Abstract
Background
Allergy is associated with considerable morbidity.
Objective
The aim of this multicenter study was to provide insight into allergy knowledge and perceptions among the population.
Methods
During the World Allergy Day, several allergy clinics conducted public meetings to encourage the awareness of and education in allergy. At the beginning, participants filled out a questionnaire to assess their knowledge about what is allergy and to determine by whom those symptoms are cared.
Results
A total of 256 participants (187 women/69 men, mean age, 31.2 ± 12.5 years) completed the survey. Of the 202 participants with symptoms, 58.9% had physician-diagnosed allergic disease. Among the 19 symptoms evaluated, 56.5% of the symptoms were recognized as related with allergy, and this increased in compliance with education level (r = +0.427; P < 0.001) but not with diagnosed allergy (P = 0.34). Sneezing was the most common symptom thought to be related with allergy-related symptom (77.5%), whereas loss of smell was the least one (37.9%). Participants were more likely to be cared by an allergologist (72.9%) followed by other specialties, when experiencing allergy.
Conclusions
Increasing the awareness for allergic symptoms is the key not only for the diagnosis but also for the optimal treatment. Therefore, education is an important component of prevention and control of allergic diseases.
Key Words: allergy, asthma, awareness, diagnosis, symptom, treatment
Allergy is a growing health problem that greatly impacts the day-to-day life of patients, as well as their families, school, professional, and social life. It is estimated that more than 20% of the worlds's population experiences from IgE-mediated allergic diseases. Despite its high prevalence, allergy is usually underestimated, underdiagnosed, and undertreated, as well. This could mask an appropriate assessment of the extent of allergy-related problems and subsequently hamper appropriate action as the allergic patient may be less inclined to stand out.1–3 Studies of randomly selected populations indicate that up to more than one-third of patients who experience symptoms of rhinitis and asthma are undiagnosed and have decreased quality of life.4–6
Allergy affects all age groups, from infancy to childhood, from adolescent to adulthood up to the elderly. The continuum of the disease or “allergic march” is a challenge for health care systems.7 Moreover, patients often need assistance in understanding their condition and encouragement to comply with the recommendations to see the improvement in their quality of life.8 Research within allergy is intense, and studies addressing the aspects of immunology, symptoms, and treatment are reported continually. But the knowledge of the allergy patient's perception of own disease and of its consequences is still scarce.9 This causes requirement of a range of measures like public information, patient education, health promotion, and guidelines. With such initiatives, early diagnosis and optimal treatment are expected.
The aim of this multicenter study was to assess the knowledge among a heterogenous population of Turkey about what is allergy and what is not and to determine by whom those symptoms are cared.
METHODS
During the World Allergy Day in December 9, 2009, group meetings were conducted at 9 centers located in 6 cities throughout Turkey. These 9 institutions were all, but one, university hospitals. Each group consisted of 16 to 50 individuals, who were mainly urban dwellers (Fig. 1). All the participants were recruited via outpatient clinics, postings in the communities, and word of mouth. Therefore, groups included not only subjects who had either a self-reported or physician-diagnosed allergic diseases and who were caretakers of a household member with allergy but also anyone regardless of allergy diagnosis.
FIGURE 1.
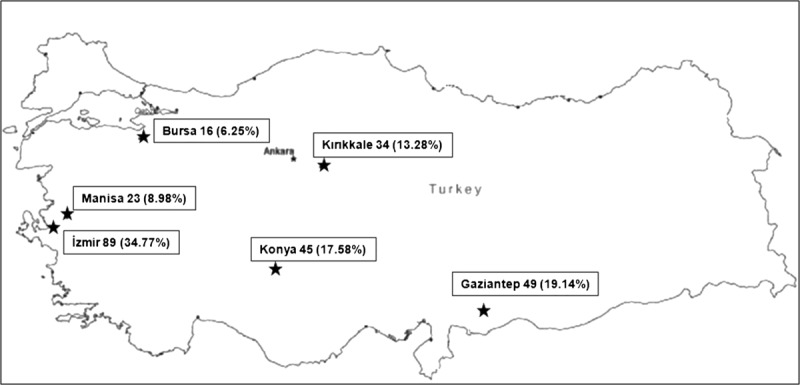
Distribution of the participants.
Detailed information was collected including age, gender, occupation, level of education, the presence of allergic symptoms, and skin prick tests done. Education level was classified as uneducated, elementary school (5–8 years), high school (11 years), and university, and/or master degree (≥15 years), according to the standards of the country. Participants gave written informed consent before the meetings.
