 Transition probabilities for moving from primary event health states to subsequent non-fatal health states are taken from Ward et al.10
Measuring cost
Data on resources used during the trial and staff contacts were recorded in case record forms and were then converted into electronic format. To determine the total 1-year costs for each group, we obtained unit costs for all relevant items of resources used in the trial:
Costs relating to EUROACTION programme and other contacts in primary care were obtained from the programme facilitators and included the EUROACTION nurses costs, training costs, production of patient educational materials and any other costs associated with implementing the programme. The average time spent by staff for all patient contacts at baseline and at 1 year was provided by each centre. Hourly wage rates of the staff salaries and training were calculated and then applied to these various patient contacts. We costed the EUROACTION family information packs, a pocket-sized personal record card, questionnaires and group sessions that each patient in the intervention group received as part of their prevention programme. Costs were applied to other contacts with health care professionals, such as GPs, outside of the intervention programme for both arms and these costs were based on national estimates of the staff salaries involved and estimates of the average time spent with the patient provided by the trial coordinators.
Cardiac-related drug costs. Data were collected on patient-specific cardiac-related medications including the drug name and dose at baseline and at 1 year. This gave point of time information, but no start or end dates. So for each patient it was assumed that they would remain on the same medication at a constant dose for the entire duration, for example, from baseline to 1 year. National cost estimates for the drugs were provided by trial coordinators from each country and were applied accordingly to the relevant dose and length of time on a patient-specific basis.
Cardiac-related procedures and tests. During the trial, patients within both groups may have required inpatient or outpatient admissions for cardiac-related procedures, or undertaken any cardiac-related tests. The procedures were costed according to HRG episodes for each country and the other tests or bed days as simple unit costs. National unit cost estimates for cardiac-related procedures and tests for each country were obtained from a database held by United BioSource Corporation (Erwin De Cock, personal communication, May 2007) for all countries, except Denmark and Poland. For these two countries, national unit cost estimates were provided from contacts within the Centre for Applied Health Services Research and Technology in Denmark (Jan Sørensen, personal communication, January 2007) and from the Ministry of Health in Poland (Andrzej Pająk, personal communication, June 2007).
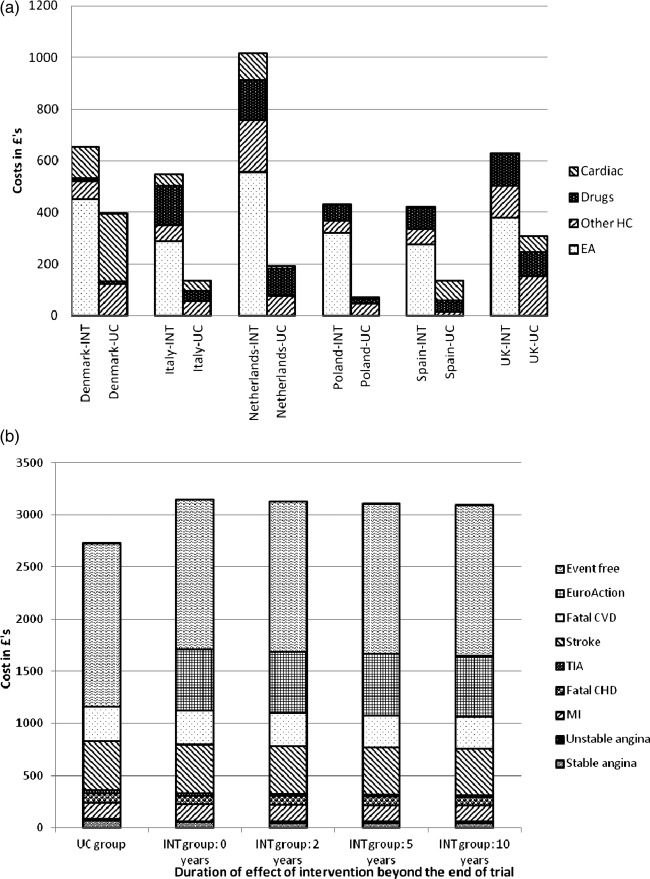
As the study was based in six countries, a costing algorithm was developed to calculate a total cost per patient for each country. The costs of the programme were valued in local currencies and then converted to 2006/2007 £ (GBP) using purchasing power parities.12 Table 1 presents the total 1-year costs by group and country. Figure 1A shows that the 1-year observed costs (split by type of cost) for the intervention group was significantly more than the UC group for all countries. This higher cost was explained by the EUROACTION intervention programme costs and contacts with EUROACTION staff, while neither arms experienced significantly high-cost cardiac interventions or cardiac medications.
