Abstract
Background:
There is limited population-based literature on rates and risk factors for revision following primary total hip replacement.
Methods:
We performed a retrospective cohort study of Medicare beneficiaries who had elective total hip replacement for osteoarthritis between July 1, 1995, and June 30, 1996. Patients were followed with use of Medicare claims through 2008. The primary end point was revision total hip replacement as indicated by hospital discharge codes according to the International Classification of Diseases, Ninth Revision. We used the Kaplan-Meier method to plot the risks of revision and of death over a twelve-year follow-up period. We used Cox proportional hazard regression models to identify preoperative risk factors for revision of primary total hip replacement. We conducted sensitivity analyses to account for competing risks of major comorbid conditions.
Results:
The risk of revision total hip replacement for patients remaining alive was approximately 2% per year for the first eighteen months and then 1% per year for the remainder of the follow-up period. The absolute risk of death over the twelve-year follow-up period exceeded the risk of revision total hip replacement by a factor of ten (59% vs. 5.7%) in patients older than seventy-five years at the time of primary total hip replacement and by a factor of three (29% vs. 9.4%) in patients sixty-five to seventy-five years old at the time of surgery. In multivariate Cox proportional hazard models, the relative risk of revision was higher in men than in women (hazard ratio [HR], 1.23; 95% confidence interval [95% CI], 1.15, 1.31) and in patients sixty-five to seventy-five years of age at the time of primary total hip replacement than in those over seventy-five years (HR, 1.47; 95% CI, 1.37, 1.58). Patients of surgeons who performed fewer than six total hip replacements annually in the Medicare population had a higher risk of revision than those whose surgeons performed more than twelve per year (HR, 1.21; 95% CI, 1.12, 1.32).
Conclusions:
Efforts to reduce the number of revision hip arthroplasties should be targeted at revisions occurring in the first eighteen months following the index arthroplasty, when revision risk is higher, and at younger patients, who are more likely to survive long enough to require revision.
Level of Evidence:
Prognostic Level II. See Instructions for Authors for a complete description of levels of evidence.
Total hip replacement is performed on more than 280,000 persons annually in the United States1. For more than 90% of these procedures, the underlying diagnosis is osteoarthritis of the hip. While the results of total hip replacement are generally excellent, implant failure may occur by a number of mechanisms, including infection, dislocation, and osteolysis leading to symptomatic loosening. Patients with symptomatic failure of a primary total hip replacement are typically referred to orthopaedic surgeons for consideration of revision surgery. Revision total hip replacement is performed on more than 40,000 persons annually in the U.S., at a direct cost exceeding $1 billion1.
Study of the risk of revision total hip replacement among patients having primary surgery and of factors associated with revision risk is challenging. Because revision is a relatively infrequent outcome that can occur a decade or more after the primary surgery, such studies must involve large cohorts of patients followed consistently over many years. To our knowledge, there are no prior population-based estimates of the risk of revision and predictors of revision risk following primary total hip replacement with complete follow-up extending over twelve years in the U.S. The Scandinavian hip registries provide estimates of revision risk and risk factors for revision. However, many of the patients entered into these large cohorts have not been followed long enough to permit precise estimates of long-term revision risk2–6.
Prior studies have identified male sex, younger age, and greater activity level as risk factors associated with revision of a primary total hip replacement7. Additional risk factors are associated with specific indications for revisions such as dislocation and infection8,9. Lower surgeon volume has been associated with higher revision risk in the first eighteen months after primary total hip replacement, with no further risk associated with surgeon volume from eighteen months to four years10. The association of surgeon volume with longer-term risk of revision for more than four years after total hip replacement has not been examined. Prior studies of revision total hip replacement have not placed revision risk in the context of the considerable mortality that patients experience in their seventh through ninth decades of life.