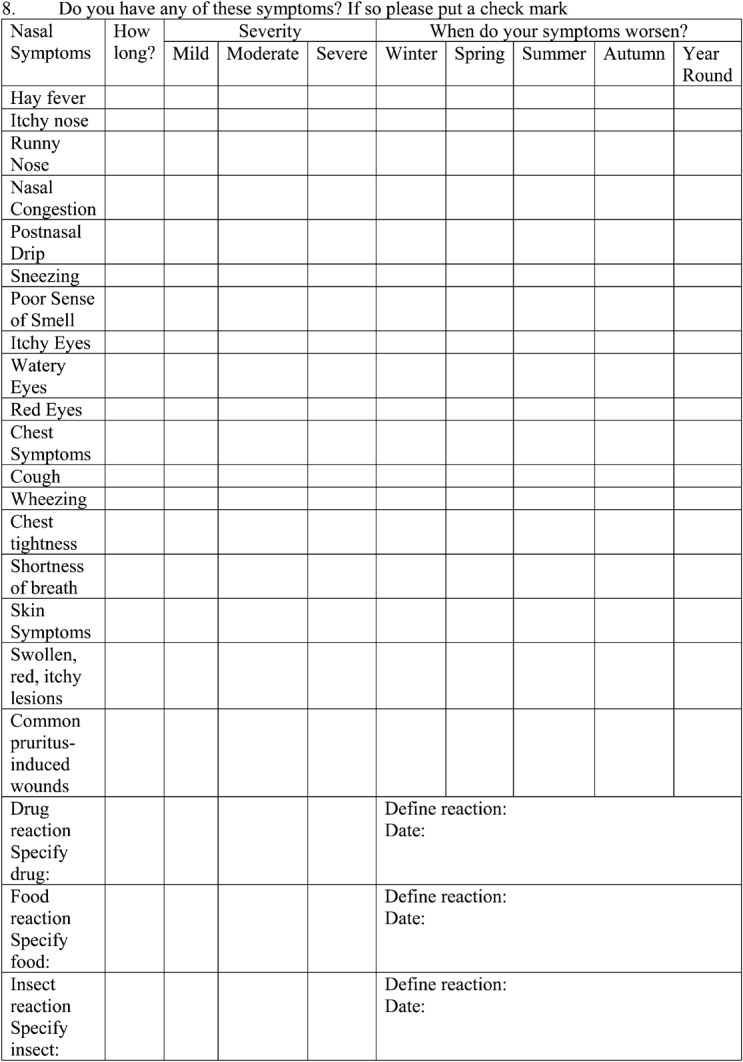
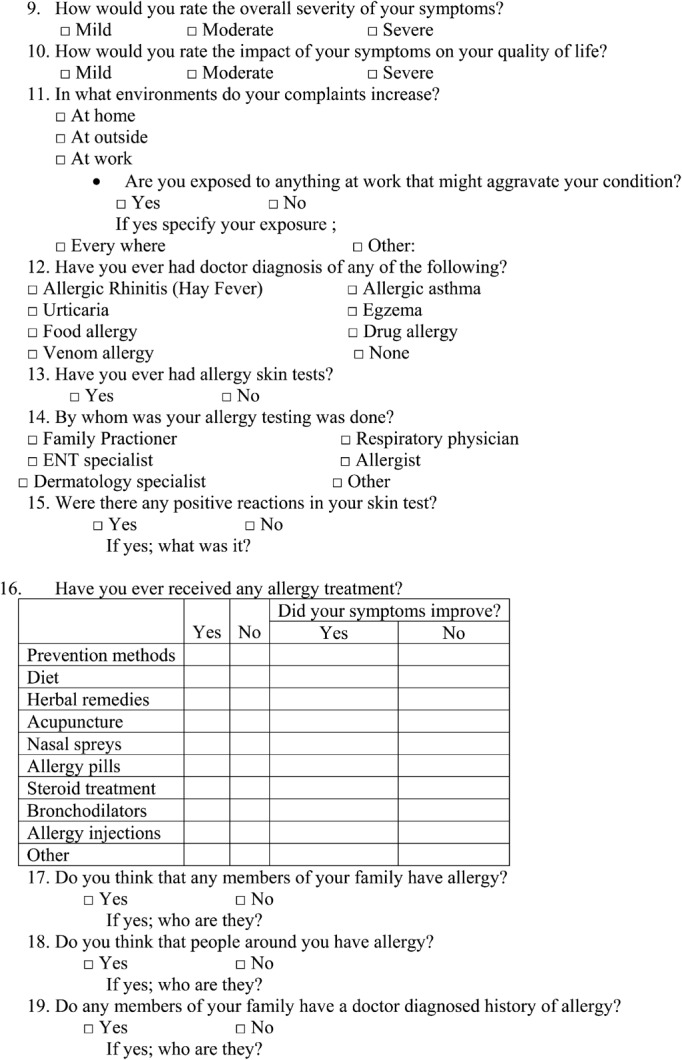
Before the beginning of the session, participants were asked to fill out a self-administered questionnaire that consisted of 19 multiple-choice questions, related to allergic symptoms and the possible specialties that could be an option in the management of allergy (Appendix). This was used to obtain information about perception on allergy and the ways of coping. Thereafter, semistructured educational sessions were given by allergy specialists using verbal and visual fragments, including information on allergic diseases and asthma, management, and avoidance of triggers interactively. The sessions lasted around half a day.