Table 1.
Observed 1-year costs for EUROACTION study (in £ GBP)
| 2006/2007 prices | Denmark | Italy | Netherlands | Poland | Spain | UK | Total |
|---|---|---|---|---|---|---|---|
| Intervention | |||||||
| N | 104 | 165 | 191 | 234 | 199 | 126 | 1019 |
| Mean (SD) | £589 (£379) | £595 (£366) | £756 (£466) | £515 (£179) | £588 (£269) | £625 (£181) | £608 (£329) |
| Median | £541 | £562 | £704 | £463 | £550 | £594 | £560 |
| IQR | £473 to £614 | £451 to £680 | £546 to £862 | £374 to £616 | £420 to £714 | £530 to £729 | £449 to £714 |
| Range | £268 to £4054 | £179 to £3733 | £166 to £5064 | £282 to £1578 | £139 to £1669 | £163 to £1206 | £139 to £5064 |
| Usual care | |||||||
| N | 154 | 194 | 123 | 160 | 193 | 181 | 1005 |
| Mean (SD) | £295 (£490) | £201 (£365) | £246 (£307) | £159 (£167) | £138 (£207) | £307 (£563) | £221 (£384) |
| Median | £193 | £146 | £125 | £105 | £68 | £196 | £142 |
| IQR | £152 to £275 | £104 to £198 | £84 to £250 | £84 to £159 | £56 to £122 | £140 to £303 | £90 to £225 |
| Range | £98 to £3364 | £70 to £4455 | £65 to £2806 | £60 to £1255 | £40 to £2173 | £73 to £6500 | £40 to £6500 |
Figure 1.
(A) One-year observed costs for the intervention and usual care groups split by type. EA, EuroAction costs; Other HC, other health care costs; Drugs, cardiac-related medication costs; Cardiac, cardiac procedure costs. (B) Mean costs for the intervention and usual care groups for the main health states in the Markov model.
Subsequent costs relating to health states occupied within the model were based on UK estimates (see online supplementary files). It was assumed that patients in a CVD-free state would continue to receive the cardiac-related medications and primary care contacts (outside of the intervention programme) that they received during the trial. The mean cost of these medications and contacts for all patients across both arms were applied to each individual patient within the model who remained in the event-free health state for subsequent years.
Health state utilities
To estimate quality-adjusted life years (QALYs) the model requires utility values for each state adjusted by age. For patients who were event free, the utility values were based on UK general population norms;13 utilities for events/states were taken from Ward et al,10 which were all were based on UK studies and were obtained using the EQ-5D (see online supplementary files).
Measuring the impact of the intervention
The study provided results only for a 1-year follow-up. We estimated results for a range of possible durations of effect, assuming that the CVD risk reduction experienced by the intervention patients persisted for 0 through to 10 additional years (11-year time horizon), after which they reverted to their individual CVD risk factor levels at the start of the study (adjusted for age). For UC patients, it was assumed that patients would remain at their 1-year CVD risk (adjusted annually by age) throughout the model.
Measuring cost-effectiveness
Using the Markov model we calculated for each patient their expected quality-adjusted survival (based on their likelihood of surviving each cycle and their expected health state utility value) and their expected costs. Cost-effectiveness was measured in terms of the incremental cost per QALY gained (ICER). Future costs and benefits were discounted at 3.5%.14
Statistical analyses
All statistical analyses were performed in Stata V.1015 or Microsoft Excel and a p value ≤0.05 was considered to be statistically significant. We present unadjusted and adjusted cost-effectiveness results. The adjusted results controlled for group allocation, age, gender, age×gender interactions, country and baseline risk factors using ordinary least squares (OLS) regressions. As only a random subsample of UC patients were seen at baseline, regression analyses were used to predict baseline values for those patients who had missing values. For total and HDL cholesterol and SBP, OLS regression was used to predict values in those patients with missing values, as a function of age, gender and country. For the three binary variables (medications, smoking and diabetes), logistic regression models were used to predict the probability of each binary outcome. Predicted values ≥0.5 were categorised to a value of 1 and values <0.5 were categorised as 0. In the adjusted models we also included an indicator for whether or not each control variable was missing.
