We enjoyed reflecting upon the article by Gaitán and colleagues, “Evolution of the Blood-Brain Barrier in Newly Forming MS Lesions”.1, 2 While the cause of MS remains unknown, a better understanding of lesion formation may provide critical clues as to the inciting event. This group has helped rekindle the debate concerning the role of blood vessels in short term lesion evolution for the 21st century. Neuropathologists have found that not all lesions have a central vessel, and lesions can be eccentric from one or multiple vessels.3, 4 Lesions may emanate from a single central nidus, grow by coalescence of periphlebitic branches, or a combination.4, 5
Our own observations based upon monthly, co-registered MRI scans using triple-dosed gadolinium (Gd, 0.3 mmol/kg, 40 min delay, 3T, 3 mm slice thickness) suggest several patterns of ring enhancing lesion (REL) development and resolution over weeks to months.6 Preceding ring formation, a nodule may appear which will later become the non-enhanced region in the ring’s center (Figure A1–5). This may be consistent with Gaitán’s suggestion of an expanding wave of inflammation recruiting additional vessels, with subsequent closure of the blood-brain barrier (BBB) within the lesion center.
Figure.
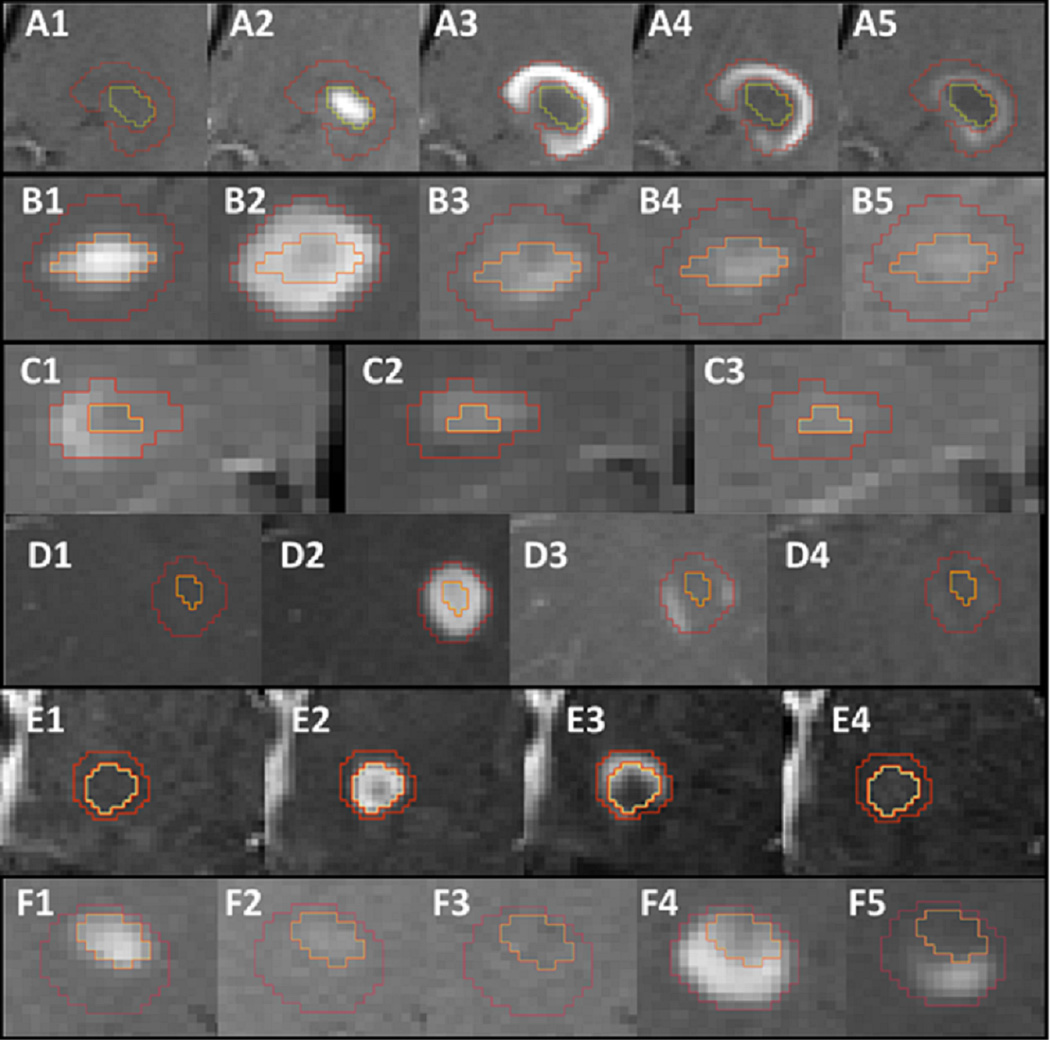
All enhancing lesions are new, based upon normal prior month scan. A. Nodular lesion (A2) evolves the next month into the hypointense center of a REL (A3). The ring progressively fades over 2 months (A3–A5) and disappears the following month (not shown). B. Nodular lesion (B1) develops into a REL with a relatively hypointense center, and resolves over 3 months as a central nodule (B3–B5). C. Open REL (C1) resolves as a central nodule over 2 months (C2–3). D. REL with relatively hypointense center (D2) resolves by fading into the periphery (D2–3). E. REL (E2) develops an expanding ring (E3) before disappearing. F. Nodular lesion (F1) disappears (F2–3) to develop a ring after central nodule resolution (F4) 4 months later.
