Abstract
Objective: This systematic review aims to assess the use and implementation of the Behavioral Model of Health Services Use developed by Ronald M. Andersen in recent studies explicity using this model.
Methods: A systematic search was conducted using PubMed in April 2011. The search strategy aimed to identify all articles in which the Andersen model had been applied and which had been published between 1998 and March 2011 in English or German. The search yielded a total of 328 articles. Two researchers independently reviewed the retrieved articles for possible inclusion using a three-step selection process (1. title/author, 2. abstract, 3. full text) with pre-defined inclusion and exclusion criteria for each step. 16 studies met all of the inclusion criteria and were used for analysis. A data extraction form was developed to collect information from articles on 17 categories including author, title, population description, aim of the study, methodological approach, use of the Andersen model, applied model version, and main results. The data collected were collated into six main categories and are presented accordingly.
Results: Andersen’s Behavioral Model (BM) has been used extensively in studies investigating the use of health services. The studies identified for this review showed that the model has been used in several areas of the health care system and in relation to very different diseases. The 1995 version of the BM was the version most frequently applied in the studies. However, the studies showed substantial differences in the variables used. The majority of the reviewed studies included age (N=15), marital status (N=13), gender/sex (N=12), education (N=11), and ethnicity (N=10) as predisposing factors and income/financial situation (N=10), health insurance (N=9), and having a usual source of care/family doctor (N=9) as enabling factors. As need factors, most of the studies included evaluated health status (N=13) and self-reported/perceived health (N=9) as well as a very wide variety of diseases. Although associations were found between the main factors examined in the studies and the utilization of health care, there was a lack of consistency in these findings. The context of the studies reviewed and the characteristics of the study populations seemed to have a strong impact on the existence, strength and direction of these associations.
Conclusions: Although the frequently used BM was explicitly employed as the theoretical background for the reviewed studies, their operationalizations of the model revealed that only a small common set of variables was used and that there were huge variations in the way these variables were categorized, especially as it concerns predisposing and enabling factors. This may stem from the secondary data sets used in the majority of the studies, which limited the variables available for study. Primary studies are urgently needed to enrich our understanding of health care utilization and the complexity of the processes shown in the BM.
Keywords: health services utilization, enabling factors, predisposing factors, need factors, Behavioral Model of Health Services Use, systematic review
Abstract
Zielsetzung: Ziel dieses systematischen Reviews ist es, einen Überblick zum Verständnis und zur Anwendung des von Ronald M. Andersen entwickelten ‚Behavioral Model of Health Services Use‘ (BM) in aktuellen empirischen Studien zu geben, die dieses Modell explizit verwendet haben.
Methoden: Im April 2011 wurde eine systematische Suche in PubMed durchgeführt. Die Suchstrategie hatte das Ziel, alle Publikationen zu identifizieren, in denen das BM in seinen unterschiedlichen Versionen zur Anwendung kam. Die Suche schloss Publikationen ein, die im Zeitraum von 1998 bis März 2011 in englischer oder deutscher Sprache veröffentlicht wurden. Insgesamt konnten 328 Artikel identifiziert werden. Das Auswahlverfahren wurde von zwei Gutachterinnen unabhängig voneinander in drei Arbeitsschritten (1. Titel/Autor, 2. Abstract, 3. Volltext) mit a priori festgelegten Einschluss- und Ausschlusskriterien durchgeführt. Für die Analyse konnten 16 Publikationen eingeschlossen werden. Die Datenextraktion dieser Publikationen erfolgte zunächst mit 17 Kategorien, die u.a. Angaben zum Autor, Titel, Studienpopulation, Studienziel, Methodologie enthielten. In einem weiteren Analyseschritt wurden diese in sechs Hauptkategorien zusammengeführt, welche primär zur Deskription der Ergebnisse genutzt werden.
Ergebnisse: Die Vielzahl der Treffer zeigt, wie weitflächig das BM im Analysezeitraum eingesetzt wurde. Die Publikationen beziehen sich dabei auf sehr unterschiedliche Bereiche des Versorgungssystems und umfassen eine Vielzahl von Erkrankungen. Es zeigte sich, dass die BM-Version, publiziert in 1995, am häufigsten verwendet wurde. Obgleich sich alle Publikationen auf das BM beziehen, findet sich in der Operationalisierung dessen eine hohe Heterogenität. Zur Erfassung der ‚predisposing factors‘ des BM wurden meist folgende Variablen verwendet: Alter (n=15), Familienstatus (n=13), Geschlecht (n=12), Schulbildung (n=11) und Ethnizität (n=10). Die am häufigsten verwendeten Variablen zur Beschreibung der ‚enabling factors‘ waren Einkommen/finanzielle Situation (n=10), Krankenversicherung (n=9) und ein „feste/r“ Hausarzt/-ärztin (n=9). Als ‚need factors‘ berücksichtigten nahezu alle Studien den allgemeinen Gesundheitsstatus (n=9) und die subjektive Einschätzung des eigenen Gesundheitszustandes (n=13) sowie eine Vielzahl unterschiedlicher Erkrankungen. Trotz der in den einzelnen Studien berichteten Zusammenhänge zwischen den einzelnen Faktoren und der Inanspruchnahme der Gesundheitsversorgung, zeigte sich in der Gesamtschau der Ergebnisse eine erhebliche Inkonsistenz. Insbesondere scheinen die den Studien zugrunde liegenden Kontextbedingungen und die unterschiedlichen Studienpopulationen einen erheblichen Einfluss auf die Existenz eines Zusammenhangs und desen Stärke und Richtung zu haben.
Schlussfolgerungen: Das BM dient zahlreichen Studien als theoretisches Analysemodell. Die damit verbundene Vorstellung einer hohen Vergleichbarkeit der Studienergebnisse wird durch die großen Unterschiede in der Operationalisierung des Modells reduziert. Zwar besteht ein gewisser „Standardkatalog“ von Variablen, der jedoch klein ist und sich durch erhebliche Unterschiede bei der Variablenkonstruktion auszeichnet. Besonders betroffen sind die ‚predisposing factors‘ und die ‚enabling factors‘. Eine Ursache könnte darin bestehen, dass die Mehrzahl der Studien Sekundärdatenanalysen und damit in der Variablenauswahl Einschränkungen unterworfen sind. Damit ist zum besseren Verständnis der im BM dargelegten Wirkungspfade die Durchführung von Primärstudien dringend geboten.
Introduction
Health care utilization is the point in health systems where patients’ needs meet the professional system. It is well known that apart from need-related factors, health care utilization is also supply-induced and thus strongly dependent on the structures of the health care system. Furthermore, many study findings have shown differences in health care utilization based on patients’ social characteristics. For instance, women tend to use outpatient health care services more often than men. In addition to the multitude of studies describing patterns of utilization in different health care settings, several scholars have developed explanatory frameworks identifying predictors of health care utilization [1]. One of the most widely acknowledged models is the Behavioral Model of Health Services Use (BM), which was developed in 1968 by the US medical sociologist and health services researcher Ronald M. Andersen [2], [3], [4], [5], [6], [7], [8], [9], [10] as a result of the third survey of the Center for Health Administration Studies and the National Opinion Research Center [5], [9].