We represented uncertainty due to sampling variation in both the unadjusted and adjusted cost-effectiveness ratios using non-parametric bootstrapping. In the unadjusted analyses we sampled individuals in our model with replacement and used their costs and outcomes over the 11-year period to compute replications of the incremental cost per QALY gained. We repeated this approach in the adjusted analyses, also adding the regressions to control for confounding factors. In each case, we generated 10 000 bootstrap replications of the cost-effectiveness ratios and used these to construct 95% confidence intervals around the point estimate of cost-effectiveness.
Sensitivity analysis
The main analysis modelling was limited to 10 years, in the absence of robust longer-term risk models. As a sensitivity analysis, we used a simplified longer-term model to check whether the conclusions of the main analysis would have been likely to be different if a longer-term perspective had been adopted, for example, 25 years. This model essentially assumed no further effect of the intervention but modelled out fully the possible QALY gains from the medium-term (11 years) differences in mortality and event rates.
Results
The baseline characteristics for the intervention group as a whole and the UC subsample who were seen at baseline are shown in table 2. There were significant differences in the distribution between countries. Mean total and HDL cholesterol levels were significantly higher for the intervention compared with the UC group. While no statistically significant differences were observed for other baseline characteristics, the 10-year CVD risk at baseline5 was numerically higher for the UC group than the intervention arm.
Table 2.
Baseline characteristics
| Intervention (n=1019) | Usual care subsample (n=252) | Usual care all (n=1005) | Statistical test* (Int. vs. UC subsample) | Statistical test* (Int. vs. UC all) | |
|---|---|---|---|---|---|
| Country | |||||
| Denmark | 104 (10.2%) | 40 (15.9%) | 154 (15.3%) | p=0.012 | p<0.001 |
| Italy | 165 (16.2%) | 47 (18.7%) | 194 (19.3%) | ||
| Netherlands | 191 (18.7%) | 37 (14.7%) | 123 (12.2%) | ||
| Poland | 234 (23.0%) | 45 (17.9%) | 160 (15.9%) | ||
| Spain | 199 (19.5%) | 41 (16.3%) | 193 (19.2%) | ||
| UK | 126 (12.4%) | 42 (16.7%) | 181 (18.0%) | ||
| Gender | |||||
| Male | 507 (49.8%) | 133 (52.8%) | 577 (57.4%) | p=0.390 | p=0.001 |
| Female | 512 (50.3%) | 119 (47.2%) | 428 (42.6%) | ||
| Risk factors required for the D'Agostino equation5 | |||||
| n (%) | |||||
| Non-smoker | 695 (68.2%) | 155 (61.5%) | – | p=0.646 | – |
| Has diabetes | 313 (30.7%) | 68 (27.0%) | – | p=0.247 | – |
| On antihypertensive drugs | 432 (42.4%) | 97 (38.5%) | – | p=0.260 | – |
| Mean (SD) | |||||
| Age | 60.5 (7.6) | 60.4 (7.3) | 61.3 (7.3) | p=0.915 | p=0.011 |
| Systolic blood pressure (mm HG) | 141.1 (18.6) | 141.6 (18.9) | – | p=0.693 | – |
| Total cholesterol (mmol/l) | 5.70 (1.02) | 5.45 (0.99) | – | p=0.001 | – |
| HDL cholesterol (mmol/l) | 1.40 (0.39) | 1.35 (0.36) | – | p=0.047 | – |
| 10-year CVD risk at baseline | 0.115 (0.087) | 0.120 (0.093) | – | p=0.426 | – |
*χ2 tests conducted for categorical variables and t tests conducted for continuous variables.
We modelled 1019 patients in the intervention arm and 1005 patients in the UC arm who were assessed at 1 year.4 The intervention group had fewer men than the UC group: 49.8% vs 57.4% men (p=0.001), and was significantly younger (mean age at 1 year: intervention: 61.5 years vs. UC: 62.3 years, p=0.011).
When testing the validity of the Framingham risk equations to the study population we found that eight intervention patients and one UC subsample patient experienced a CHD event. The risk equations produced a close match, predicting 8.5 patients with a first CHD event in the intervention group and 2.0 in the UC subsample.