The objectives of this study were to address these research gaps by examining the risk of revision following primary total hip replacement for osteoarthritis in the U.S. Medicare population and to examine the effects of sociodemographic factors and surgeon and hospital volume on the risk of revision over a twelve-year period of follow-up. We also placed the absolute risk of revision after primary total hip replacement among patients who were more than sixty-five years old at the time of surgery in the context of patient mortality in this age group.
Materials and Methods
We performed a retrospective claims-based cohort study of revision following primary total hip replacement in the U.S. Medicare population. The sample included Medicare beneficiaries who had primary elective total hip replacement for osteoarthritis from July 1, 1995, through June 30, 1996. On the basis of coded diagnoses and procedures in the total hip replacement hospitalization, we excluded patients with other underlying diagnoses. We also excluded patients enrolled in a Medicare health maintenance organization, as submission of claims is inconsistent in this group. We described this cohort in detail in prior work10,11. Because this is a claims-based cohort study, subjects are identified and followed longitudinally solely with claims data.
We followed patients in claims through December 31, 2008. The primary outcome was revision total hip replacement identified with use of International Classification of Diseases, Ninth Revision (ICD-9) codes at hospital discharge. The code for revision was 81.53 prior to September 30, 2005, and 00.70 to 00.73 subsequently. We recognized that revisions on the right and left side cannot be distinguished in Medicare claims12. Therefore, if subjects had a primary total hip replacement on the contralateral side after the index primary procedure, we censored the subject at the time of the subsequent primary procedure because a revision following these two primary total hip replacements could not reliably be attributed to the index total hip replacement. We could not exclude patients with a total hip replacement on the contralateral side prior to the index primary procedure or prior to sixty-five years of age because we did not have claims data for years prior to 1995 and because patients do not enter Medicare coverage until they are sixty-five years old.
We used the Kaplan-Meier method to estimate and depict graphically the cumulative revision risk, stratified by the age of the patient at the time of surgery, sex of the patient, and annual volume of total hip replacements performed by the surgeon. We depicted the Kaplan-Meier estimates in two ways. First, per convention, for each month of the follow-up period, we plotted the proportion of patients free of revision among those who were alive at the start of the month. The second approach captured the competing risk of mortality in this aging cohort. At the month of follow-up, we graphed the proportions of patients who were alive and revision-free, those who had died without revision, and those (either dead or alive) who had had a revision.
We examined risk factors for revision of primary total hip replacement using a Cox proportional hazards model. The dependent variable in the model was time to revision total hip replacement over the twelve-year follow-up period. Independent variables were ascertained at the time of total hip replacement and included patient age, sex, race, Medicaid eligibility (proxy for low income), and comorbidity, as well as hospital and surgeon annual volume of total hip replacements in the Medicare population. We dichotomized age as sixty-five to seventy-five years or as more than seventy-five years and race as white or nonwhite. Comorbidity was assessed with the claims-based Charlson comorbidity index and was dichotomized as zero or one comorbidity versus two or more13,14. Hospital and surgeon volume were calculated from claims and comprised the annual volume of primary total hip replacements performed by the hospital (or surgeon) on Medicare beneficiaries from July 1995 through June 1996. On the basis of prior work11,15, we categorized hospital volume as one to twenty-five, twenty-six to fifty, and more than fifty total hip replacements per year in the Medicare population. Similarly, surgeon volume was categorized as less than six, six to twelve, and more than twelve total hip replacements per year in the Medicare population. We used the piecewise exponential model to estimate the effects of surgeon volume on risk of revision total hip replacement in different time periods: the first eighteen months postoperatively, eighteen months to nine years, and nine or more years postoperatively.
We performed a sensitivity analysis to account for competing risks in patients with total hip replacement. Competing risks occur when the patient may experience outcomes that alter or prevent the primary outcome of revision total hip replacement from occurring16,17. For example, if a patient has a stroke and becomes less mobile, a revision may be delayed or never undertaken. Our sensitivity analysis considered death, fracture, stroke, and myocardial infarction, identified in Medicare claims, as competing risks for revision. Potential predictors of revision were evaluated with use of a proportional hazards model for the cumulative incidence of revision adjusting for competing risks18. Patients were censored at the end of follow-up, twelve years, or when they received a second primary total hip replacement.
