Abstract
The United States has set a national goal to eliminate health disparities. This article emphasizes the importance of food systems in generating and exacerbating health disparities in the United States and suggests avenues for reducing them. It presents a conceptual model showing how broad food system conditions interplay with community food environments—and how these relationships are filtered and refracted through prisms of social disparities to generate and exacerbate health disparities. Interactions with demand factors in the social environment are described. The article also highlights the separate food systems pathway to health disparities via environmental and occupational health effects of agriculture.
Keywords: health disparities, public health, agriculture, access to food, healthy foods, sustainably produced food, Farm Bill
INTRODUCTION
The United States has set a national goal to eliminate health disparities.1 This article reviews literature describing how food systems generate and exacerbate key health disparities in the United States. The article is framed around a new conceptual model describing a set of pathways by which food systems may affect health and increase health disparities. It highlights promising directions for future research and policy to address and shift these pathways.
A food systems approach begins with the recognition that the roots of health disparities include but go deeper than individual choice, nutrition, or price. They reach outwards to community factors like access and deeper to broad social, economic, and political forces that impact food supply, nutrient quality, and affordability. Further, some of the health disparities are driven by the environmental and social impacts of food production and processing. The roots and pathways are not linear but rather reflect complex processes and feedback loops such as that of consumer demand. This article relies on a series of definitions:
Health disparities refer to the gaps in health status (e.g., life expectancy, infant and maternal mortality rates, obesity and diet-related disease, and other measures) among groups of people based on differences in factors such as socioeconomic status (SES), race, ethnicity, immigration status, environmental exposures, gender, education, disability, geographic location, or sexual orientation.1
Food systems are systems comprised of all of the processes involved in getting food from farm to table to disposal, including production, processing, distributing, preparing, marketing, accessing, consuming, and disposing. Food systems also involve people, farms, businesses, communities, interventions, policies, and politics.2–4
Healthy food: although there is no single accepted definition, generally we use the term to refer to food high in nutrients and low in calories, fats, sodium, and additives/processed ingredients—particularly fruits and vegetables (FV) that are among the foods encouraged in the Dietary Guidelines for Americans.5
Good food: as defined by the W.K. Kellogg Foundation, is food that is “healthy, green, fair and affordable.”6
Strong evidence ties racial/ethnic and socioeconomic disparities to diet quality or diet healthfullness7–11 and to obesity and diet-related disease.12–15 For example, nationally African Americans die from stroke (age-adjusted) at 146% of the white rate; of heart disease at 131% the white rate; and of diabetes at 208%.16 Beyond eating foods that are high in essential nutrients, there are differences in ability to access calories altogether. An estimated 11.1% of Americans have “low food security” and 4.1% have “very low food security” with African Americans and Latinos estimated to have double the national rates.17 In the United States, food insecurity has been found to be highly correlated with obesity.18
In contemporary US society, and within professional and research communities, diet has primarily been considered at the individual level, and interventions to improve diets and related health outcomes have largely targeted individual knowledge, attitudes, and behaviors.19–23 We describe extensive evidence that multiple social-level and community-level factors— both in food systems and in social disparities—constrain and affect the choices individuals make. Accordingly, focusing exclusively on individual behavior in the absence of larger systemic changes may not only be less effective or ineffective, but it can also result in victim-blaming.21,23 A food systems approach supports attention to multilevel strategies for addressing food system health risks and disparities. Such an understanding is critical in designing and implementing effective interventions, including those primarily targeted at individuals, communities, broad food systems, or multiple levels at once.
Food systems’ impacts on health disparities also go beyond the “eating” pathway. Low-income, minority, and immigrant communities also suffer from high exposure to occupational24–29 and community30,31 health threats associated with food production and processing methods.