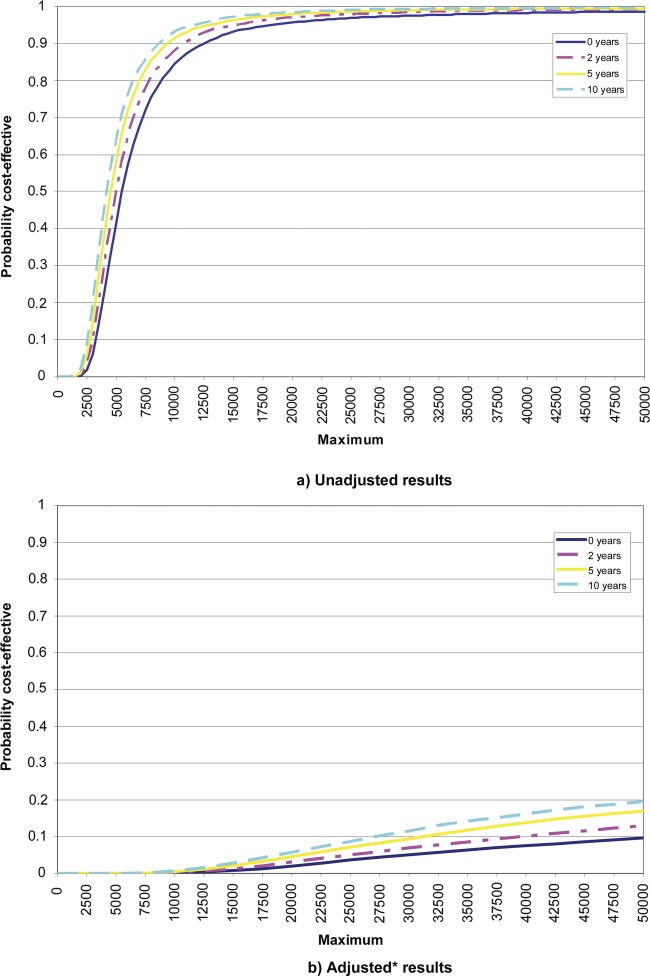
Figure 1B further emphasises that the observed additional costs of the EUROACTION intervention programme and staff costs were not offset by the estimated reduced costs of cardiac interventions in the subsequent years. In terms of the unadjusted results, the incremental costs of the intervention are £362–£419 depending on the duration of the effect of the intervention and the incremental QALYs are 0.076–0.085 (see table 3). As expected, the incremental costs fall and the incremental QALYs rise as the duration of the effect of the intervention beyond the end of the trial increases. The incremental cost per QALY gained range from £5539 (95% CI £2625–£29 627) to £4266 (95% CI £2059 to £15 945). The unadjusted cost-effectiveness acceptability curves (CEACs) under each scenario are in figure 2A and highlights the results in table 3 that in all scenarios over 95% of the bootstrapped replications are less than £20 000.
Table 3.
Results from cost-effectiveness model
| Duration of effect of intervention beyond the end of the trial (model time horizon=11* years in all cases) |
||||
|---|---|---|---|---|
| 0 years | 2 years | 5 years | 10 years | |
| Unadjusted costs and QALYs | ||||
| Usual care mean cost (SD) | £2727 (£29) | £2727 (£29) | £2727 (£29) | £2727 (£29) |
| Intervention mean cost (SD) | £3146 (£33) | £3126 (£31) | £3105 (£31) | £3089 (£31) |
| Usual care mean QALYs (SD) | 6.755 (0.021) | 6.755 (0.021) | 6.755 (0.021) | 6.755 (0.021) |
| Intervention mean QALYs (SD) | 6.831 (0.021) | 6.835 (0.021) | 6.838 (0.021) | 6.840 (0.021) |
| Incremental costs (95% CI) | £419 (£332 to £505) | £399 (£315 to £483) | £378 (£294 to £462) | £362 (£278 to £447) |
| Incremental QALYs (95% CI) | 0.076 (0.017 to 0.135) | 0.079 (0.020 to 0.138) | 0.083 (0.024 to 0.142) | 0.085 (0.026 to 0.144) |
| ICER | £5539 | £5031 | £4561 | £4266 |
| 95% CI | £2625 to £29 627 | £2412 to £22 520 | £2202 to £18 155 | £2059 to £15945 |
| % of bootstrapped ICERs <£20k | 95.7 | 97.0 | 97.9 | 98.4 |
| % of bootstrapped ICERs < £30k | 97.6 | 98.4 | 99.0 | 99.2 |
| Adjusted costs and QALYs‡ | ||||
| Incremental costs (95% CI) | £474 (£368 to £580) | £463 (£358 to £568) | £450 (£343 to £557) | £441 (£331 to £550) |
| Incremental QALYs (95% CI) | −0.009 (−0.041 to 0.023) | −0.007 (−0.038 to 0.025) | −0.005 (−0.036 to 0.027) | −0.003 (−0.035 to 0.029) |
| ICER | Dominated† | Dominated† | Dominated† | Dominated† |
| 95% CI | £21 695 to dominated† | £18 495 to dominated† | £15 908 to dominated† | £14 485 to dominated† |
| % of bootstrapped ICERs <£20k | 1.97 | 3.16 | 4.57 | 5.76 |
| % of bootstrapped ICERs <£30k | 5.05 | 6.98 | 9.42 | 11.54 |
ICER, incremental cost-effectiveness ratio; QALYs, quality-adjusted life years;
*One- year study follow-up period plus a 10-year model.
