Abstract
Background:
The increase in the number of individuals with an unhealthily high body weight is particularly relevant in the United States. Obesity (body mass index ≥30 kg/m2) is a well-documented risk factor for the development of osteoarthritis. Furthermore, an increased prevalence of total knee arthroplasty in obese individuals has been observed in the last decades. The primary aim of this systematic literature review was to determine whether obesity has a negative influence on outcome after primary total knee arthroplasty.
Methods:
A search of the literature was performed, and studies comparing the outcome of total knee arthroplasty in different weight groups were included. The methodology of the included studies was scored according to the Cochrane guidelines. Data extraction and pooling were performed. The weighted mean difference for continuous data and the weighted odds ratio for dichotomous variables were calculated. Heterogeneity was calculated with use of the I2 statistic.
Results:
After consensus was reached, twenty studies were included in the data analysis. The presence of any infection was reported in fourteen studies including 15,276 patients (I2, 26%). Overall, infection occurred more often in obese patients, with an odds ratio of 1.90 (95% confidence interval [CI], 1.46 to 2.47). Deep infection requiring surgical debridement was reported in nine studies including 5061 patients (I2, 0%). Deep infection occurred more often in obese patients, with an odds ratio of 2.38 (95% CI, 1.28 to 4.55). Revision of the total knee arthroplasty, defined as exchange or removal of the components for any reason, was documented in eleven studies including 12,101 patients (I2, 25%). Revision for any reason occurred more often in obese patients, with an odds ratio of 1.30 (95% CI, 1.02 to 1.67).
Conclusions:
Obesity had a negative influence on outcome after total knee arthroplasty.
Level of Evidence:
Prognostic Level II. See Instructions for Authors for a complete description of levels of evidence.
The prevalence of obesity in industrialized and emerging countries is reaching epidemic proportions1. The increase in the population of individuals with a high body weight is particularly relevant in the United States2. Obesity is a well-documented risk factor for the development of osteoarthritis3-5. A body mass index (BMI) of ≥30 kg/m2 is generally categorized as obese, but the threshold value for the BMI that accurately separates individuals who are at high or low risk of developing osteoarthritis has not been definitely established. Treatment of arthritis is initially nonoperative, but total joint arthroplasty often becomes necessary if the disease progresses. Consequently, the performance of joint arthroplasty in obese individuals has increased in the last decades.
Although obesity appears to have a negative influence on the complication rate and the survival of total knee arthroplasty, we are aware of no definitive proof in the literature. Amin et al.6 observed that obesity did not influence the five-year outcome of total knee arthroplasty. Benjamin et al.7 reported similar complication rates for total knee arthroplasty in obese compared with nonobese individuals in a study that included 316 patients. A large study of 8892 patients revealed no significant difference between patients who were obese and those who were nonobese with regard to survival and complications8, and several smaller studies also failed to show a difference between these two groups9-11. Chesney et al.12 and Foran et al.13,14 described a trend toward a greater number of complications in obese patients. Only a few studies have reported significantly more complications in obese compared with nonobese patients15,16. The fact that several studies have reported trends toward more complications could indicate that the power of individual studies is too low. Thus, the present meta-analysis of the results of all studies compared the outcome and survival of primary total knee arthroplasty between two BMI groups, <30 and ≥30 kg/m2. The primary aim of this systematic review of the literature was to determine whether obesity had a negative influence on patient outcome after primary total knee arthroplasty.
Materials and Methods
Our search strategy followed the recommendations of the Cochrane collaboration17. The databases of PubMed/MEDLINE, the Cochrane Database of Systematic Reviews, and Embase from 1970 to 2009 were searched for publications on obesity and total knee arthroplasty. The search terms “arthroplasty,” “knee,” “weight,” “BMI,” and “obesity” were used. Furthermore, the reference lists of retrieved publications were checked manually for additional studies that potentially met the inclusion criteria but had not been found by the electronic search. Two investigators (G.M.M.J.K. and D.H.) independently reviewed the literature to identify relevant articles for full-text review. The reviewers independently applied the criteria described above and below to the full text of these articles to select articles for inclusion in this review. The reviewers are orthopaedic surgeons who are familiar with total knee arthroplasty surgery and are also trained and experienced in performing meta-analyses. Disagreement regarding the search was resolved by consensus, with arbitration by a third author (J.A.M.B.) if differences remained.