Statistical Analysis
The data were analyzed with the statistical package SPSS 17.0 (SPSS, Inc, Chicago, IL) for Windows. Frequencies were calculated for the entire group by descriptive statistics. Student t test was used to ascertain the significance of differences between mean values of 2 continuous variables. Pearson correlation test was used for investigating the relationship between 2 quantitative continuous variables. The level P < 0.05 was considered as the cutoff value for significance.
RESULTS
Of the 266 returned questionnaires, a few were excluded from the analysis because either their descriptive characteristics were missing (3) or the questionnaire was not fully completed (7). Therefore, 256 participants were included in the final analysis. Participants' age ranged from 12 to 83 years (mean ± SD, 31.2±12.5 years) with no significant difference between the genders (P = 0.6). The majority (73%) of subjects were female. Characteristics of the study group are shown in Table 1. Almost one-third comprised housewifes, and 29.4% comprised students. More than half (57.3%) of the subjects had received more than 8 years of education, and 40.3% had elementary school education only.
TABLE 1.
Characteristics of the Participants
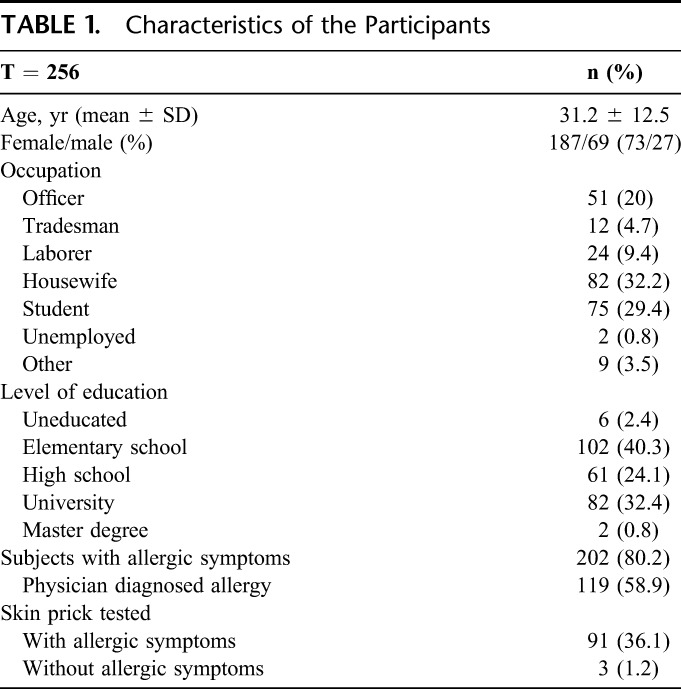
Of the 202 subjects with allergic symptoms, 45.1% was skin tested and 58.9% was diagnosed as “allergic” by a health care professional. On the other hand, 5.6% of subjects with no allergic symptoms were reported to be skin tested. Although complaints regarding allergy was found to be increased with decreased education, no significant correlation was found between physician-diagnosed allergy and education level in patients with symptoms.
Among the 19 symptoms evaluated, 56.5% were marked as related to allergy, with a significant difference between the genders (women 60.5% vs. men 49.2%; P = 0.02). Nasal and skin complaints were more prominently identified as the symptoms of allergy. Sneezing was the leading symptom (77.5%), whereas loss of smell (37.9%) was the least one related to allergic conditions (Table 2). Mean of the total symptom count was 11 for the participants with physician-diagnosed allergy, whereas it was 10 for those with no complaints, showing no significant difference (P = 0.3). Recognition of allergic symptoms was evaluated in those with the same relevant symptoms and those without. As almost all the participants pointed out at least one nasal and/or chest symptom related with allergy, there was no significant difference. Only the symptoms related with skin, as well as drug and insect reactions, were found to be significantly recognized as allergic in subjects with symptoms compared with those without symptoms (Fig. 2).
TABLE 2.