The BM is a multilevel model that incorporates both individual and contextual determinants of health services use. In doing so, it “… divides the major components of contextual characteristics in the same way as individual characteristics have traditionally been divided—those that predispose …, enable …, or suggest need for individual use of health services” ([9], p. 652). In their most recent explication of the model, Andersen & Davidson [3] described these three major components as follows:
Predisposing factors. Individual predisposing factors include the demographic characteristics of age and sex as “biological imperatives” ([3], p. 7), social factors such as education, occupation, ethnicity and social relationships (e.g., family status), and mental factors in terms of health beliefs (e.g., attitudes, values, and knowledge related to health and health services). Contextual factors predisposing individuals to the use of health services include the demographic and social composition of communities, collective and organizational values, cultural norms and political perspectives.
Enabling factors. Financing and organizational factors are considered to serve as conditions enabling services utilization. Individual financing factors involve the income and wealth at an individual’s disposal to pay for health services and the effective price of health care which is determined by the individual’s health insurance status and cost-sharing requirements. Organizational factors entail whether an individual has a regular source of care and the nature of that source. They also include means of transportation, travel time to and waiting time for health care. At the contextual level, financing encompasses the resources available within the community for health services, such as per capita community income, affluence, the rate of health insurance coverage, the relative price of goods and services, methods of compensating providers, and health care expenditures. Organization at this level refers to the amount, varieties, locations, structures and distribution of health services facilities and personnel. It also involves physician and hospital density, office hours, provider mix, quality management oversight, and outreach and education programs. Health policies also fall into the category of contextual enabling factors.
Need factors. At the individual level, Andersen and Davidson [3] differentiate between perceived need for health services (i.e., how people view and experience their own general health, functional state and illness symptoms) and evaluated need (i.e., professional assessments and objective measurements of patients’ health status and need for medical care). At the contextual level, they make a distinction between environmental need characteristics and population health indices. Environmental need reflects the health-related conditions of the environment (e.g., occupational and traffic and crime-related injury and death rates). Population health indices are overall measures of community health, including epidemiological indicators of mortality, morbidity, and disability.
The BM has frequently been used in studies, mainly those conducted in the United States and the United Kindom. It has also been applied in numerous systematic reviews on different aspects of health care utilization to structure their results [11], [12], [13], [14], [15], [16]. In other countries, such as Germany, only recently has there been increased awareness and use of the model. In Germany, for instance, it was adopted by the Federal Health Reporting System for analyzing health services utilization within the country [17], [18].
The present systematic review was conducted to assess the results of recent studies which explicitly employed the BM as their theoretical background. The broader rationale for this review was to explore: (1) the use of different versions of the BM, (2) the application and operationalization of the BM and (3) evidence for the influencing factors specified in the BM.
Methods
A systematic review was conducted between April and July 2011. Despite minor changes, the methods used for this review follow the PRISMA Statement (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [19]. The PRISMA statement, which provides a guideline for authors when reporting systematic reviews, contains a 27-item checklist and a four-phase flow diagram specifying important topics to be included in the Abstract, Introduction, Methods and Discussion sections. The present review, which aims to provide a theoretically-based analysis of utilization in health care, was conducted as part of a larger scientific network project (“Utilization of health-related services in Germany – theoretical approaches, methods and empirical results in medical sociology,” NWIN) funded by the Deutsche Forschungsgemeinschaft (German Research Foundation, grant no.: JA 1849/1-1).
Literature search and study selection
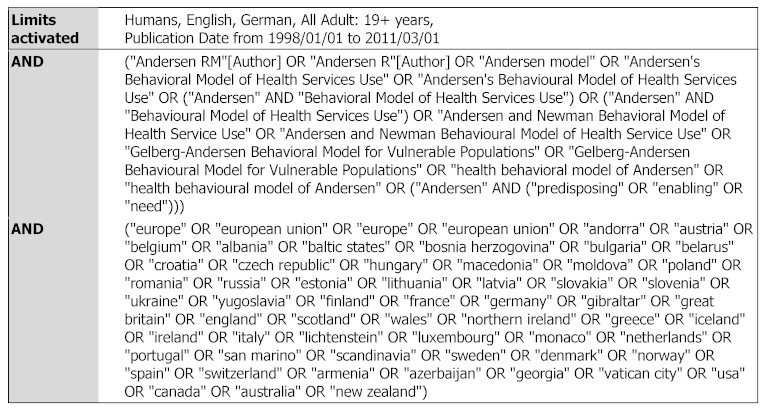
PubMed was selected as the only database for the systematic review and was searched in April 2011 (last search on April 24, 2011). The search strategy (see Table 1 (Tab. 1)) aimed to identify articles in which the Andersen model had been applied and which had been published in English or German between 1998 and March 2011. The search was limited to studies conducted with adults in Europe and Anglo-American countries (USA, Canada, Australia and New Zealand) in order to achieve comparability. To ensure that all potentially relevant articles had been identified, the search terms used included Andersen’s name as well as the terminology used in Andersen’s Behavioral Model and derived models. No limits were set as to the study design used and whether the Behavioral Model had been compared to other approaches.
Table 1. Search strategy.
Selection
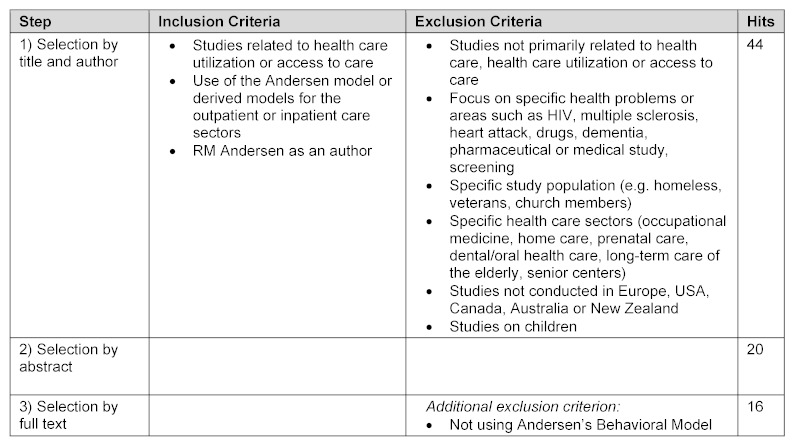
The selection of articles followed systematic review methodology and included the following steps: 1) title and author, 2) abtract and 3) full text. Inclusion and exclusion criteria were defined before each step (see Table 2 (Tab. 2)).
Table 2. Inclusion and exclusion criteria used for study selection.