Analyses were performed with use of SAS software (version 9.2; SAS Institute, Cary, North Carolina) and R version 2.11.1. All study activities were approved by the Human Studies Committee at Partners HealthCare and through Data Use Agreements with the Centers for Medicare and Medicaid Research.
Source of Funding
This study was funded by the National Institutes of Health (NIH). The NIH played no role in our investigation beyond providing the funding.
Results
Cohort Characteristics
During the study period, 76,627 patients on Medicare underwent total hip replacement. Of these, 51,347 met the eligibility criteria for this study and were included in the analysis. Baseline features of the cohort are shown in Table I.
TABLE I.
Baseline Features of Study Cohort of 51,347 Medicare Beneficiaries Undergoing Primary Total Hip Replacement from July 1995 through June 1996
| Feature | No. of Patients | Percentage |
| Sex | ||
| Male | 18,921 | 37 |
| Female | 32,426 | 63 |
| Age at time of primary total hip replacement | ||
| 65-75 yr | 30,895 | 60 |
| >75 yr | 20,452 | 40 |
| Comorbidity (Charlson score) | ||
| >1 | 6584 | 13 |
| 0–1 | 44,763 | 87 |
| Medicaid eligibility | ||
| Yes | 2836 | 6 |
| No | 48,511 | 94 |
| Race* | ||
| White | 48,420 | 95 |
| Nonwhite | 2474 | 5 |
| Annual volume of total hip replacements done at hospital where primary total hip replacement performed† | ||
| 1–25 | 18,187 | 35 |
| 26–50 | 14,573 | 28 |
| >50 | 18,587 | 36 |
| Annual volume of total hip replacements done by surgeon who performed the primary total hip replacement*† | ||
| 1–6 | 13,372 | 27 |
| 7–12 | 15,459 | 31 |
| >12 | 20,305 | 41 |
Data on race were missing for 453 patients (0.9%), and data on surgeon volume for 2221 patients (4.3%) were missing. No data were missing for other variables.
Listed volumes indicate only Medicare patients who had total hip replacement.
The risk of revision arthroplasty over the follow-up period is illustrated with Kaplan-Meier curves (Figs. 1-A and 1-B). These figures demonstrate graphically the early incidence of revision of approximately 2% over the first eighteen months and then the steady occurrence of revision (at a lower rate of approximately 1% per year) over the subsequent decade. The figures also demonstrate the effects of patient age and sex and surgeon volume. In analyses that considered separately the effects of surgeon volume in the first three time periods evaluated, lower surgeon volume was associated with a greater hazard of revision in the first eighteen months, but not in the subsequent two periods.
Fig. 1-A. Kaplan-Meier curves showing the risk of revision total hip replacement among surviving patients.
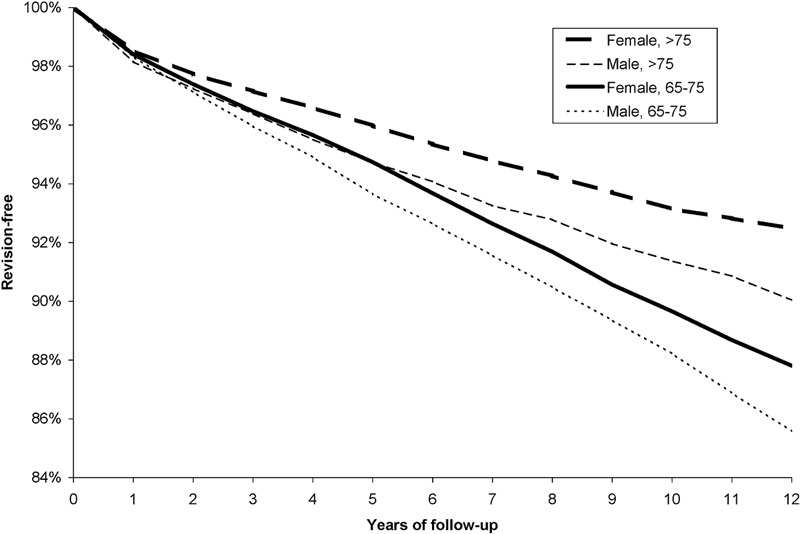
The revision-free survival curve is stratified by age at the time of primary total hip replacement (sixty-five to seventy-five years of age compared with more than seventy-five years) and sex.