A study was included if it represented a comparative trial in which the outcome of primary total knee arthroplasty was reported according to BMI. Studies involving all types of cemented and noncemented total knee prosthesis designs were included. Review articles, expert opinions, surgical techniques, and abstracts from scientific meetings were excluded. Only articles written in English were included. Studies were not blinded by author, affiliation, or source.
Our primary research question was to determine whether the outcome of primary total knee arthroplasty was influenced by BMI. Outcomes of interest were infection (deep, superficial, or any), revision for infection, aseptic loosening, hematoma, venous thromboembolism, perioperative fracture, nerve damage, tendon or ligament rupture, Knee Society Score18, Knee Society function subscore, and range of knee motion.
The methodology of the randomized clinical trials and controlled clinical trials was independently assessed by two reviewers (E.S. and D.D.). First, the methodology was assessed with use of the list of criteria recommended by the Cochrane Collaboration Back Review Group19, with adaptation of the bias criteria for observational studies. Second, the criteria listed on The Journal of Bone and Joint Surgery web site, which are an adaptation of the criteria developed by the Centre for Evidence-Based Medicine (Oxford, United Kingdom), were used to define the level of evidence. Disagreement was resolved by group assessment.
The data from the included studies were extracted by two reviewers (G.M.M.J.K., D.H.), with use of a data extraction tool tested in a pilot study and were verified by a third reviewer (W.D.). The available data from the selected studies were then pooled with use of the review manager software from the Cochrane collaboration.
The weighted mean difference and accompanying 95% confidence interval (CI) were calculated for continuous variables, and the weighted odds ratio and 95% CI were calculated for dichotomous variables. If a continuous variable was reported with a range, the standard deviation was calculated with use of the method described by Walter and Yao20. The heterogeneity of the included studies was calculated with use of the I2 statistic, which describes the percentage of variation across studies that is due to heterogeneity rather than chance21. Assessment of heterogeneity in a meta-analysis is crucial because the presence or absence of true heterogeneity (variability among studies) can affect the statistical model that should be used. An I2 value of 0% can be considered to represent no heterogeneity; 25%, low; 50%, moderate; and 75%, high. For an I2 value of up to 50%, it is correct to use a fixed-effects model when pooling the data; for a higher heterogeneity, a random-effects model should be used. We also assessed heterogeneity by means of a chi-square analysis, with p < 0.1 considered suggestive of statistical heterogeneity.
Source of Funding
This study was supported in part by NIH (National Institutes of Health) grant 5K23 AR052392-05 (W.D.) and by an AOSSM/MTF (American Orthopaedic Society for Sports Medicine/Musculoskeletal Transplant Foundation) Career Development Award Supplement (W.D.).
Results
A flow diagram showing the selection of the studies is shown in Figure 1. After consensus was reached, twenty studies were included for data analysis. The baseline characteristics and methodology of the included trials are summarized in the Appendix6-16,22-30.
Fig. 1.