Participants' Assessment of Relationship of Various Symptoms With Allergy
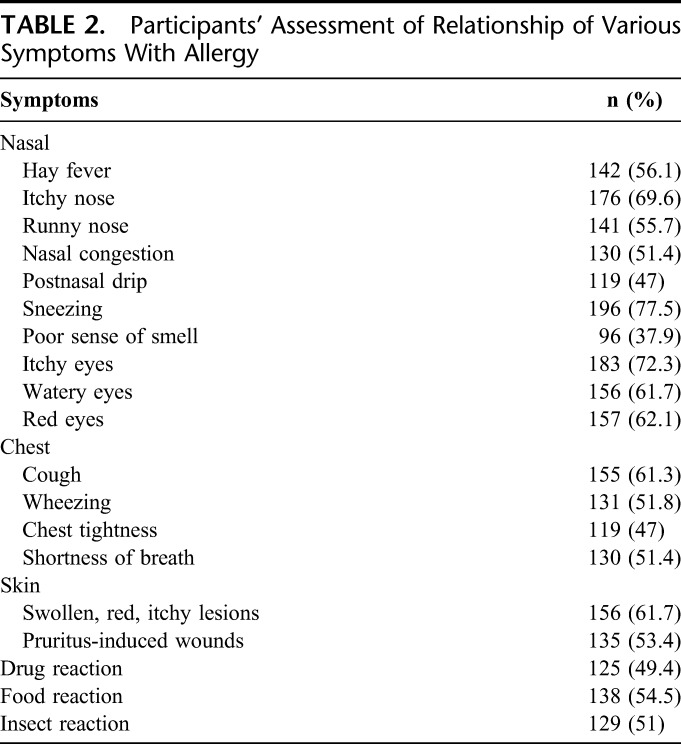
FIGURE 2.
Allergic symptom recognition of the participants according to the presence of the relevant symptom (values given as percentages). Only the P values with significant importance are given.
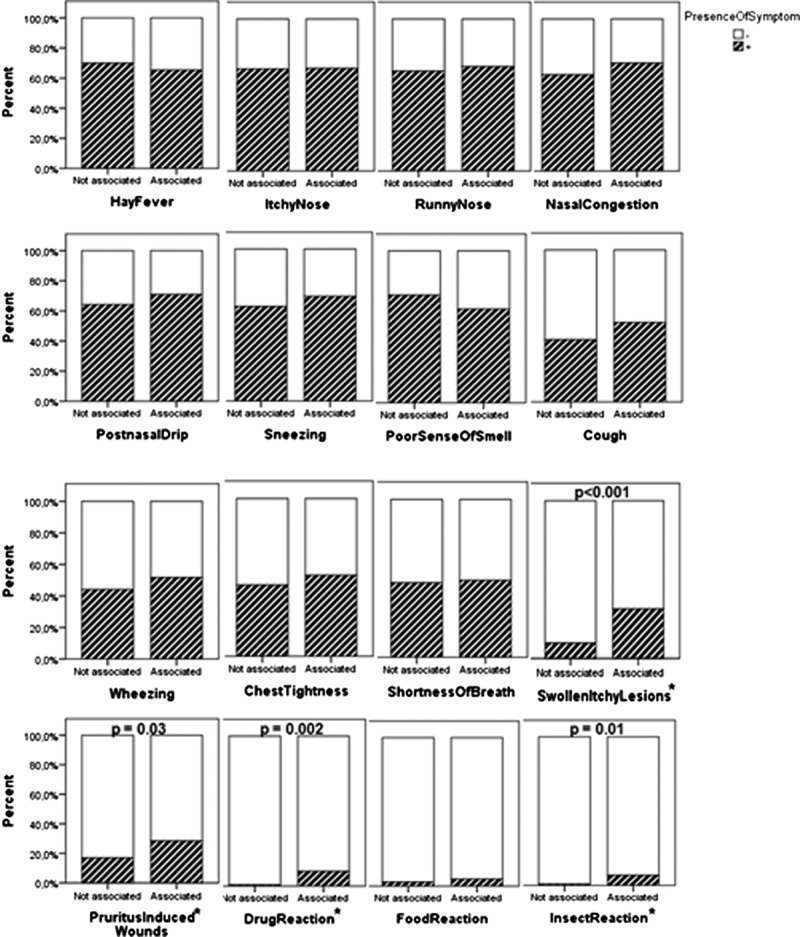
Participants with the physician-diagnosed allergic rhinitis recognized hay fever (P = 0.02), runny nose (P = 0.005), nasal congestion (P = 0.006), and postnasal drip (P = 0.048) as possibly allergic symptoms significantly more than the other participants, whereas there was no significant difference between these 2 groups in recognition of sneezing (P = 0.2), itchy nose (P = 0.15), and poor sense of smell (P = 0.7). Also, participants with the physician-diagnosed asthma recognized cough (P = 0.045) and wheezing (P = 0.025), but not shortness of breath (P = 0.15) and chest tightness (P = 0.1), as possibly allergic symptoms significantly more than the other participants. Moreover, participants with the physician-diagnosed skin allergy, as well as drug, food or insect allergy, significantly (P < 0.001) recognized symptoms/reactions as possibly allergic more than the other participants. A significant education-related awareness was observed in the recognition of symptoms (r = 0.427; P < 0.001). In the presence of symptoms, almost 3 quarters of the participants stated that allergy should be cared by an allergologist, followed by other specialties, that is, pulmonologist, dermatologist, ear-nose and throat specialist, family practitioner, and ophthalmologist (Fig. 3). Among the 19 symptoms evaluated, the more the number of symptoms recognized as possibly allergic, the more they chose to see an allergist (P < 0.001).