Fig. 1-B. Kaplan-Meier curves showing the risk of revision total hip replacement among surviving patients.
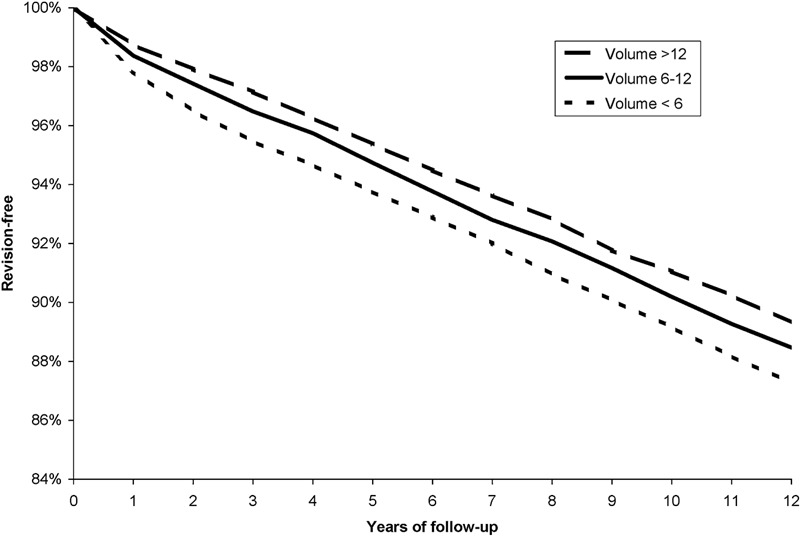
The revision-free survival curve is stratified by the annual volume of total hip replacements done by the surgeon who performed the primary total hip replacement (fewer than six, six to twelve, and more than twelve primary total hip replacements per year in the Medicare population).
The risks of revision arthroplasty compared with the mortality risks over the period of follow-up are illustrated in Figures 2-A and 2-B. As the figures demonstrate, among patients greater than seventy-five years old, 59% died within the twelve-year follow-up window. Another 5.7% had a revision, and 35% were alive and at risk for revision. Among patients who were sixty-five to seventy-five years old at the time of the primary total hip replacement, 29% died within the twelve-year follow-up period, while another 9.4% had a revision and 62% were alive and at risk for revision.
Fig. 2-A. The proportion of patients who died over the course of follow-up (dotted area), those who had a revision (black), and those who were alive and at risk for revision (gray). The revision group includes those who remained alive and those who had a revision and then died.
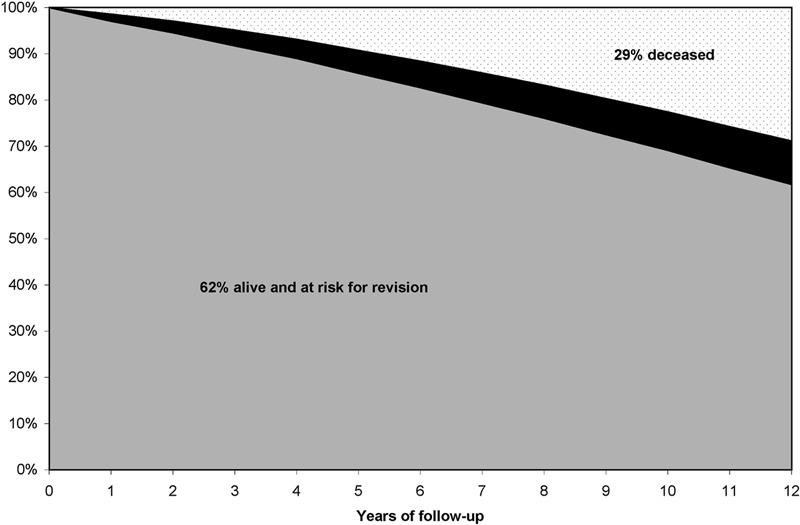
Among patients who were sixty-five to seventy-five years old at the time of primary total hip replacement, the revised group comprised 9.4% of the original cohort; 29% had died.