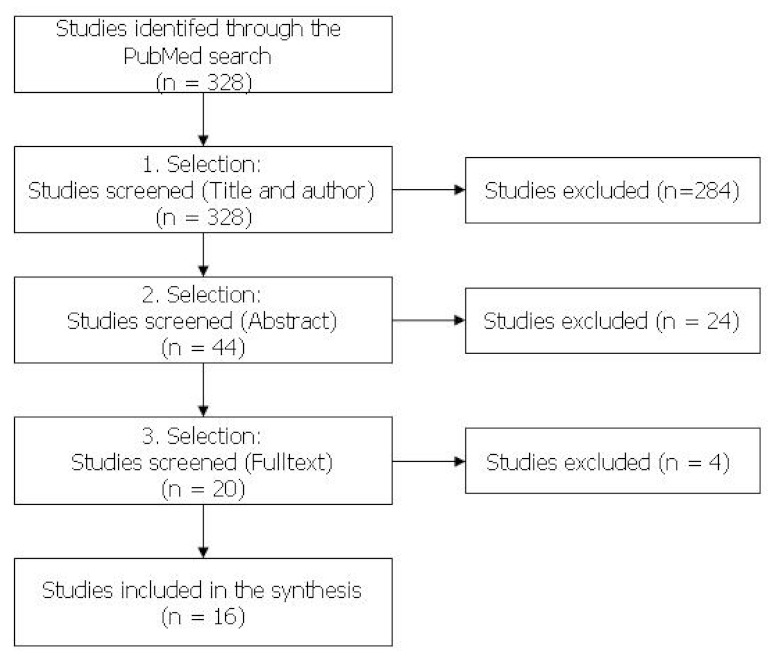
Each step of the selection process was conducted independently by two researchers (BB and DG). The results were then compared and, in cases of disagreement, discussed until a consensus was reached. Of the initial 328 studies retrieved through the PubMed search, only 16 met all of the inclusion criteria (see Figure 1 (Fig. 1)).
Figure 1. Study selection flow chart.
Data analysis
In preparation for data synthesis, a data extraction form was developed to collect information on 17 categories: author, title, publication year, country, sample size, gender, age of participants, population description (e.g., ethnicity, social background), setting (e.g., outpatient or inpatient care), aim of the study, disease of interest, data source, methodological approach, variables researched, use of the Andersen model, applied model version, and main results. All of the studies were coded independently by both researchers based on these 17 pre-defined categories. All relevant information from the studies was collated into a table. An additional quality analysis (e.g., SIGN) was not conducted.
Next, the original categories were further collated into the following six categories, which form the main basis for the presentation of the review’s results:
Study characteristics (details of the study, methodology, data source, etc.)
Sample and participants (sample size, description of the participants, etc.)
Setting
Aim of the study (general aim, disease of interest)
Use of the Andersen model (model version, applied model components)
Main results
To present quantitative data (age, sample size, etc.), ranges were chosen as summary measures. Central themes and topics (e.g., methods, aims and settings) were extracted from the studies, summarized and presented according to their frequency of occurrence in the studies. The data collected from the studies was then further categorized based on the three main factors of the Andersen model (predisposing, enabling and need factors). Thus, all relevant topics were extracted from the studies. When new topics were identified, the category system was expanded. This information was then summarized for each category.
Results
Study characteristics
The main study characteristics of the 16 studies included in this review are detailed in Table 3 (Tab. 3). The 16 studies included were published between 1999 and 2011 and were conducted in the US (n=9), Canada (n=4), US and Canada (n=1), Australia (n=1) or Germany (n=1).
Table 3. Study characteristics.
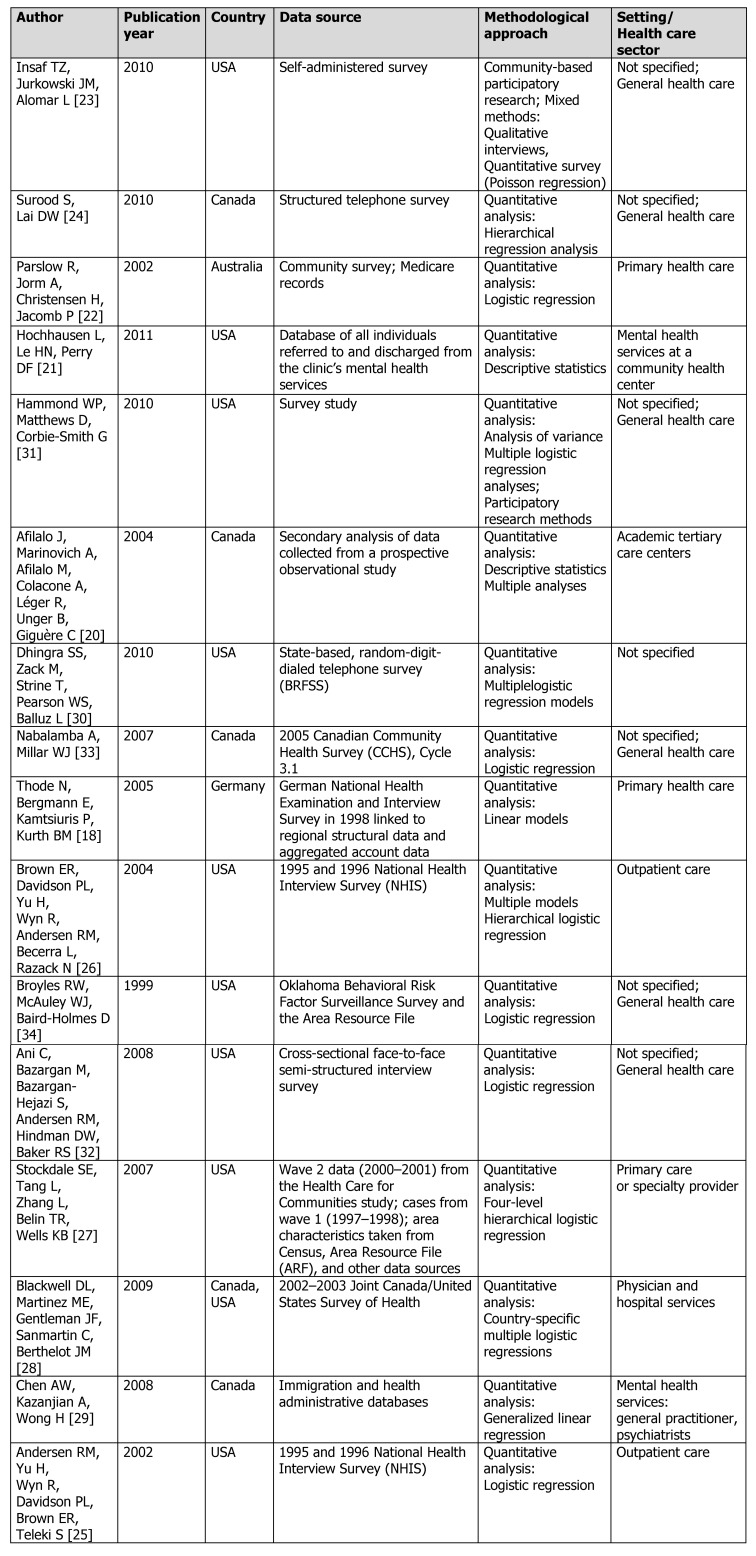
Secondary data, primarily from national surveys, were used as the sole source of information in almost all of the studies (n=14). In two studies, data were taken from hospital records [20], [21], and in the Australian study, data from Medicare records were used [22]. Primary data were only collected in three studies [22], [23], [24], one of which used focus groups in order to identify topics and develop questions for a subsequent survey [23]. The other two conducted a telephone survey [24] and a community survey [22].