FIGURE 3.
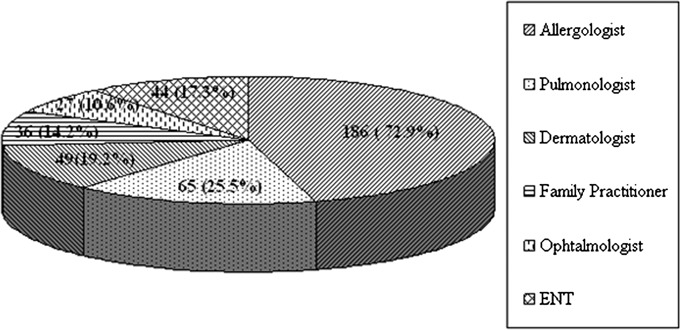
Preference of specialties in the management of allergic symptoms.
DISCUSSIONS
This multicenter study has shown that awareness of allergy was usually underestimated among the population, as approximately half of the allergic symptoms were recognized. Although our results cannot be generalized due to relatively small size and biased toward women and nonprofessionals, the awareness in this group of participants increased significantly in compliance with the education level but not with the diagnosed allergy. Mainly, the nasal and skin symptoms were evaluated as “allergic,” probably because that they are the most common sites of allergic diseases. However, the symptoms related with nasal and/or chest were not found to be significantly recognized more as allergic in subjects with symptoms compared with the ones without symptoms. These results showed us the degree of ignorance about the subjects' own possibly allergic symptoms.
Despite the intense research worldwide within allergy, the allergic patient's knowledge and perception of their own condition is scarce. In the United States, the knowledge was found to be poor, and the respondents tended to minimize the stigma associated with food allergy.10 In this present survey, the allergic patients' perception of their own disease was found to be inadequate, in consistent with the literature. Education seems an essential part of treatment and disease control. Therefore, it may be recommended not only to raise public awareness to promote a greater understanding but also to educate and support the health care needs of individuals with allergy. Health care professionals—taking into consideration the patient's attitudes, beliefs, expectations, and their needs—must ensure that their patients understand the nature of the disease. Patients must be informed correctly about their disease, its causes, treatment, and capabilities of prevention and environmental control.
Knowledge and health seeking behavior for allergy diseases are thought to be different in various communities. In a study performed by de Monchy,9 knowledge of allergy patients' perception of their own disease was examined by telephone-based survey techniques in 10 European countries. They included both patients with an objective medical diagnosis and those without, as was done in our study. According to that study, a clear inverse age relation to respiratory allergy was seen and this was influenced by gender, that is, more prevalent in younger men and older women.11 Although, women significantly evaluated the symptoms better compared with men, their results disclosed that the perceived restrictions on and problems of persons with allergy are very similar irrespective of nationality, the specific allergy, and the allergic disease. They reported that family, physicians, and the society underestimate and disregard the consequences of atopic diseases.9,11
In our study, group meetings were used for obtaining general information about the topic, as well as to elicit popular knowledge and concerns about allergy. Trainers from each center facilitated the meetings. In general, many participants mentioned that allergy was not accepted as a real disease (personal communications, AF Kalpaklioglu and Ilkay Koca, 2009). Furthermore, many subjects with allergy (or who cared for a household member with allergy) revealed uncertainties about the nature and management of this chronic condition. Recent studies showed that a critical need for more information about allergy and allergic diseases and that this requirement is present but unmet by health care systems and patient organizations. Conversely, it was reported that the professional advice was perceived to be of little or even of no value.9 This may be one of the reasons why our participants, irrespective of diagnosed allergy, showed no difference in recognizing allergic symptoms.