In discussing food-related health disparities, it is critical to highlight the concept of the human right to adequate food. As defined by the United Nations, the right includes the adequacy of the food supply as determined by nutritional adequacy, access, food safety and quality, and cultural acceptability; and the stability of food supply and access as determined by environmental sustainability and social sustainability. The rights framework emphasizes the right to be able to obtain one's own food more than the right for government to provide food; but where such need arises, a framework in human rights shifts the dialogue from that of perceived charity to governmental obligation. Thought the United States has thus far refused to be bound by “right to adequate food” principles, it did sign on to United Nations (UN) Voluntary Guidelines endorsing a similarly broad approach.32 This article does not discuss the right to adequate food at length; however, these concepts undergird our analysis.
METHODS
To conduct this review, an outline of key topics was developed. To identify well-conducted and widely cited studies on topics of concern, as well as data from government and other established sources, searches were performed in databases including PubMed, Scopus, and Google Scholar between October 2008 and March 2009. Further, using a “snowballing” approach, other references were identified based on literature cited within reviewed articles. Some of the covered topics were extensively addressed in the literature, with the findings synthesized in current literature review papers. In these cases, we relied primarily on the existing reviews, supplemented with seminal or particularly strong articles for examples. For a few topics, there was minimal available evidence in the peer reviewed literature, and “grey literature” articles of reasonable quality had to be utilized. These were identified via author knowledge, the Google search engine, and snowballing approaches.
CONCEPTUAL MODEL
Complementing the human rights approach to adequate food, we present a new conceptual model (Figure 1) that illustrates how food systems influence health and contribute to health disparities. The model uses a systems framework directing attention to the interrelatedness of factors at different levels and to important feedback loops such as supply and demand.
FIGURE 1.
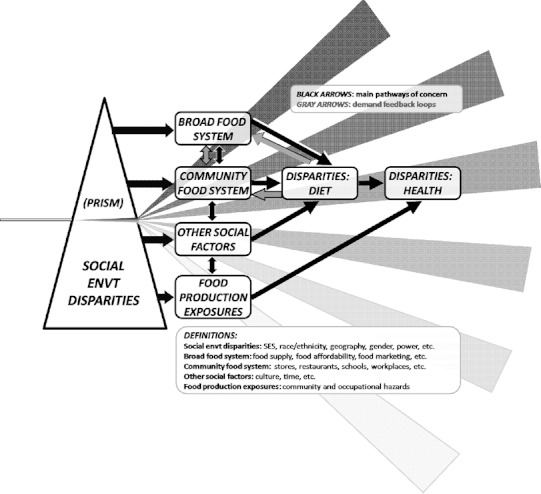
Concept model: food systems and health disparities.
The concept model shows how broad food system conditions (including: food supply—what is produced and how it is produced, and food affordability—both price and the food safety net; and marketing) interplay with the food systems and food environments operating in communities (stores, restaurants, schools, workplaces, and local policy). It shows how these in turn have reciprocal relationships with other factors in the social environment (including culture and time), to affect individual propensity to eat a healthy and sustainable diet. The model uses the metaphor of prisms that refract single beams of light into spectra. In the model, prisms of disparities in the social environment (including by SES, race/ethnicity, geography, gender, and power) refract the entire set of relationships, so that different sectors of society may vary widely in the types and quantities of food they are most likely to find available, affordable, and culturally acceptable. These processes are iterative and interactive.
Through “feedback” loops shown in grey, disparities in individual and community likelihood of obtaining good food can affect the extent to which such foods are made available either in certain communities or society wide. For example, some storekeepers report reluctance to stock healthier food choices, citing one reason as the perceived low demand for those foods in their communities.33 Another example is that increasing knowledge about food system concerns among college students has led to a level of demand for more sustainable campus food that has caused large institutional food providers to change their offerings.34
Individual food choices and the psychosocial factors that affect them of course vary within and between communities. Demographics are not destinies. However, the factors described above may contribute to aggregate-level disparities in healthfulness of preferences and choices.