All of the reviewed studies employed quantitative analysis methods. Multiple logistic regression analysis was the predominant statistical approach taken (N=13). Additionally, two studies applied linear regression models, and one study exclusively conducted a descriptive analysis. One study took a qualitative community-based participatory research (CBPR) approach with focus groups [23].
Seven studies examined health services utilization in general rather than concentrating on a specific health care sector. Two studies focused on outpatient care [25], [26], three focused on the primary care sector [18], [22], [27], one focused on physician and hospital services [28], one focused on tertiary care [20], and two focused on mental health services – in one case, services provided by a community center [21]; in the other, services by general practitioners and psychatrists [29].
Characteristics of the study populations
Sample sizes
The sample sizes of the studies varied from N=220 [24] to N=169,546 [30].
Gender
Most of the studies (N=13) included both women and men. Two studies investigated only female immigrants from Latin America [21], [23] and one study exclusively investigated African American men [31].
Age of participants
Reporting of data on participants’ age varied. Nearly half of the studies (N=6) reported mean ages ranging from 22.3 years to 65.8 years [20], [21], [24], [25], [31], [32]. Three studies reported percentages of people within defined age groups (e.g., 29% <35 years or 29% >55 years) [27], [29], [30]. Six studies reported age ranges for their participants (19–64 years, 18–79 years and 20–24 years) [18], [22], [25], [26], [28], [33]. Two studies did not report the age of their participants [23], [34].
Population description
Nearly half of the studies (N=7) included samples of the general population. In six of these studies, the participants were recruited at the household or community level; in one study, they were recruited at an emergency department [20]. Three studies focused on low- or lower-income populations [25], [26], [34]. Another three studies focused specifically on immigrants – two on Asians who immigrated to Canada [24], [29] and one on Latin American women who immigrated to the US [21]. Another three studies focused on specific ethnic groups. Two of these examined African Americans living in the US [31], [32] and one examined Latinas living in the US [23].
Use of the Andersen model
Applied model versions
Different versions of the Andersen model were found to have been used in the reviewed studies. In some studies, the authors indicated using more than one version of the model as the theoretical framework for their work. More than half of the studies [18], [20], [21], [22], [23], [26], [29], [30], [31], [33] applied the 1995 version of Andersen’s Behavioral Model [2]. The Andersen-Newman Service Utilization Model (Andersen and Newman, 1973) was used in five studies [22], [24], [29], [30], [34]. Two studies [27], [32] employed Andersen and colleagues’ Behavioral Model for Vulnerable Populations (Gelberg, Andersen, and Leake, 2000) and two studies [28], [29] applied Andersen’s Behavioral Model of Families’ Use of Health Services [5]. Two other studies [25], [29] used the Behavioral Model of Health Services Use [3], placing emphasis on contextual and community variables.
Variables researched
Table 4 (Tab. 4) gives an overview of the key variables examined in the studies. It also indicates the number of studies that applied each variable. The most frequently researched predisposing factors were age, marital status, gender/sex, education, ethnicity/nativity and employment status. The enabling factors most often studied were income/financial situation, health insurance, having a usual source of care/family doctor, and availability of medical services/inpatient and outpatient care facilities. The most frequently examined need factors were health status (mental or physical), self-reported/perceived health, diabetes, depressive symptoms, hypertension, heart disease, cancer, number of prior medical/chronic conditions, and daily activities/limitation in daily activities.
Table 4. Key variables examined by the reviewed studies.
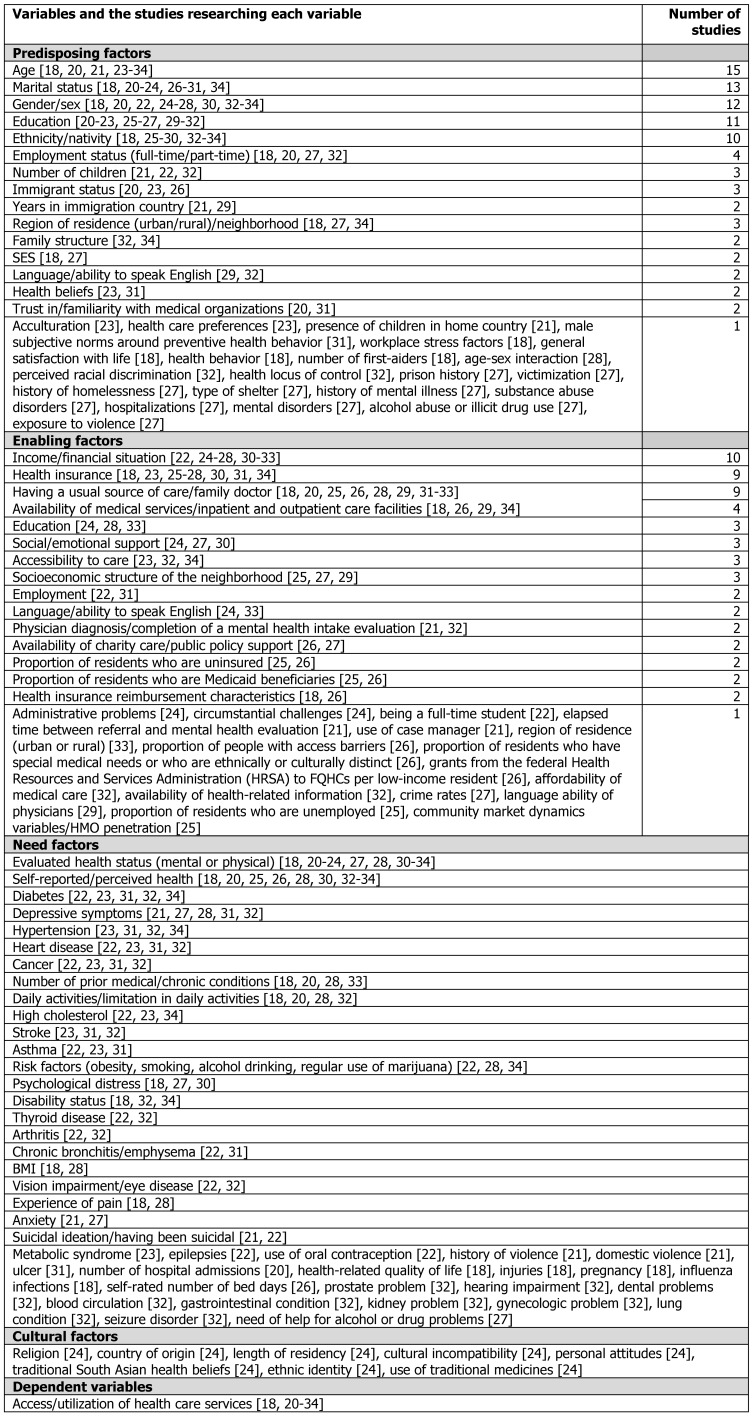
For the most part, the reviewed studies categorized variables in the same way. However, differences were found in the way some studies classified variables as predisposing and enabling variables. (Table 4 (Tab. 4) shows the variables as they were originally categorized in the reviewed studies.) In order to structure and present the review’s findings in this article, the variables were pooled and assigned to only one of the categories (predisposing, enabling or need factors) based on Andersen & Davidson’s 3 most recent explication of the model. In cases where recategorization was necessary, changes made to the original categorization have been noted.