Fig. 2-B. The proportion of patients who died over the course of follow-up (dotted area), those who had a revision (black), and those who were alive and at risk for revision (gray). The revision group includes those who remained alive and those who had a revision and then died.
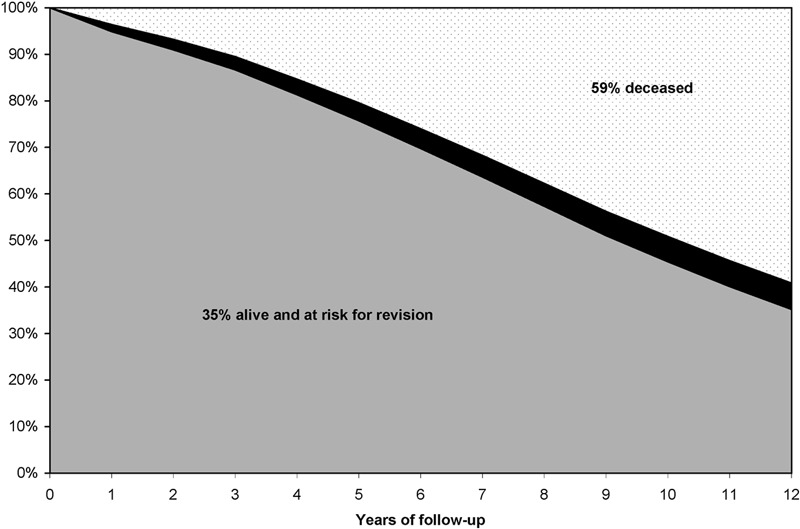
Among patients who were more than seventy-five years old at the time of primary total hip replacement, the revised group (black) comprised 5.7% of the original cohort; 59% had died.
Bivariate Analyses of Revision Risk
We performed bivariate Cox proportional hazards models with time to revision as the dependent variable. Separate models were created for each potential predictor. Younger patient age, male sex, and surgeon volume of fewer than six total hip replacements per year in the Medicare population were all associated with higher revision rates, with hazard ratios for these factors of ≥1.24 (Table II). Hospital volume of fewer than twenty-five total hip replacements per year (compared with more than fifty procedures) had a hazard ratio (HR) of 1.14 (95% confidence interval [95% CI], 1.07, 1.23). All other variables were not significantly associated with revision total hip replacement, with hazard ratios between 0.90 and 1.02, indicating <10% relative change in risk across levels of the variable.
TABLE II.
Univariate and Multivariate Associations Between Baseline Variables and Risk of Revision Total Hip Replacement Among Medicare Beneficiaries Undergoing Primary Total Hip Replacement from July 1995 through June 1996
| Bivariate* |
Multivariate† |
|||
| Variable | Hazard Ratio | 95% Confidence Interval | Hazard Ratio | 95% Confidence Interval |
| Sex | ||||
| Male | 1.26 | 1.18, 1.34 | 1.23 | 1.15, 1.31 |
| Female | 1.0 | |||
| Age | ||||
| 65-75 yr | 1.49 | 1.40, 1.60 | 1.47 | 1.37, 1.58 |
| >75 yr | 1.0 | |||
| Race | ||||
| White | 0.90 | 0.79, 1.03 | ||
| Nonwhite | 1.0 | |||
| Medicaid eligibility | ||||
| Yes | 0.92 | 0.80, 1.06 | ||
| No | 1.0 | |||
| Comorbidity (Charlson score) | ||||
| >1 | 1.02 | 0.93, 1.12 | ||
| 0–1 | 1.0 | |||
| Hospital volume‡ | ||||
| 1–25 | 1.14 | 1.07, 1.23 | ||
| 26–50 | 1.01 | 0.94, 1.10 | ||
| >50 | 1.0 | |||
| Surgeon volume‡ | ||||
| 1–5 | 1.24 | 1.15, 1.34 | 1.21 | 1.12, 1.32 |
| 6–12 | 1.09 | 1.02, 1.18 | 1.08 | 1.00, 1.17 |
| >12 | 1.0 | 1.0 | – | |
Hazard ratios obtained from bivariate Cox proportional hazards models. †Hazard ratios obtained from multivariate Cox proportional hazards model. N = 49,136 for the multivariate model.