The graphic implies a list of potential sites for intervention by targeting each point where there is an arrow. Many interventions to change the food system/health relationship fall into two broad categories: those using population-based strategies, aimed at changing factors affecting the entire population; and targeted strategies aimed at changing the food system exposures or food demand within specific sectors of the population. It is important to recognize that though a rising tide may lift all boats, and population-based public health interventions may improve conditions for all, they can simultaneously increase health disparities. In particular, efforts using new information or technologies may have this paradoxical effect. As Paul Farmer has observed, the group that starts out healthier is often better educated with more resources and is therefore more likely to use new technology or information more rapidly and effectively, thus experiencing a greater gain in health status than those with poorer health, less education, and fewer resources.35,36 Figure 2 dramatizes this concept. It contrasts a targeted intervention, which may increase good food consumption for the specific targeted population but have little effect on others, with a population-based intervention, which may slightly improve outcomes across the board but have the strongest effect on those most likely to engage with it, thus ironically increasing the disparity.
FIGURE 2.
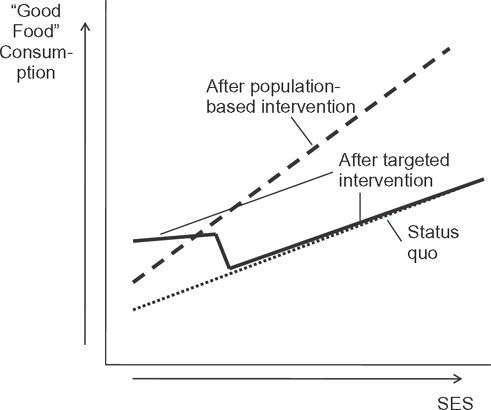
Population-based interventions may increase health disparities (hypothesized).
We also highlight a separate food system/health pathway outside of food consumption: the environmental and occupational health impacts of the industrialized food system are also filtered through prisms of disparities, leading to differential community and occupational exposures. This article spends less time on this pathway than on some others.
ELABORATING THE PATHWAYS
Broad Food System
In this section, we discuss how the broad food system factors of supply and affordability affect health disparities.
Food supply—What is produced, how it is produced
The US food supply has changed since 1970. The contours of the food supply contribute (along with other factors) to the relatively poor diet quality among Americans, including underconsumption of vegetables, fruits, and whole grains, concurrent with overconsumption of sugar/sweeteners, oils and fats, red meats, refined grains, and processed foods.37–40 Indeed, a federal study showed that US agricultural production would need to change substantially to enable the population to eat according to USDA dietary recommendations.40 Here, we focus on how the contours of the US food supply and its production (and the policies and power that shape them) may contribute to health disparities.
First, food system policy has affected the content of the food supply. Such policy is driven by financial and political power in the food system, including agribusiness and food processing lobbies.41,42 Historically, US Farm Bill policy aimed to assure food availability and stabilize prices for consumers and farmers by managing supply. But since the 1970s, the policy goal has been to reduce prices and increase supply of key commodity crops including corn and soybeans.38 Contrary to common intuition, economic evidence has not clearly shown that subsidies directly lower consumer prices to the extent purchasing is likely affected.43–47 However, due to the low prices for key items promoted through farm policy, manufacturers have had an incentive to use these items as ingredients in processed foods—and to concentrate marketing resources on such items with relatively high profit margins.38 These low-cost commodity items have also contributed to the proliferation of industrial food animal production and consequent low prices of retail meat. (As commodity prices have escalated, driven by ethanol production, oil prices, and other factors, industrial producers of animals have suffered and some animal product prices have risen for consumers. The impact on processed food producers has been smaller, owing in part to the relatively small percentage of processed food costs comprised by the commodity products.) There is no comparable incentive for production, manufacturing, or marketing of healthier food items, such as fruits and vegetables.
