Abstract
Abstract:
Allergist/clinical immunologist maintenance of certification and training program reaccreditation are mandatory in some countries. The World Allergy Organization conducted surveys in 2009 and 2011 to assess where such programs were available and to promote the establishment of such programs on a global level. This was done with the presumption that after such an “inventory,” World Allergy Organization could offer guidance to its Member Societies on the promotion of such programs to assure the highest standards of practice in the field of allergy and clinical immunology. This review draws on the experience of countries where successful programs are in place and makes recommendations for those wishing to implement such programs for the specialty.
Key Words: allergy and clinical immunology, allergist, physician skills, physician competencies, physician performance measurement
Medical science and the practice of medicine are continuously evolving at an ever-increasing rate. The public expects the medical profession to deliver the highest quality of care to patients. Development and maintenance of professional standards through maintenance of certification (MOC) is one method to do so. This is a self-sustaining process promoted by different entities in various parts of the world. The purpose of MOC is to make sure that the physicians adhere to updated standards in the specialty and to ensure cost-effectiveness in their practice. In addition, the same process indirectly influences and discourages unacceptable medical practices.1 Medical specialty certification, in the field of allergy/immunology, begins the process of assuring quality medical care.2,3 Beyond initial certification, MOC is mandatory to guarantee that the process of learning and staying current with medical advancements is a lifelong process.4,5 Six core competencies are identified by the American Board of Medical Specialties to be important in the process. They include patient care, professionalism, practice improvement, medical knowledge, communications, and systems-based practice.6
The World Allergy Organization (WAO) is an international umbrella organization whose members consist of 89 regional and national allergy and clinical immunology societies from around the world. By collaborating with its member societies, WAO provides direct educational outreach programs, symposia, and lectures to members in 100 countries.7 The WAO Board of Directors initiated this project to make an inventory of MOC practices in the national member society countries. In 2009 and 2011, a survey was conducted among the members of the Education Council, the Specialty and Training Council, and other WAO bodies having rapport with the existing national systems for the MOC and for accreditation and reaccreditation of training programs and schemes. The aim of the survey was to ascertain whether such programs were well established at a global level, or if there is a need for WAO to offer guidance to its membership on the introduction and maintenance of programs to promote high standards in the practice of allergy and clinical immunology. The responses received from different geographical regions suggested that although some countries had systems in place to conduct one or both of these processes in the field of allergy and clinical immunology (Table 1), the global coverage was far from universal. This review draws on the experience of countries where successful systems are in place to make recommendations for those wishing to implement a national system for allergy and clinical immunology specialists.
TABLE 1.
MOC/Accreditation of training programs

A system to ensure continuous professional development (CPD) of medical specialists requires 2 complementary components:
A defined process for MOC for specialists. This includes specific procedures, goals, and time intervals.
Approved training programs to cover key specialist competencies and their continuous upgrading and revalidation—accreditation and reaccreditation of training programs.
The WAO Position Paper, “Requirements for physician competencies in allergy: key clinical competencies appropriate for the care of patients with allergic or immunologic diseases,”8 outlined the optimal level of knowledge, technical and skills objectives, and desirable attitudes for the allergy/clinical immunology specialist. Depending on the local needs and circumstances, such lists may provide a useful foundation for the development of MOC and training program reaccreditation in the field of allergy and clinical immunology (see Appendix). Training programs presently in use, in countries where such procedures are mandatory, could also provide useful models for countries where such programs do not exist.
The 2 components, MOC of individuals and reaccreditation of training programs, should derive from and complement the continuous process of graduate and postgraduate education. They should provide a vehicle to achieve smooth transition to maturity of medical specialists and thus ensure the growth of manpower resources in allergy and clinical immunology. Their structure and function at a national level may differ depending on the relationships between the specialist community, academia, and the physician-licensing authorities (Table 2).
TABLE 2.
