Abstract
Purpose
To evaluate 14-week effects of intravitreal ranibizumab or triamcinolone in eyes receiving focal/grid laser for diabetic macular edema (DME) and panretinal photocoagulation (PRP).
Methods
Three hundred and forty-five eyes with a visual acuity of 20/320 or better, center-involved DME receiving focal/grid laser, and diabetic retinopathy receiving prompt PRP were randomly assigned to sham (n=123), 0.5-mg ranibizumab (n=113) at baseline and 4 weeks, or 4-mg triamcinolone at baseline and sham at 4 weeks (n=109). Treatment was at investigator discretion from 14 to 56 weeks.
Results
Mean changes (±standard deviation) in visual acuity letter score from baseline were significantly better in the ranibizumab (+1±11, P<0.001) and triamcinolone (+2±11, P<0.001) groups compared with the sham group (-4±14) at the 14-week visit, mirroring retinal thickening results. These differences were not maintained when study participants were followed for 56 weeks for safety outcomes. One eye (0.9%, 95% CI: 0.02% to 4.7%) developed endophthalmitis after receiving ranibizumab. Cerebrovascular/cardiovascular events occurred in 4%, 7%, and 3% of the sham, ranibizumab, and triamcinolone groups, respectively.
Conclusions
The addition of 1 intravitreal triamcinolone or 2 ranibizumab injections in eyes receiving focal/grid laser for DME and PRP is associated with better visual acuity and decreased macular edema by 14 weeks. Whether continued long-term intravitreal treatment is beneficial cannot be determined from this study.
Keywords: proliferative diabetic retinopathy, diabetic macular edema, panretinal photocoagulation, ranibizumab, triamcinolone, randomized clinical trial, Diabetic Retinopathy Clinical Research Network
INTRODUCTION
Scatter photocoagulation (also referred to as panretinal photocoagulation or PRP) has been the standard treatment for proliferative diabetic retinopathy (PDR) since the Diabetic Retinopathy Study demonstrated that PRP should be considered when an eye approaches or has high risk PDR.1 The 2-year risk of severe visual acuity loss (<5/200 at 2 consecutive visits 4 months apart) without treatment in the Diabetic Retinopathy Study was reduced by approximately 60%. Data from the Early Treatment Diabetic Retinopathy Study (ETDRS) Group suggest that the 5-year risk of severe visual acuity loss for those with PDR could be reduced to approximately 1% with careful follow-up, prompt PRP, and vitrectomy when necessary.2
Although PRP is remarkably effective at reducing visual loss if applied in a timely and appropriate manner, worsening of existing macular edema, often accompanied by visual acuity loss, is a recognized side effect of PRP. Documentation of this side effect is limited and consists mainly of case reports and case series.3–6 In the ETDRS among eyes with center-involved macular edema (as graded on stereoscopic fundus photographs) at baseline, 19% lost ≥10 letters, including 11% that lost ≥15 letters, 4 months following baseline PRP (unpublished data from the ETDRS dataset analyzed by the Jaeb Center for Health Research). However, in a study conducted by the Diabetic Retinopathy Clinical Research Network (DRCR.net), eyes without center-involved diabetic macular edema (DME) at the time of PRP that underwent PRP in a single session did not develop an increase in edema or a reduction of visual acuity that was judged to be clinically meaningful.7 Specifically, in eyes without DME involving the center of the macula, median increases in optical coherence tomography (OCT) central subfield thickness 17 weeks after initiating PRP in 1 or 4 sittings was +14 or +15 μm (25th percentile = +5 or +6, 75th percentile = +20 or +34 μm), respectively, with little decrease in visual acuity (median −1 letter, 25th and 75th percentile = −4 and +2 letters).7
If vascular endothelial growth factor (VEGF) has a role in the development or exacerbation of DME,8, 9 then anti-VEGF drugs or corticosteroids or both might have a role in reducing PRP-induced exacerbation of pre-existing DME in the setting of severe non-proliferative diabetic retinopathy (NPDR) or PDR. Small randomized trials and case reports have suggested such a benefit for intravitreal triamcinolone given as an adjunct to PRP in patients with DME.10, 11 Since the start of this current trial, several additional small randomized trials and retrospective studies have been published that suggest a benefit of intravitreal anti-VEGF drugs or corticosteroids for DME.12–16 In addition, the DRCR.net has reported benefits for at least 1 year of intravitreal ranibizumab treatment of DME in the absence of diabetic retinopathy requiring simultaneous PRP, and has reported exploratory analyses suggesting that triamcinolone can reduce the risk of diabetic retinopathy progression.17, 18
In 2007, the DRCR.net began this randomized trial of 364 eyes with center-involved DME to evaluate the short term effects of intravitreal ranibizumab or intravitreal triamcinolone on pre-existing DME and visual acuity in eyes receiving PRP for severe NPDR or non-high risk PDR and also receiving focal/grid laser for DME. Given that PRP was to be completed within 49 days, and it was desired to have the intravitreal ranibizumab or triamcinolone present while the acute effects of PRP on macular edema could occur, the treatment protocol included intravitreal ranibizumab injections at the baseline and the 4 week visit, and intravitreal triamcinolone injection at the baseline visit. There were no restrictions or study guidelines on treatment for DME or diabetic retinopathy after 14 weeks and the study was not designed to determine if there was a long-term benefit of the initial intravitreal treatment. The 56-week follow-up was collected for safety outcomes only.
METHODS
This phase 3 randomized, multi-center clinical trial was conducted by the DRCR.net at 48 clinical sites in the United States. The study adhered to the tenets of the Declaration of Helsinki. The protocol and Health Insurance Portability and Accountability Act compliant informed consent forms were approved by multiple institutional review boards. Each study participant gave written informed consent to participate in the study following an informed consent process. Independent study oversight was provided by a data and safety monitoring committee. The study is listed on www.clinicaltrials.gov, under identifier NCT00445003 (website registration date March 6, 2007) and the protocol is available on the DRCR.net website (www.drcr.net, accessed October 1, 2010). Key aspects of the protocol pertinent to this report are summarized below.
Study Population
Eligible study participants were at least 18 years old with type 1 or type 2 diabetes and without substantial renal disease or uncontrolled hypertension. The major eligibility criteria for a study eye included : (1) presence of severe NPDR or PDR, (2) presence of center-involved DME on clinical exam and central subfield thickness on time domain optical coherence tomography (OCT) (Stratus, Carl Zeiss Meditec, Dublin, CA) ≥250 μm, and (3) best-corrected Electronic-Early Treatment Diabetic Retinopathy Study (E-ETDRS Visual Acuity Test©19) visual acuity letter score ≥24 (approximate Snellen equivalent 20/320 or better). Principal exclusion criteria included: (1) prior PRP that was sufficiently extensive that the investigator did not believe that ≥ 1200 additional burns were needed or possible, (2) treatment for DME within the prior 4 months, (3) history of open-angle glaucoma or steroid-induced intraocular pressure (IOP) elevation that required IOP-lowering treatment, and (4) IOP ≥25 mmHg. At the onset of the study, a study participant could contribute only 1 study eye. However, during the course of the study the protocol was modified to allow participants to have 2 study eyes, provided both were eligible at the time of study entry, with random assignment to different treatments.
Key Aspects of Study Design
After eligibility was determined at the clinical center and informed consent was obtained, study participants with 1 study eye were assigned randomly on the DRCR.net website (using a permuted blocks design stratified by visual acuity and the number of sittings planned to complete the PRP) with equal probability to one of 3 treatment groups: (1) sham injection at baseline and 4 weeks, (2) intravitreal injections of 0.5-mg ranibizumab (Lucentis™, Genentech, Inc., South San Francisco, CA) at baseline and 4 weeks, or (3) intravitreal injection of 4-mg triamcinolone acetonide (Trivaris®, Allergan, Inc.) at baseline and sham injection at 4 weeks. Study participants with 2 study eyes were randomized with equal probability to receive one of the 3 treatment scenarios: sham in the eye with a greater visual acuity score and ranibizumab or triamcinolone in the eye with a lower visual acuity score OR ranibizumab or triamcinolone acetonide in the eye with a greater visual acuity score and sham in the eye with a lower visual acuity score (if both eyes had the same visual acuity letter score, the right eye was considered the eye with the greater visual acuity score).
The initial sham or intravitreal injection was given on the day of randomization. Focal/grid laser for DME was performed 3 to 10 days after the injection for all treatment groups. PRP could be initiated immediately after the focal/grid laser or on a subsequent day, but was to be initiated within 14 days of the baseline injection and fully completed within 49 days of randomization. Additional PRP was performed only if the size or amount of neovascularization increased following completion of the study-required PRP. Follow-up visits were conducted at 1, 4, 14 (primary outcome), 34, and 56 weeks after randomization. Eyes in the ranibizumab group received a second injection and eyes in the sham or triamcinolone groups received a sham injection at the 4-week visit. After the 14-week visit, additional treatment for DME and diabetic retinopathy could be given at investigator discretion as part of standard care (i.e. there were no requirements for repeated ranibizumab, triamcinolone or focal/grid laser treatments). Study participants were masked to treatment assignments. The visual acuity examiner and OCT technician at the primary outcome visit (14 weeks) were masked to treatment groups. All adverse events were recorded, irrespective of whether the event was considered treatment-related.
Study Treatment
Sham and intravitreal injections were preceded by a povidone iodine prep of the conjunctiva. For a sham injection, the hub of a syringe (without a needle) was pressed against the conjunctival surface to simulate the force of an actual injection. Use of antibiotics in the pre-injection, peri-injection, or post-injection period was at investigator discretion.
The focal/grid laser technique was modified from the original ETDRS protocol as described previously and used in prior DRCR.net protocols.20, 21 PRP consisted of 1200 to 1600 burns given over 1 to 3 sittings, as detailed in the protocol (www.drcr.net, accessed October 1, 2010) with completion of the regimen within 49 days of randomization. To avoid bias from knowledge of treatment group assignment, the investigator declared prior to randomization the number of sittings planned to complete the PRP and the approximate number of burns planned for each sitting. Additional anesthesia in the form of retrobulbar, peribulbar or sub-Tenon’s injection could be used at investigator discretion. Slit lamp or an indirect laser delivery system could be used. Lasers with the capability of producing automated patterns (e.g. the PASCAL laser) could be used according to guidelines designed to create equivalent burn characteristics to standard laser. Before the administration of each required PRP sitting after the initial application of PRP, visual acuity was measured. If best-corrected visual acuity decreased from baseline by 10 or more letters (2 or more lines) and the investigator believed the decrease was due to exacerbation of macular edema, the investigator could choose to defer additional PRP for 2 weeks or longer until it was deemed that the risk of adding PRP no longer outweighed the benefits.
Examination Procedures
At baseline and at each follow-up visit except the 1-week visit, best-corrected visual acuity letter score was measured in the study eye at 3 meters by a certified tester using the E-ETDRS visual acuity test©.19 Visual acuity letter scores were measured at the 1-week visit using the baseline refraction. Following pupil dilation, OCT images were obtained at baseline and at each follow-up visit by a certified operator using a standardized protocol as done in a previous DRCR.net protocol on a time domain OCT. If the automated thickness measurements were judged by the Reading Center to be inaccurate on any submitted image, center point thickness was measured manually and this value was used to impute a value for the central subfield based on a correlation of the 2 measures of 0.98 as published previously. 17 At baseline, 29% of 362 baseline scans (2 were lost by the sites) had a central subfield thickness measurement imputed whereas the quality of 2 other scans did not permit automatic or manual grading of the central subfield thickness. During follow-up, 7% of 1,673 follow-up scans had a central subfield thickness measurement imputed and 8 (<1%) had compromised quality that precluded manual grading. Although an imputed thickness <250 μm does not necessarily mean that the true thickness measurement is <250 μm if it had been measureable, manual grading of the baseline scans resulted in an imputed baseline central subfield thickness of <250 μm for 49 eyes (14%). Of note, 12 (24%) of the 49 scans with imputed central subfield thickness <250 μm were from one clinical site, representing 63% of the 19 baseline scans from that site. All data except safety data are presented with exclusion of eyes from that clinical site (19 eyes from 14 subjects), although results were similar when evaluated with inclusion of eyes from that clinical site (data not shown). Results also were similar when evaluated with exclusion of all eyes with a baseline central subfield thickness <250 μm from any clinical site (data not shown). Baseline OCT images also were assessed by the University of Wisconsin-Madison Fundus Photographic Reading Center for cystoid abnormalities and subretinal fluid.
Standard ETDRS 7-field color stereoscopic fundus photographs were obtained at baseline, 14 weeks, and 56 weeks by a certified photographer and graded at the reading center using validated procedures.22 Additional testing included measurement of hemoglobin A1c and blood pressure at baseline and the following procedures at baseline and each follow-up visit: (1) slit lamp examination, (2) fundus examination following pupil dilation, and (3) measurement of IOP.
Statistical Methods
The primary outcome was the mean change in visual acuity from baseline to 14 weeks. A sample size of 364 eyes was planned to have 90% power to detect a difference in the change in the visual acuity letter score from baseline to 14 weeks in two 2-group comparisons (ranibizumab group versus sham group and triamcinolone group versus sham group) assuming a population difference of 6.0, standard deviation of 16, correlation between the baseline and 14-week visual acuities of 0.61, a type 1 error rate of 0.0245 (adjusted for multiple comparisons and for alpha spending in interim analyses to maintain an overall type 1 error rate of 0.05), and no more than 10% loss to follow up.
The primary analysis followed the intent-to-treat principle and included all randomized eyes with the exception of 19 eyes randomized from one clinical site where 63% of eyes had baseline imputed central subfield thickness <250 μm. Data were included in the 14-week analysis for all examinations performed between 70 and 153 days (10 to 22 weeks) from randomization. For the eyes without 14-week data, the last-observation-carried forward method was used to impute data for the primary analysis. Similar results were produced when analyses (1) used Monte Carlo Markov Chains23 to impute missing data, (2) included only eyes with a completed 14-week examination, (3) were performed with truncation of outlier values to be at most 3 standard deviations from the mean, and (4) were performed using ranks of the visual acuity letter scores (instead of the actual scores) transformed to have normal distributions using van der Waerden scores (data not shown).
For analyses other than the primary analysis, only data from completed visits were used with no imputation for missing data. For some results, medians and interquartile ranges have been reported instead of or in addition to means and standard deviations to describe the distribution of the data.