†The intervention is more costly and yield fewer QALYs than usual care.
‡Adjusting for the following baseline characteristics: age, gender, age×gender, country, total and HDL cholesterol, SBP, antihypertensive medications, smoking and diabetes.
Figure 2.
Cost-effectiveness acceptability curves. (A) Unadjusted results. (B) Adjusted results. *Adjusted for differences between groups by age, gender, country and baseline risk factors.
After controlling for differences in age, gender, country and baseline risk factors, the intervention is associated with higher costs and lower QALYs than the UC arm in every scenario (an example of the various regression models is shown in the online supplementary files). As a result, the intervention is dominated by UC. Although there is considerable uncertainty around those point estimates with the 95% confidence intervals ranging from acceptably cost-effective to highly dominated, the probability of being cost-effective is very low, as shown in the adjusted CEACs in figure 2B (additional adjusted CEACs, controlling for age, gender and country only are in the online supplementary files). At a cost-effectiveness threshold of £20 000 the EUROACTION intervention will be cost-effective in under 6% of cases.
Due to baseline differences, we conducted age–sex-matched subgroup analyses and the adjusted results confirmed that the intervention remained dominated, even when an optimistic timeframe was considered (an example of age–sex-matched subgroup analysis is shown in the online supplementary files).
The sensitivity analysis produced predictable results that in no way changed the conclusions of the analysis. Using the unadjusted data, the cost-effectiveness of the intervention was further enhanced, and using the adjusted data the domination of UC over the intervention remained.
Discussion
Although this large European trial demonstrated that a nurse-coordinated preventive cardiology programme in primary care helped more high-risk patients to achieve the lifestyle and risk factor targets in comparison with UC, this does not appear to be cost-effective. However, these cost-effectiveness analyses require careful qualification because they are subject to a number of uncertainties which are a consequence of the study design and important limitations in the statistical model used.
The differences in the adjusted and unadjusted results emphasise that the study design, based on matching pairs of general practices in each country, did not eliminate baseline differences between the two groups in cardiovascular risk factors. These differences meant that the two groups had different levels of baseline risk, higher in intervention than UC, but the economic results have adjusted for these baseline differences. Though these differences were small in absolute terms they have a substantial effect on the estimates of absolute risk of future cardiovascular events, and therefore on the difference in effectiveness between intervention and UC. Additionally, the study recorded its primary endpoints at baseline and at 1 year, and to avoid ‘contamination’ by recording risk factor levels in UC, baseline measurements were only made in a subsample of UC patients. Thus, we do not have before and after measurements for 75% of the UC patients.
Our cost-effectiveness analysis did not include partners. If partners were included it might improve the cost-effectiveness, but we have no good measure of the effect on partners to know how substantial the impact on the incremental cost-effectiveness ratio might be.
Our estimates of the risk of future CVD events are based on published risk equations.5 These are derived from a large, well-characterised cohort (8491 participants) and predict CVD risk as opposed to CHD risk alone. The C statistic for the model ranges from 0.76 (men) to 0.79 (women), suggesting that additional risk factors could potentially improve the model's discriminatory power. Other risk models have included risk factors such as family history of CVD, social deprivation and biomarkers, for example, hs-CRP,16 17 although these models also have their own limitations.
However, to date lifestyle factors such as dietary habits and physical inactivity, although important in the aetiology of CHD18 and independent of the other major risk factors, have not been included in such risk scores, because they are difficult to accurately quantify. The omission of these important lifestyle factors in the Framingham risk equations may be particularly relevant in our study as the cornerstone of the EUROACTION programme was lifestyle change which was clearly evident in the study's most striking achievements in this area including significantly higher fruit and vegetable consumption (p=0.005); physical activity levels (p=0.01) and weight loss (p=0.005).