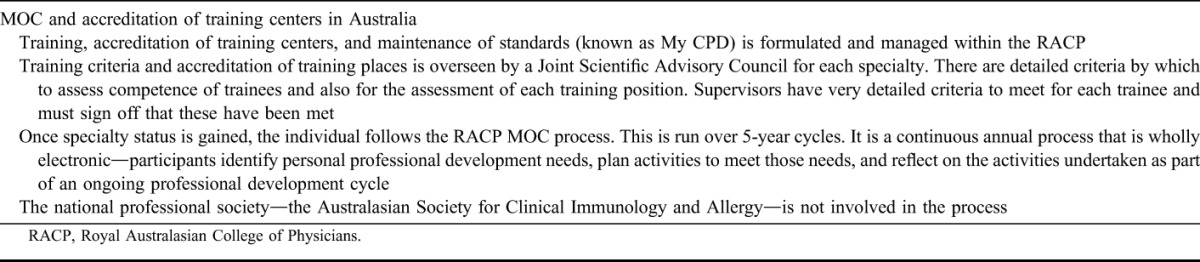
A Successful System—MOC in Australia
FRAMEWORK FOR MOC/REACCREDITATION OF TRAINING PROGRAM MODELS
The MOC/reaccreditation of training program models in allergy and clinical immunology should take into account the specific features of allergic diseases, recognizing that these are systemic diseases with underlying immunological mechanisms and with a wide variety of organ manifestations.9,10 They need to address the wide-ranging skills, knowledge, and competencies required for a specialist (ie, the allergist/clinical immunologist). However, there are conceptual differences between MOC of specialists and accreditation/reaccreditation of training programs, which necessitate separate assessment programs for each of these 2 entities. Ideally, the MOC or recertification of specialists should be based on the same standards of achievement as the ones that regulate the first time certification. Such standards should be decided by the leaders of the specialty, or the corresponding government medical authorization body (as in several countries, it is not the society that gives the certification but a medical council or relevant government authority in medicine), and the standards should be periodically updated in line with the most current medical literature and the needed care of the population served. Although the first time certification is the starting point of an independent specialist career and should therefore require particular scrutiny on the part of a certification authority, the subsequent MOC time points should provide for evidence of incorporation of novel diagnostic and treatment modalities into an individual's clinical practice. Therefore, the MOC procedures should make use of continuous medical education (CME) and CPD systems for life-long learning at the regional level, national level, and where available, international level. The time points for MOC should reflect the evolution of new information in the specialty. The process should not be punitive. Typically, 3 or 4 MOC cycles would be appropriate for a lifetime specialist career of 30 to 35 years. The oversight of MOC of specialists preferably should be exercised by the professional authority issuing the initial certification and not by the governmental institutions and agencies.
At a national level, the process of accreditation/reaccreditation of training programs should involve the participation of a broad circle of experts, specialty organizations, and training program directors or their designees, and it should be driven “on demand” by practice-changing innovations. Such programs should be required to provide evidence of graduating a certain number of students to specialist status over a given period (eg, a 5-year period) as a measure of their effectiveness.
WAO can contribute to the establishment of globally recognized standards in allergy and clinical immunology practice in 2 ways. First, by establishing and regularly updating the recommendations for physician training in allergy and clinical immunology to provide the following:
A model of required and desirable specialist knowledge, technical and skill objectives, and desirable attitudes for the initial certification and MOC of individuals, which will in turn provide a benchmark for training program content for accreditation/reaccreditation purposes (Appendix);
A self-assessment tool for allergists who are considering their individual educational needs and CME requirements, for example, accreditation programs that involve reading online lectures and updates and answering multiple choice questions and awarding “knowledge” accreditation points, which local allergy training councils will accept for the purposes of recertification. In addition, there could be recommended mechanisms of assessing clinical competence and procedures by the local medical councils/bodies.
Second, by recommending the global introduction of MOC standards to help national societies provide a lobby for a challenging, cost-effective, mostly nonpunitive educational process and also to propose how it should be implemented. The national societies of allergy and clinical immunology, and training program directors or their designees, should be the natural interface for the adoption of new practices for the existing programs, and it should maintain a dialogue with allergy/clinical immunology specialists and appropriate health care organizations. This cross talk should allow both specialists and institutions to have a say in incorporating their respective needs into the training program accreditation/reaccreditation process. At the same time, precautions should be in place to prevent commercial bias and self-serving behavior.
Understandably, variations are expected between countries, depending upon the maturity of the specialty and whether allergy and/or allergy/clinical immunology is recognized as a separate specialty or a subspecialty. This fact probably accounts for the poor rate of response to the WAO survey because in countries where allergy/clinical immunology is not recognized as a specialty, individuals refrained from answering the questionnaire. This limitation could be overcome further down the road by adding data through personal contacts and telephone calls. Where allergy and/or allergy/clinical immunology does not currently have specialty recognition, the WAO recommendations for the competencies required to treat patients with allergic and immunologic diseases may be particularly helpful for the individual specialist seeking to identify appropriate CPD and CME educational activities. This review article should be a benchmark for societies and national medical bodies around the globe to help them establish such programs, setting up their own time frame for achieving it.