Two pairwise comparisons were made for all analyses. The alpha level was set to 0.02 for the primary outcome comparison using a Bonferroni adjustment for multiple comparisons to preserve the overall type I error rate ≤0.05, while adjusting for alpha spending of 0.01 for 2 interim data reviews (that used alpha spending functions f(t) = min (αt3, α) and f*(t) = min (αt2, α), respectively), and was set to 0.025 for all other outcome comparisons. For all continuous outcomes, the treatment group comparisons were made using analysis of covariance (ANCOVA) models with generalized estimating equations (GEE) to account for correlated data from subjects with 2 study eyes. The interactions between various subgroups and the treatment group were also tested. In view of the large number of factors evaluated, only interactions with P values <0.01 were considered unlikely to be due to chance. For binary outcomes, GEE was also used to account for correlated data from subjects with 2 study eyes, with differences in proportions between treatment groups estimated using binomial regression and relative risks estimated using Poisson regression with robust variance estimation.24 All analyses, unless otherwise specified, included adjustments for the 2 randomization stratification variables; baseline visual acuity and number of sittings to complete the PRP. In addition, models with central subfield thickness as the outcome included baseline central subfield thickness as a covariate and models with retinal volume as the outcome included baseline retinal volume as a covariate. All P values are 2-sided. SAS version 9.1 (SAS Institute, Cary, NC) was used for all analyses.
RESULTS
Between March 2007 and June 2009, 319 study participants (mean age 55±12 years; 40% women) were enrolled, 26 (8%) with 2 study eyes. The 345 study eyes with DME were randomly assigned to either the sham injection group (N=123), ranibizumab injection group (N=113), or triamcinolone injection group (N=109). At baseline, the mean visual acuity letter score in study eyes was 64±15 (approximately 20/50) and the mean OCT central subfield retinal thickness was 392±151 μm. Based on investigator assessment, severe NPDR was present in 18% of eyes and PDR in the other 82%. Based on reading center assessment, moderately severe NPDR or less severe retinopathy was present in 20% of eyes, severe NPDR was present in 5%, and PDR was present in the other 75%, including 35% with high risk PDR (level 71 or 75). The baseline characteristics of the 3 groups were similar (Table 1).
Table 1.
Baseline Study Participant and Ocular Characteristics
| Sham+ Focal/Grid/PRP Laser N = 123 |
Ranibizumab+ Focal/Grid/PRP Laser N = 113 |
Triamcinolone+ Focal/Grid/PRP Laser N = 109 |
|
|---|---|---|---|
| Women, no. (%) | 44 (36%) | 48 (42%) | 44 (40%) |
| Age (yrs) Median (25th, 75th percentile) | 54 (45, 61) | 57 (48, 64) | 58 (49, 64) |
| Race, no. (%) | |||
| White | 76 (62%) | 72 (64%) | 61 (56%) |
| African-American | 11 (9%) | 15 (13%) | 18 (17%) |
| Hispanic or Latino | 31 (25%) | 23 (20%) | 27 (25%) |
| Asian | 3 (2%) | 1 (1%) | 2 (2%) |
| American Indian/Alaskan Native | 1 (1%) | 0 | 1 (1%) |
| Native Hawaiian/Other Pacific Islander | 0 | 1 (1%) | 0 |
| Unknown/not reported | 1 (1%) | 1 (1%) | 0 |
| Diabetes type, no. (%) | |||
| Type 1 | 20 (16%) | 13 (12%) | 12 (11%) |
| Type 2 | 101 (82%) | 93 (82%) | 95 (87%) |
| Uncertain | 2 (2%) | 7 (6%) | 2 (2%) |
| Duration of diabetes (yrs) Median (25th, 75th percentile) * | 15 (8, 21) | 15 (10, 21) | 15 (10, 19) |
| Hemoglobin A1c Median (25th, 75th percentile)† | 7.9 (7.0, 9.6) | 8.1 (7.1, 9.9) | 8.1 (7.0, 9.7) |
| Prior cardiovascular event, no. (%) ‡ | 21 (17%) | 35 (31%) | 28 (26%) |
| Hypertension, no. (%) | 97 (79%) | 88 (78%) | 82 (75%) |
| Number of study eyes | |||
| 1 study eye | 97 (79%) | 100 (88%) | 96 (88%) |
| 2 study eyes | 26 (21%) | 13 (12%) | 13 (12%) |
| Prior scatter photocoagulation§, no. (%) | 16 (13%) | 20 (18%) | 19 (17%) |
| No prior treatment for DME, no. (%) | 80 (65%) | 75 (66%) | 72 (66%) |
| Prior laser for DME, no. (%) | 40 (33%) | 33 (29%) | 36 (33%) |
| Prior intravitreal triamcinolone for DME, no. (%) | 1 (1%) | 9 (8%) | 3 (3%) |
| Prior vitrectomy for DME, no. (%) | 2 (2%) | 0 | 0 |
| Prior peribulbar triamcinolone for DME, no. (%) | 1 (1%) | 0 | 1 (1%) |
| Prior anti-VEGF for DME, no. (%) | 6 (5%) | 1 (1%) | 3 (3%) |
| IOP (mmHg) Median (25th, 75th percentile) | 15 (13, 18) | 16 (14, 18) | 15 (13, 18) |
| Currently on IOP lowering medicine for glaucoma or ocular hypertension, no. (%) | 0 | 3 (3%) | 0 |
| Lens status (clinical exam), no. (%) | |||
| Phakic | 111 (90%) | 91 (81%) | 99 (91%) |
| Pseudophakic | 12 (10%) | 22 (19%) | 10 (9%) |
| Classification of DME (clinical exam), no. (%) | |||
| Predominantly focal | 37 (30%) | 19 (17%) | 27 (25%) |
| Neither predominantly focal or diffuse | 18 (15%) | 25 (22%) | 14 (13%) |
| Predominantly diffuse | 68 (55%) | 69 (61%) | 68 (62%) |
| Baseline visual acuity letter score (approximate Snellen equivalent) by randomization strata | |||
| Median (25th, 75th percentile) | 67 (52, 75) | 68 (56, 75) | 67 (59, 75) |
| ≥66 (better than 20/50) | 66 (54%) | 64 (57%) | 61 (56%) |
| ≤65 (20/50 or worse) | 57 (46%) | 49 (43%) | 48 (44%) |
| Baseline visual acuity letter score (approximate Snellen equivalent) | |||
| 93–89 (20/16) | 0 | 0 | 3 (3%) |
| 88–84 (20/20) | 7 (6%) | 8 (7%) | 6 (6%) |
| 83–79 (20/25) | 10 (8%) | 8 (7%) | 5 (5%) |
| 78–74 (20/32) | 22 (18%) | 24 (21%) | 23 (21%) |
| 73–69 (20/40) | 20 (16%) | 15 (13%) | 10 (9%) |
| 68–64 (20/50) | 11 (9%) | 14 (12%) | 23 (21%) |
| 63–59 (20/63) | 11 (9%) | 10 (9%) | 14 (13%) |
| 58–54 (20/80) | 8 (7%) | 11 (10%) | 7 (6%) |
| 53–49 (20/100) | 6 (5%) | 7 (6%) | 3 (3%) |
| 48–44 (20/125) | 7 (6%) | 6 (5%) | 4 (4%) |
| 49–43 (20/160) | 7 (6%) | 5 (4%) | 5 (5%) |
| 38–34 (20/200) | 6 (5%) | 2 (2%) | 5 (5%) |
| 33–29 (20/250) | 4 (3%) | 1 (1%) | 1 (1%) |
| 28–24 (20/320) | 4 (3%) | 2 (2%) | 0 |
|
Central subfield thickness (μm) on OCT|| Median (25th,75th percentile) |
355 (285, 510) | 352 (283, 476) | 359 (271, 472) |
|
Retinal volume (mm3) on OCT|| Median (25th,75th percentile) |
9.4 (8.4, 10.6) | 9.2 (8.3, 11.0) | 9.1 (8.1, 10.0) |
| OCT cystoid abnormality** (questionable or definite), no. (%) | 108 (88%) | 96 (86%) | 93 (88%) |
| OCT subretinal fluid present** (questionable or definite), no. (%) | 30 (24%) | 31 (28%) | 32 (30%) |
| ETDRS Retinopathy severity level (ETDRS description) from photograph grading, no. (%) | |||
| Level 35, 43 (Mild/Moderate NPDR) | 6 (5%) | 5 (5%) | 6 (6%) |
| Level 47 (Moderately severe NPDR) | 26 (22%) | 15 (14%) | 10 (10%) |
| Level 53 (Severe NPDR) | 5 (4%) | 6 (6%) | 5 (5%) |
| Level 60 (Prior PRP without active neovascularization) | 2 (2%) | 4 (4%) | 3 (3%) |
| Level 61 (Mild/Moderate PDR) | 48 (40%) | 36 (33%) | 38 (36%) |
| Level 71, 75 (High-risk PDR) | 32 (27%) | 43 (39%) | 43 (41%) |
DME = diabetic macular edema; ETDRS = Early Treatment Diabetic Retinopathy Study; VEGF = vascular endothelial growth factor; IOP = intraocular pressure;; NPDR = non-proliferative diabetic retinopathy; PRP = panretinal photocoagulation; PDR = proliferative diabetic retinopathy.
For study participants that answered ‘Uncertain’ type of diabetes was imputed using the age the study participant first started using insulin treatment.
Missing Hemoglobin A1c data for study participants in the sham+ focal/grid/PRP laser, ranibizumab+ focal/grid/PRP laser, and triamcinolone+ focal/grid/PRP laser groups, respectively: 3, 10, and 6.
Includes any pre-existing cardiovascular condition.
Per eligibility criteria the investigator believed that there was still room for 1200–1600 burns.
Missing (or ungradeable) optical coherence tomography (OCT) and fundus photograph data as follows for the laser+ focal/grid/PRP laser, ranibizumab+ focal/grid/PRP laser, and triamcinolone+ focal/grid/PRP laser groups, respectively: central subfield (1, 1, and 2), retinal volume (41, 35, and 38), cystoids change (0, 1, and 3) and retinopathy severity (4, 4, and 4).
From reading center grading.
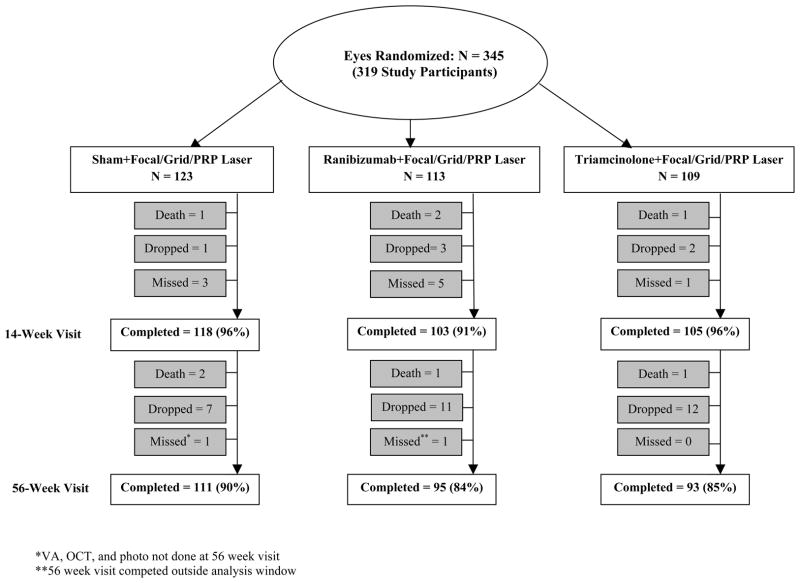
Follow Up
Visit completion rates are shown in Figure 1 (available at ###). Four (1%) study participants died prior to the 14-week primary outcome visit and 4 died subsequently; all from causes apparently unrelated to study treatment. For the remaining study participants, the 14-week visit was completed for 118 eyes (96%) in the sham group, 103 eyes (91%) in the ranibizumab group, and 105 eyes (96%) in the triamcinolone group. The 56-week visit was completed for 111 eyes (90%) in the sham group, 95 eyes (84%) in the ranibizumab group, and 93 eyes (85%) in the triamcinolone group.
Figure 1.
Completion of Follow-up for Study Eyes.
Fourteen week completed visits include visits that occurred between 70 and 153 days (between 10 and 22 weeks) from randomization. Fifty-six week completed visits include visits that occurred between 315 and 468 days (between 45 and 67 weeks) from randomization.
PRP=Panretinal photocoagulation.
Treatment
Treatment for DME prior to the Primary Outcome (14-week) Visit
Except for 1 eye in the triamcinolone group that did not receive an injection, all other eyes received the randomization-assigned sham or intravitreal injection at baseline. A second ranibizumab injection was given at the 4-week study visit in 108 eyes (96%) of the 113 eyes in the ranibizumab group (the 4-week visit was missed for 5 eyes). One eye in the triamcinolone group received triamcinolone at the 4-week visit when sham should have been given. Topical antibiotics appeared to be given less frequently before or after sham injections than before or after ranibizumab or triamcinolone injections (data not shown).
Focal/grid laser was performed in all eyes except 2 eyes (2%) and 3 eyes (3%) in the ranibizumab and triamcinolone groups, respectively. Of those eyes with focal/grid laser, 9 (7%), 7 (6%) and 10 (9%) were performed outside of the 3 to 10 day window from randomization in the sham, ranibizumab, and triamcinolone groups, respectively. Prior to the 14-week visit, no additional (alternative) treatment for DME was given.
Initial PRP Treatment
PRP was not completed in 1 eye (1%), 2 eyes (2%), and 2 eyes (2%) in the sham, ranibizumab, and triamcinolone groups, respectively. Of those eyes with PRP, PRP was completed within 49 days of randomization in 108 eyes (89%), 97 eyes (87%), and 87 eyes (81%) in the sham, ranibizumab, and triamcinolone groups, respectively. PRP was completed in 1 sitting in 49 eyes (40%), 38 eyes (34%), and 41 eyes (38%) in the sham, ranibizumab, and triamcinolone groups, respectively. PRP characteristics did not differ appreciably by treatment group (Table 2).
Table 2.