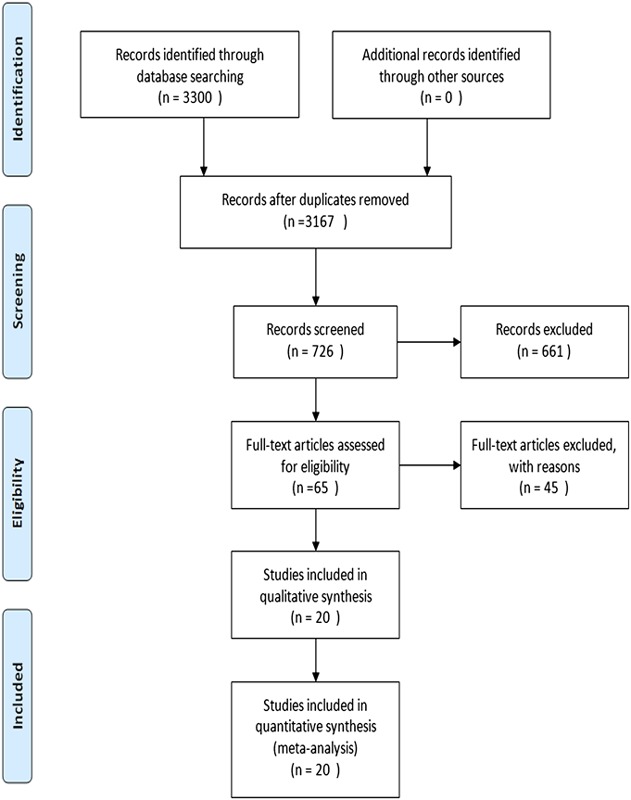
Flowchart showing identification of the included studies.
Data regarding the presence of any infection were extracted from the studies in which this outcome was reported; in addition, deep and superficial infections were analyzed separately in studies that distinguished between them. The presence of any infection was reported in fourteen studies including 15,276 patients; these studies had a low heterogeneity, with an I2 of 26% (Fig. 2). Overall, infection occurred more often in obese patients, with an odds ratio of 1.90 (95% CI, 1.46 to 2.47). Superficial infection was reported separately in nine studies including 4905 patients; the heterogeneity among these studies was low, with an I2 of 6%. Superficial infection occurred more often in obese patients, with an odds ratio of 2.17 (95% CI, 1.47 to 3.13). Deep infection requiring surgical debridement was reported separately in nine studies including 5061 patients; no heterogeneity was found among these studies (I2, 0%). Deep infection occurred more often in obese patients, with an odds ratio of 2.38 (95% CI, 1.28 to 4.55) (Table I).
Fig. 2.
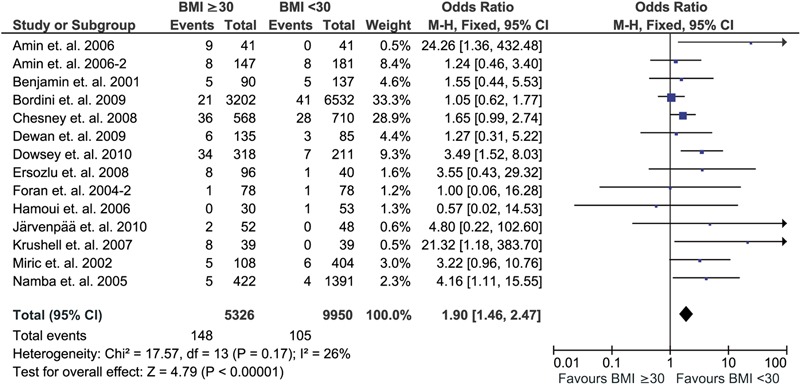
Overall infection rate after total knee arthroplasty according to body mass index (BMI, in kg/m2). M-H = Mantel-Haenszel, CI = confidence interval, and df = degrees of freedom.
TABLE I.
Results of the Meta-Analysis
| Outcome | No. of Patients | No. of Events | Heterogeneity, I2 (%) | Odds Ratio or Difference (95% CI) |
| Any infection | 15,276 | 253 | 26 | 1.90 (1.46 to 2.47) |
| Superficial infection | 4905 | 126 | 6 | 2.17 (1.47 to 3.13) |
| Deep infection | 5061 | 45 | 0 | 2.38 (1.28 to 4.55) |
| Any revision | 12,101 | 277 | 25 | 1.30 (1.02 to 1.67) |
| Revision for infection | 13,686 | 75 | 0 | 0.98 (0.61 to 1.56) |
| Revision for aseptic loosening | 10,207 | 135 | 0 | 1.23 (0.87 to 1.75) |
| Intraoperative fracture | 10,363 | 17 | 0 | 1.03 (0.38 to 2.78) |
| Nerve injury | 10,217 | 12 | 0 | 0.89 (0.28 to 2.86) |
| Intraoperative tendon/ligament rupture | 10490 | 16 | 29 | 0.97 (0.35 to 2.70) |
| Venous thromboembolism | 13,459 | 106 | 0 | 1.19 (0.78 to 1.82) |
| Knee Society Score | 670 | — | 0 | 3.23 (1.57 to 4.90)* |
| Knee Society function subscore | 1302 | — | 84 |
A positive difference indicates a higher score in the nonobese group.