Listed volumes indicate only Medicare patients who had total hip replacement.
Multivariate Analyses of Revision Risk
Multivariate analyses included all of the independent variables listed in Table I (patient age, sex, race, Medicaid eligibility, and comorbidity and hospital and surgeon volume). The results of these analyses (Table II) showed that younger patient age (sixty-five to seventy-five years [HR, 1.47; 95% CI, 1.37, 1.58) was associated independently with increased revision risk after adjusting for all other variables, as was male sex (HR, 1.23; 95% CI, 1.15, 1.31) and having surgery performed by a low-volume surgeon (fewer than six total hip replacements per year compared with more than twelve per year [HR, 1.21; 95% CI, 1.12, 1.32]). We did not observe a significant interaction between the association of surgeon volume and either patient age or sex on the risk of revision. The hazards for the three strata of surgeon volume differed significantly in the first eighteen months after total hip replacement, with patients of surgeons with the lowest volume having the greatest risk of revision (HR, 1.65; 95% CI, 1.39, 1.97). The hazards did not differ across volume strata over subsequent follow-up.
The competing risk models confirmed the results of the primary analysis, identifying the same principal predictors of revision risk as the primary analysis—younger patient age, male sex, and lower-volume surgeon. Detailed results of the competing risk models are presented in the Appendix.
Discussion
We examined the risk of revision following a primary total hip replacement in a cohort of 51,347 Medicare beneficiaries who had elective primary total hip replacement between July 1995 and June 1996. Men had higher rates of revision than women, and younger patients (those who were sixty-five to seventy-five years old at the time of primary total hip replacement) had a higher rate than older patients. The risk of dying over the twelve-year follow-up period far exceeded the risk of revision, especially among the cohort of patients over seventy-five years old at the time of primary total hip replacement, for whom the risk of death over the twelve-year follow-up was tenfold greater than the risk of revision.
Our data are consistent with other literature showing an increasing risk of revision associated with younger age and with male sex2,7,19. Also, as we showed previously, the risk of revision was highest in the first eighteen months after surgery, likely reflecting early technical failures10. The influence of surgeon volume on the risk of revision occurs in the first eighteen months postoperatively and not thereafter, suggesting that surgeon experience influences the risk of technical failure but not the risk of failure over the longer term, which likely reflects intrinsic limitations in implant durability. The association of surgeon volume with early failures is similar for younger and older patients, and for men and women. We note that the surgeon volumes in the present report reflect procedures performed in Medicare beneficiaries. Approximately two-thirds of primary total hip replacements are performed in Medicare recipients, and the other third in patients less than sixty-five years old1. Thus, the Medicare volumes reported in this paper can be multiplied by 1.5 to provide a rough estimate of total volumes for the average surgeon. This simplification may not be valid for particular surgeons. Because older patients are at high risk of morbidity and mortality, competing risks may distort estimates of revision risk. We performed analyses that took competing risks into account; these sensitivity analyses largely confirmed the findings of the primary analyses.