Panretinal Photocoagulation Treatment
| Sham+ Focal/Grid/PRP Laser | Ranibizumab+ Focal/Grid/PRP Laser | Triamcinolone+ Focal/Grid/PRP Laser | |
|---|---|---|---|
|
| |||
| N = 123 | N = 113 | N = 109 | |
| Initial PRP planned to start on the same day as focal/grid laser (declared prior to randomization), No. (%) | 71 (58%) | 66 (58%) | 65 (60%) |
| Initial PRP started on the same day as focal/grid laser, No. (%) | |||
| Yes | 68 (55%) | 69 (61%) | 60 (55%) |
| No | 54 (44%) | 41 (36%) | 46 (42%) |
| PRP and/or focal/grid laser not done | 1 (1%) | 3 (3%) | 3 (3%) |
| Initial PRP on the same day as focal/grid laser planned/performed, No. (%) | |||
| Yes/Yes | 62 (50%) | 60 (53%) | 54 (50%) |
| Yes/No | 8 (7%) | 4 (4%) | 9 (8%) |
| No/Yes | 6 (5%) | 9 (8%) | 6 (6%) |
| No/No | 46 (37%) | 37 (33%) | 37 (34%) |
| PRP and/or focal/grid laser not done | 1 (1%) | 3 (3%) | 3 (3%) |
| Number of PRP sittings investigator planned to perform (declared prior to randomization), No. (%) | |||
| 1 | 47 (38%) | 40 (35%) | 44 (40%) |
| 2 | 57 (46%) | 54 (48%) | 47 (43%) |
| 3 | 19 (15%) | 19 (17%) | 18 (17%) |
| Number of PRP sittings performed, No. (%) | |||
| 1 | 49 (40%) | 38 (34%) | 41 (38%) |
| 2 | 58 (47%) | 56 (50%) | 50 (46%) |
| 3 | 15 (12%) | 16 (14%) | 16 (15%) |
| 4 | 0 | 1 (1%) | 0 |
| PRP not done | 1 (1%) | 2 (2%) | 2 (2%) |
| Number of PRP sittings planned/performed, No. (%) | |||
| 1/1 | 46 (37%) | 37 (33%) | 40 (37%) |
| 1/2 | 1 (1%) | 3 (3%) | 4 (4%) |
| 2/2 | 54 (44%) | 50 (44%) | 44 (40%) |
| 2/1 or 3 | 2 (2%) | 2 (2%) | 2 (2%) |
| 3/3 | 15 (12%) | 15 (13%) | 15 (14%) |
| 3/1 or 2 or 4 | 4 (3%) | 4 (4%) | 2 (2%) |
| PRP not done | 1 (1%) | 2 (2%) | 2 (2%) |
|
| |||
| N = 122 | N = 111 | N = 107 | |
| Proportion of Eyes with PRP Completed in the protocol window (49 days from randomization)* | 108 (89%) | 97 (87%) | 87 (81%) |
| Number of days from randomization to last PRP sitting* | 26 (14, 41) | 30 (14, 43) | 28 (14, 42) |
| Median (25th, 75th quartiles) [range] | [3, 71] | [3, 171] | [3, 72] |
| Retrobulbar or peribulbar anesthesia used*, No. (%) | 23 (19%) | 14 (13%) | 22 (21%) |
| PRP completed in 1 sitting | 15 (31%) | 9 (24%) | 17 (41%) |
| PRP completed in Multiple sittings (anesthesia administered during at least 1 sitting) | 8 (11%) | 5 (7%) | 5 (8%) |
| PRP automated pattern used*, No. (%) | 36 (30%) | 21 (19%) | 21 (20%) |
| PRP completed in 1 sitting | 13 (27%) | 7 (18%) | 5 (12%) |
| PRP completed in Multiple sittings | 23 (32%) | 14 (19%) | 16 (24%) |
| Indirect laser delivery system used*, No. (%) | 0 | 1 (1%) | 4 (4%) |
| PRP completed in 1 sitting | 0 | 0 | 1 (2%) |
| PRP completed in Multiple sittings | 0 | 1 (1%) | 3 (5%) |
| Total number of burns*† | |||
| Median (25th, 75th quartiles) | 1541 (1281, 1833) | 1410 (1252, 1634) | 1430 (1246, 1815) |
| Baseline retinopathy severity (reading center assessment): NPDR | 1448 (1276, 1805) | 1369 (1223, 1517) | 1416 (1259, 1589) |
| Baseline retinopathy severity (reading center assessment): PDR | 1600 (1305, 1842) | 1474 (1257, 1781) | 1457 (1243, 1835) |
NPDR= Nonproliferative diabetic retinopathy; PDR= Proliferative diabetic retinopathy; PRP=Panretinal Photocoagulation.
Exclude 5 eyes with PRP not performed
Exlcude 12 eyes with missing/nongradable retinopathy severity
Additional PRP Treatment
After completion of the study-required full PRP, additional PRP prior to the 14-week visit was given in 1 eye in the ranibizumab group. There was little to no difference identified among the 3 groups with respect to additional PRP given after 14-weeks, including 21 eyes (19%) in the ranibizumab group (P = 0.39) and 24 eyes (23%) in the triamcinolone group (P=0.77) compared with the sham group (29 eyes [24%]).
Additional Standard Care Treatment for DME at or after the 14-week Visit
Treatment for DME at or after the 14-week visit, which was part of standard care at investigator discretion, was administered to fewer eyes in the ranibizumab group (48 eyes [44%]; P = 0.04) and triamcinolone group (45 eyes [42%]; P = 0.004) compared with the sham group (71 eyes [59%]) (Table 3).
Table 3.
Additional Treatments for Diabetic Macular Edema from 14-Week to 56-Week Visit
| Sham+ Focal/Grid/PRP Laser N = 123 |
Ranibizumab+ Focal/Grid/PRP Laser N = 113 |
Triamcinolone+ Focal/Grid/PRP Laser N = 109 |
|
|---|---|---|---|
| 14 weeks to 56 weeks | |||
| Eyes with additional treatments (number of treatment applied) | 71 (120) | 48 (84) | 45 (78) |
| Additional treatment, No.* | |||
| Bevacizumab | 14 | 12 | 9 |
| Ranibizumab | 1 | 0 | 3 |
| Triamcinolone | 3 | 8 | 2 |
| Pegaptanib | 0 | 0 | 3 |
| Laser | 31 | 10 | 21 |
| Vitrectomy | 2 | 1 | 0 |
| Bevacizumab + Triamcinolone | 2 | 0 | 2 |
| Ranibizumab+Triamcinolone | 0 | 1 | 0 |
| Bevacizumab + Laser | 8 | 5 | 0 |
| Ranibizumab + Laser | 0 | 3 | 0 |
| Triamcinolone + Laser | 7 | 4 | 5 |
| Pegaptanib+Laser | 1 | 0 | 0 |
| Triamcinolone + Vitrectomy | 0 | 1 | 0 |
| Pegaptanib+Vitrectomy | 0 | 1 | 0 |
| Triamcinolone + Laser+Vitrectomy | 0 | 1 | 0 |
| Bevacizumab + Triamcinolone + Laser | 2 | 1 | 0 |
| Eyes with anti-VEGF Treatment (number of treatments applied) | 28 (39) | 23 (32) | 17 (32) |
Number of eyes, each combination of treatment only counted once. VEGF=Vascular endothelial growth factor; PRP=Panretinal photocoagulation.
Effect of Treatment on Visual Acuity through the Primary Outcome (14-week) Visit
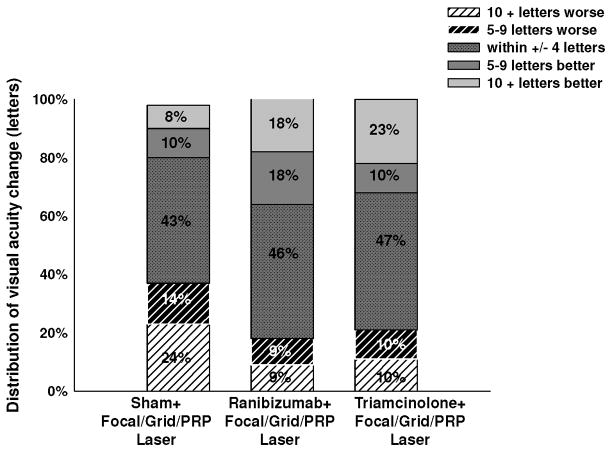
As shown in Table 4 and Figure 2, for the 14-week primary outcome, the mean change ±standard deviation (SD) in the visual acuity letter score from baseline was −4±14 in the sham group, +1±11 in the ranibizumab group (P<0.001 compared with the sham group), and +2±11 in the triamcinolone group (P<0.001 compared with the sham group). The results (Figure 3) reflected both a greater proportion of eyes with an improvement of ≥10 letters (19%, P=0.02 and 22%, P=0.002) and a lower proportion of eyes with a worsening of ≥10 letters (9%, P=0.004 and 10%, P=0.005) in the ranibizumab and triamcinolone groups, respectively, compared with the sham group (8% for ≥10 letter gain and 23% for ≥10 letter loss). Most of the overall improvement in visual acuity from baseline in the ranibizumab and triamcinolone treated groups occurred by the 4-week study visit (Figure 2).
Table 4.
Change in Visual Acuity (Last Observation Carried Forward) from Baseline to 14-Week Visit (Primary Outcome)*
| Sham+ Focal/Grid/PRP Laser | Ranibizumab+ Focal/Grid/PRP Laser | Triamcinolone+ Focal/Grid/PRP Laser | |
|---|---|---|---|
|
| |||
| N = 123 | N = 113 | N = 109 | |
| Change in visual acuity (letter score) | |||
| Mean±standard deviation | −4±14 | +1±11 | +2±11 |
| Median (25th, 75th percentile) | −2 (−8, +3) | +2 (−3, +7) | +1 (−3, +8) |
| Difference in mean change from sham+focal/grid/PRP laser (95% CI) [P Value]† | +5.6 (2.2, 9.0) [P < 0.001] |
+6.7 (3.2, 10.1) [P < 0.001] |
|
| Distribution of change, no. (%) | |||
| ≥15 letter improvement | 5 (4%) | 8 (7%) | 11 (10%) |
| 14–10 letter improvement | 5 (4%) | 13 (12%) | 13 (12%) |
| 9–5 letter improvement | 12 (10%) | 20 (18%) | 13 (12%) |
| Same ±4 letters | 54 (44%) | 53 (47%) | 50 (46%) |
| 5–9 letters worse | 19 (15%) | 9 (8%) | 11 (10%) |
| 10–14 letters worse | 10 (8%) | 2 (2%) | 8 (7%) |
| ≥15 letters worse | 18 (15%) | 8 (7%) | 3 (3%) |
| Difference in proportion with ≥10 letter improvement from sham+ focal/grid/PRP laser (95% CI)‡ | +10% (+1%, +20%) | +14% (+4%, +25%) | |
| Relative risk (95% CI) [P Value]† for comparison with sham+focal/grid/PRP laser |
1.0 | 2.79 (1.33, 5.87) [P = 0.002] |
3.58 (1.69, 7.61) [P < 0.001] |
| Difference in proportion with ≥10 letter worsening from sham+ focal/grid/PRP laser (95% CI)‡ | −13% (−24%, −3%) | −13% (−23%, −3%) | |
| Relative risk (95% CI) [P Value]† for comparison with sham+focal/grid/PRP laser |
1.0 | 0.40 (0.19, 0.87) [P = 0.008] |
0.44 (0.21, 0.91) [P = 0.01] |
Visits occurring between 70 and 153 days (between 10 and 22 weeks) from randomization were included as 14-week visits. When more than 1 visit occurred in this window, data from the visit closest to the 14-week target date were used. For other eyes without any 14-week data (5 eyes in the sham+focal/grid/PRP laser group, 10 eyes in the ranibizumab+focal/grid/PRP laser group, and 4 eyes in the triamcinolone+focal/grid/PRP laser group and) the last observation carried forward method was used to impute data for the primary analysis.
Adjusted for baseline visual acuity, number of planned panretinal photocoagulation (PRP) sittings, and correlation between 2 study eyes. Confidence intervals(CI) are adjusted for multiple comparisons.
Adjusted for correlation between 2 study eyes. CIs are adjusted for multiple comparisons.
Figure 2.
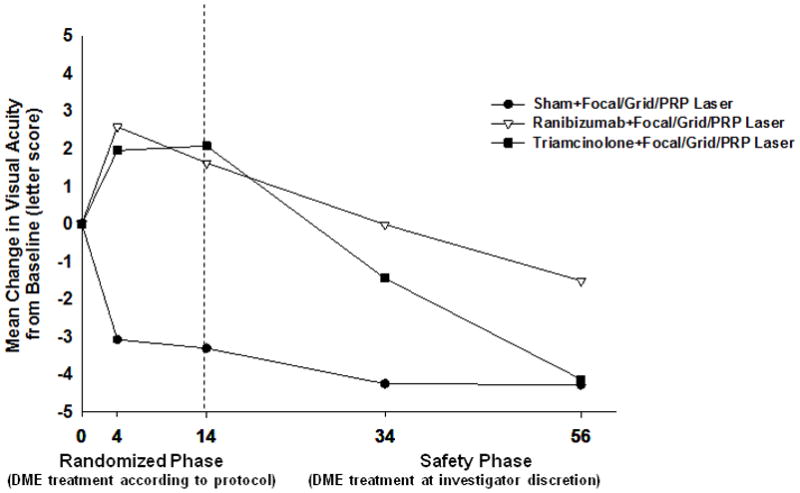
Mean Change in Visual Acuity at Follow-up Visits.
Values that were larger than ± 30 letters were assigned a value of 30. P values for difference in mean change in visual acuity from sham+focal/grid/PRP laser at the 14-week visit: ranibizumab+focal/grid/PRP laser <0.001 and triamcinolone+focal/grid/PRP laser groups <0.001. Fourteen week completed visits include visits that occurred between 70 and 153 days (between 10 and 22 weeks) from randomization. Fifty-six week completed visits include visits that occurred between 315 and 468 days (between 45 and 67 weeks) from randomization.
PRP=Panretinal photocoagulation.
Figure 3.
Distribution of Visual Acuity Change (letters) from Baseline to the 14-Week Visit. Fourteen week completed visits include visits that occurred between 70 and 153 days (between 10 and 22 weeks) from randomization.
PRP=Panretinal photocoagulation.
There were no obvious clinically important differential treatment effects (interactions) at the 14-week primary outcome visit for any of the following subgroups: prior treatment for DME, baseline visual acuity, baseline OCT-measured central subfield thickness, baseline level of diabetic retinopathy, description of edema by the treating ophthalmologist as predominantly focal or predominantly diffuse, PRP in single sitting vs. multiple sittings, or baseline hemoglobin A1c level (Table 5). Fourteen-week primary outcome results were similar to the overall results when excluding all eyes with an imputed baseline central subfield thickness <250 μm (data not shown). There were only 26 study participants with 2 study eyes, precluding any adequate comparison of results in these eyes compared with study participants with only 1 study eye.
Table 5.