Revision of the total knee arthroplasty, defined as exchange or removal of the components for any reason, was documented in eleven studies including 12,101 patients. Heterogeneity among these studies was low, with an I2 of 25%. Revision for any reason occurred more often in obese patients, with an odds ratio of 1.30 (95% CI, 1.02 to 1.67). With the numbers available, the revision rate did not differ significantly between obese and nonobese patients when revision surgery for infection and revision for aseptic loosening were analyzed separately (Table I).
The complications that occurred during the surgical procedure were mentioned in only four studies. The low heterogeneity among these studies allowed pooling of the results and, on the basis of the numbers, no significant differences were found in the occurrence of intraoperative fracture, nerve injury, or tendon or ligament rupture. This lack of difference may be the result of the small number of events in these studies (Table I).
The main postoperative complication not related to the implant was the occurrence of a clinically manifest deep venous thromboembolism and/or pulmonary embolism. Nine studies with a total of 13,459 patients reported on this complication, and the results were pooled since no heterogeneity among the studies was found (I2, 0%). This complication rate did not differ significantly between obese and nonobese patients (odds ratio, 1.19; 95% CI, 0.78 to 1.82).
The most commonly reported functional outcomes in the studies were the Knee Society Score and Knee Society function subscore. Nine studies including 670 patients reported the Knee Society Score for obese and nonobese patients. After pooling of the studies, which had an I2 of 0%, this score showed a difference of 3.23 points (95% CI, 1.57 to 4.90 points) in favor of the nonobese patients; however, the clinical significance of such a small difference on a scale of 0 to 100 can be questioned. The Knee Society function subscore was reported for a greater number of patients, but it could not be pooled because of the high heterogeneity (I2, 84%).
Subgroup analyses of certain outcomes were performed for short or long-term follow-up. The overall infection rate was analyzed for studies that reported the short-term outcome, since infection may be better documented in such studies. The eight studies including 13,133 patients that reported short-term results indicated a twofold greater infection rate in the obese patients (odds ratio, 2.06; 95% CI, 1.46 to 2.91); the heterogeneity was moderate (I2, 46%) (Fig. 3). In addition, revision for any reason was analyzed for studies with more than five years of follow-up, since the number of revisions was expected to increase with elapsed time. The nine studies including 2284 patients that fulfilled this criterion indicated the revision rate to be twice as high in the obese patients in the long term (odds ratio, 1.79; 95% CI, 1.15 to 2.78) (I2, 0%) (Fig. 4).
Fig. 3.
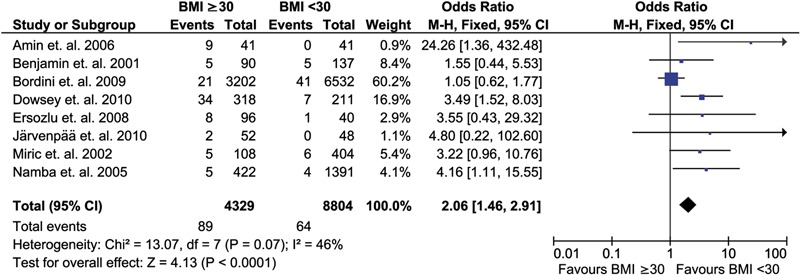
Overall infection rate after total knee arthroplasty according to body mass index (BMI, in kg/m2) in studies with short-term follow-up. M-H = Mantel-Haenszel, CI = confidence interval, and df = degrees of freedom.
Fig. 4.