Despite the availability of effective treatments, factors such as individual beliefs, attitudes, behavior, and inadequate patient-clinician communication may contribute to poor adherence to treatment, especially in chronic diseases such as asthma and allergy.12 It has been previously suggested that cultural factors have an impact on the manner in which patients and families explain asthma.13 The high prevalence of perceived allergy disorders at household level in Tanzania was shown to be associated with poor understanding on the possible causes and preventive measures.14 Therefore, it is increasingly recognized that health care professionals must understand the different beliefs of their patients to improve both communication and adherence to treatment.15 Recently, van Dellen et al16 have shown on their first published data in Europe that beliefs about asthma and its treatment can be addressed during patient–clinician interactions. Community-based, group-health education workshops were shown to have significant complementary value for patients who are dissatisfied with conventional asthma education.17 However, continuous education is needed as a limited asthma education programme in a hospital setting was shown to have a significant but short-lived improvements on patients’ asthma.18
A study among Californian adults with asthma found that 13% of those who have not completed high school reported problems understanding their doctors, compared with 6% of high school graduates and only 2 to 3% of those with at least some college. Those with less education are more likely to experience low health literacy, which relates to a person's ability to understand and act on health related information.19 In agreement with these findings, our present study showed a significant education-related awareness in the recognition of symptoms. This is an important outcome because it proves that every patient should be evaluated by her/his realities, to reduce disparities. Development and dissemination of linguistically and culturally appropriate allergy education programs and materials with tailoring of allergy education interventions to individual literacy levels should be encouraged. We believe that along with the results of our study, personalized patient education and tailor-made treatment seems to be a key step in allergy management.
As there are lots of misconceptions on the nature, impact and seriousness of allergic diseases, and their care and prevention, the European Federation of Allergy and Airways Diseases Patients Association has drawn up a manifesto comprising a 6-point strategy to counteract the growing prevalence of allergic disease both in Europe and globally.20 This kind of network will facilitate collaborations and create a valuable platform for sharing of knowledge and experiences.
We have shown that female participants significantly evaluated the symptoms better than male participants. Actually, this finding is consistent with previous research, which suggests that female patients because of greater selective attention to their bodies and an increased attribution of bodily sensations to physical illness have historically perceived an excess of symptoms compared with male patients, even when both sexes are healthy.21 But there was no difference in the recognition of symptoms between the groups with or without allergic symptoms (P < 0.3), proving that there is a significant lack of awareness in recognizing allergy diseases.
In the present group of subjects with allergic symptoms, although 58.9% had a physician-diagnosed allergic disease, only 45.1% of them declared to be skin tested. This result stresses the necessity of an intense effort to raise allergy awareness among health care professionals. Similarly, Stingone and Claudio22 found that only 54.9% of asthmatic children with an allergy diagnosis reported allergy testing in New York City. In a study concerning the pediatricians' attitudes toward allergy, in 1971, 75% of the pediatricians felt that the specialty of allergy had great importance compared with 99% after 27 years. Although the value of skin testing had increased, only 36% felt it had great value. The authors concluded that allergists must be more aggressive in developing the knowledge, attitudes, and practices of physicians relative to the field of allergy. Despite the fact that the value of skin testing had increased, only 36% felt it had great value. The authors concluded that allergists must be more aggressive in developing the knowledge, attitudes, and practices of physicians relative to the field of allergy.23
There is no comprehensive information available concerning how care is provided for allergic patients. A questionnaire survey was conducted in 33 institutions in 26 European countries to determine who cares for those with asthma, allergic dermatitis, and rhinitis.24 Although a wide difference in the use of various health care professionals for allergic symptoms was reported in different countries, our patients with allergic conditions seem to prefer a specialized management in correlation with the increased number of symptoms recognized; almost 3 quarters stated that allergy should be cared by an allergologist. It is important to note that the specialties chosen were preferences of the patients, not whom they had seen. Unfortunately, there is no an allergy patient organization in Turkey. Nonetheless, as in some European countries, both allergy specialists and allergy centers are very few in Turkey.
There is much greater awareness of guidelines for asthma and much less usage of guidelines in the management of allergic diseases. The results of a survey performed by Roberts et al24 concluded that these differences cannot be explained by the availability of neither different health care professionals nor health care expenditure. Therefore, methods of improving postgraduate medical education should be ensured to increase physicians' awareness for optimal allergy treatment based on solid scientific evidences.
Our study has some limitations. Because the participants volunteered to take part in this meeting, those who experienced allergic symptoms could have been enrolled more. Other limitations are that some participants did not respond to every question, although parents answered on behalf of their children.
The initial aim of our study was to understand knowledge, attitudes, and beliefs about allergy (including asthma), assessed by questionnaires at baseline and reevaluate the results immediately after an educational session. This reevaluation could not be succeeded due to logistic and financial reasons. However, this is the first study, at least to our knowledge, that evaluates not only the awareness of allergic conditions in patients who declare to be experiencing symptoms related to allergic diseases but also on public level. Consequently, increased allergy knowledge is needed not only among the affected individuals but also among the general public.