Change in Visual Acuity (Last Observation Carried Forward) from Baseline to 14-Week Visit* Among Subgroups
| Subgroup | Change in Visual Acuity Mean±standard deviation | ≥10 Letter Improvement | ≥10 Letter Worsening | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Sham, Ranib, Triam, N | Sham+ Focal/Grid/PRP Laser | Ranibizumab +Focal/Grid/PRP Laser | Triamcinolone +Focal/Grid/PRP Laser | Sham+ Focal/Grid/PRP Laser | Ranibizumab +Focal/Grid/PRP Laser | Triamcinolone +Focal/Grid/PRP Laser | Sham+ Focal/Grid/PRP Laser | Ranibizumab +Focal/Grid/PRP Laser | Triamcinolone + Focal/Grid/PRP Laser | |
| Prior treatment for DME | ||||||||||
| No | 80, 75, 72 | −4±13 | +2±12 | +2±11 | 9% | 20% | 22% | 25% | 9% | 10% |
| Yes | 43, 38, 37 | −5±14 | +1±9 | +3±11 | 7% | 16% | 22% | 19% | 8% | 11% |
| Baseline visual acuity letter score (approximate Snellen equivalent) | ||||||||||
| ≥66 (better than 20/50) | 66, 64, 61 | −5±12 | −1±9 | 0±7 | 0 | 6% | 10% | 24% | 11% | 10% |
| ≤65 (20/50 or worse) | 57, 49, 48 | −2±16 | +4±13 | +5±13 | 18% | 35% | 38% | 21% | 6% | 10% |
| Baseline central subfield thickness | ||||||||||
| <400 μm | 76, 68, 65 | −3±13 | +1±9 | +2±9 | 8% | 15% | 15% | 22% | 6% | 8% |
| ≥400 μm | 46, 44, 42 | −6±15 | +2±14 | +2±12 | 9% | 25% | 31% | 24% | 14% | 14% |
| Diabetic Retinopathy Severity from graded photos | ||||||||||
| NPDR | 37, 26, 21 | −2±10 | 0±10 | −2±8 | 8% | 15% | 10% | 14% | 8% | 14% |
| PDR | 82, 83, 84 | −5±15 | +2±12 | +3±11 | 9% | 20% | 26% | 24% | 10% | 8% |
| Diffuse vs. focal edema as characterized by investigator† | ||||||||||
| Typical/predominantly focal | 37, 19, 27 | −1±12 | 0±16 | +1±10 | 11% | 21% | 7% | 19% | 11% | 7% |
| Neither predominantly focal or diffuse | 18, 25, 14 | −5±14 | +1±6 | −1±8 | 11% | 12% | 0 | 28% | 0 | 14% |
| Typical/predominantly diffuse | 68, 69, 68 | −5±14 | +2±12 | +3±11 | 6% | 20% | 32% | 24% | 12% | 10% |
| Number of PRP sittings performed | ||||||||||
| 1 sitting | 49, 38, 41 | −2±12 | +2±7 | +2±12 | 8% | 8% | 27% | 18% | 3% | 12% |
| multiple sittings | 73, 73, 66 | −5±14 | +1±13 | +2±10 | 8% | 23% | 20% | 26% | 12% | 9% |
| PRP Automated Pattern Used | ||||||||||
| Yes | 36, 21, 21 | −4±12 | +2±13 | 0±10 | 6% | 29% | 24% | 31% | 5% | 14% |
| No | 86, 90, 86 | −4±14 | +1±11 | +3±11 | 9% | 16% | 22% | 20% | 10% | 9% |
| Baseline Hemoglobin A1c | ||||||||||
| <8% | 61, 46, 48 | −3±11 | +3±10 | 0±11 | 7% | 22% | 15% | 16% | 7% | 13% |
| ≥8% | 59, 57, 55 | −6±16 | 0±12 | +4±10 | 7% | 16% | 31% | 31% | 11% | 7% |
DME = diabetic macular edema; Ranib = ranibizumab; Triam = Triamcinolone; NPDR = nonproliferative diabetic retinopathy; PRP = panretinal photocoagulation.
Visits occurring between 70 and 153 days (between 10 and 22 weeks) from randomization were included as 14-week visits. When more than 1 visit occurred in this window, data from the visit closest to the 14-week target date were used. For other eyes without any 14-week data (5 eyes in the sham+focal/grid/PRP laser group, 10 eyes in the ranibizumab+focal/grid/PRP laser group, and 4 eyes in the triamcinolone+focal/grid/PRP laser group) the last observation carried forward method was used to impute data for the primary analysis.
Investigators were asked, ‘If diabetic macular edema (DME) is present, indicate how you would characterize its type, focal vs. diffuse, in your own daily practice. You are free to use, or not use, optical coherence tomography, fluorescein angiograms, and/or fundus photographs in addition to your clinical examination.’
Effect of Treatment on Retinal Thickening through the Primary Outcome (14-week) Visit
In general, treatment group comparisons for mean central subfield thickness paralleled the visual acuity comparisons. Specifically, mean central subfield thickness increased slightly from baseline to the 4-week visit in the sham group (+10 ± 97 μm) and decreased from baseline to the 4-week visit in both the ranibizumab group (−91 ± 161 μm) and triamcinolone group (−106 ± 132 μm) (Figure 4). At the 14-week primary outcome visit, the mean central subfield thickness change from baseline was similar to the 4-week change in the sham (+10 vs. −5 μm) and triamcinolone (−106 μm vs. −92 μm) groups, but the 4-week change in central subfield thickness in the ranibizumab group (−91 μm) apparently worsened 10 weeks after the 4 week injection (−39 μm). Nevertheless, the difference between sham and the 2 treatment groups remained statistically significant for both the ranibizumab (P = 0.01) and the triamcinolone (P < 0.001) groups (Table 6, Figures 4 and 5). More eyes in the sham group (44 eyes [38%]) at 14-weeks had an increase in central subfield thickness ≥ 10% with at least a 25 μm increase from baseline compared with those in the ranibizumab and triamcinolone groups (17 eyes [17%] and 10 eyes [10%], respectively). Of the 44 eyes in the sham group exhibiting a central subfield thickness increase ≥ 10% with at least a 25 μm increase, 15 (34%) had concordant decrease in visual acuity of ≥ 10 letters at 14 weeks, and represented approximately half of the eyes in this group with this amount of visual acuity loss. Similarly, of the 17 eyes in the ranibizumab group and the 10 eyes in the triamcinolone group with a central subfield thickness increase ≥10% and at least a 25 μm increase at 14 weeks, 2 eyes (12%) and 1 eye (10%), respectively, had concordant decreases in visual acuity of ≥10 letters at 14 weeks. OCT retinal volume results at the 14-week visit were similar to those of OCT central subfield thickness (Table 7, available at ###).
Figure 4.
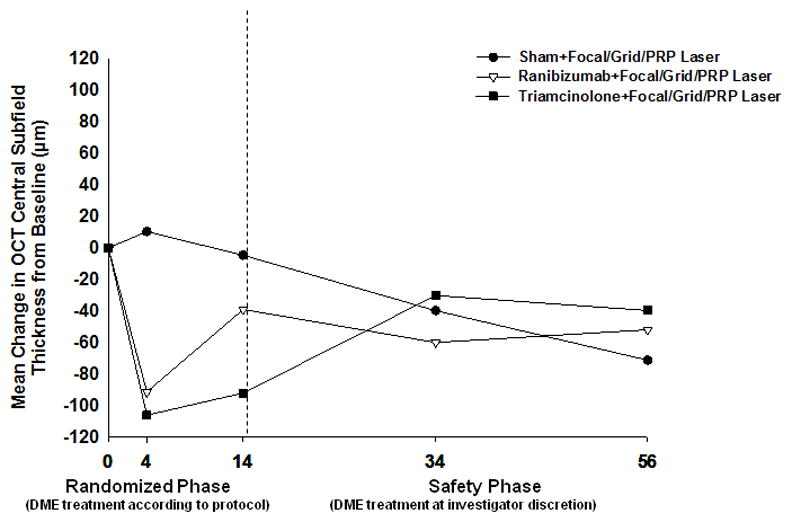
Mean Change in Optical Coherence Tomography Central Subfield Retinal Thickening at Follow-up Visits.
P values for difference in mean change in OCT central subfield retinal thickness from sham+focal/grid/PRP laser at the 14-week visit: ranibizumab+focal/grid/PRP laser = 0.01 and triamcinolone+focal/grid/PRP laser <0.001. Fourteen week completed visits include visits that occurred between 70 and 153 days (between 10 and 22 weeks) from randomization. Fifty-six week completed visits include visits that occurred between 315 and 468 days (between 45 and 67 weeks) from randomization.
OCT = optical coherence tomography; PRP=Panretinal photocoagulation.
Table 6.
Change in Retinal Thickness from Baseline to 14-Week Visit*
| Change in OCT Central Subfield Thickness | Sham+ Focal/Grid/PRP Laser | Ranibizumab+ Focal/Grid/PRP Laser | Triamcinolone+ Focal/Grid/PRP Laser |
|---|---|---|---|
|
| |||
| N = 115 | N = 100 | N = 103 | |
| Overall Change† | |||
| Thickness(μm) Median (25th, 75th percentile) | 362 (287, 484) | 312 (259, 453) | 265 (230, 304) |
| Change from baseline (μm) Mean±standard deviation | −5±113 | −39±127 | −92±115 |
| Change from baseline (μm) Median (25th, 75th percentile) | 0 (−80, +70) | −26 (−92, +15) | −75 (−168, −17) |
| Difference in mean change from sham+focal/grid/PRP laser (95% CI) [P Value] ‡ | −35 (−64, −6) [P = 0.007] |
−100 (−128, −71) [P < 0.001] |
|
| Thickness ≥10% increase with at least a 25 μm increase from baseline, no. (%) | 44 (38%) | 17 (17%) | 10 (10%) |
| Relative risk (95% CI) [P Value] ‡ for comparison with sham+focal/grid/PRP laser | 1.0 | 0.44 (0.25, 0.79) [P = 0.002] |
0.24 (0.12, 0.48) [P < 0.001] |
| Thickness <250 with at least a 25 μm decrease from baseline, no. (%) | 12 (10%) | 17 (17%) | 28 (27%) |
| Relative risk (95% CI) [P Value] ‡ for comparison with sham+focal/grid/PRP laser | 1.0 | 2.07 (0.96, 4.47) [P = 0.04] |
3.15 (1.56, 6.36) [P < 0.001] |
| LogOCT, no (%) || | |||
| Two or more step improvement | 9 (8%) | 12 (12%) | 28 (27%) |
| At least 1, but less than 2 step improvement | 17 (15%) | 20 (20%) | 27 (26%) |
| Less than 1 step improvement and less than 1 step worsening | 67 (58%) | 58 (58%) | 45 (44%) |
| At least 1 step but less than 2 step worsening | 18 (16%) | 7 (7%) | 2 (2%) |
| Two or more step worsening | 4 (3%) | 3 (3%) | 1 (1%) |
|
| |||
| Baseline thickness <400 μm | N = 73 | N = 60 | N = 64 |
|
| |||
| Thickness(μm) Median (25th, 75th percentile) | 315 (254, 377) | 273 (246, 320) | 255 (225, 282) |
| Change from baseline (μm) Mean±standard deviation | +31±95 | −12±70 | −35±71 |
| Change from baseline (μm) Median (25th, 75th percentile) | +28 (−20, +93) | −9 (−61, +15) | −23 (−78, +11) |
| Thickness ≥10% increase with at least a 25 μm increase from baseline, no. (%) | 35 (48%) | 10 (17%) | 8 (13%) |
| Thickness <250 with at least a 25 μm decrease from baseline | 11 (15%) | 14 (23%) | 18 (28%) |
| LogOCT, no. (%) || | |||
| Two or more step improvement | 4 (5%) | 3 (5%) | 7 (11%) |
| At least 1, but less than 2 step improvement | 6 (8%) | 12 (20%) | 14 (22%) |
| Less than 1 step improvement and less than 1 step worsening | 42 (58%) | 40 (67%) | 40 (63%) |
| At least 1 step but less than 2 step worsening | 17 (23%) | 4 (7%) | 2 (3%) |
| Two or more step worsening | 4 (5%) | 1 (2%) | 1 (2%) |
|
| |||
| Baseline thickness ≥400 μm | N = 42 | N = 40 | N = 39 |
|
| |||
| Thickness(μm) Median (25th, 75th percentile) | 498 (395, 570) | 469 (369, 547) | 293 (247, 391) |
| Change from baseline (μm) Mean±standard deviation | −67±116 | −80±175 | −186±111 |
| Change from baseline (μm) Median (25th, 75th percentile) | −77 (−171, +37) | −81 (−184, −4) | −193 (−246, −132) |
| Thickness ≥10% increase with at least a 25 μm increase from baseline, no. (%) | 9 (21%) | 7 (18%) | 2 (5%) |
| Thickness <250 with at least a 25 μm decrease from baseline | 1 (2%) | 3 (8%) | 10 (26%) |
| LogOCT, no. (%) || | |||
| Two or more step improvement | 5 (12%) | 9 (23%) | 21 (54%) |
| At least 1, but less than 2 step improvement | 11 (26%) | 8 (20%) | 13 (33%) |
| Less than 1 step improvement and less than 1 step worsening | 25 (60%) | 18 (45%) | 5 (13%) |
| At least 1 step but less than 2 step worsening | 1 (2%) | 3 (8%) | 0 |
| Two or more step worsening | 0 | 2 (5%) | 0 |
Visits occurring between 70 and 153 days (between 10 and 22 weeks) from randomization were included as 14-week visits. When more than 1 visit occurred in this window, data from the visit closest to the 14-week target date were used.
Missing (or ungradeable) data as follows for the sham+focal/grid/PRP laser group, ranibizumab+focal/grid/PRP laser group, and triamcinolone+focal/grid/PRP laser groups, respectively: 3, 3, and 2.
Adjusted for baseline optical coherence tomography (OCT) retinal thickness and visual acuity, number of planned panretinal photocoagulation (PRP) sittings, and correlation between 2 study eyes. Confidence intervals (CI) are adjusted for multiple comparisons.
Logarithmic transformation of OCT central subfield thickness (LogOCT) is calculated by taking the log base 10 of the ratio of the central subfield thickness divided by 200 and rounding to the nearest hundredth. The change is the change in the log values.
Figure 5.