As will be discussed in other sections, it is lower income, ethnic minority, less educated, inner-city, and/or rural communities that are especially likely to have their available food options dominated by these mainstream and less healthy offerings. This is due to a combination of physical, social, and economic access as well as marketing and cultural factors. If the mainstream food supply were healthier and produced more sustainably, and if the economic and legal incentives for food production, manufacturing, marketing, and sales were shifted to promote a healthier food supply overall, prices, access, and social norms might change, and some diet-related health disparities might be reduced. Possible impacts might be most apparent among communities that consume the most mainstream and heavily marketed food and foods that are made most affordable through current food system policy.
Second, within the food system, there are disparities in access to sustainably produced food such as organic FV. Much more research is needed to understand possible health impacts from consuming sustainably produced foods. A literature review by the Organic Center identified evidence suggesting some nutritional benefits of organic foods versus conventional, including in the areas of antioxidants and total polyphenols48; an alternate review of the same literature by the UK Food Standards Agency suggested no nutritional differences, although it excluded examination of antioxidants and reviewed polyphenols differently.49 Both studies found increased nitrates in conventional produce, which are linked with negative health effects. Sustainably produced foods may also result in reduced chemical exposure via pesticide residues. At least as importantly, the consumers may also feel emotionally positive about cobenefits such as rebuilding the soil, preserving water supplies, promoting local economies and civic connections, mitigating climate change, and contributing to greater food system resilience—and thus may be motivated to eat more produce.48,50,51
However, more sustainably produced food tends to cost more at the retail level than conventionally produced food, due to higher production costs, lack of centralized distribution infrastructure, relative lack of government support, the costs of industrial production that are externalized (put onto others), and, often, fewer economies of scale. As discussed below, despite these higher costs, some evidence suggests broad interest in and significant spending on food produced with fewer chemicals among low-income and minority populations.52 Improved investment in sustainable agriculture and food processing research, farm support, marketing, and distribution networks could further increase affordable access to sustainably produced foods.
A third way that broad food system factors and the overall food supply may affect health disparities is through macro, long-term influences on domestic and global food prices. Though US farm policy aims to drive prices down, it has led to instability and, at times, price shocks that can hit the poor hardest. The constancy of the US food supply and of the prices within it are also affected by factors including social and economic conditions, agricultural and trade policies, production technologies, and environmental conditions.53–55 Converging ecological crises of climate change, and of water, soil, and fossil fuel depletion, are likely to contribute to long-term reductions in agricultural supply and substantial price impacts. Even such seemingly unrelated factors as biofuel production and commodity speculation in financial markets are shown to have had important impacts on supply and prices.56,57 These price and supply impacts may be expected to hit hardest for consumers with low incomes—not to mention agricultural producers and low-income rural communities.
Fourth, there is alternately a possibility that these threats and resultant dislocations or incentives might motivate at least a partial relocalization of food production and a turn toward more ecologically sustainable agriculture methods. It is also possible that new “green” investments in response to crises could help make such options increasingly available across socioeconomic strata. Improving access to healthy, local, sustainably produced food also supports building the infrastructure needed to scale up good food production for all, including rebuilding the local food economy to serve the citizens within their respective regions.51 Some evidence suggests not only that community gardening increases food access, but that it also may positively influence diet and social connection.58,59 As the economic downturn worsens, the trend toward “grow your own” appears to be increasing,60 although it must be recognized that growing one's own food takes time, water, usable soil or space, skills/training, and startup resources.
Finally, we note that US farm policy and the food system it supports have been sustained in part by historic alliances between agricultural and anti-hunger lobbies and the rural and urban legislators with whom they work. Anti-hunger lobbies have focused traditionally on access to calories through food stamps and commodity food programs. It is possible that new coalitions could contribute to an altered political calculus for future farm bills by supporting not only these food access programs but also efforts to address disparities via access to and affordability of healthy and sustainably produced food and via reducing hazardous agricultural exposures.