In conclusion, the results of our survey highlight the need to conduct continuous and repetitive education to raise the awareness on allergy and to mitigate the effects of the disease among the affected individuals, as well as in the society.
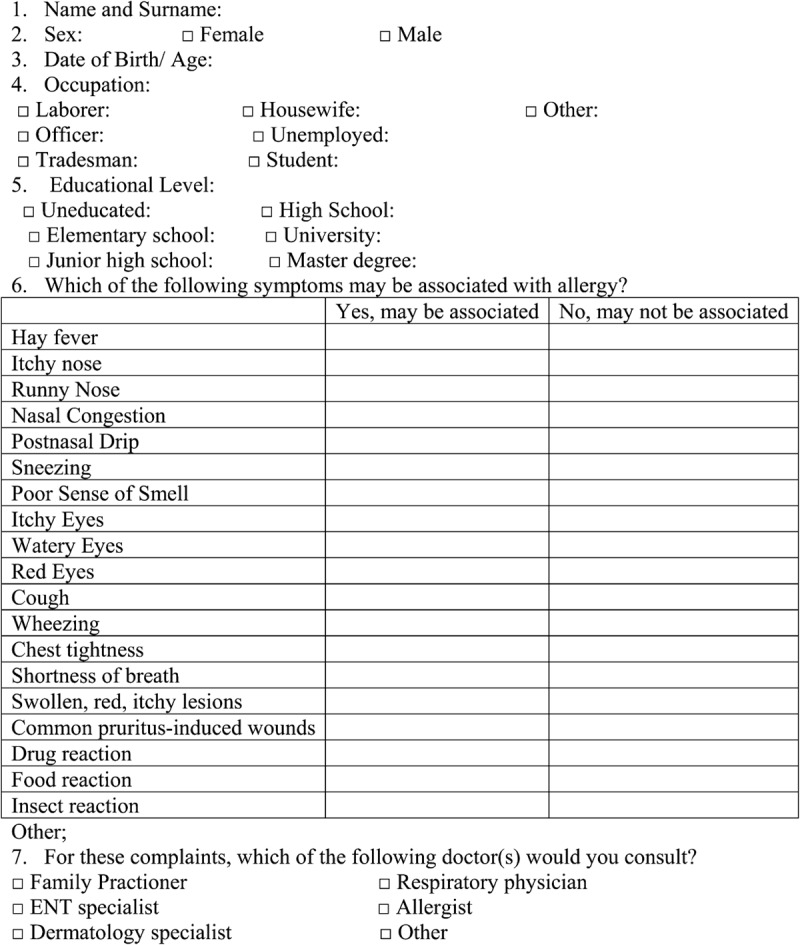
APPENDIX. ALLERGY and YOU
REFERENCES
- 1.Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, et al. World Health Organization; GA(2)LEN; AllerGen. Allergic rhinitis and its impact on asthma (ARIA) 2008 update (in collaboration with theWorld Health Organization, GA2LEN and AllerGen). Allergy. 2008;63:8–160. doi: 10.1111/j.1398-9995.2007.01620.x. [DOI] [PubMed] [Google Scholar]
- 2.Rydén O, Andersson B, Andersson M. Disease perception and social behaviour in persistent rhinitis: a comparison between patients with allergic and nonallergic rhinitis. Allergy. 2004;59:461–464. doi: 10.1046/j.1398-9995.2003.00331.x. [DOI] [PubMed] [Google Scholar]
- 3.Nolte H, Nepper-Christensen S, Backer V. Unawareness and undertreatment of asthma and allergic rhinitis in a general population. Respir Med. 2006;100:354–362. doi: 10.1016/j.rmed.2005.05.012. [DOI] [PubMed] [Google Scholar]
- 4.Bousquet J, Knani J, Henry C, et al. Undertreatment in a nonselected population of adult patients with asthma. J Allergy Clin Immunol. 1996;98:514–521. doi: 10.1016/s0091-6749(96)70084-2. [DOI] [PubMed] [Google Scholar]
- 5.Nish WA, Schwietz LA. Underdiagnosis of asthma in young adults presenting for USAF basic training. Ann Allergy. 1992;69:239–242. [PubMed] [Google Scholar]
- 6.Nathell L, Larsson K, Jensen I. Determinants of undiagnosed asthma. Allergy. 2002;57:687–693. doi: 10.1034/j.1398-9995.2002.23560.x. [DOI] [PubMed] [Google Scholar]
- 7.Leynaert B, Bousquet J, Neukirch C, Liard L, Neukirch F. Perennial rhinitis: an independent risk factor for asthma in nonatopic subjects: results from the European Community Respiratory Health Survey. J Allergy Clin Immunol. 1999;104:301–304. doi: 10.1016/s0091-6749(99)70370-2. [DOI] [PubMed] [Google Scholar]
- 8.Juniper EF. Quality of life in adults and children with asthma and rhinitis. Allergy. 1997;52:971–977. doi: 10.1111/j.1398-9995.1997.tb02416.x. [DOI] [PubMed] [Google Scholar]
- 9.de Monchy J, Andersen PS, Bergmann KC, Chivato T, Holm-Hansen A, Jarisch R, et al. Living & Learning with allergy: a European perception study on respiratory allergic disorders. Respir Med. 2004;98:404–412. doi: 10.1016/j.rmed.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 10.Gupta RS, Kim JS, Springston EE, Smith B, Pongracic JA, Wang X, Holl J. Food allergy knowledge, attitudes, and beliefs in the United States. Ann Allergy Asthma Immunol. 2009;103:43–50. doi: 10.1016/S1081-1206(10)60142-1. [DOI] [PubMed] [Google Scholar]
- 11.Dahl R, Andersen PS, Chivato T, Valovirta E, de Monchy J. National prevalence of respiratory allergic disorders. Respir Med. 2004;98:398–403. doi: 10.1016/j.rmed.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 12.Apter AJ, Reisine ST, Affleck G, Barrows E, ZuWallack RL. Adherence with twice-daily dosing of inhaled steroids. Socioeconomic and health-belief differences. Am J Respir Crit Care. 1998;157:1810–1817. doi: 10.1164/ajrccm.157.6.9712007. [DOI] [PubMed] [Google Scholar]