The consistent differences in failure rates seen between younger and older patients and between men and women (Fig. 1-A) raise the question of whether shorter follow-up periods could be used to assess differences in implant performance rather than the longer (twelve-year) periods of observation utilized in this study. Such a strategy would be less resource-intensive than twelve-year follow-up. This idea cannot be addressed directly by our study and merits further investigation. However, since surgeon practices may influence early failures, while implant and patient characteristics influence the later ones, this strategy may not capture risk profiles over time accurately.
The study has important limitations. First, ICD-9 coding does not distinguish between right and left-sided procedures. Up to 30% of the revisions that occur following primary total hip replacement are performed on the contralateral side, even with censoring of patients who had a second primary total hip replacement during the follow-up period12. The likelihood that the revision is performed on the index compared with the contralateral hip is not influenced by patient age or sex or surgeon volume, the three factors associated with revision risk in this analysis12. However, the revision risks shown in Figures 1 and 2 may be overstated by as much as 30%, and the misclassification may have blunted the associations we observed. Further, censoring the data on patients who had a contralateral primary total hip replacement over the period of follow-up may have inadvertently undercounted some bona fide revisions of the index hip. The more general point is that administrative data contain relatively little clinical information, and ICD-9 coding does not convey nuanced clinical information perfectly. These issues create important limitations in the inferences that can be derived from studies that are based on administrative data. Thus, our findings must be confirmed in studies that retain the national scope of this analysis but overcome the ambiguities of administrative data.
Second, revision arthroplasty is an ambiguous proxy for total hip replacement failure. Revision requires that surgery be offered to and accepted by the patient. Some patients with symptomatic loosening of the prosthesis may be too sick or frail to undergo surgery, others may simply not present for care, and still others may be offered revision total hip replacement but prefer not to undergo the surgery. Consequently, actual rates of symptomatic failure of total hip replacement are likely to be higher than observed revision rates.
Third, while the length of follow-up is a strength of this study, it also means that the index procedures were done in the mid-1990s. Implant technology, surgical technique, and rehabilitation practice have evolved over the subsequent years. It is conceivable that the associations between covariates and revision documented in these analyses may have been altered because of changes in implant technology and the process of care occurring over the last fifteen years.
The observation that patients over seventy-five years of age undergoing primary total hip replacement face a tenfold higher risk of death than of revision over the subsequent twelve years has important implications for patient decision-making, quality improvement, and research. From a decision-making standpoint, these older patients should place revision risk in perspective as they discuss the advantages and drawbacks of total hip replacement with their physicians. Because they face a 60% risk of death over the next twelve years, their absolute risk of revision is just 6%. Patients in the sixty-five to seventy-five-year-old group face a somewhat higher absolute risk of revision—approximately 10%. By extension, patients less than sixty-five years old (and especially those in their fifties) face still higher absolute risks of revision over a ten to twenty-year time frame.
The observation that patients who have total hip replacement after the age of sixty-five years are much more likely to die than to have a revision total hip replacement points to the importance of optimizing short-term outcomes of total hip replacement in the elderly, such as complications and restoration of function. Long-term survival data on implants, as can potentially be obtained by longitudinal joint replacement registries, will be of particular value in assessing and optimizing the outcomes of younger patients who are much more likely to live long enough to face possible revision surgery.
Further study of the predictors of revision in younger patients would provide a more quantitative assessment of these trade-offs and should be a research priority. These observations also impact the optimal frequency with which to monitor patients with radiographs following surgery. Finally, our findings suggest that the development of innovative technologies to improve implant longevity should target younger populations with advanced arthritis, who have a longer anticipated time span in which the implants might fail and require revision arthroplasty.
Appendix
Tables showing the incidence and average time for each event type and the results from models adjusting for competing risk are available with the online version of this article as a data supplement at jbjs.org.
Supplementary Material
Disclosure of Potential Conflicts of Interest
Tables showing the incidence and average time for each event type and the results from models adjusting for competing risk
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1. United States Department of Health & Human Services. HCUP nationwide inpatient sample. 2009.