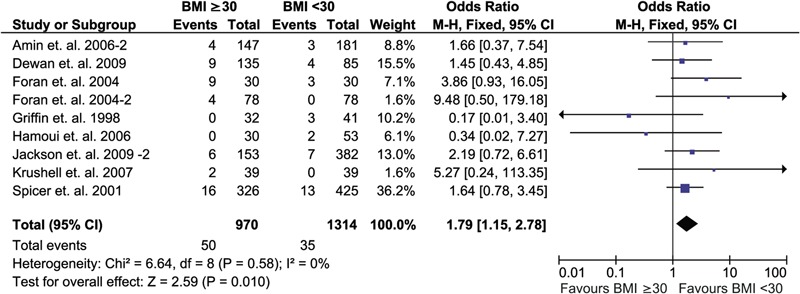
Overall revision rate after total knee arthroplasty according to body mass index (BMI, in kg/m2) in studies with follow-up of more than five years. M-H = Mantel-Haenszel, CI = confidence interval, and df = degrees of freedom.
Discussion
The aim of our systematic review of the literature was to show whether obesity leads to a worse outcome following total knee arthroplasty. Our results showed that patients with a BMI of ≥30 kg/m2 had more infections and a higher revision rate compared with patients with a BMI of <30 kg/m2. Total knee arthroplasty in obese patients was therefore associated with higher risks in both the short and the long term. We believe that obese patients should be informed of the above-mentioned risks and should be advised to lose weight. Many patients will fail to achieve this goal without professional help, so we refer obese patients with osteoarthritis to a multidisciplinary obesity outpatient clinic. If this approach fails to result in weight loss, the patient at least benefits from a thorough analysis of existing comorbidity and optimization of his or her medical condition. We do not withhold a total knee arthroplasty from these patients, but we inform them extensively regarding the risk that their obesity poses with regard to this procedure.
The study by Bordini et al.8 may have introduced a bias in our meta-analysis of infection. This study could have influenced the outcome because the study population was large (8892 patients) and the infection rate was dramatically low, with four superficial infections and fifty-eight revisions for infection. The superficial infection rate was only 0.04%, and the rate of any infection (calculating revision for infection as representing deep infection) was 0.6%. We performed an additional analysis in which this study was omitted from the calculation of the infection rate in the studies with short-term outcome. This did alter the results of the meta-analysis, with the obese group scoring worse for infection risk, with an odds ratio of 3.57 (95% CI, 2.17 to 5.88). Heterogeneity remained low, with an I2 of 0%.
It is reasonable to assume that obese patients have more comorbidities than nonobese patients, and that this is theoretically the reason for the higher complication rates in the obese group. However, obese patients without other comorbidities do not have the same risk as obese patients with other comorbidities. The choice of the threshold for the BMI value was based on a consensus that 30 kg/m2 represents the cutoff between obese and nonobese individuals. We chose to use 30 kg/m2 as the threshold even though a BMI of ≥25 kg/m2 indicates that an individual is overweight. A BMI of 25 kg/m2 to <30 kg/m2 is becoming more common and is starting to be considered as more or less normal. Not all of the included studies used a BMI value of 30 kg/m2 as the threshold for obesity. Some used a threshold of 35 kg/m2, although no justification for the use of that threshold was provided27,29. To assess the effect of weight on the outcome, it would be best to use BMI as a continuous variable in the analysis.
Obtaining Level-I evidence for the impact of morbid obesity on the outcome of total knee arthroplasty is difficult; a highest-quality study cannot be performed since blinding is only partially possible. We chose to include all comparative studies in this systematic review since that represented the best evidence available at present. Differentiation between retrospective and prospective trials can be difficult because many authors present a study with prospective data collection and retrospective analysis of the data as being prospective in design. Scoring of the methodology, however, showed that the studies included in this review were comparable and that pooling them was therefore justifiable.
We conclude that obesity had a negative influence on the outcome of patients treated with total knee arthroplasty, with more short-term complications and poorer long-term outcome compared with nonobese patients.
Appendix
Tables summarizing the methodological validity and characteristics of the included studies are available with the online version of this article as a data supplement at jbjs.org.