Predisposing factors
Age
Significant associations between age and utilization of health care services were found in the majority of the studies [18], [20], [21], [24], [25], [27], [28], [29], [30], [31], [32], [33], [34]. However, the direction of this association differed substantially depending on other participant characteristics. For example, it was found that the elderly were less likely to use alcohol, drug, and mental health services (ADM) than younger people [27]. Other studies found that older residents had low odds of specialist consultations [33], but high odds of four or more consultations with general practitioners [28], [31], [33]. In a sample of African Americans and Latinos living in the US, it was found that older participants were more likely to report having obtained a physician diagnosis for their medical conditions than their younger counterparts (70% of those ≥60 years vs. 58% of those ≤30 years) [32]. In young male and female immigrants, mental health consultations with general practitioners increased substantially with age (RR per year = 1.08 and 1.10) [29], and in low-income Latina immigrants, older women were about 1.04 times as likely to use mental health services as their younger counterparts (p<.01) [21]. In Canada and the US, young women aged 18 to 44 were found to be more likely to contact a doctor than older women [28]. The same study found that women aged 45 to 64 had lower odds of being hospitalized than younger and older women and that men aged 45 to 64 had higher odds of being hospitalized than younger and older men [28].
Gender
Associations were also frequently demonstrated between gender/sex and utilization of health care services [18], [22], [25], [30], [34]. Three studies analyzing gender/sex as a single variable reported that women were more likely to visit a physician than men [22], [30], [34]. These studies included samples of young Australian adults [22], US community-dwelling respondents [30] and low-income persons in the US [34]. Another study analyzing the variables age and gender/sex in combination found that younger age (19 to 39 years) and male gender were risk factors for not visiting a physician during the previous year [25].
Ethnicity/nativity
Various studies reported associations between ethnicity or nativity and the utilization of health care services [25], [26], [27], [28], [29], [30], [33], [34]. Two studies conducted in the US found that black non-Hispanics, Hispanics, Asians or other racial ethnic groups [25], [30] and non-Hispanic others (e.g., Asians or Native Americans) [28] were significantly less likely than white non-Hispanics to receive treatment. Another US study of vulnerable subgroup members identified non-whites as having lower likelihoods of alcohol, drug, and mental health service use [27]. In Canada, visible minorities and Aboriginal people were found to be less likely to report specialist consultations than whites [33], and in the US, blacks were found to consume more physician care than other ethnic groups [34]. A sample of recent Chinese immigrants living in Canada differed in their mental health service utilization based on their geo-political origins. Whereas immigrants from Macau and Taiwan had the lowest rates of mental health visits to physicians, immigrants from mainland China and Hong Kong had higher rates (with the exception of young men from Hong Kong). The authors argue that these discrepancies may stem from ‘‘sub-cultural’’ differences among Chinese immigrants of different origins [29]. In the same sample, the length of time an immigrant had been living in Canada was associated with a significant increase in the rate of mental health visits in all sex and age groups [29].
Ethnicity, as a factor influencing health service utilization, was also looked at in combination with health insurance status. A study including a sample of lower-income adults in the US showed that among those insured, African Americans and American Indians/Alaska Natives were more likely than non-Latino whites to have a usual source of care. Furthermore, among the uninsured, having a usual source of care was more prevalent in Latinos than in non-Latino whites. However, the study found that Latinos, predominantly Mexican-origin Latinos, did worse (in terms of not having a usual source of care) in areas with a large low-income population [26].
Education
In six studies, education was significantly associated with utilization of health care services [22], [25], [28], [29], [30], [31]. One study showed that African American men in the lowest education group had the lowest odds of scheduling a routine health examination [31]; another found that, among recent Chinese immigrants in Canada, men and women with university degrees were more likely to have mental health consultations than their less educated counterparts [29]. In one study, which considered education an enabling resource, Canadian and US adults with less income and education had fewer contacts with doctors than their counterparts [28].
In a sample of low-income children and adults residing in large metropolitan statistical areas in the US, those who were Latino and Asian with less education were more likely to have less access to medical care [25]. Similarly, an Australian study found that younger adults who visited a general practitioner were more likely to be educated [22]. Contrary to these findings, however, a random telephone survey in the US observed that respondents with less than a high school education were more likely to have used health professional services for the treatment of mental or emotional problems than those with at least some college education [30].
Marital status
Marital status was repeatedly found to be associated with utilization of health care services [22], [23], [29], [30], [31], [32]. However, the direction of this association differed in the reviewed studies. One study examining routine health care services use among Latino women in the US reported that women who were not married were more likely to delay care than married women [23]. Similarly, an Australian study noted that married women were more likely to visit a general practitioner than unmarried women [22]. In a sample of African American men, those who were married were also more likely to schedule a routine health examination [31]. In the case of mental health services, it was found that persons who were previously married or never married were more likely to have received psychiatric treatment than those who were currently married [30]. A sample of recent Chinese immigrants in Canada revealed that unmarried women had lower rates of general practitioner visits for mental health problems than married women (RR=0.94 and 0.92); contrarily, single men had higher visit rates than married men (RR=1.22).
Among studies examining multifactorial influences on health services utilization, one study found that medically under-served single African-American and Latino parents and those living with a smaller family more frequently reported having received a physician diagnosis [32]. Another study observed that younger Australian women who were separated, divorced, or living with children were more likely to visit a general practitioner compared to their counterparts [22].
Cultural norms and traditional health beliefs/behavior
Cultural norms and traditional health beliefs or behavior were also identified in some studies as predisposing factors for the utilization of health care services. A community-based participatory study on Puerto Rican Latinas living in the Capital District of New York State identified women preferring to be seen by a Latino doctor (PRR 1.18) and those using alternative medicine (PRR 1.28) as being significantly more likely to delay care [23]. Traditional male role norms around the disclosure of vulnerability were found to have a negative impact on African American men's routine health examination receipt [31]. One study, which examined the impact of culture on the use of Western health services by older South Asian Canadians, found that having fewer cultural barriers and a lower level of agreement with South Asian health beliefs, but a stronger South Asian ethnic identity were related to using more types of Western health services [24]. This study originally considered cultural factors as a separate category.
Trust in/familiarity with medical organizations
Trust in and familiarity with medical organizations were also significantly associated with the use of health services. The odds of routine health examinations were lower in African American men who reported less trust in medical organizations and who believed that they should keep their concerns and emotions private [31]. Nonurgent patients who visited emergency departments without first seeking care from a primary care provider reported that they had done so because they felt more familiar with the emergency department (11%) and trusted its services (7%) [20].