- 2.Hallan G, Lie SA, Furnes O, Engesaeter LB, Vollset SE, Havelin LI. Medium- and long-term performance of 11,516 uncemented primary femoral stems from the Norwegian arthroplasty register. J Bone Joint Surg Br. 2007;89:1574-80 [DOI] [PubMed] [Google Scholar]
- 3.Mäkelä K, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. Cemented total hip replacement for primary osteoarthritis in patients aged 55 years or older: results of the 12 most common cemented implants followed for 25 years in the Finnish Arthroplasty Register. J Bone Joint Surg Br. 2008;90:1562-9 [DOI] [PubMed] [Google Scholar]
- 4.Mäkelä KT, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. Total hip arthroplasty for primary osteoarthritis in patients fifty-five years of age or older. An analysis of the Finnish arthroplasty registry. J Bone Joint Surg Am. 2008;90:2160-70 [DOI] [PubMed] [Google Scholar]
- 5.Espehaug B, Furnes O, Engesaeter LB, Havelin LI. 18 years of results with cemented primary hip prostheses in the Norwegian Arthroplasty Register: concerns about some newer implants. Acta Orthop. 2009;80:402-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hailer NP, Garellick G, Kärrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthop. 2010;81:34-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnsen SP, Sørensen HT, Lucht U, Søballe K, Overgaard S, Pedersen AB. Patient-related predictors of implant failure after primary total hip replacement in the initial, short- and long-terms. A nationwide Danish follow-up study including 36,984 patients. J Bone Joint Surg Br. 2006;88:1303-8 [DOI] [PubMed] [Google Scholar]
- 8.Pedersen AB, Svendsson JE, Johnsen SP, Riis A, Overgaard S. Risk factors for revision due to infection after primary total hip arthroplasty. A population-based study of 80,756 primary procedures in the Danish Hip Arthroplasty Registry. Acta Orthop. 2010;81:542-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conroy JL, Whitehouse SL, Graves SE, Pratt NL, Ryan P, Crawford RW. Risk factors for revision for early dislocation in total hip arthroplasty. J Arthroplasty. 2008;23:867-72 [DOI] [PubMed] [Google Scholar]
- 10.Losina E, Barrett J, Mahomed NN, Baron JA, Katz JN. Early failures of total hip replacement: effect of surgeon volume. Arthritis Rheum 2004;50:1338-43 [DOI] [PubMed] [Google Scholar]
- 11.Katz JN, Losina E, Barrett J, Phillips CB, Mahomed NN, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2001;83-A:1622-9 [DOI] [PubMed] [Google Scholar]
- 12.Katz JN, Wright EA, Baron JA, et al. Predictive value of Medicare claims data for identifying revision of index hip replacement was modest. J Clin Epidemiol. 2011; 64:543-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-83 [DOI] [PubMed] [Google Scholar]
- 14.Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol. 1993;46:1075-9, 81-90 [DOI] [PubMed] [Google Scholar]
- 15.Mahomed NN, Barrett JA, Katz JN, Phillips CB, Losina E, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Rates and outcomes of primary and revision total hip replacement in the United States Medicare population. J Bone Joint Surg Am. 2003;85:27-32 [DOI] [PubMed] [Google Scholar]
- 16.Pepe MS, Mori M. Kaplan-Meier, marginal or conditional probability curves in summarizing competing risks failure time data? Stat Med. 1993;12:737-51 [DOI] [PubMed] [Google Scholar]
- 17.Pintilie M. Competing risks: a practical perspective (statistics in practice). West Sussex, England: Wiley; 2006 [Google Scholar]
- 18.Fine JP GR. A proportional hazards model for the subdistribution of competing risk. J Am Statist Assoc. 1988;94:496-509 [Google Scholar]
- 19.Corbett KL, Losina E, Nti AA, Prokopetz JJ, Katz JN. Population-based rates of revision of primary total hip arthroplasty: a systematic review. PLoS One. 2010;5:e13520 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest
Tables showing the incidence and average time for each event type and the results from models adjusting for competing risk