It is thus possible that our estimates of relative differences in absolute risk between the groups may understate the full effects of the intervention on long-term CVD risk. However, we showed that the risk equations are able to predict CHD events in the study population in the 1-year follow-up period, but the accuracy of the risk equations over the 10-year period of our study remains untested.
Our modelling also requires an assumption about how long any differential effect of the intervention persists. Nothing is known about the longer-term effects of EUROACTION, and there are few studies that have looked at longer-term changes. The longest follow-up to a relevant lifestyle change appears to be the OXCHECK study, which showed that the benefits of health checks were sustained over 3 years.19 20 However, whatever the duration of effect beyond the trial, and even when a 25-year model was used, the policy conclusions remain the same.
Finally, our model uses a regression analysis approach so that a UK-specific estimate can be drawn from the complete multinational EUROACTION dataset on net resource use, costs and net effects of the intervention. The epidemiological, utilities and cost data for the longer-term modelling of risk and events are based on UK data alone. Thus, the results are applicable to the UK and not specifically to the other EUROACTION countries. While formal analysis would be needed to confirm this, the coefficients on the country parameters in the regression analyses of both costs and outcomes suggest that the cost-effectiveness would be broadly similar in the other countries.
Conclusion
Although the EUROACTION study demonstrated in high-risk patients in primary care significant improvements in lifestyle and CVD risk factors, it is not possible to show, using the best available risk equations, that the intervention was cost-effective. The available risk modelling is based on a limited number of risk factors, which do not include diet or physical activity, and a healthier lifestyle was the most important outcome of this trial. Therefore, whether or not an intervention such as that offered by EUROACTION is cost-effective remains an open question that could be answered by a longer-term trial with major adverse cardiovascular events as the primary endpoint.
Supplementary Material
Acknowledgments
EUROACTION is an initiative of the European Society of Cardiology which highlights its commitment to improve the quality of life of the European population by reducing the impact of cardiovascular diseases. The study protocol conforms to the ethical guidelines of the 1995 Declaration of Helsinki with ethics committee approval in all countries and for every centre. Written informed consent was obtained from every subject.
Appendix
EUROACTION Steering group
A scientific steering group approved the protocol and the design for this matched pair cluster-randomised controlled trial, and is responsible for the scientific integrity of the study. The steering group has the following membership: D Wood (London, UK, Chairman), G De Backer (Ghent, Belgium), D De Bacquer (Ghent, Belgium), M Buxton (Uxbridge, UK), I Graham (Dublin, Ireland), A Howard (Nice, France), K Kotseva (London, UK), S Logstrup (Brussels, Belgium), H McGee (Dublin, Ireland), M Mioulet (Nice, France), K Smith (Dundee, UK), D Thompson (York, UK), T Thomsen (Glostrup, Denmark), T van der Weijden (Maastricht, the Netherlands).
National coordinators
The national coordinators for each country are also members of the steering committee. They are responsible for identifying and recruiting general practices, obtaining ethics committee approval, appointing and supervising staff in the centres and contributing scientifically to the publication of results. The EUROACTION National Coordinators and Primary care leaders are as follows:
Denmark: T Thomsen, K Brockelmann; Italy: P Fioretti, A Desideri, S Brusaferro; Poland: A Pajak, K. Kawecka-Jaszcz, P Jankowski, T Grodzicki; Spain: J De Velasco, A Maiques; Netherlands: T van der Weijden; UK: D Wood, J Morrell.
Coordinating and Data Management Centre
The Coordinating and Data Management Centre is the Department of Cardiovascular Medicine, National Heart and Lung Institute at Charing Cross Campus, Imperial College, London, UK (Head Professor David Wood). The following staff have specific responsibilities as described: K Kotseva, Senior Clinical Research Fellow; S Connolly, Research Fellow; C Jennings, Study Nurse Coordinator; A Mead, Chief Dietician; J Jones, Superintendent Physiotherapist; A Holden, Physical activity Coordinator; T Collier, Statistician; M Alston, D Charlesworth, P Homewood, K Pandya, M Somaia, IT specialists/Data managers; S Graves, Research Administrator; W Leacock, D Xenikaki, Administrative Assistants. The following experts advised the Coordinating Centre on dietary and physical activity assessment: Professor Gary Frost, Professor Barry Margetts, Dr Mike Nelson and Dr Charlie Foster.