Different patterns of ring resolution may suggest heterogeneity in the subsequent cascade of immunologic events. Often, the ring will fade over months until it is no longer apparent (Figure A1–5). However, we have also observed a ring returning to a nodule (Figure B1–5, C1–3), a ring fading from the inside to the outer rim (Figure D1–3), an expanding ring (Figure E1–4), and a ring that develops several months after nodule resolution (Figure F1–5). Interestingly, multiple resolution patterns can occur within the same individual.
Important questions remain as to why some MS lesions in some patients form rings. Why is the Gd concentration restricted from the lesion center? Are vessels becoming occluded as Gaitan and colleagues suggest? Or can this be coordinated reconstitution of the BBB? Is the ring an expanding wave of indiscriminate inflammation, or may it represent a strategy to limit inflammatory infiltration with continued surveillance and even repair. Most critically, why does a lesion form in the first place? Is it due to an intrinsic process within the brain parenchyma (“inside in”), or from immune cells entering from the periphery (“outside in”)?7
Multiple unanswered questions about lesion origin continue to plague the MS community. We agree that imaging should continue to help answer more of these questions.8
Acknowledgements
The BECOME study was supported by Bayer Schering Pharma. RTN is supported by NIH K23NS052430 and PQ by NIH T32NS007205.
Footnotes
All coauthors have seen and agree with the contents of the manuscript.
This submission is not under review at any other publication
Conflicts of Interest: PQ: Speaking: Teva Neurosciences. DC: Employee of Biogen Idec. LJW: none. SC: Speaking, consulting, research support: Merck Serono, Bayer, Merck, Genmab. RTN: Research support: Acorda Therapeutics; Speaking/consulting: Acorda Therapeutics, Bayer Healthcare, Biogen Idec, EMD Serono, Teva Neurosciences.
Contributor Information
Peiqing Qian, Department of Neurology, Washington University, St. Louis, MO, USA.
Diego Cadavid, Biogen Idec, Cambridge MA, USA.
Leo J. Wolansky, Capital Health System, Trenton, NJ, USA.
Stuart D. Cook, Neurology, UMDNJ, NJ, USA.
Robert T. Naismith, Neurology, Washington University, St. Louis, MO, USA.
REFERENCES
- 1.Gaitán MI, Shea CD, Dphil IEE, et al. Evolution of the blood-brain barrier in newly forming multiple sclerosis lesions. Annals of Neurology. 2011 doi: 10.1002/ana.22472. n/a-n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lassmann H. A dynamic view on the blood brain barrier in active MS lesions. Annals of Neurology. 2011 doi: 10.1002/ana.22494. n/a-n/a. [DOI] [PubMed] [Google Scholar]
- 3.Dow RS, Berglund G. Vascular patterns of lesions of multiple sclerosis. Arch Neurol Psychiatry. 1942;47:1–18. [Google Scholar]
- 4.McAlpine D, Lumsden CE, Acheson ED. Multiple sclerosis: a reappraisal. 2nd ed. Baltimore: The Williams and Wilkins Company; 1972. [Google Scholar]
- 5.Fog T. The topography of plaques in multiple sclerosis with special reference to cerebral plaques. Acta Neurol Scand Suppl. 1965;15:1–161. [PubMed] [Google Scholar]
- 6.Cadavid D, Wolansky LJ, Skurnick J, et al. Efficacy of treatment of MS with IFNβ-1b or glatiramer acetate by monthly brain MRI in the BECOME study. Neurology. 2009;72:1976–1983. doi: 10.1212/01.wnl.0000345970.73354.17. [DOI] [PubMed] [Google Scholar]
- 7.Henderson APD, Barnett MH, Parratt JDE, Prineas JW. Multiple sclerosis: Distribution of inflammatory cells in newly forming lesions. Annals of Neurology. 2009;66:739–753. doi: 10.1002/ana.21800. [DOI] [PubMed] [Google Scholar]
- 8.Katz D, Taubenberger JK, Cannella B, McFarlin DE, Raine CS, McFarland HF. Correlation between magnetic resonance imaging findings and lesion development in chronic, active multiple sclerosis. Annals of Neurology. 1993;34:661–669. doi: 10.1002/ana.410340507. [DOI] [PubMed] [Google Scholar]