Language
Only one study explicitly reported associations between language and service use. The findings from this study suggest that language alone does not predispose individuals to the use of health services. The study, which investigated mental health care use among Chinese immigrants in Canada, found, for example, that whereas men who were able to speak English were more likely to visit a general practitioner, women who could speak English had a lower rate of psychiatric visits. The authors considered various reasons for this finding, including that immigrant men may feel greater pressure to succeed in their new country. In addition, they suspect that since Chinese immigrants in British Columbia receive health care primarily from Chinese-speaking general practitioners, their English skills may be less relevant to access to health care [29].
Region of residence (urban/rural)
Region of residence was also associated with health care utilization. In one study, living in an urban area significantly increased the likelihood of residents to contact a doctor [18]. In another, residents of more rural counties or regions with fewer available health care services were less likely to visit a physician than their counterparts [34].
Community structure/social composition
Two studies reported on the influence of community structure and social composition on health care utilization. One study found that lower-income adults living in a community with a large population that depends on the health care safety net were less likely to have a usual source of care [26]. In the other study, higher socioeconomic status of the neighborhood was associated with decreased utilization rates in young males [29].
Enabling factors
Income/financial situation
Associations identified between income and service use varied in the reviewed studies. US adults with lower income had lower likelihoods of doctor contacts [28] and less access to alcohol, drug, and mental health care [27]. Another US study, however, found that persons with annual household incomes less than $50,000 were more likely to receive psychiatric treatment than those with incomes of $75,000 or higher [30], and an Australian study with young adults found that those who reported financial problems during the previous year were more likely to visit a general practitioner [22]. In under-served African American and Latino populations, less financial strain was associated with physician diagnosis rather than self-diagnosis [32].
Insurance
Several studies found that being insured significantly increased the likelihood of service use or decreased the delay of health care in different population groups [23], [25], [26], [27], [28], [30], [34]. In the US, uninsured women from Latin America were significantly more likely to delay care than their insured counterparts [23]. A study on lower-income adults living in large urban communities in the US found that health insurance status influenced the relationship between the relative size of a community’s safety-net dependent population and the access of lower-income adults [26].
Studies also found that service use varied by type of health insurance. According to one study, which investigated the influence of health sector market conditions on vulnerable subgroups’ use of alcohol, drug, and mental health services, study participants with Medicare, Medicaid, private fully managed, and private partially managed insurance had a higher likelihood of utilization in areas with higher Health Maintenance Organizations (HMO) penetration than participants with other types of insurance or no insurance plan [27]. Another study found that poor Medicaid recipients with supplemental insurance were more likely to use care than those without supplemental coverage [34].
Usual source of care
Having a usual source of care was repeatedly associated with increased service use [18], [28], [31], [34]. In a sample of African American men, those who had a usual source of care were found to be more likely to schedule and obtain a routine health examination [31]. Likewise, a study of adults in both Canada and the US showed that those who did not have a regular doctor were much less likely to have contacted a doctor over the previous year than those who did [28]. One German study even found that, contrary to the anticipated role of family doctors as gatekeepers who reduce the number of contacts with other doctors, people with a family doctor actually had more contacts with doctors overall [18].
Physician diagnosis/completion of a mental health intake evaluation
In an under-served African American and Latino population, physician diagnosis was associated with better accessibility to medical services [32]. A study of low-income Latina immigrants found that completing a mental health intake evaluation predicted service use and that women who completed evaluations were 32.13 times more likely to use services than those who did not [21]. The study also discovered that longer elapsed time between referral to mental health services and completion of the evaluation significantly predicted less use of services [21].
Case manager
The same study of low-income Latina immigrants found that using the services of a case manager significantly increased the likelihood of mental health services use. Women with case managers were 3.49 times more likely to use mental health services than those without case managers [21].
Availability of health-related information
A study of under-served African Americans and Latinos in the US found an association between physician diagnosis of medical conditions – as opposed to self-diagnosis – and a greater availability of health-related information [32].
Affordability of medical care
In the same study, affordability of medical care services was also associated with physician-based diagnosis of medical conditions [32].
Health care safety net supply
For lower-income adults living in large urban communities in the US, the extent of a community’s health care safety net, such as total Medicaid payments in the area and number of safety-net clinics, substantially influenced residents’ realized access to services [26]. The same study also indicated that lower-income residents had better access to health services in metropolitan statistical areas where the Medicaid program paid providers more. The authors considered this an important form of direct support for safety-net providers [26].
Health care market
Health care market conditions also influenced access to medical care. In one study of lower-income adults, greater competition among HMOs did not impact their access to medical care regardless of their insurance status [26]. Another study found that the existence of more federally funded community health centers and a less equal distribution of income positively influenced low-income adults’ access to medical care [25].
Emotional social support
Only one study, conducted in the US, reported associations between emotional support and use of health services. This study showed that people who always received emotional support were less likely to use health care services for the treatment of mental or emotional issues than those reporting to usually, sometimes, rarely, or never receive emotional support [30].
Need factors
Evaluated health status
Several studies reported significant associations between physical and mental status and the utilization of health services [18], [22], [23], [24], [28], [30], [33], [34]. In nearly all cases, poorer physical and mental health was a significant predictor of increased utilization. In one study, however, Canadian adults in fair or poor health were not significantly different from those in excellent health with respect to contacting a doctor [28].
In a US study of medically vulnerable population groups (the elderly, poor and uninsured), those with a history of diabetes, hypertension, or high blood cholesterol had significantly more physician visits than others [34]. Persons with more mentally and physically unhealthy days were found to be more likely to receive treatment than their counterparts [30]. Women with chronic diseases (PRR 1.24) were more likely to delay care than their counterparts [22], [23] and those using oral contraceptives were more likely to visit a general practitioner [22].
In Canadian and US adults, restriction of activity, chronic conditions, and depressive episodes had an increasing effect on doctor contacts and hospitalizations. Those who experienced any restriction of activity were more likely to use hospital and physician services. In the same sample, the likelihood of contacting a doctor was higher in persons with two or more chronic conditions (Canadian OR=3.64; US OR=3.85) compared to those with only one (Canadian OR=2.54; US OR=2.05). Additionally, Canadian and US adults who had experienced a depressive episode during the previous year were more likely to have been hospitalized than those who had not (Canadian OR=2.16; US OR=1.69) [28].
Perceived need and self-rated health
Perceived need and self-rated health were also associated with health services use in some studies [20], [30], [34]. Respondents who rated their health status as poor or fair and experienced at least one disability per day [34] and those with less than excellent self-rated health were significantly more likely to receive treatment than those with excellent self-rated health [30]. A reason given by nonurgent patients for presenting to emergency departments rather than seeking care from primary care providers was perceived need (22%). Respondents believed that their respective condition was serious enough to warrant emergency care [20].
Discussion
During the study selection process, it became apparent that the Behavioral Model had been applied to a broad range of health services sectors and diseases. Most of the initially identified studies had to be excluded as they focused on very specific health services sectors or diseases (e.g., long-term care, nursing homes, HIV, and dental care) and made drawing comparisons between studies nearly impossible. This, of course, limits the scope of the results analyzed in this systematic review. In addition, the vast majority of the studies reviewed were conducted in the US and Canada, which reduces the external validity of the review’s findings.