Central Laboratory
Central Laboratory analysis of total cholesterol, HDL cholesterol, triglycerides, glucose and HbA1c are undertaken by A McLelland, R Birrell and G Beastall in the Department of Pathological Biochemistry, Royal Infirmary, Glasgow (Head of Department J Shepherd).
Statistical centres
The statistical analyses for the primary endpoints were undertaken by D De Bacquer, Statistician, from the Department of Public Health (Head of Department G De Backer), Ghent University, Belgium, and supplementary analyses by T Collier, Statistician, Department of Medical Statistics, London School of Hygiene and Tropical Medicine, University of London, UK.
Health economics centre
Martin J Buxton, Professor of Health Economics and Director: Health Economics Research Group, Brunel University, UK; Hema Mistry and Matthew Dyer, Research Fellows in Health Economics, Brunel University.
Primary care centres
Denmark: Intervention Centre: Sundhedscenteret Skanderborg. Dr Lisbeth Rosborg, GP/Practice Manager; Susanne Holck Mogensen, Nurse.
Usual Care Centre: Gasvej 5, 8700 Horsens. Dr Henrik Zanoni, GP; Lene Henriksen, Nurse.
Italy: Intervention Centre: Rive dai Stimatinis 12, 33013 Gemona del Friuli. Dr Beppino Colle, Primary Care Intervention Coordinator; Dr Massimiliano Rugolo, Principal Investigator/GP; Tilla Gurisatti, Nurse.
Usual Care Centre: Via S. Valentino 20, 33100 Udine. Dr Mario Casini, Italy Usual Care Coordinator. Dr Fabrizio Gangi, Italy Usual Care PI/GP. Daniela Gurisatti and Loredana Trevisani, Nurses.
Netherlands: Intervention Centre: Gezondheidscentrum Hoensbroek-Noord. Dr Martijn van Nunen and Dr Bem Bruls, GPs; Jasja Janssen, Nurse; Mrs Mathil Sanders, Practice Manager.
Usual Care Centre: Dr Mieke Winten-Huisman and Dr Marc Eyck, GPs; Rene van den Heuvel and Claudia Gessing, Nurses.
Poland: Intervention Centre: Centrum Medycyny Profilaktycznej w Krakowie. Dr Krystyna Pająk, Principal Investigator; Lidia Dwojak, Practice Manager; Joanna Sładek-Ratajewicz, GP; Barbara Waligóra and Irena Smarzyńska, Nurses.
Usual Care Centre: Podstawowa Opieka Zdrowotna—Szpital Uniwersytecki w Krakowie. Dr Maria Fornal, Principal Investigator; Dr Jolanta Walczewska, GP; Barbara Wojtanis and Helena Kamińska, Nurses.
Spain: Intervention Centre: Centro de Salud Salvador Pau, Valencia. Dr Jorge Navarro, Principal Investigator; Gemma Méndez Pérez, Nurse; Dr Maria Jose Donat, Dr Raquel Prieto, Dr Rosario Gonzalez, Dr Teresa Almela, Dr Amaparo Garcia and Dr Francisco Cortes, GPs.
Usual Care Centre: Centro de Salud de Manises, Valencia. Dr Lorenzo Pascual, Principal Investigador; Rocio Marco, Nurse; Dr Juan Manuel García, Practice Manager; Dr Antonia Ibañez, Dr Cecilia Ruiz, Dr Santos Plaza, Dr Amparo Moreno and Dr Carmen Lloret, GPs.
UK: Intervention Centre: Seaside Medical Centre, Eastbourne. Dr Tim Gietzen, Principal Investigator; Sjouke Ashton, Nurse; George Bordoli, Associate Nurse; Daniel Brookbank and Angela Hughes, Practice Managers.
Usual Care Centre: Green Street Clinic, Eastbourne. Dr Ian McNaughton, Principal Investigator; Shirley Colvin, Nurse; Heather King, Practice Manager.
Footnotes
Contributors: DW and MB are part of the steering committee and approved the protocol and the design for this matched paired cluster-randomised trial. DW was responsible for the overall direction of the project. HM and MD conducted the economic analysis under the supervision of SM and MB and with guidance from DW. KK was responsible for local data collection. HM drafted the manuscript with input from all authors; all authors have approved the final manuscript and were involved in the interpretation of the results.