ADMINISTRATIVE AND LEGAL ASPECTS
The concept of MOC presumes the existence of a recognized certifying authority. It would be advisable to have a national administrative nongovernmental authority responsible for enunciating the national standard and hosting the process of certification and MOC of allergy/clinical immunology specialists and also for vetting the process at regular intervals. The scientific content and logistic structure and functions should be defined by a legal document issued by the governing institution or a legislative body.
The organization of the procedure for accreditation and reaccreditation of training programs should be the joint task of the national societies of allergy/clinical immunology and the national training programs, or corresponding national medical government bodies who are authorized to provide such certification. This procedure may be sanctioned by the administrative body, under whose jurisdiction the certification and MOC of medical specialists occurs.
SUMMARY
Systems that support the need for allergists/clinical immunologists to pursue lifelong education to maintain and update their clinical competency and to ensure that training programs are up-to-date and effective will lead to improved patient care and enhance recognition of the specialty of Allergy and Clinical Immunology.
For those countries wishing to implement such systems, WAO offers the following recommendations for the institution and standardization of programs designed to ensure the development and maintenance of skills and competencies for the allergist/clinical immunologist:
The guiding factor in the development of a program is that it will benefit both patients and physicians
The program should be nonpunitive to the physician for whom it is intended
The program should contain a didactic element; the process to implement it should be a learning experience ending in an examination, which demonstrates increased medical knowledge
Multiple sources of information are necessary to demonstrate the competency of the physician seeking MOC, including patients, ancillary staff, fellow specialists, and other physicians and health professionals. Multiple assessment tools are necessary, including open-book testing of knowledge, proctored examinations, practice assessment, patient care outcomes, and quality improvement
The process should be flexible and adaptable to changes in medicine, science, and the practice of allergy and clinical immunology, and it should recognize local needs, availability of medications and diagnostic tests, and service capabilities
Outcomes should be identified that can be monitored and quantified to verify that the process is beneficial
If problems appear in the MOC for individuals, or in the procedures for revalidation of training programs, which have the potential to jeopardize patient care or the education of physicians, a remediation process to rectify the problems and processes is necessary. If these problems cannot be rectified, then the physician or the training program in question should not be recertified/reaccredited.
ACKNOWLEDGMENT
The authors thank Karen Henley, staff liaison to the Education Council, for her support in the development of this article.
APPENDIX. Recommended Objectives for Physician Competencies in Allergy
The following lists are taken from the “Requirements for physician competencies in allergy: key clinical competencies appropriate for the care of patients with allergic or immunologic diseases.”8 Based on the local needs and service capabilities, these recommendations may be divided as appropriate into “recommended” and “desirable” objectives, or omitted if inappropriate to the local situation.
A. Knowledge Objectives
Immune mechanisms involved in the development of immunologically mediated diseases and, in particular, allergic sensitization and disease formation.
Genetic and environmental factors, including infectious diseases, involved in the genesis of allergic diseases.
Pathogenesis of rhinoconjunctivitis, otitis, rhinosinusitis, asthma, atopic dermatitis, urticaria, and angioedema; drug and food allergy; insect allergy and anaphylaxis; and the concept that most allergic diseases are systemic in etiology.
Relationship between tissue inflammation and repair.
Mechanisms of IgE-mediated immediate phase and late or delayed phase allergic reactions.
Mechanisms of non-IgE-mediated allergic reactions and other disorders in the differential diagnosis of allergic disease: These diseases include, but are not limited to, nonallergic rhinitis, drug-induced rhinitis, acute and chronic rhinosinusitis, nonallergic asthma, cough, bronchitis, non-IgE-mediated anaphylaxis, idiopathic urticaria, eczema, otitis, conjunctivitis, eosinophilic esophagitis, gastroenteritis, and colitis, celiac-like syndromes, food-induced enteropathies leading to gastroesophageal reflux, esophagitis, gastritis, and gut motility disorders, including constipation.
National, regional, and global epidemiology of allergic diseases.
Local airborne, contact, and occupational allergens.
Classification and relative importance of all relevant allergens and their biological characteristics, including heat and digestive stability and cross-reactivity, understanding of local pollen counts and the characteristics of various aeroallergens and routes of allergen exposure.