Supplementary Material
Disclosure of Potential Conflicts of Interest
Tables summarizing the methodological validity and characteristics of the included studies
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Campos P, Saguy A, Ernsberger P, Oliver E, Gaesser G. The epidemiology of overweight and obesity: public health crisis or moral panic? Int J Epidemiol. 2006. Feb;35(1):55-60 Epub 2005 Dec 8 [DOI] [PubMed] [Google Scholar]
- 2.Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, Hayflick L, Butler RN, Allison DB, Ludwig DS. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005. Mar 17;352(11):1138-45 [DOI] [PubMed] [Google Scholar]
- 3.Stürmer T, Günther KP, Brenner H. Obesity, overweight and patterns of osteoarthritis: the Ulm Osteoarthritis Study. J Clin Epidemiol. 2000. Mar 1;53(3):307-13 [DOI] [PubMed] [Google Scholar]
- 4.Flugsrud GB, Nordsletten L, Espehaug B, Havelin LI, Meyer HE. Risk factors for total hip replacement due to primary osteoarthritis: a cohort study in 50,034 persons. Arthritis Rheum. 2002. Mar;46(3):675-82 [DOI] [PubMed] [Google Scholar]
- 5.Flugsrud GB, Nordsletten L, Espehaug B, Havelin LI, Engeland A, Meyer HE. The impact of body mass index on later total hip arthroplasty for primary osteoarthritis: a cohort study in 1.2 million persons. Arthritis Rheum 2006. Mar;54(3):802-7 [DOI] [PubMed] [Google Scholar]
- 6.Amin AK, Patton JT, Cook RE, Brenkel IJ. Does obesity influence the clinical outcome at five years following total knee replacement for osteoarthritis? J Bone Joint Surg Br. 2006. Mar;88(3):335-40 [DOI] [PubMed] [Google Scholar]
- 7.Benjamin J, Tucker T, Ballesteros P. Is obesity a contraindication to bilateral total knee arthroplasties under one anesthetic? Clin Orthop Relat Res. 2001. Nov;(392):190-5 [DOI] [PubMed] [Google Scholar]
- 8.Bordini B, Stea S, Cremonini S, Viceconti M, De Palma R, Toni A. Relationship between obesity and early failure of total knee prostheses. BMC Musculoskelet Disord. 2009. Mar 5;10:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bourne RB, McCalden RW, MacDonald SJ, Mokete L, Guerin J. Influence of patient factors on TKA outcomes at 5 to 11 years followup. Clin Orthop Relat Res. 2007. Nov;464:27-31 [DOI] [PubMed] [Google Scholar]
- 10.Hamoui N, Kantor S, Vince K, Crookes PF. Long-term outcome of total knee replacement: does obesity matter? Obes Surg. 2006. Jan;16(1):35-8 [DOI] [PubMed] [Google Scholar]
- 11.Ersozlu S, Akkaya T, Ozgur AF, Sahin O, Senturk I, Tandogan R. Bilateral staged total knee arthroplasty in obese patients. Arch Orthop Trauma Surg. 2008. Feb;128(2):143-8 Epub 2007 Aug 11 [DOI] [PubMed] [Google Scholar]
- 12.Chesney D, Sales J, Elton R, Brenkel IJ. Infection after knee arthroplasty a prospective study of 1509 cases. J Arthroplasty. 2008. Apr;23(3):355-9 [DOI] [PubMed] [Google Scholar]
- 13.Foran JR, Mont MA, Etienne G, Jones LC, Hungerford DS. The outcome of total knee arthroplasty in obese patients. J Bone Joint Surg Am. 2004. Aug;86(8):1609-15 [DOI] [PubMed] [Google Scholar]
- 14.Foran JR, Mont MA, Rajadhyaksha AD, Jones LC, Etienne G, Hungerford DS. Total knee arthroplasty in obese patients: a comparison with a matched control group. J Arthroplasty. 2004. Oct;19(7):817-24 [DOI] [PubMed] [Google Scholar]
- 15.Dowsey MM, Liew D, Stoney JD, Choong PF. The impact of pre-operative obesity on weight change and outcome in total knee replacement: a prospective study of 529 consecutive patients. J Bone Joint Surg Br. 2010. Apr;92(4):513-20 [DOI] [PubMed] [Google Scholar]