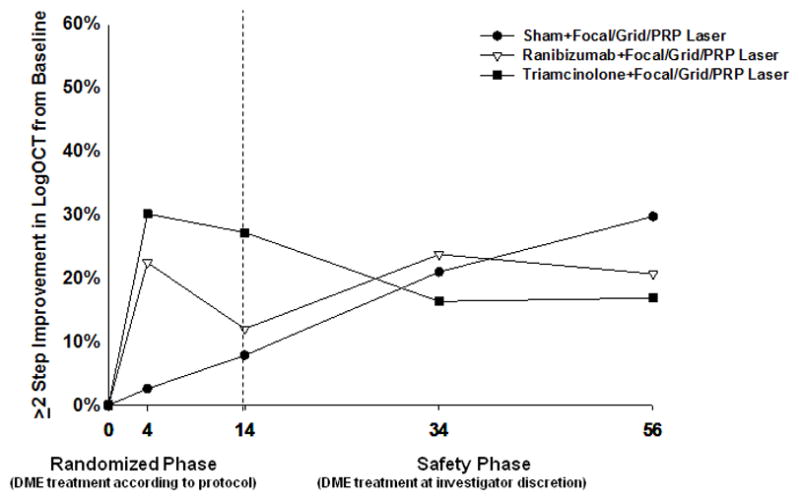
Two or More Step Improvement in the Logarithmic Transformation of Optical Coherence Tomography Central Subfield Thickness from Baseline.
Fourteen week completed visits include visits that occurred between 70 and 153 days (between 10 and 22 weeks) from randomization. Fifty-six week completed visits include visits that occurred between 315 and 468 days (between 45 and 67 weeks) from randomization.
logOCT = logarithmic transformation of optical coherence tomography calculated by taking the log base 10 of the ratio of the central subfield thickness divided by 200 and rounded to the nearest hundredth.
DME=Diabetic macular edema; PRP=Panretinal photocoagulation.
Table 7.
Change in Optical Coherence Tomography Retinal Volume from Baseline to 14-Week Visit*
| Change in OCT Retinal Volume† | Sham+ Focal/Grid/PRP Laser | Ranibizumab+ Focal/Grid/PRP Laser | Triamcinolone+ Focal/Grid/PRP Laser |
|---|---|---|---|
|
| |||
| N = 69 | N = 66 | N = 66 | |
| Total volume (mm3) at 14 weeks | |||
| Mean±standard deviation | 9.7±1.8 | 9.3±1.9 | 7.9±1.0 |
| Median (25th, 75th percentile) | 9.6 (8.4, 10.6) | 8.8 (7.9, 10.3) | 7.7 (7.3, 8.4) |
| Change in volume (mm3) from baseline † | |||
| Mean±standard deviation | +0.1±1.1 | −0.4±1.3 | −1.3±1.3 |
| Median (25th, 75th percentile) | +0.2 (−0.4, +0.5) | −0.2 (−1.1, +0.2) | −1.3 (−2.1, −0.2) |
| Difference in mean change from sham+focal/grid/PRP laser (95% CI) [P Value] ‡ | −0.6 (−1.0, −0.2) [P = 0.001] |
−1.7 (−2.1, −1.3) [P<0.001] |
|
Visits occurring between 70 and 153 days (between 10 and 22 weeks) from randomization were included as 14-week visits. When more than 1 visit occurred in this window, data from the visit closest to the 14-week target date were used.
Missing (or ungradeable) data as follows for the sham+focal/grid/PRP laser, ranibizumab+focal/grid/PRP laser, and triamcinolone+focal/grid/PRP laser groups respectively: 49, 37, and 39.
Adjusted for baseline optical coherence tomography (OCT) retinal volume, OCT retinal thickness and visual acuity, number of planned panretinal photocoagulation (PRP) sittings, and correlation between 2 study eyes. Confidence intervals (CI) are adjusted for multiple comparisons.
Evaluations of Visual Acuity and Retinal Thickening at the 56-Week Study Safety Visit
The study was not designed to evaluate effectiveness of either intravitreal ranibizumab or intravitreal triamcinolone on visual acuity or retinal thickening beyond the 14-week study visit. The originally randomly assigned treatments were specified only during the first 14 weeks with other treatments commonly observed thereafter, especially in the sham group. Evaluations at the 34- and 56-week study visit are provided only asfor the purposes of longer-term safety information. By the 56-week study visit (Table 8, Figure 2), the mean change ± SD in the visual acuity letter score from baseline was −6±17 in the sham group, −4±21 in the ranibizumab group (P = 0.44 compared with the sham group), and −5±16 in the triamcinolone group (P=0.63 compared with the sham group). By the 56-week study visit (Table 9, Figures 4 and 5), the mean change ± SD in the central subfield thickness from baseline was −71±156 in the sham group, −52±227 in the ranibizumab group (P = 0.25 compared with the sham group), and −40±138 in the triamcinolone group (P = 0.45 compared with the sham group). Mean change in volume from baseline paralleled the mean change in central subfield thickness from baseline to the 56-week study visit (data not shown).
Table 8.
Change in Visual Acuity from Baseline to 56-Week Visit*
| Sham+ Focal/Grid/PRP Laser | Ranibizumab+ Focal/Grid/PRP Laser | Triamcinolone+ Focal/Grid/PRP Laser | |
|---|---|---|---|
|
| |||
| N = 111 | N = 95 | N = 93 | |
| Change in visual acuity (letter score) | |||
| Mean±standard deviation | −6±17 | −4±21 | −5±16 |
| Median (25th, 75th percentile) | −3 (−11, +4) | +1 (−12, +8) | −3 (−12, +3) |
| Difference in mean change from sham+focal/grid/PRP laser (95% CI) [P Value]† | +1.9 (−3.7, +7.5) [P = 0.44] |
+1.2 (−4.4, +6.8) [P = 0.63] |
|
| Distribution of change, no. (%) | |||
| ≥15 letter improvement | 6 (5%) | 12 (13%) | 7 (8%) |
| 14–10 letter improvement | 9 (8%) | 10 (11%) | 5 (5%) |
| 9–5 letter improvement | 9 (8%) | 12 (13%) | 8 (9%) |
| Same ±4 letters | 39 (35%) | 27 (28%) | 31 (33%) |
| 5–9 letters worse | 16 (14%) | 8 (8%) | 14 (15%) |
| 10–14 letters worse | 8 (7%) | 8 (8%) | 8 (9%) |
| ≥15 letters worse | 24 (22%) | 18 (19%) | 20 (22%) |
| Difference in proportion with ≥10 letter improvement from sham+ focal/grid/PRP laser (95% CI)‡ | +8% (−4%, +20%) | +0.2% (−10%, +10%) | |
| Relative risk (95% CI) [P Value]† for comparison with sham+focal/grid/PRP laser |
1.0 | 2.00 (1.04, 3.87) [P = 0.02] |
1.22 (0.57, 2.63) [P = 0.55] |
| Difference in proportion with ≥10 letter worsening from sham+focal/grid/PRP laser (95% CI)‡ | −1% (−15%, +13%) | +2% (−13%, +16%) | |
| Relative risk (95% CI) [P Value]† for comparison with sham+focal/grid/PRP laser |
1.0 | 0.95 (0.58, 1.55) [P = 0.82] |
1.04 (0.64, 1.69) [P = 0.85] |
Visits occurring between 315 and 468 days (between 45 and 67 weeks) from randomization were included as 56-week visits. When more than 1 visit occurred in this window, data from the visit closest to the 56-week target date were used.
Adjusted for baseline visual acuity, number of planned panretinal photocoagulation (PRP) sittings, and correlation between 2 study eyes. Confidence intervals (CI) are adjusted for multiple comparisons.
Adjusted for correlation between 2 study eyes. Confidence intervals are adjusted for multiple comparisons.
Table 9.
Change in Retinal Thickness from Baseline to 56-Week Visit*
| Change in OCT Central Subfield Thickness | Sham+ Focal/Grid/PRP Laser | Ranibizumab+ Focal/Grid/PRP Laser | Triamcinolone+ Focal/Grid/PRP Laser |
|---|---|---|---|
|
| |||
| N = 101 | N = 92 | N = 89 | |
| Overall Change† | |||
| Thickness(μm) Median (25th, 75th percentile) | 282 (225, 352) | 297 (239, 390) | 288 (248, 400) |
| Change from baseline (μm) Mean±standard deviation | −71±156 | −52±227 | −40±138 |
| Change from baseline (μm) Median (25th, 75th percentile) | −45 (−179, +33) | −53 (−150, +20) | −34 (−128, +41) |
| Difference in mean change from sham+focal/grid/PRP laser (95% CI) [P Value] ‡ | +22 (−22, +66) [P = 0.25] |
+15 (−30, +60) [P = 0.45] |
|
| Thickness ≥10% increase with at least a 25 μm increase from baseline, no. (%) | 28 (28%) | 18 (20%) | 25 (28%) |
| Relative risk (95% CI) [P Value] ‡ for comparison with sham+focal/grid/PRP laser | 1.0 | 0.74 (0.42, 1.31) [P = 0.24] |
0.97 (0.58, 1.62) [P = 0.91] |
| Thickness <250 with at least a 25 μm decrease from baseline, no. (%) | 27 (27%) | 27 (29%) | 18 (20%) |
| Relative risk (95% CI) [P Value] ‡ for comparison with sham+focal/grid/PRP laser | 1.0 | 1.13 (0.68, 1.87) [P = 0.60] |
0.76 (0.42, 1.36) [P = 0.29] |
| LogOCT, no (%) || | |||
| Two or more step improvement | 30 (30%) | 19 (21%) | 15 (17%) |
| At least 1, but less than 2 step improvement | 15 (15%) | 25 (27%) | 19 (21%) |
| Less than 1 step improvement and less than 1 step worsening | 42 (42%) | 34 (37%) | 41 (46%) |
| At least 1 step but less than 2step worsening | 9 (9%) | 7 (8%) | 9 (10%) |
| Two or more step worsening | 5 (5%) | 7 (8%) | 5 (6%) |
Visits occurring between 315 and 468 days (between 45 and 67 weeks) from randomization were included as 56-week visits. When more than 1 visit occurred in this window, data from the visit closest to the 56-week target date were used.
Missing (or ungradeable) data as follows for the sham+focal/grid/PRP laser group, ranibizumab+focal/grid/PRP laser group, and triamcinolone+focal/grid/PRP laser group, and respectively: 10, 3, 4.
Adjusted for baseline optical coherence tomography (OCT) retinal thickness and visual acuity, number of planned panretinal photocoagulation (PRP) sittings, and correlation between 2 study eyes. Confidence intervals (CI) are adjusted for multiple comparisons.
Logarithmic transformation of OCT central subfield thickness (LogOCT) is calculated by taking the log base 10 of the ratio of the central subfield thickness divided by 200 and rounding to the nearest hundredth. The change is the change in the log values.
Major Ocular Adverse Events
Major ocular adverse events are summarized in Table 10. One (0.9%, 95% CI: 0.02% to 4.7%) of 116 study eyes (0.4% of 227 intravitreal injections) in the ranibizumab group had endophthalmitis with a visual acuity letter score (approximate Snellen equivalent) of 39 (20/160) at the 56-week visit. Three eyes (2%) in the sham group, 1 eye (<1%) in the ranibizumab group, and 1 eye (<1%) in the triamcinolone group had a tractional retinal detachment by the 14-week visit. Four eyes (3%) in the sham group, 5 eyes (5%) in the ranibizumab group, and 1 eye (<1%) in the triamcinolone group developed a tractional retinal detachment afterwards.
Table 10.
Major Ocular Adverse Events during Follow-Up
| Sham+ Focal/Grid/PRP Laser | Ranibizumab+ Focal/Grid/PRP Laser | Triamcinolone+ Focal/Grid/PRP Laser | |
|---|---|---|---|
| Up to 14 week visit | N = 133 |
N = 116 # injections = 227 |
N = 115 # injections = 115 |
| Endophthalmitis, no. (%)* | 0 | 1 (0.9%) | 0 |
| Ocular vascular event, no. (%) | 0 | 0 | 0 |
| Retinal detachment†, no. (%) | 4 (3%) | 1 (1%) | 1 (1%) |
| Vitrectomy‡, no. (%) | 1 (1%) | 0 | 1 (1%) |
| Vitreous hemorrhage, no. (%) | 16 (12%) | 6 (5%) | 7 (6%) |
| Elevated IOP/glaucoma, no. (%) | |||
| Increase ≥10 mmHg from baseline | 3 (2%) | 0 | 20 (17%) |
| IOP ≥30 mmHg | 2 (2%) | 0 | 5 (4%) |
| Initiation of IOP-lowering medication at any visit|| | 2 (2%) | 0 | 2 (2%) |
| Number of eyes meeting one or more of the above | 3 (2%) | 0 | 20 (17%) |
| Glaucoma surgery | 0 | 0 | 0 |
| Cataract Surgery | |||
| Phakic at baseline | N = 120 | N = 93 | N = 105 |
| No. (%) with cataract surgery | 0 | 0 | 0 |
|
| |||
| After 14 to 56 week visit | N = 131 | N = 111 | N = 112 |
| Endophthalmitis, no. (%) | 0 | 0 | 0 |
| Ocular vascular event, no. (%) | 0 | 0 | 0 |
| Retinal detachment†, no. (%) | 4 (3%) | 5 (5%) | 1 (1%) |
| Vitrectomy‡, no. (%) | 17 (13%) | 8 (7%) | 7 (6%) |
| Vitreous hemorrhage, no. (%) | 28 (21%) | 25 (23%) | 20 (18%) |
| Elevated IOP/glaucoma, no. (%) | |||
| Increase ≥10 mmHg from baseline | 6 (5%) | 6 (5%) | 10 (9%) |
| IOP ≥30 mmHg | 4 (3%) | 4 (4%) | 4 (4%) |
| Initiation of IOP-lowering medication at any visit after the 14-week visit | 7 (5%) | 5 (5%) | 17 (15%) |
| Number of eyes meeting one or more of the above | 11 (8%) | 7 (6%) | 20 (18%) |
| IOP-lowering medication at 56 visit | 3 (2%) | 4 (4%) | 9 (9%) |
| Glaucoma surgery § | 0 | 1 (1%) | 1 (1%) |
| Cataract Surgery | |||
| Phakic at 14 weeks | N = 119 | N = 91 | N = 102 |
| No. (%) with cataract surgery | 2 (2%) | 3 (3%) | 6 (6%) |
PRP=panretinal photocoagulation.
One case related to study drug injection in the ranibizumab+focal/grid/PRP laser group.
All had tractional detachment except two eyes had unspecified retinal detachment (one by 14-week visit and one after 14-week visit)
All were for PDR
Excludes eyes with intraocular pressure (IOP) lowering medications at baseline.
Includes 2 Ahmed valve (neovascular glaucoma).