Food affordability: Price, food assistance, and emergency food
Price. Consumers describe price as a key factor in food purchasing decisions, and price elasticity is greater the more limited the household budget.61 Controlled analyses of factors in purchasing decisions have found that cost is significantly more important among lower-income and among non-white compared to higher income and white respondents.62,63
Low-income persons typically must spend greater percentages of their incomes to buy food than others, although they spend less money overall.64 Many studies dating at least to the 1960s have examined the question of whether the poor pay more for the same food basket. A 1997 review article64 and a more recent study65 found that the poor did pay more than others, although the differentials were small. Another study found slightly lower prices in lower-income areas.66 The evidence is mixed regarding whether accounting for suburban/urban/rural status and store type (smaller and non-chain stores cannot obtain the economies of scale of larger stores67) would wash out any poor-pay-more price differential. The results may vary by area. Further clarification may help guide interventions addressing health disparities via the food system.
Evidence that the higher price of healthier foods contributes to poor diets among lower-income populations is growing. In general, nutrient-dense foods like FV are more expensive than energy-dense foods with relatively high sugar and fat content.61,68–72 As suggested above, this price differential may be partly fueled by agriculture policy incentives.38 The effective price differential for energy-dense foods is further increased due to longer shelf life.73 Some studies suggest that it is possible to eat a nutrient-rich diet at comparable cost to an energy-dense one,74 and some observers have noted that though unhealthy foods may be less expensive per calorie, healthier foods can be less expensive and more filling on a per meal basis than pre-prepared alternatives.75 Others argue that for many, this change may require considerable new knowledge and effort, as well as departures from flavor preference, familiarity, and cultural/social norms.70
Powell and Chaloupka76 reviewed the literature on price interventions to address obesity and overweight, specifically taxation (increasing the price of unhealthy goods through a sales tax) and price subsidies (decreasing the cost of healthier items, in this context FV). They found that decreasing the price of healthy products (which are more price elastic) tends to be more effective than increasing the price of unhealthy products. Their review states that though a range of price points were associated with health outcomes, larger price changes in particular had “a measurable effect” on weight, especially among youth, those with low SES, and those at particular risk for overweight. A USDA study concluded that if FV prices were subsidized by 10%, fruit consumption among low-income Americans would rise by 2.1% to 5.2% and vegetables by 2.1% to 4.9%—a substantial rise, though still leaving consumption well below the USDA's recommended dietary allowance.77
Taxing unhealthy foods and beverages is regressive. Some argue that these regressive taxes may be acceptable because they could have greater benefits for lower-income individuals than others. Public support increases if the funds raised are used to support obesity prevention; using them to increase access to healthy foods is a particularly direct way to address the regressiveness.78 Brownell and Frieden suggest that adding a 1 cent per ounce excise tax could result in a 10% reduction in sugar sweetened beverage consumption.78
Much more research is needed to examine in detail the public health impacts of varying price strategies for different foods, in different contexts, and for different consumer groups.
Food assistance and emergency food. The inability to afford adequate, nutritious food can exacerbate the health disparities linked with food deprivation and can have multigenerational effects. The food safety net is a necessary response in this society. Here, we focus on the two largest US assistance programs, the Supplemental Nutrition Assistance Program or SNAP (previously known as food stamps), which provides financial assistance for food purchases based on economic need; and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), which provides vouchers for healthier foods to children and pregnant women. We examine program reach, adequacy, and nutrition.
How adequate is coverage for reaching eligible populations and providing sufficient, nutritious food? There are important noncovered populations, including new and undocumented immigrants. Even among those eligible based on income, health, and other criteria, SNAP and WIC reached only about two thirds and half of the eligible.79,80 Barriers to participation include not knowing of eligibility, stigma, and negative attitudes toward using government benefits and administrative requirements versus the amount of benefits.81
Among those who do access the programs, evidence suggests that the programs fall short of covering food costs, although they do increase the ability to afford food; and that they improve nutritional well-being, particularly for children.82–85 There are concerns that the cyclic food scarcity in the monthly SNAP program may contribute to obesity. When benefits run out at the end of each month, there may be little to eat, particularly for women, who may forego food to assure that their children can eat73 or turn to cheaper, readily available processed foods high in fat and sugar. When food stamps are again available, biological and psychological drives may promote overconsumption, the weight gain effects of which can be increased through slowed metabolism.18 Changed payment schedules merit further exploration.