All of the included studies explicitly employed Andersen’s Behavioral Model as their theoretical background. Most used the 1995 version of the model, which is the fourth revision of the model initially developed in the 1960s. This model version reflects the multiple influences on health services’ use and on health status by including feedback loops that represent the mutual influence of outcome, predisposing factors, perceived need and health behavior [2]. Other model versions were also applied depending on the study subject and population (e.g., Andersen and colleagues’ Behavioral Model for Vulnerable Populations [35] and Andersen’s Behavioral Model of Families’ Use of Health Services [5]). The most recent version of the model [3] was only used in one study, which is surprising given that the 2001 version is the most detailed explication of the model, and all but one of the reviewed studies were conducted after its publication.
As evidenced by Table 4 (Tab. 4), although the studies investigated a wide variety of indicators, most of the studies focused on similar main variables, which we have labeled “key variables”. The main predisposing variables examined were age, gender/sex, education, and ethnicity, and the main enabling factors were income/financial situation, health insurance, and having a usual source of care/family doctor. It is difficult to provide an overall assessment of the need factors examined in the studies since this review specifically focused on studies that used the Andersen model and it is possible that other studies on relevant variables (e.g., specific disease states as need factors) were overlooked.
As previously mentioned, the majority of the reviewed studies conducted secondary data analyses, which means that the authors were forced to choose from among the variables collected in the original primary studies. The dominance of certain variables (i.e., key variables) may be the result of either a theoretical or a pragmatic decision.
For the most part, the researched variables were categorized identically in the reviewed studies, with only some studies differing in their classification of predisposing and enabling variables. These differing classifications suggest that certain variables play a dual role in health services use, which corresponds to the 2001 version of the Behavioral Model. For example, the socioeconomic status of a neighborhood may be seen as both a predisposing factor (e.g., in terms of supply-induced demand effects) and an enabling factor due to its association with individual and community income. Also, age and sex may be categorized as individual demographic predisposing factors and, at the same time, used as proxies of need factors due to their associations with morbidity [29].
As evidenced by the findings presented in the Results section, it is nearly impossible to identify the factor having the “strongest influence” on health services utilization. Even for age, a seemingly simple indicator of service utilization, the findings showed inconsistencies in the strength and direction of this association. Since none of the studies used complex statistical methods, such as the testing of multivariate models, it is impossible to adequately assess the correlations between the examined variables. Therefore, the explanatory power of the results is restricted and is often limited to single indicators. The complexity of the Behavioral Model has clearly not been conveyed in the production and presentation of these results.
There is a strong of need for (internationally conducted) primary studies that apply the Behavioral Model, that adequately operationalize the complexity of the model and that use complex statistical analysis that reflects its complexity (e.g., path analysis). Such studies would make it possible to go beyond examinations and descriptions of individual indicators and to better understand the associations between the main factors (predisposing, enabling, need) and investigate feedback loops.
Notes
Acknowledgements
The writing of this article was carried out as part of the scientific network project “Utilization of health-related services in Germany – theoretical approaches, methods and empirical results in medical sociology” (NWIN). The project is funded by the Deutsche Forschungsgemeinschaft (German Research Foundation, grant no.: JA 1849/1-1).
Competing interests
The authors declare that they have no competing interests.
References
- 1.Ricketts TC, Goldsmith LJ. Access in health services research: the battle of the frameworks. Nurs Outlook. 2005 Nov-Dec;53(6):274–280. doi: 10.1016/j.outlook.2005.06.007. Available from: http://dx.doi.org/10.1016/j.outlook.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 2.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995 Mar;36(1):1–10. doi: 10.2307/2137284. Available from: http://dx.doi.org/10.2307/2137284. [DOI] [PubMed] [Google Scholar]
- 3.Andersen RM, Davidson PL. Improving access to care in America: individual and contextual indicators. In: Andersen RM, Rice TH, Kominski EF, editors. Changing the U.S. health care system: key issues in health services, policy, and management. San Francisco, CA: Jossey-Bass; 2001. pp. 3–30. [Google Scholar]
- 4.Bradley EH, McGraw SA, Curry L, Buckser A, King KL, Kasl SV, Andersen R. Expanding the Andersen model: the role of psychosocial factors in long-term care use. Health Serv Res. 2002 Oct;37(5):1221–1242. doi: 10.1111/1475-6773.01053. Available from: http://dx.doi.org/10.1111/1475-6773.01053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andersen RM. Families' use of health services: a behavioral model of predisposing, enabling and need components [dissertation] West Lafayette, In: Purdue University; 1968. Available from: http://docs.lib.purdue.edu/dissertations/AAI6902884/ [Google Scholar]
- 6.Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc. 1973;51(1):95–124. doi: 10.2307/3349613. Available from: http://dx.doi.org/10.2307/3349613. [DOI] [PubMed] [Google Scholar]
- 7.Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9(3):208–220. [PMC free article] [PubMed] [Google Scholar]
- 8.Aday LA, Andersen RM, Fleming GV. Health care in the U.S.: equitable for whom? Beverly Hills, CA: Sage; 1980. [Google Scholar]
- 9.Andersen RM. National health surveys and the behavioral model of health services use. Med Care. 2008 Jul;46(7):647–653. doi: 10.1097/MLR.0b013e31817a835d. Available from: http://dx.doi.org/10.1097/MLR.0b013e31817a835d. [DOI] [PubMed] [Google Scholar]
- 10.Davidson PL, Andersen RM, Wyn R, Brown ER. A framework for evaluating safety-net and other community-level factors on access for low-income populations. Inquiry. 2004;41(1):21–38. doi: 10.5034/inquiryjrnl_41.1.21. Available from: http://dx.doi.org/10.5034/inquiryjrnl_41.1.21. [DOI] [PubMed] [Google Scholar]