Funding: Sponsored solely by AstraZeneca through the provision of an unconditional educational grant. AstraZeneca had no involvement in the study design; in the collection, analysis and interpretation of the data; in the writing of the report; and in the decision to submit the paper for publication.
Competing interests: None.
Ethics approval: All countries involved in the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: There are no additional data.
References
- 1.Graham I, Atar D, Borch-Johnsen K, et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Fourth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (Constituted by representatives of nine societies and by invited experts). Eur Heart J 2007;28:2375–414 [DOI] [PubMed] [Google Scholar]
- 2.Kotseva K, Wood D, De Backer G, et al. EUROASPIRE III. Management of cardiovascular risk factors in asymptomatic high-risk patients in general practice: cross-sectional survey in 12 European countries. Eur J Cardiovasc Prev Rehabil 2010;17:530–40 [DOI] [PubMed] [Google Scholar]
- 3.Wood DA, Kotseva K, Jennings C, et al. , on behalf of the EUROACTION Study Group EUROACTION: A European Society of Cardiology demonstration project in preventive cardiology. Eur Heart J 2004;6(Supplement J):J3–J15 [Google Scholar]
- 4.Wood DA, Kotseva K, Connolly S, et al. Nurse-coordinated multidisciplinary, family-based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: a paired, cluster-randomised controlled trial. Lancet 2008;371:1999–2012 [DOI] [PubMed] [Google Scholar]
- 5.D'Agostino RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care. The Framingham Heart Study. Circulation 2008;117:743–53 [DOI] [PubMed] [Google Scholar]
- 6.Miller DK, Homan SM. Determining transition probabilities: confusion and suggestion. Med Decis Making 1994;14:52–8 [DOI] [PubMed] [Google Scholar]
- 7.Sutcliffe SJ, Fox KF, Wood DA, et al. Incidence of coronary heart disease in a health authority in London: review of a community register. BMJ 2003;326:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bamford J, Sandercock P, Dennis M, et al. A prospective study of acute cerebrovascular disease in the community: the Oxfordshire Community Stroke Project 1981–86. I. Methodology, demography and incident cases of first-ever stroke. J Neurol Neurosurg Psychiatry 1988;51:1373–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dennis MS, Bamford JM, Sandercock PA, et al. Incidence of transient ischemic attacks in Oxfordshire, England. Stroke 1989;20:333–9 [DOI] [PubMed] [Google Scholar]
- 10.Ward S, Lloyd Jones M, Pandor A, et al. A systematic review and economic evaluation of statins for the prevention of coronary events. Health Technol Assess 2007;11:1–160 [DOI] [PubMed] [Google Scholar]
- 11.Briggs A, Mihaylova B, Sculpher M, et al. Cost-effectiveness of perindopril in reducing cardiovascular events in patients with stable coronary artery disease using data from the EUROPA study. Heart 2007;93:1081–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Organisation for Economic Co-operation and Development (OECD CPI) OECD consumer price indices. July 2007. http://www.oecd.org/ (accessed 9 Sept 2012).
- 13.Kind P, Dolan P, Gudex C, et al. Variations in population health status: results from a United Kingdom national questionnaire survey. BMJ 1998;316:736–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Institute for Health and Clinical Excellence (NICE) Guide to methods of technology appraisal. London, June 2008 [PubMed] [Google Scholar]
- 15.StataCorp Stata Statistical Software: Release 10.0. College Station, TX, USA: Stata Corporation, 2007 [Google Scholar]
- 16.Ridker PM, Buring JE, Rifai N, et al. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk Score. JAMA 2007;297:611–19 [DOI] [PubMed] [Google Scholar]
- 17.Woodward M, Brindle P, Tunstall-Pedoe H. SIGN group on risk estimation. Adding social deprivation and family history to cardiovascular risk assessment: the ASSIGN score from the Scottish Heart Health Extended Cohort (SHHEC). Heart 2007;93:172–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937–52 [DOI] [PubMed] [Google Scholar]
- 19.Fleming P, Godwin M. Lifestyle interventions in primary care: systematic review of randomized controlled trials. Can Fam Physician 2008;54:1706–13 [PMC free article] [PubMed] [Google Scholar]
- 20.Imperial Cancer Research Fund OXCHECK Study Group Effectiveness of health checks conducted by nurses in primary care: final results of the OXCHECK study. BMJ 1995;310:1099–104 [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.