- 13.Peterson JW, Sterling YM, Stout JW. Explanatory models of asthma from African-American caregivers of children with asthma. J Asthma. 2002;39:577–590. doi: 10.1081/jas-120014922. [DOI] [PubMed] [Google Scholar]
- 14.Justin-Temu M, Risha P, Abla O, Massawe A. Incidence, knowledge and health seeking behaviour for perceived allergies at household level: a case study in Ilala district Dar es Salaam Tanzania. East Afr J Public Health. 2008;5:90–93. [PubMed] [Google Scholar]
- 15.National Asthma Education and Prevention Program. Expert Panel Report II: National Guidelines for the Diagnosis and Management of Asthma, Clinical Practice Guidelines. Bethesda, MD: National Hearth, Lung and Blood Institute, National Institutes of Health; 1997. [Google Scholar]
- 16.van Dellen QM, van Aalderen WMC, Bindels PJE, Öry FG, Bruil J, Stronks K PEACE study group. Asthma beliefs among mothers and children from different ethnic origins living in Amsterdam, the Netherlands. BMC Public Health. 2008;8:380. doi: 10.1186/1471-2458-8-380. ( http://www.biomedcentral.com/1471-2458/8/380) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zayas LE, McLean D. Asthma patient education opportunities in predominantly minority urban communities. Health Educ Res. 2007;22:757–769. doi: 10.1093/her/cyl070. [DOI] [PubMed] [Google Scholar]
- 18.Abdulwadud O, Abramson M, Forbes A, James A, Walters EH. Evaluation of a randomised controlled trial of adult asthma education in a hospital setting. Thorax. 1999;54:493–500. doi: 10.1136/thx.54.6.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Babey SH, Meng YY, Jones M. Many Californians with asthma have problems understanding their doctor. Policy brief. UCLA Cent Health Policy Res. 2009;(PB2009–1):1–8. [PubMed] [Google Scholar]
- 20.European Federation of Allergy and Airways Diseases Patients Association (EFA). EFA. Manifesto of the European allergy patient. In: Kazan Sophie., editor. Brussels: EFA; 2006. [Google Scholar]
- 21.Gijsbers van Wijk CM, van Vliet KP, Kolk AM, Everaerd WT. Symptom sensitivity and sex differences in physical morbidity: a review of health surveys in the United States and The Netherlands. Women Health. 1991;17:91–124. doi: 10.1300/J013v17n01_06. [DOI] [PubMed] [Google Scholar]
- 22.Stingone JA, Claudio L. Disparities in allergy testing and health outcomes among urban children with asthma. J Allergy Clin Immunol. 2008;122:748–753. doi: 10.1016/j.jaci.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 23.Khan SN, Slavin RG. Pediatricians' attitudes towards allergy: past and present attitudes of pediatricians towards allergy. Ann Allergy Asthma Immunol. 2000;85:189–193. doi: 10.1016/S1081-1206(10)62465-9. [DOI] [PubMed] [Google Scholar]
- 24.Roberts N, Papageorgiou P, Partridge MR. Delivery of asthma and allergy care in Europe. J Asthma. 2009;46:767–772. [PubMed] [Google Scholar]