A vibrant area of program development and study involves efforts to incentivize dietary choices through food assistance programs. For example, starting in Fall 2009, WIC clients will receive monthly FV vouchers for grocery stores and in some states, farmers’ markets. Such initiatives are a step forward and in some cases effectively double purchasing power, though the voucher dollar values remain fairly low (e.g., $10 in San Diego).86
Though food assistance programs provide funding, emergency food programs provide food; a food systems approach includes assessing what food is made available. USDA-provided agricultural commodities, provided below cost, comprise one fifth of federal dollars spent on school lunch and are also a substantial component of the Emergency Food Assistance Program (TEFAP).87 Though the food provided is often relatively unhealthy, many food programs have been so underfunded that they continue to rely heavily upon this source, although this may be changing.88 The programs also benefit commodity growers by assuring markets for their surplus and have contributed to powerful urban-rural alliances supporting the status quo on commodity subsidies in food and agriculture policy. Similarly, many emergency food programs rely substantially on surplus food from supermarkets, manufacturers, and other sources, and this food is often of an unhealthy variety. For example, the Maryland Food Bank routinely dispenses soda and candy to hungry families. Generally speaking, emergency food programs provide relatively few fresh FV, due to cost, shelf life, shipping/refrigeration costs, and seasonality.
Observers including Winne,89 Poppendieck,90 and Berg91 powerfully question the charitable anti-hunger sector at its core, due to the “codependencies” it fosters, the “ideology of voluntarism” as opposed to governmental obligation as part of commitment to the human right to adequate food, and, most fundamentally, the fact that they distract the energy of those who could be working to change the root causes of hunger, such as poverty.
Beyond formal food assistance programs, lower-income families rely on backup strategies including growing, subsistence hunting, trapping or fishing, family and friend networks, faith-based and community organizations, and store credit. Further research and policy development are needed to understand prevalence and processes of different compensation strategies, to identify policies that can facilitate positive arrangements, and to protect individuals from potential negative effects, from food safety threats to familial power imbalances to loss of access to credit as small stores are replaced by large ones.92–94
Food and beverage marketing
In 2008, the industries spent $7.82 billion on food and beverage marketing and $5.62 billion on restaurant marketing, representing 15% and 28% increases since 2004.95,96 Marketing may affect perceptions, knowledge, and behaviors not only by promoting particular items, brands, and categories of food but also by promoting social identification and positive associations with brands. The impacts of marketing may operate through pathways including environmental cues to action without intervening knowledge or attitude change and promotion of gratification behaviors.97 Such marketing can also create a false impression that certain foods are culturally appropriate and others not. Marketing decisions and strategies are primarily driven by economics and profit; the public's health is not a significant consideration.98 Given the above-described economies food corporations can obtain by producing processed foods with low-cost subsidized ingredients, it is not surprising that these relatively unhealthy foods are heavily marketed.
Audience segmentation in content and placement is a basic tenet of marketing, but to the extent the practice is effective in greater promotion of unhealthy foods in some communities than others, it can lead to behaviors and norms that exacerbate health disparities. Yancey et al99 found that disparities in placement of outdoor food and beverage marketing may contribute to behaviors that increase risk for obesity. Studies have also found that more food commercials aired during “African American” shows than others, and that the distribution of items advertised was more heavily skewed toward unhealthy items.100,101 Additional research shows that low-income children watch more television and have greater media exposure—and thus more exposure to food commercials—than their higher-income peers.102 When the US Federal Trade Commission compelled 44 major food companies to provide food marketing data, only half stated that they did not target advertising based on gender, race, and ethnicity. Many of the remaining half do; numerous examples are provided in the report.103
Few interventions and policies are specifically developed to reduce differential food marketing by race/ethnicity. Possible approaches include zoning changes, counter-advertising, marketing guidelines,99 “shaming” the advertisers publicly, media literacy education,102 and even legal challenges on civil rights and right to health grounds.