- Therapy
- (a) Use and route of administration of antihistamines; mast cell stabilizers; bronchodilators; nasal, oral, and parenterel, topical, and inhaled glucocorticosteroids; decongestants; leukotriene modifiers; theophylline; adrenergic agonists; anticholinergics; mucolytics; antibiotics; adrenaline; and all other pharmacologic and immunologic agents used to treat allergic and immunologic diseases.
- (b) Use of emollients, antibiotics, topical glucocorticosteroids, immune modulators, and all other agents and techniques used to manage eczema and other allergic skin disorders.
- (c) Use of immune modulators, such as specific allergen immunotherapy, monoclonal antibodies, including anti-IgE, and immunoglobulin replacement used to treat allergic and immunologic disorders, knowledge of immune modulators that are being developed for clinical use in allergic and immunologic disorders.
- (d) Methods and value of allergen-avoidance techniques.
- (e) Avoidance diets and nutritional implications of dietary modification.
- (f) Knowledge of national and international guidelines for the management of anaphylaxis, allergic and immunologic disorders in adults and children, with particular emphasis on safety and efficacy of all therapies.
Investigation and management of adverse reactions to drugs and vaccines.
Methods to measure cells and mediators in biological fluids and tissues.
Primary and secondary prevention of allergy, particularly in children.
Understanding of the social and psychological issues associated with allergic diseases.
Diagnosis and management of occupational allergic diseases.
Methods to monitor home or work environments for allergens associated with allergic diseases.
Understanding of environmental factors such as pollutants and occupational allergens and of viral respiratory tract infections that affect allergic sensitization and disease development.
Recognition/diagnosis and treatment or appropriate referral of patients with humoral and cellular immunodeficiencies, hereditary and acquired complement deficiencies, and phagocytic disorders, depending upon whether the specialist is an allergist or allergist/clinical immunologist.
B. Skills Objectives
-
Clinical skills
-
Differential diagnosis, evaluation, and management or appropriate immunological referral of the following:
Eczema
Rhinoconjunctivitis
Conjunctivitis
Rhinosinusitis
Atopic dermatitis
Asthma, cough, dyspnea, and recurrent wheeze
Acute and chronic urticaria, including physical urticarias
Angioedema, including hereditary angioedema
Anaphylaxis
Food allergy and intolerance
Drug and vaccine allergies or intolerance
Insect allergy/hypersensitivity
Oral allergy syndrome
Latex allergy
Occupational allergy, asthma, eczema
Otitis
Common variable immunoglobulin deficiency and related immunodeficiencies
Primary immunodeficiencies
Secondary immunodeficiencies
Complement deficiencies
Abnormalities of phagocytic cells
Management of patients with multiple or complex allergies and eosinophilic disorders.
-
Management of patients with multiple food allergies, requiring avoidance diets.
Provision of allergen avoidance advice.
Safe supervision of food and drug challenges.
Assessment of patients for immunotherapy. Proper administration of immunotherapy including immunotherapy dose adjustment and management of complications. Supervision of immunotherapy protocols. Recognition and management of allergic reactions associated with immunotherapy.
Recognition of indications for and the skills to perform, interpret, and understand the limitations of skin prick, intradermal, patch, and delayed type skin tests, and specific in vitro IgE antibody tests.
Interpretation of natural allergen and environmental exposures.
Evaluation and differentiation of non-IgE-mediated hypersensitivity reactions.
Investigation and management of behavioral problems related to allergic and immunologic diseases.
Improvement of patient compliance with pharmacotherapy regimens through personalized disease management plans.
Management in the community of patients at risk of anaphylactic reactions, incorporating an understanding of integrated care pathways.
Diagnosis, treatment, and/or referral of primary and secondary humoral and cellular immunodeficiencies. Such diseases include, but are not limited to, X-linked agammaglobulinemia, common variable immunodeficiency, functional antibody deficiency, severe combined immunodeficiency, thymic dysplasia, Wiskott–Aldrich syndrome, ataxia telangiectasia, and various lymphocyte activation defects.
Safe and effective administration of intravenous and subcutaneous gamma globulin.
Recognition and management or appropriate referral of hereditary and acquired complement deficiencies.
Knowledge about and treatment/referral of phagocytic cell disorders, such as Chediak–Higashi syndrome, chronic granulomatous disease, leukocyte adhesion defects, and a variety of congenital and acquired neutropenias.
C. Technical Skills and Knowledge About Technical Procedures—Objectives
Performance and interpretation of skin prick, intradermal, patch tests, and delayed hypersensitivity tests.
Performance of diagnostic testing for suspected drug, biological, or vaccine allergy.