- 11.Hulka BS, Wheat JR. Patterns of utilization. The patient perspective. Med Care. 1985 May;23(5):438–460. doi: 10.1097/00005650-198505000-00009. Available from: http://dx.doi.org/10.1097/00005650-198505000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Padgett DK, Brodsky B. Psychosocial factors influencing non-urgent use of the emergency room: a review of the literature and recommendations for research and improved service delivery. Soc Sci Med. 1992 Nov;35(9):1189–1197. doi: 10.1016/0277-9536(92)90231-E. Available from: http://dx.doi.org/10.1016/0277-9536(92)90231-E. [DOI] [PubMed] [Google Scholar]
- 13.de Boer AG, Wijker W, de Haes HC. Predictors of health care utilization in the chronically ill: a review of the literature. Health Policy. 1997 Nov;42(2):101–115. doi: 10.1016/S0168-8510(97)00062-6. Available from: http://dx.doi.org/10.1016/S0168-8510(97)00062-6. [DOI] [PubMed] [Google Scholar]
- 14.Phillips KA, Morrison KR, Andersen R, Aday LA. Understanding the context of healthcare utilization: assessing environmental and provider-related variables in the behavioral model of utilization. Health Serv Res. 1998 Aug;33(3 Pt 1):571–596. [PMC free article] [PubMed] [Google Scholar]
- 15.McCusker J, Karp I, Cardin S, Durand P, Morin J. Determinants of emergency department visits by older adults: a systematic review. Acad Emerg Med. 2003 Dec;10(12):1362–1370. doi: 10.1111/j.1553-2712.2003.tb00011.x. Available from: http://dx.doi.org/10.1111/j.1553-2712.2003.tb00011.x. [DOI] [PubMed] [Google Scholar]
- 16.Kadushin G. Home health care utilization: a review of the research for social work. Health Soc Work. 2004 Aug;29(3):219–244. doi: 10.1093/hsw/29.3.219. Available from: http://dx.doi.org/10.1093/hsw/29.3.219. [DOI] [PubMed] [Google Scholar]
- 17.Thode N, Bergmann E, Kamtsiuris P, Kurth BM. Einflussfaktoren auf die Inanspruchnahme des deutschen Gesundheitswesens und mögliche Steuerungsmechanismen. Berlin: Robert Koch Institut; 2004. Available from: http://www.rki.de/EN/Content/Health_Monitoring/Projects/Inanspruchnahmen/predictors_for_ambulatory_medical_care_utilization_in_germany.pdf. [Google Scholar]
- 18.Thode N, Bergmann E, Kamtsiuris P, Kurth BM. Einflussfaktoren auf die ambulante Inanspruchnahme in Deutschland. [Predictors for ambulatory medical care utilization in Germany]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2005 Mar;48(3):296–306. doi: 10.1007/s00103-004-1004-3. (Ger). Available from: http://dx.doi.org/10.1007/s00103-004-1004-3. [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009 Jul 21;339:b2535. doi: 10.1136/bmj.b2535. Available from: http://dx.doi.org/10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Afilalo J, Marinovich A, Afilalo M, Colacone A, Léger R, Unger B, Giguère C. Nonurgent emergency department patient characteristics and barriers to primary care. Acad Emerg Med. 2004 Dec;11(12):1302–1310. doi: 10.1197/j.aem.2004.08.032. Available from: http://dx.doi.org/10.1197/j.aem.2004.08.032. [DOI] [PubMed] [Google Scholar]
- 21.Hochhausen L, Le HN, Perry DF. Community-based mental health service utilization among low-income Latina immigrants. Community Ment Health J. 2011 Feb;47(1):14–23. doi: 10.1007/s10597-009-9253-0. Available from: http://dx.doi.org/10.1007/s10597-009-9253-0. [DOI] [PubMed] [Google Scholar]
- 22.Parslow R, Jorm A, Christensen H, Jacomb P. Factors associated with young adults' obtaining general practitioner services. Aust Health Rev. 2002;25(6):109–118. doi: 10.1071/AH020109a. Available from: http://dx.doi.org/10.1071/AH020109a. [DOI] [PubMed] [Google Scholar]
- 23.Insaf TZ, Jurkowski JM, Alomar L. Sociocultural factors influencing delay in seeking routine health care among Latinas: a community-based participatory research study. Ethn Dis. 2010;20(2):148–154. [PubMed] [Google Scholar]
- 24.Surood S, Lai DW. Impact of culture on use of Western health services by older South Asian Canadians. Can J Public Health. 2010 Mar-Apr;101(2):176–180. doi: 10.1007/BF03404367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Andersen RM, Yu H, Wyn R, Davidson PL, Brown ER, Teleki S. Access to medical care for low-income persons: how do communities make a difference? Med Care Res Rev. 2002 Dec;59(4):384–411. doi: 10.1177/107755802237808. Available from: http://dx.doi.org/10.1177/107755802237808. [DOI] [PubMed] [Google Scholar]
- 26.Brown ER, Davidson PL, Yu H, Wyn R, Andersen RM, Becerra L, Razack N. Effects of community factors on access to ambulatory care for lower-income adults in large urban communities. Inquiry. 2004;41(1):39–56. doi: 10.5034/inquiryjrnl_41.1.39. Available from: http://dx.doi.org/10.5034/inquiryjrnl_41.1.39. [DOI] [PubMed] [Google Scholar]
- 27.Stockdale SE, Tang L, Zhang L, Belin TR, Wells KB. The effects of health sector market factors and vulnerable group membership on access to alcohol, drug, and mental health care. Health Serv Res. 2007 Jun;42(3 Pt 1):1020–1041. doi: 10.1111/j.1475-6773.2006.00636.x. Available from: http://dx.doi.org/10.1111/j.1475-6773.2006.00636.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blackwell DL, Martinez ME, Gentleman JF, Sanmartin C, Berthelot JM. Socioeconomic status and utilization of health care services in Canada and the United States: findings from a binational health survey. Med Care. 2009 Nov;47(11):1136–1146. doi: 10.1097/MLR.0b013e3181adcbe9. Available from: http://dx.doi.org/10.1097/MLR.0b013e3181adcbe9. [DOI] [PubMed] [Google Scholar]
- 29.Chen AW, Kazanjian A, Wong H. Determinants of mental health consultations among recent Chinese immigrants in British Columbia, Canada: implications for mental health risk and access to services. J Immigr Minor Health. 2008 Dec;10(6):529–540. doi: 10.1007/s10903-008-9143-5. Available from: http://dx.doi.org/10.1007/s10903-008-9143-5. [DOI] [PubMed] [Google Scholar]
- 30.Dhingra SS, Zack M, Strine T, Pearson WS, Balluz L. Determining prevalence and correlates of psychiatric treatment with Andersen's behavioral model of health services use. Psychiatr Serv. 2010 May;61(5):524–528. doi: 10.1176/appi.ps.61.5.524. Available from: http://dx.doi.org/10.1176/appi.ps.61.5.524. [DOI] [PubMed] [Google Scholar]
- 31.Hammond WP, Matthews D, Corbie-Smith G. Psychosocial factors associated with routine health examination scheduling and receipt among African American men. J Natl Med Assoc. 2010 Apr;102(4):276–289. doi: 10.1016/s0027-9684(15)30600-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ani C, Bazargan M, Bazargan-Hejazi S, Andersen RM, Hindman DW, Baker RS. Correlates of self-diagnosis of chronic medical and mental health conditions in under-served African American and Latino populations. Ethn Dis. 2008;18(2 Suppl 2):S2–105. [PubMed] [Google Scholar]
- 33.Nabalamba A, Millar WJ. Going to the doctor. Health Rep. 2007 Feb;18(1):23–35. [PubMed] [Google Scholar]
- 34.Broyles RW, McAuley WJ, Baird-Holmes D. The medically vulnerable: their health risks, health status, and use of physician care. J Health Care Poor Underserved. 1999 May;10(2):186–200. doi: 10.1353/hpu.2010.0498. Available from: http://dx.doi.org/10.1353/hpu.2010.0498. [DOI] [PubMed] [Google Scholar]
- 35.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000 Feb;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]