Up to the 14-week visit, 16 eyes (12%) in the sham group, compared with 6 eyes (5%) and 7 eyes (6%) in the ranibizumab and triamcinolone groups, respectively, had a vitreous hemorrhage. Among eyes with vitreous hemorrhage, 9 eyes (56%), 2 eyes (40%), and 1 eye (14%) worsened ≥10 letters from baseline to 14-week visit in the sham, ranibizumab, and triamcinolone groups, respectively. Vitrectomy for PDR (which included 5 eyes which developed a tractional retinal detachment) was performed by the 56-week visit in 18 eyes (15%) in the sham group, 8 eyes (7%) in the ranibizumab group, and 7 eyes (6%) in the triamcinolone group, including 1 eye (<1%) in the sham group, no eyes in the ranibizumab group, and 1 eye (<1%) in the triamcinolone group prior to the 14-week visit. The occurrence of adverse events related to IOP was more frequent in eyes in the triamcinolone group than in the ranibizumab or sham groups (Table 10).
Systemic Adverse Events
There were no systemic adverse events with a difference in frequency among the 3 groups that could not be attributed to chance however, there were 4 (4%) cardiovascular or cerebrovascular events, as defined by the Antiplatelet Trialists’ Collaboration,25 in the sham group compared with 8 (7%) in the ranibizumab group (P=0.33) and 4 (3%) in the triamcinolone group (P=0.86). In the ranibizumab group, 1 event occurred approximately 5 weeks after randomization, between baseline and the second ranibizumab injection, 1 event occurred approximately 3 weeks after the 4 week injection, and the events for the remaining 6 study participants occurred more than 4 weeks after the 4-week injection (Table 11 and Figure 6). There were no differences in frequency of Antiplatelet Trialists’ Collaboration events between ranibizumab and sham or triamcinolone groups when stratified by prior history of cardiovascular events. All reported systemic adverse events and study eye ocular adverse events are shown in Tables 12 (available at ###) and Table 13 (available at ###).
Table 11.
Antiplatelet Trialists’ Collaboration* Events through 56-Week Visit
| Sham+ Focal/Grid/PRP Laser N† = 102 |
Ranibizumab+ Focal/Grid/PRP Laser N† = 116 |
Triamcinolone+ Focal/Grid/PRP Laser N† = 115 |
|
|---|---|---|---|
| Non-fatal myocardial infarction, no. (%) | 1 (1%) | 3 (3%) | 0 |
| Non-fatal cerebrovascular accident – ischemic or hemorrhagic (or unknown), no. (%) | 1 (1%) | 3 (3%) | 4 (3%) |
| Vascular death (from any potential vascular or unknown cause), no. (%) | 2 (2%) | 3 (3%) | 0 |
| Any APTC event, no. (%) | 4 (4%) | 8§ (7%) | 4 (3%) |
|
| |||
| Participants with prior cardiovascular events|| | N=19 | N=37 | N=30 |
| Any APTC event, no. (%) | 1 (5%) | 3 (8%) | 0 |
| Participants without prior cardiovascular events | N=83 | N=79 | N=85 |
| Any APTC event, no. (%) | 3 (4%) | 5 (6%) | 4 (5%) |
Antiplatelet Trialists’ Collaboration. BMJ. 1994 Jan 8;308(6921):81–106.
PRP=Panretinal photocoagulation; APTC= Antiplatelet Trialists’ Collaboration.
N = Number of Study Participants. Study participants with 2 study eyes are assigned to the non-sham group. Multiple events within a study participant are only counted once per event.
1event occurred between baseline and 4 week injections, 1 event occurred approximately 3 weeks after the 4- week injection, and other events from the remaining 6 study participants occurred over 4 weeks after the 4-week injection.
According to participant reported history.
Figure 6.
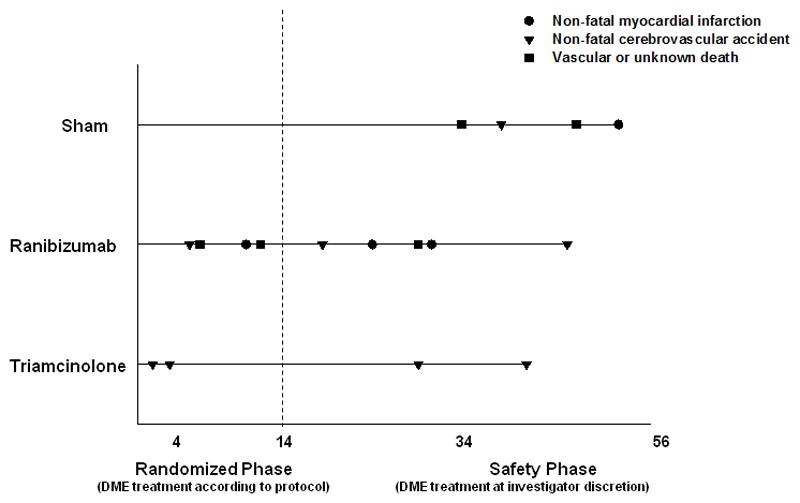
Cardiovascular Events According to the Antiplatelet Trialists’ Collaboration* through 56-Week Visit.
*Antiplatelet Trialists’ Collaboration. BMJ. 1994 Jan 8;308(6921):81–106.
Non-fatal cerebrovascular accidents include ischemic, hemorrhagic or unknown. Vascular death includes any potential vascular or unknown cause.
DME=Diabetic macular edema.
Table 12.
Summary of all Systemic Adverse Events through 56-Week Visit of Follow-up*
| Sham +Focal/Grid/PRP Laser | Ranibizumab+ Focal/Grid/PRP Laser | Triamcinolone +Focal/Grid/PRP Laser | Ranibizumab/Sham** | Triamcinolone/Sham** | |
|---|---|---|---|---|---|
|
| |||||
| Total Number of Events | N = 128 | N = 178 | N = 168 | N = 44 | N = 39 |
| Blood and lymphatic system disorders | |||||
| Anaemia | 4 | 1 | 5 | 0 | 1 |
| Anaemia of chronic disease | 0 | 1 | 0 | 0 | 0 |
| Lymphadenopathy | 1 | 0 | 0 | 0 | 0 |
| Lymphoedema | 1 | 0 | 0 | 0 | 0 |
| Lymphoma | 1 | 0 | 0 | 0 | 0 |
| Cardiac disorders | |||||
| Angina pectoris | 0 | 1 | 1 | 0 | 0 |
| Arteriosclerosis coronary artery | 1 | 1 | 0 | 0 | 0 |
| Atrial flutter | 0 | 1 | 0 | 0 | 0 |
| Cardiac failure | 2 | 0 | 0 | 0 | 0 |
| Cardiac failure congestive | 1 | 6 | 3 | 0 | 1 |
| Cardiomegaly | 0 | 0 | 0 | 1 | 0 |
| Chest discomfort | 1 | 0 | 0 | 0 | 0 |
| Coronary artery disease | 0 | 1 | 2 | 0 | 0 |
| Coronary artery occlusion | 1 | 0 | 0 | 0 | 0 |
| Ischaemic cardiomyopathy | 0 | 1 | 0 | 0 | 0 |
| Myocardial infarction | 1 | 4 | 0 | 0 | 0 |
| Palpitations | 0 | 0 | 1 | 0 | 0 |
| Tachycardia | 1 | 0 | 0 | 0 | 1 |
| Ear and labyrinth disorders | |||||
| Ear pain | 0 | 1 | 0 | 0 | 0 |
| Otitis externa | 0 | 0 | 0 | 0 | 1 |
| Endocrine disorders | |||||
| Diabetes mellitus | 0 | 0 | 2 | 1 | 0 |
| Diabetes mellitus inadequate control | 0 | 1 | 1 | 0 | 0 |
| Diabetic gastroparesis | 1 | 1 | 2 | 0 | 0 |
| Diabetic ulcer | 1 | 0 | 0 | 0 | 0 |
| Hyperglycaemia | 1 | 2 | 0 | 0 | 0 |
| Hyperthyroidism | 0 | 0 | 0 | 0 | 1 |
| Hypoglycaemia | 2 | 3 | 1 | 0 | 0 |
| Hypothyroidism | 0 | 2 | 1 | 0 | 0 |
| Gastrointestinal disorders | |||||
| Abdominal pain | 0 | 0 | 4 | 0 | 0 |
| Abdominal pain upper | 0 | 0 | 2 | 0 | 0 |
| Appendiceal abscess | 1 | 0 | 0 | 0 | 0 |
| Appendicitis | 2 | 0 | 0 | 0 | 0 |
| Constipation | 0 | 0 | 3 | 0 | 0 |
| Diarrhoea | 1 | 1 | 0 | 3 | 0 |
| Diverticulum | 0 | 0 | 2 | 0 | 0 |
| Dysgeusia | 0 | 0 | 1 | 0 | 0 |
| Dyspepsia | 0 | 1 | 0 | 0 | 1 |
| Dysphagia | 0 | 0 | 1 | 0 | 0 |
| Faecaloma | 0 | 1 | 0 | 0 | 0 |
| Gastrooesophageal reflux disease | 1 | 2 | 2 | 0 | 1 |
| Impaired gastric emptying | 1 | 0 | 0 | 0 | 0 |
| Intestinal obstruction | 1 | 0 | 0 | 0 | 0 |
| Nausea | 4 | 4 | 6 | 0 | 1 |
| Oesophageal varices haemorrhage | 0 | 0 | 0 | 1 | 0 |
| Pancreatitis | 0 | 0 | 1 | 0 | 0 |
| Peptic ulcer | 0 | 0 | 1 | 0 | 0 |
| Rectal haemorrhage | 0 | 1 | 0 | 0 | 0 |
| Tooth infection | 0 | 0 | 1 | 0 | 0 |
| Vomiting | 1 | 1 | 5 | 0 | 0 |
| General disorders and administration site conditions | |||||
| Chest pain | 0 | 7 | 0 | 0 | 3 |
| Cyst | 2 | 0 | 0 | 0 | 0 |
| Death | 3 | 2 | 1 | 0 | 0 |
| Hernia | 0 | 0 | 2 | 0 | 0 |
| Oedema peripheral | 0 | 1 | 1 | 0 | 1 |
| Pyrexia | 1 | 0 | 1 | 0 | 1 |
| Swelling | 0 | 1 | 0 | 0 | 0 |
| Hepatobiliary disorders | |||||
| Cholelithiasis | 0 | 0 | 1 | 0 | 0 |
| Immune system disorders | |||||
| Asthma | 0 | 0 | 0 | 1 | 0 |
| Drug hypersensitivity | 0 | 1 | 0 | 0 | 0 |
| Hypersensitivity | 0 | 1 | 0 | 0 | 0 |
| Seasonal allergy | 1 | 0 | 1 | 0 | 0 |
| Infections and infestations | |||||
| Bronchitis | 0 | 1 | 1 | 0 | 1 |
| Bronchopneumonia | 0 | 0 | 1 | 0 | 0 |
| Candidiasis | 1 | 0 | 0 | 0 | 0 |
| Cystitis | 1 | 0 | 0 | 0 | 0 |
| Gangrene | 0 | 0 | 0 | 1 | 0 |
| Gastroenteritis | 0 | 1 | 2 | 0 | 0 |
| Gastroenteritis viral | 2 | 1 | 0 | 0 | 0 |
| Infection | 2 | 0 | 1 | 0 | 0 |
| Influenza | 1 | 3 | 1 | 0 | 1 |
| Localised infection | 3 | 2 | 4 | 0 | 1 |
| Onychomycosis | 0 | 0 | 1 | 0 | 0 |
| Osteomyelitis | 1 | 1 | 1 | 0 | 0 |
| Pharyngitis | 1 | 0 | 0 | 0 | 0 |
| Pneumonia | 1 | 4 | 3 | 0 | 1 |
| Respiratory tract infection | 1 | 0 | 0 | 0 | 0 |
| Sepsis | 0 | 0 | 0 | 0 | 1 |
| Sinusitis | 1 | 1 | 2 | 0 | 1 |
| Skin bacterial infection | 0 | 0 | 0 | 1 | 0 |
| Skin infection | 1 | 0 | 1 | 2 | 0 |
| Streptococcal infection | 0 | 0 | 0 | 0 | 1 |
| Tinea pedis | 0 | 1 | 0 | 0 | 0 |
| Upper respiratory tract infection | 2 | 0 | 4 | 1 | 2 |
| Urinary tract infection | 3 | 1 | 1 | 2 | 1 |
| Injury, poisoning and procedural complications | |||||
| Animal bite | 0 | 1 | 0 | 0 | 0 |
| Burns second degree | 0 | 1 | 0 | 0 | 0 |
| Fall | 3 | 0 | 3 | 0 | 0 |
| Fibula fracture | 0 | 0 | 0 | 1 | 0 |
| Foot fracture | 0 | 2 | 2 | 0 | 0 |
| Head injury | 0 | 0 | 1 | 0 | 0 |
| Hip fracture | 1 | 0 | 0 | 0 | 0 |
| Injury | 1 | 0 | 0 | 0 | 0 |
| Joint injury | 1 | 0 | 0 | 0 | 0 |
| Laceration | 1 | 0 | 0 | 0 | 0 |
| Limb injury | 1 | 2 | 0 | 0 | 0 |
| Road traffic accident | 0 | 0 | 0 | 0 | 1 |
| Subdural haematoma | 0 | 0 | 0 | 1 | 0 |
| Thermal burn | 0 | 2 | 1 | 0 | 0 |
| Upper limb fracture | 0 | 0 | 1 | 0 | 0 |
| Wrist fracture | 0 | 0 | 1 | 0 | 0 |
| Investigations | |||||
| Blood glucose decreased | 1 | 0 | 0 | 0 | 0 |
| Blood potassium increased | 0 | 1 | 0 | 0 | 0 |
| Heart rate decreased | 0 | 1 | 0 | 0 | 0 |
| Oxygen saturation decreased | 0 | 1 | 0 | 0 | 0 |
| Metabolism and nutrition disorders | |||||
| Dehydration | 0 | 1 | 1 | 0 | 0 |
| Diabetes mellitus inadequate control | 1 | 1 | 3 | 0 | 0 |
| Dyslipidaemia | 1 | 1 | 1 | 2 | 0 |
| Fluid overload | 1 | 0 | 1 | 0 | 0 |
| Fluid retention | 0 | 0 | 0 | 1 | 0 |
| Hypercholesterolaemia | 3 | 5 | 3 | 1 | 0 |
| Hyperkalaemia | 2 | 2 | 0 | 0 | 0 |
| Hyperlipidaemia | 0 | 1 | 1 | 0 | 0 |
| Hypocalcaemia | 1 | 0 | 0 | 0 | 0 |
| Hypokalaemia | 0 | 0 | 0 | 1 | 0 |
| Hypomagnesaemia | 0 | 1 | 0 | 0 | 0 |
| Hyponatraemia | 0 | 1 | 0 | 0 | 0 |
| Vitamin D deficiency | 0 | 0 | 1 | 0 | 1 |
| Musculoskeletal and connective tissue disorders | |||||
| Arthralgia | 1 | 2 | 0 | 1 | 0 |