Safe preparation and administration of immunotherapy vaccines.
Performance of allergen provocation tests, such as nasal, conjunctival, bronchial, and oral challenges, and food and medication challenges.
Performance of patch testing for contact dermatitis.
Performance or knowledge of rhinoscopy and laryngoscopy, nasal endoscopy, acoustic rhinometry, and rhinomanometry.
Performance of basic lung function testing, including spirometry and bronchial provocation tests (methacholine or histamine or mannitol challenges, measurement of flow-volume loops and pulse oximetry, and pre- and postbronchodilator testing).
Knowledge of how and when to measure exhaled nitric oxide, and how and when to perform whole-body plethysmography and impulse oscillometry.
Knowledge of how and when to use various tests to measure airway inflammation and/or constriction, including induced sputum and/or bronchial and bronchoalveolar lavage.
Assessment of environmental hazards in occupational allergy.
Management of exclusion diets and provocation diets.
Knowledge of and ability to interpret measurements of immune function, including serum immunoglobulin levels, IgG subclass levels, pre- and postimmunization antibody titers, isohemagglutinin titers, and other ancillary tests for use in the differential diagnosis of congenital or acquired humoral immunodeficiency.
Measurement and interpretation of laboratory tests to diagnose hereditary angioedema and complement deficiencies.
Measurement of phagocytic and chemotactic function.
D. Attitudes
Ability to work with colleagues in other disciplines.
Appreciation of the scope and limitations of allergy testing.
Appreciation of the limitations and problems created by the so-called complementary medicine or alternative allergy practices.
Understanding of the role of patient support groups and ability and willingness to work with patient support organizations.
Appreciation of all the issues relating to patient confidentiality and the ethical standards expected of all physicians.
Understanding of the research protocols, the ethics of experimental design, data analysis, biostatistics, good clinical practice, good laboratory practice, and a willingness to become involved in either clinical or basic translational research.
Knowledge of the country-specific legal framework for reporting of occupational diseases and assisting patients in obtaining compensation for occupational diseases.
An ability to be a clinical decision maker, communicator, collaborator, manager, health care advocate, and scholar.
REFERENCES
- 1.Shaw K, Cassel CK, Black C, Levinson W. Shared medical regulation in a time of increasing calls for accountability and transparency: comparison of recertification in the United States, Canada, and the United Kingdom. JAMA. 2009;302:2008–2014 [DOI] [PubMed] [Google Scholar]
- 2.Norcini JJ, Kimball HR, Lipner RS. Certification and specialization: do they matter in the outcome of acute myocardial infarction? Acad Med. 2000;75:1193–1198 [DOI] [PubMed] [Google Scholar]
- 3.Horowitz SD, Miller SH, Miles PV. Board certification and physician quality. Med Educ. 2004;38:10–11 [DOI] [PubMed] [Google Scholar]
- 4.Brennan TA, Horwitz RI, Duffy FD, Cassel CK, Goode LD, Lipner RS. The role of physician specialty board certification status in the quality movement. JAMA. 2004;292:1038–1043 [DOI] [PubMed] [Google Scholar]
- 5.Holmboe ES, Wang Y, Meehan TP, Tate JP, Ho SY, Starkey KS, Lipner RS. Association between maintenance of certification examination scores and quality of care for medicare beneficiaries. Arch Intern Med. 2008;168:1396–1403 [DOI] [PubMed] [Google Scholar]
- 6.American Board of Medical Specialties Available at: http://www.abms.org/maintenance_of_certification/MOC_competencies.aspx Accessed January 15, 2012.
- 7.World Allergy Organization (WAO) Available at: http://www.worldallergy.org/wao_societies/aboutwao.php Accessed January 15, 2012.
- 8.Kaliner MA, Del Giacco S, Crisci CD, Frew AJ, Liu G, et al. ; WAO Specialty and Training Council Requirements for physician competencies in allergy: key clinical competencies appropriate for the care of patients with allergic or immunologic diseases. World Allergy Organ J. 2008;1:42–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Del Giacco S, Rosenwasser LJ, Crisci CD, Frew AJ, Kaliner MA, et al. What is an allergist? A position statement of the WAO Specialty and Training Council. World Allergy Organ J 2008;1:19–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pawankar R, Canonica GW, Holgate ST, Lockey RF, eds. WAO White Book on Allergy. Milwaukee, WI: World Allergy Organization; 2011:1–216 Available at: http://www.worldallergy.org/definingthespecialty/white_book.php [Google Scholar]