- 16.Järvenpää J, Kettunen J, Kröger H, Miettinen H. Obesity may impair the early outcome of total knee arthroplasty. Scand J Surg. 2010;99(1):45-9 [DOI] [PubMed] [Google Scholar]
- 17.Lefebvre C, Manheimer E, Glanville J. Cochrane Highly Sensitive Search Strategy for identifying randomized trials in MEDLINE: sensitivity-maximizing version. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration 2008. http://www.cochrane-handbook.org. [Google Scholar]
- 18.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989. Nov;(248):13-4 [PubMed] [Google Scholar]
- 19.van Tulder M, Furlan A, Bombardier C, Bouter L; Editorial Board of the Cochrane Collaboration Back Review Group. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (Phila Pa 1976). 2003. Jun 15;28(12):1290-9 [DOI] [PubMed] [Google Scholar]
- 20.Walter SD, Yao X. Effect sizes can be calculated for studies reporting ranges for outcome variables in systematic reviews. J Clin Epidemiol. 2007. Aug;60(8):849-52 Epub 2007 Mar 23 [DOI] [PubMed] [Google Scholar]
- 21.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003. Sep 6;327(7414):557-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amin AK, Clayton RA, Patton JT, Gaston M, Cook RE, Brenkel IJ. Total knee replacement in morbidly obese patients. Results of a prospective, matched study. J Bone Joint Surg Br. 2006. Oct;88(10):1321-6 [DOI] [PubMed] [Google Scholar]
- 23.Dewan A, Bertolusso R, Karastinos A, Conditt M, Noble PC, Parsley BS. Implant durability and knee function after total knee arthroplasty in the morbidly obese patient. J Arthroplasty. 2009. Sep;24(6 Suppl):89-94, 94.e1-3. Epub 2009 Jul 2 [DOI] [PubMed] [Google Scholar]
- 24.Griffin FM, Scuderi GR, Insall JN, Colizza W. Total knee arthroplasty in patients who were obese with 10 years followup. Clin Orthop Relat Res. 1998. Nov;(356):28-33 [DOI] [PubMed] [Google Scholar]
- 25.Jackson MP, Sexton SA, Walter WL, Walter WK, Zicat BA. The impact of obesity on the mid-term outcome of cementless total knee replacement. J Bone Joint Surg Br. 2009. Aug;91(8):1044-8 [DOI] [PubMed] [Google Scholar]
- 26.Krushell RJ, Fingeroth RJ. Primary total knee arthroplasty in morbidly obese patients: a 5- to 14-year follow-up study. J Arthroplasty. 2007. Sep;22(6 Suppl 2):77-80 Epub 2007 Jul 26 [DOI] [PubMed] [Google Scholar]
- 27.Miric A, Lim M, Kahn B, Rozenthal T, Bombick D, Sculco TP. Perioperative morbidity following total knee arthroplasty among obese patients. J Knee Surg. 2002. Spring;15(2):77-83 [PubMed] [Google Scholar]
- 28.Naal FD, Neuerburg C, Salzmann GM, Kriner M, von Knoch F, Preiss S, Drobny T, Munzinger U. Association of body mass index and clinical outcome 2 years after unicompartmental knee arthroplasty. Arch Orthop Trauma Surg. 2009. Apr;129(4):463-8 Epub 2008 Apr 15 [DOI] [PubMed] [Google Scholar]
- 29.Namba RS, Paxton L, Fithian DC, Stone ML. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J Arthroplasty. 2005. Oct;20(7 Suppl 3):46-50 [DOI] [PubMed] [Google Scholar]
- 30.Spicer DD, Pomeroy DL, Badenhausen WE, Schaper LA, Jr, Curry JI, Suthers KE, Smith MW. Body mass index as a predictor of outcome in total knee replacement. Int Orthop. 2001;25(4):246-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest
Tables summarizing the methodological validity and characteristics of the included studies