| Back pain | 1 | 1 | 1 | 1 | 0 |
| Hand fracture | 0 | 0 | 1 | 0 | 0 |
| Joint sprain | 0 | 0 | 1 | 0 | 0 |
| Multiple fractures | 0 | 0 | 1 | 0 | 0 |
| Muscle spasms | 0 | 0 | 3 | 0 | 0 |
| Musculoskeletal pain | 0 | 0 | 1 | 0 | 0 |
| Myalgia | 2 | 0 | 0 | 0 | 0 |
| Neck pain | 0 | 0 | 1 | 0 | 0 |
| Osteoarthritis | 0 | 0 | 0 | 1 | 0 |
| Pain in extremity | 0 | 0 | 3 | 0 | 1 |
| Pelvic fracture | 0 | 1 | 0 | 0 | 0 |
| Periarthritis | 1 | 0 | 0 | 0 | 0 |
| Rheumatoid arthritis | 0 | 0 | 1 | 0 | 0 |
| Rib fracture | 1 | 0 | 0 | 0 | 0 |
| Neoplasms benign, malignant and unspecified (incl cysts and polyps) | |||||
| Bladder cancer | 0 | 1 | 0 | 0 | 0 |
| Meningioma | 0 | 1 | 0 | 0 | 0 |
| Skin cancer | 0 | 1 | 1 | 0 | 0 |
| Nervous system disorders | |||||
| Carotid artery occlusion | 0 | 0 | 0 | 0 | 1 |
| Carpal tunnel syndrome | 1 | 1 | 0 | 0 | 0 |
| Cerebrovascular accident | 1 | 3 | 2 | 0 | 1 |
| Convulsion | 0 | 1 | 1 | 0 | 0 |
| Dysarthria | 0 | 1 | 0 | 0 | 0 |
| Facial palsy | 0 | 1 | 0 | 0 | 0 |
| Headache | 6 | 9 | 4 | 6 | 3 |
| Hypoaesthesia oral | 0 | 0 | 1 | 0 | 0 |
| Insomnia | 0 | 1 | 0 | 2 | 0 |
| Ischaemic stroke | 0 | 0 | 1 | 0 | 0 |
| Neuropathy peripheral | 0 | 1 | 0 | 0 | 0 |
| Restless legs syndrome | 0 | 0 | 1 | 0 | 0 |
| Somnolence | 0 | 0 | 1 | 0 | 0 |
| Syncope | 0 | 1 | 0 | 0 | 0 |
| Syncope vasovagal | 0 | 0 | 1 | 2 | 0 |
| Tinnitus | 0 | 0 | 1 | 0 | 0 |
| Tremor | 0 | 2 | 0 | 0 | 0 |
| Vertigo | 0 | 1 | 0 | 0 | 0 |
| Psychiatric disorders | |||||
| Anxiety | 2 | 4 | 0 | 0 | 1 |
| Depression | 2 | 4 | 1 | 1 | 0 |
| Hallucination | 0 | 1 | 0 | 0 | 0 |
| Insomnia | 0 | 0 | 1 | 0 | 0 |
| Mental disorder | 0 | 1 | 0 | 0 | 0 |
| Renal and urinary disorders | |||||
| Haematuria | 1 | 0 | 2 | 0 | 0 |
| Nephropathy | 1 | 0 | 0 | 0 | 0 |
| Neurogenic bladder | 1 | 0 | 0 | 0 | 0 |
| Obstructive uropathy | 0 | 1 | 0 | 0 | 0 |
| Pelvic pain | 1 | 0 | 0 | 0 | 0 |
| Renal disorder | 0 | 0 | 1 | 0 | 0 |
| Renal failure | 2 | 4 | 2 | 0 | 0 |
| Renal failure acute | 2 | 1 | 0 | 0 | 0 |
| Renal failure chronic | 2 | 1 | 0 | 0 | 0 |
| Renal impairment | 3 | 0 | 3 | 0 | 0 |
| Reproductive system and breast disorders | |||||
| Epididymitis | 1 | 0 | 0 | 0 | 0 |
| Erectile dysfunction | 0 | 0 | 1 | 0 | 0 |
| Prostatitis | 1 | 0 | 0 | 0 | 0 |
| Prostatomegaly | 1 | 1 | 0 | 0 | 0 |
| Testicular pain | 1 | 0 | 0 | 0 | 0 |
| Testicular swelling | 0 | 0 | 1 | 0 | 0 |
| Respiratory, thoracic and mediastinal disorders | |||||
| Acute respiratory failure | 0 | 1 | 0 | 0 | 0 |
| Asthma | 0 | 1 | 0 | 0 | 0 |
| Cough | 0 | 3 | 0 | 1 | 0 |
| Dyspnoea | 0 | 4 | 2 | 0 | 0 |
| Lung neoplasm | 0 | 0 | 2 | 0 | 0 |
| Nasopharyngitis | 2 | 6 | 6 | 2 | 0 |
| Oropharyngeal pain | 0 | 0 | 0 | 1 | 0 |
| Pharyngolaryngeal pain | 0 | 2 | 0 | 0 | 0 |
| Pleural effusion | 1 | 2 | 0 | 0 | 0 |
| Pulmonary fibrosis | 0 | 0 | 0 | 1 | 0 |
| Pulmonary oedema | 0 | 3 | 0 | 0 | 0 |
| Respiratory distress | 0 | 2 | 0 | 0 | 0 |
| Respiratory tract congestion | 0 | 1 | 0 | 0 | 0 |
| Rhinitis allergic | 1 | 0 | 0 | 1 | 1 |
| Rhinorrhoea | 1 | 1 | 0 | 0 | 0 |
| Sinusitis | 0 | 0 | 3 | 0 | 1 |
| Skin and subcutaneous tissue disorders | |||||
| Cellulitis | 1 | 1 | 1 | 0 | 0 |
| Folliculitis | 1 | 0 | 0 | 0 | 0 |
| Hyperhidrosis | 0 | 1 | 0 | 0 | 0 |
| Skin lesion | 0 | 0 | 1 | 0 | 0 |
| Skin nodule | 1 | 0 | 0 | 0 | 0 |
| Skin ulcer | 0 | 1 | 2 | 1 | 1 |
| Surgical and medical procedures | |||||
| Benign tumour excision | 0 | 0 | 1 | 0 | 0 |
| Cholecystectomy | 0 | 1 | 0 | 0 | 0 |
| Coronary arterial stent insertion | 0 | 1 | 1 | 0 | 0 |
| Stent placement | 0 | 0 | 0 | 0 | 1 |
| Surgery | 0 | 0 | 1 | 0 | 0 |
| Toe amputation | 0 | 0 | 1 | 0 | 0 |
| Uterine dilation and curettage | 1 | 0 | 0 | 0 | 0 |
| Vascular disorders | |||||
| Arteriovenous fistula | 1 | 0 | 0 | 0 | 0 |
| Hypertension | 5 | 7 | 6 | 2 | 1 |
| Iliac artery occlusion | 0 | 0 | 1 | 0 | 0 |
| Peripheral vascular disorder | 0 | 0 | 2 | 0 | 0 |
| Thrombosis | 0 | 0 | 1 | 0 | 0 |
| Transient ischaemic attack | 0 | 2 | 0 | 0 | 2 |
PRP= Panretinal photocoagulation
Comprehensive list of all systemic adverse events as reported by the site using the Medical Dictionary for Regulatory Activities coding.
Study participants with 2 study eyes.
Table 13.
Summary of Study Eye Ocular Adverse Events through 56-Week Visit of Follow-up
| Sham+ Focal/Grid/PRP Laser | Ranibizumab+ Focal/Grid/PRP Laser | Triamcinolone+ Focal/Grid/PRP Laser | |
|---|---|---|---|
|
| |||
| Total Number of Events | N = 277 | N = 242 | N = 255 |
| Anterior chamber | |||
| Anterior chamber cell | 0 | 0 | 1 |
| Corneal dystrophy | 0 | 0 | 1 |
| Hyphaema | 1 | 2 | 0 |
| Cataract | |||
| Cataract nuclear | 1 | 0 | 1 |
| Cataract operation | 1 | 0 | 2 |
| Conjunctiva | |||
| Conjunctival haemorrhage | 5 | 13 | 10 |
| Conjunctival hyperaemia | 1 | 0 | 1 |
| Conjunctivitis | 0 | 1 | 0 |
| Dry eye | 2 | 2 | 1 |
| Eye discharge | 1 | 2 | 0 |
| Keratoconjunctivitis sicca | 0 | 1 | 1 |
| Pinguecula | 0 | 0 | 1 |
| Cornea | |||
| Corneal abrasion | 1 | 0 | 0 |
| Corneal defect | 1 | 1 | 1 |
| Corneal epithelium defect | 1 | 0 | 0 |
| Corneal oedema | 1 | 0 | 0 |
| Corneal pigmentation | 1 | 0 | 0 |
| Punctate keratitis | 4 | 1 | 0 |
| External | |||
| Eye irritation | 8 | 7 | 1 |
| Lacrimation increased | 4 | 3 | 1 |
| Glaucoma-IOP | |||
| Angle closure glaucoma | 0 | 0 | 1 |
| Borderline glaucoma | 0 | 0 | 1 |
| Glaucoma | 1 | 2 | 2 |
| Ocular hypertension | 0 | 0 | 1 |
| Inflammation | |||
| Iritis | 1 | 0 | 3 |
| Iris | |||
| Iris bombe | 0 | 1 | 0 |
| Lens | |||
| Cataract | 4 | 2 | 9 |
| Cataract cortical | 2 | 3 | 1 |
| Cataract subcapsular | 0 | 2 | 9 |
| Posterior capsule | |||
| opacification | 0 | 1 | 1 |
| Lids | |||
| Blepharitis | 4 | 3 | 2 |
| Chalazion | 1 | 0 | 0 |
| Erythema of eyelid | 0 | 0 | 1 |
| Eyelid oedema | 2 | 1 | 2 |
| Eyelid ptosis | 0 | 1 | 0 |
| Miscellaneous-eye | |||
| Ocular hyperaemia | 3 | 2 | 3 |
| Photopsia | 2 | 2 | 0 |
| Sinusitis | 1 | 0 | 0 |
| Foreign body in eye | 0 | 1 | 3 |
| Intraocular pressure increased | 8 | 9 | 18 |
| Iris neovascularisation | 8 | 1 | 2 |
| Neovascularisation | 2 | 0 | 2 |
| Cutis laxa | 0 | 0 | 2 |
| Ecchymosis | 0 | 0 | 1 |
| Eyelid erosion | 0 | 0 | 1 |
| Herpes virus infection | 0 | 1 | 0 |
| Injection site discomfort | 0 | 1 | 0 |
| Corneal dystrophy | 0 | 0 | 1 |
| Visual impairment | 3 | 4 | 5 |
| Optic nerve | |||
| Optic disc disorder | 0 | 0 | 1 |
| Retina | |||
| Diabetic retinal oedema | 3 | 3 | 0 |
| Diabetic retinopathy | 2 | 1 | 1 |
| Macular degeneration | 0 | 0 | 2 |
| Macular ischaemia | 0 | 0 | 1 |
| Macular oedema | 1 | 0 | 3 |
| Maculopathy | 11 | 12 | 9 |
| Retinal degeneration | 1 | 1 | 0 |
| Retinal detachment | 10 | 6 | 3 |
| Retinal exudates | 1 | 2 | 1 |
| Retinal haemorrhage | 3 | 4 | 1 |
| Retinal neovascularisation | 5 | 1 | 4 |
| Retinal pigment epitheliopathy | 0 | 0 | 1 |
| Retinal tear | 0 | 1 | 0 |
| Subretinal fibrosis | 0 | 0 | 1 |
| Vitreous adhesions | 0 | 0 | 1 |
| Sensation-pain | |||
| Abnormal sensation in eye | 3 | 3 | 1 |
| Eye pain | 19 | 19 | 14 |
| Eye pruritus | 9 | 2 | 2 |
| Eyelid pain | 0 | 1 | 0 |
| Foreign body sensation in eyes | 4 | 4 | 2 |
| Strabismus | |||
| Extraocular muscle paresis | 0 | 1 | 1 |
| Visual field | |||
| Visual field defect | 1 | 1 | 0 |
| Visual symptoms/abnormality | |||
| Amaurosis fugax | 1 | 0 | 0 |
| Diplopia | 2 | 5 | 1 |
| Halo vision | 1 | 0 | 0 |
| Photophobia | 7 | 4 | 8 |
| Photopsia | 4 | 9 | 3 |
| Vision blurred | 22 | 17 | 22 |
| Visual acuity reduced | 8 | 4 | 9 |
| Visual disturbance | 1 | 4 | 2 |
| Visual impairment | 4 | 5 | 3 |
| Vitreous | |||
| Endophthalmitis | 0 | 1 | 0 |
| Myodesopsia | 16 | 13 | 16 |
| Vitreous detachment | 4 | 3 | 1 |
| Vitreous disorder | 2 | 0 | 1 |
| Vitreous floaters | 7 | 9 | 13 |
| Vitreous haemorrhage | 47 | 35 | 33 |
| Vitreous opacities | 2 | 0 | 1 |
| Vitrectomy | 1 | 1 | 0 |
PRP=Panretinal photocoagulation
DISCUSSION
In this randomized clinical trial of eyes receiving PRP and concurrent focal/grid laser for DME, 2 ranibizumab injections or 1 triamcinolone injection more likely led to statistically significant improvements in visual acuity from baseline to 14 weeks compared with 2 sham injections (Table 4, Figure 2, and Figure 3). The study was not designed to evaluate effectiveness of either intravitreal ranibizumab or intravitreal triamcinolone on visual acuity or retinal thickening beyond the 14-week study visit, so that evaluations at the 34- or 56-week study visit are provided only asfor the purpose of longer-term safety information. As expected, differences from the sham group did not persist through the 34- or 56-week follow-up visits (Table 8 and Figure 2). Changes in retinal thickness parallel the visual acuity outcomes (Tables 6, 7 and 9, and Figure 4). Since the treating ophthalmologists in this study were unmasked to the treatment assignment, one important potential weakness of this study design includes the possibility of bias introduced if the ophthalmologist were to change the way she or he applied PRP (e.g., 1 vs. more than 1 sitting, more vs. fewer total spots, or timing relative to injection). However, a bias could not be detected with respect to these parameters, nor with respect to how focal/grid laser was applied (Table 2). Furthermore, prior to the 14-week visit, no additional (alternative) treatment for DME was given in any of the 3 treatment groups which could have biased the results (Table 3).
There was little change in the median visual acuity or OCT central subfield thickness from baseline to 14 weeks in the group of eyes receiving sham treatment in this study, however, these eyes did received focal/grid laser for DME involving the central macula at time of entry. In 3 previous studies17, 21, 26 by the DRCR.net in which focal/grid laser was applied to eyes with central DME and similar levels of visual acuity in the absence of concomitant PRP, the OCT central subfield thickness had favorably changed at 16 weeks by medians (25th, 75th percentiles) of −33 (−90, +13), −27 (−61, +13), and −34 (−101, +10) μm, respectively. The median (25th, 75th percentile) change in visual acuity was also favorable at +2 (−4, +7), +1 (−3, +6), and +2 (−3, +8), respectively (unpublished data). Thus, the control arm of this study indicates that eyes with central DME receiving prompt PRP at time of focal/grid laser for DME appear more likely to have increased macular edema and visual acuity loss in the short term than eyes without central DME receiving prompt PRP (in the absence of focal/grid laser)7 as well as eyes with central DME receiving focal/grid laser but not prompt PRP. Also consistent with a previous DRCR.net study, eyes in both the ranibizumab and triamcinolone groups appeared less likely to undergo additional PRP, develop vitreous hemorrhage, develop tractional retinal detachment, or undergo vitrectomy.17
Despite continued meticulous attention to use of a lid speculum and antiseptic to the injection site, there still is a risk of endophthalmitis when using intravitreal injections to treat diabetic retinopathy, as occurred in 1 eye in this study receiving ranibizumab. A previous DRCR.net study evaluating intravitreal anti-VEGF drugs in patients with diabetes, only some of whom had previously treated PDR, did not identify an increased risk of tractional retinal detachments, cerebrovascular accidents, or cardiovascular events.17 This study expands on the previously published findings in a cohort of study participants who underwent PRP, and again did not identify an increased risk of tractional retinal detachments, cerebrovascular accidents, or cardiovascular events following 1 (triamcinolone) or 2 (ranibizumab) intravitreal injections beyond that which could be attributed to chance alone. The safety of ranibizumab injections, continued for a longer period of time in persons with diabetes, remains largely unknown; although, there are several additional randomized clinical trials underway.
In a trial reported previously by the DRCR.net, which evaluated ranibizumab for center-involved DME when PRP was not performed, there were no differences in systemic adverse events that could not be attributed to chance alone when comparing ranibizumab and sham groups.17 There were more cardiovascular or cerebrovascular events as defined by the Antiplatelet Trialists’ Collaboration reported in the ranibizumab group compared with the sham group (Table 11) however, these occurred only once between the baseline injection and the second injection and once approximately 3 weeks after the 4-week study visit injection. The remaining events occurred at some point beyond 4 weeks after the final 4-week study visit injection (Figure 6) when it is assumed that all study drug was cleared from the study participant’s body.
As has been reported in prior studies,13, 14, 27 triamcinolone was associated in this study with an increased risk of elevated IOP. Unlike in prior studies, triamcinolone was not associated with a higher incidence of cataract surgery through 1 year. Whether this was because of the younger age of this cohort compared with prior studies, a lower enthusiasm to operate on cataracts in this cohort with more advanced levels of diabetic retinopathy, or other factors, is unknown.
In summary, the risk of short-term exacerbation of macular edema and associated visual acuity loss following PRP in eyes also receiving focal/grid laser for DME can be reduced by intravitreal triamcinolone or ranibizumab. These results are not maintained by the 34- or 56-week visit with discontinuation of intravitreal treatments after 1 (triamcinolone at baseline) or 2 (ranibizumab at baseline and 4-week) injections however, this study was not designed to evaluate effectiveness of either intravitreal ranibizumab or intravitreal triamcinolone on visual acuity or retinal thickening beyond the 14-week study visit. Evaluations at the 34- or 56-week study visit are provided only for longer-term safety information. The impact and clinical implications of continuing these treatments beyond 14 weeks cannot be determined from this study. While there likely is no increased risk of tractional retinal detachments or cerebrovascular accidents beyond that of chance alone for patients similar to those in this trial and receiving ranibizumab as given in this trial, the side effects of long term intravitreal ranibizumab or steroid use have to be balanced against potential benefits. the benefits and risks of long-term intravitreal ranibizumab or triamcinolone use in eyes receiving focal/grid laser for DME when also receiving PRP remains largely unknown.
Supplementary Material
Acknowledgments
Financial Support: Supported through a cooperative agreement from the National Eye Institute and the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Department of Health and Human Services EY14231, EY14229, EY018817
Footnotes
The most recently published list of the Diabetic Retinopathy Clinical Research Network investigators and staff who participated in this study can be found at www.drcr.net.
An address for reprints will not be provided.
Financial Conflicts of Interest: A complete list of all DRCR.net investigator financial disclosures can be found at www.drcr.net
Financial Disclosure: The funding organization (National Institutes of Health) participated in oversight of the conduct of the study and review of the manuscript but not directly in the design or conduct of the study, nor in the collection, management, analysis, or interpretation of the data, or in the preparation of the manuscript. Genentech provided the ranibizumab for the study and Allergan, Inc. provided the triamcinolone for the study. In addition, Genentech and Allergan, Inc. provided funds to DRCR.net to defray the study’s clinical site costs. As described in the Diabetic Retinopathy Clinical Research Network (DRCR.net) Industry Collaboration Guidelines (available at www.drcr.net), the DRCR.net had complete control over the design of the protocol, ownership of the data, and all editorial content of presentations and publications related to the protocol. A complete list of all DRCR.net investigator financial disclosures can be found at www.drcr.net.
Financial disclosures: Alexander Brucker: Genentech (C, G). Dr. Brucker recused himself from his role as Editor-in-Chief of RETINA when this manuscript was submitted to RETINA and Dr. Brucker was not involved in the DRCR.net decision to submit the manuscript to RETINA. Lloyd P. Aiello: Genentech (O) Andrew Antoszyk: Genentech (C, G) Allergan (G) Susan S. Bressler: Genentech (G) Allergan (G) Dennis Marcus: Genentech (C, G, T, B) Neil Bressler: Grants to investigators at The Johns Hopkins University are negotiated and administered by the institution (such as the School of Medicine) which receives the grants, typically through the Office of Research Administration. Individual investigators who participate in the sponsored project(s) are not directly compensated by the sponsor, but may receive salary or other support from the institution to support their effort on the projects(s). Dr. Neil Bressler is Principal Investigator of grants at The Johns Hopkins University sponsored by the following entities (not including the National Institutes of Health): Allergan, Bausch & Lomb, Carl Zeiss Meditec, EMMES Corporation, Genentech, Lumenis, Notal Vision*, Novartis, QLT, Regeneron, Steba Biotech, Abbott Medical Optics, ForSight Labs, LLC and Genzyme Corporation. Dr. Susan Bressler’s consulting arrangement with Notal Vision in connection with Dr. Neil Bressler’s role as principal investigator on a Notal Vision-sponsored research grant has been reviewed and managed by The Johns Hopkins University School of Medicine in accordance with its conflict of interest policy.
References
- 1.The Diabetic Retinopathy Study Research Group. Preliminary report on effects of photocoagulation therapy. Am J Ophthalmol. 1976;81(4):383–96. doi: 10.1016/0002-9394(76)90292-0. [DOI] [PubMed] [Google Scholar]
- 2.Ferris FL., 3rd How effective are treatments for diabetic retinopathy? JAMA. 1993;269(10):1290–1. [PubMed] [Google Scholar]
- 3.Myers SM. Macular edema after scatter laser photocoagulation for proliferative diabetic retinopathy. Am J Ophthalmol. 1980;90(2):210–6. doi: 10.1016/s0002-9394(14)74855-x. [DOI] [PubMed] [Google Scholar]
- 4.McDonald HR, Schatz H. Visual loss following panretinal photocoagulation for proliferative diabetic retinopathy. Ophthalmology. 1985;92(3):388–93. doi: 10.1016/s0161-6420(85)34016-2. [DOI] [PubMed] [Google Scholar]
- 5.Early Treatment Diabetic Retinopathy Study Research Group. Early photocoagulation for diabetic retinopathy. ETDRS report number 9. Ophthalmology. 1991;98(5 suppl):766–85. [PubMed] [Google Scholar]
- 6.Shimura M, Yasuda K, Nakazawa T, et al. Quantifying alterations of macular thickness before and after panretinal photocoagulation in patients with severe diabetic retinopathy and good vision. Ophthalmology. 2003;110:2386–94. doi: 10.1016/j.ophtha.2003.05.008. [DOI] [PubMed] [Google Scholar]
- 7.Diabetic Retinopathy Clinical Research Network. Observational study of the development of diabetic macular edema following panretinal (scatter) photocoagulation given in 1 or 4 sittings. Arch Ophthalmol. 2009;127(2):132–40. doi: 10.1001/archophthalmol.2008.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Antonetti DA, Barber AJ, Hollinger LA, et al. Vascular endothelial growth factor induces rapid phosphorylation of tight junction proteins occludin and zonula occluden 1. A potential mechanism for vascular permeability in diabetic retinopaty and tumors. J Bio Chem. 1999;274:23463–7. doi: 10.1074/jbc.274.33.23463. [DOI] [PubMed] [Google Scholar]
- 9.Aiello LP, Avery RL, Arrigg PG, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med. 1994;331(22):1480–7. doi: 10.1056/NEJM199412013312203. [DOI] [PubMed] [Google Scholar]
- 10.Zacks DN, Johnson MW. Combined intravitreal injection of triamcinolone acetonide and panretinal photocoagulation for concomitant diabetic macular edema and proliferative diabetic retinopathy. Retina. 2005;25:135–40. doi: 10.1097/00006982-200502000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Maia OO, Jr, Takahashi BS, Costa RA, et al. Combined laser and intravitreal triamcinolone for proliferative diabetic retinopathy and macular edema: one-year results of a randomized clinical trial. Am J Ophthalmol. 2009;147(2):291–7. e2. doi: 10.1016/j.ajo.2008.08.024. [DOI] [PubMed] [Google Scholar]
- 12.Cunningham ET, Jr, Adamis AP, Altaweel M, et al. A phase II randomized double-masked trial of pegaptanib, an anti-vascular endothelial growth factor aptamer, for diabetic macular edema. Ophthalmology. 2005;112:1747–57. doi: 10.1016/j.ophtha.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 13.Gillies MC, Sutter FK, Simpson JM, et al. Intravitreal triamcinolone for refractory diabetic macular edema: two-year results of a double-masked, placebo-controlled, randomized clinical trial. Ophthalmology. 2006;113:1533–8. doi: 10.1016/j.ophtha.2006.02.065. [DOI] [PubMed] [Google Scholar]
- 14.Martidis A, Duker JS, Greenberg PB, et al. Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology. 2002;109(5):920–7. doi: 10.1016/s0161-6420(02)00975-2. [DOI] [PubMed] [Google Scholar]
- 15.Scott IU, Edwards A, et al. Diabetic Retinopathy Clinical Research Network. A phase II randomized clinical trial of intravitreal bevacizumab for diabetic macular edema. Ophthalmal. 2007;114(10):1860–7. doi: 10.1016/j.ophtha.2007.05.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nguyen QD, Shah SM, Heier JS, et al. Primary End Point (Six Months) Results of the Ranibizumab for Edema of the mAcula in diabetes (READ-2) study. Ophthalmology. 2009;116(11):2175–81. e1. doi: 10.1016/j.ophtha.2009.04.023. [DOI] [PubMed] [Google Scholar]
- 17.The Diabetic Retinopathy Clinical Research Network. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010;117(6):1064–77. e35. doi: 10.1016/j.ophtha.2010.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bressler NM, Edwards AR, Beck RW, et al. Exploratory analysis of diabetic retinopathy progression through 3 years in a randomized clinical trial that compares intravitreal triamcinolone acetonide with focal/grid photocoagulation. Arch Ophthalmol. 2009;127(12):1566–71. doi: 10.1001/archophthalmol.2009.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beck RW, Moke PS, Turpin AH, et al. A computerized method of visual acuity testing: adaptation of the early treatment of diabetic retinopathy study testing protocol. Am J Ophthalmol. 2003;135(2):194–205. doi: 10.1016/s0002-9394(02)01825-1. [DOI] [PubMed] [Google Scholar]
- 20.Fong DS, Strauber SF, et al. Writing Committee for the Diabetic Retinopathy Clinical Research Network. Comparison of the modified Early Treatment Diabetic Retinopathy Study and mild macular grid laser photocoagulation strategies for diabetic macular edema. Arch Ophthalmol. 2007;125(4):469–80. doi: 10.1001/archopht.125.4.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Diabetic Retinopathy Clinical Research Network. A randomized trial comparing intravitreal triamcinolone acetonide and focal/grid photocoagulation for diabetic macular edema. Ophthalmology. 2008;115(9):1447–9. 9, e1–10. doi: 10.1016/j.ophtha.2008.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Early Treatment Diabetic Retinopathy Study Research Group. Grading diabetic retinopathy from stereoscopic color fundus photographs - an extension of the modified Airlie House classification. ETDRS report number 10. Ophthalmology. 1991;98:786–806. [PubMed] [Google Scholar]
- 23.Little RJA, Rubin DB. Statistical Analysis with Missing Data. New York: Wiley; 1987. pp. 255–9. [Google Scholar]
- 24.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 25.Antiplatelet Trialists’ Collaboration. Collaborative overview of randomised trials of antiplatelet therapy--I: Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. BMJ. 1994;308(6921):81–106. [PMC free article] [PubMed] [Google Scholar]
- 26.Diabetic Retinopathy Clinical Research Network. The course of response to focal/grid photocoagulation for diabetic macular edema. Retina. 2009;29(10):1436–43. doi: 10.1097/IAE.0b013e3181bcef6b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ockrim ZK, Sivaprasad S, Falk S, et al. Intravitreal triamcinolone versus laser photocoagulation for persistent diabetic macular oedema. Br J Ophthalmol. 2008;92(6):795–9. doi: 10.1136/bjo.2007.131771. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.