Community Food System
There is a strong, growing, and well-reviewed literature describing reduced physical access to healthy food in low-income and minority communities, both urban and rural.104–107 This literature fits into wider bodies of literature identifying US residential segregation and neighborhood-level health disparities. We discuss the following community food environments: stores and direct to consumer marketing; restaurants; schools; and workplaces. We also discuss community food policy interventions. Other community nutrition interventions, such as Meals on Wheels or senior citizens’ meal programs, are not discussed here.
Stores and direct to consumer markets
Stores. Literature generally shows that compared to smaller stores, supermarkets stock a greater selection of produce and healthy food items and generally have lower prices due to economies of scale and, often, to competition. Supermarkets have been moving out of inner cities since the 1960s, following the movement of wealthier populations to the suburbs.108,109 USDA data suggest that by 2011, 40% of US food sales may occur in “non-traditional grocery stores” including discount stores, drug stores, and mass merchandisers.110
Though literature is mixed, most studies have found that predominantly minority, low-income, and rural communities are particularly likely to face low access to supermarkets, chain supermarkets, and healthier foods.64,104–106,111,112 A 2009 USDA national analysis also emphasized the importance of income inequality and racial segregation.106 Studies have found that corner stores and other sites in low-income areas tend to offer an abundance of processed foods and few fresh items, whereas healthier food is generally more available in white than in non-white communities.104–106
Physical access is an important factor because though it is often possible to travel farther for healthier food options and lower prices, the travel may be particularly inconvenient for those with lower incomes, due to transportation and other barriers.73,113 Neighborhood crime levels might also be a concern, affecting safety and limiting the shopping options some consumers are willing to use. Some consumers shop in multiple stores at varying distances based on price, convenience, and other—not well-studied—factors.73,113,114 For example, a community food assessment in Baltimore found that on average, respondents spent $280/month at supermarkets and $140/month at corner stores, making many more trips to the latter.115
Relatively few studies have directly examined the association between healthy food access and healthy food consumption,116 but most find such associations for both supermarket access and level of healthy foods in community stores. For example, Franco et al., using direct observation within stores and a large population sample, found that even after adjusting for age, sex, income, and education, people in areas with the lowest category of food availability had a significantly less healthy diet.117 Finally, a small literature completes the circle, directly associating food access and store type with health differentials. In published reviews, studies generally showed lower rates of obesity associated with increased supermarket access (although there were some inconsistencies) and the converse for convenience store access.104,107
There are several case studies of chain supermarkets opening in underserved areas with positive impacts on the community and thriving sales for the stores.118 Though few examined public health impacts, one that did is Wrigley et al.119 They found a small increase in FV servings per week, with the most increase among those with the poorest initial diets.
One of the largest programs to bring food stores to low-income and minority communities is Pennsylvania's Fresh Food Financing Initiative (FFFI), now being replicated elsewhere. FFFI, with both public and private funds, created a $120 million financing pool dedicated to increasing supermarket development and rehabilitation by providing grants and loans. Over 52 projects have been funded, resulting in an additional 1.3 million square feet of retail space. Evaluation plans are underway.120 Increasing the number of supermarkets is costly and takes years to implement. Other initiatives work to modify environments in existing food stores to influence availability and encourage healthier food choices. A review of interventions aiming to improve conditions in food stores found mixed results. Point-of-purchase interventions (generally in-store marketing or education materials) often improved consumer knowledge, but that did not always translate into healthier food choices.121 Most evaluations did not include control stores. An examination of initiatives in several supermarkets found that increasing size of the produce display substantially, such as to 200% of original size, increased produce sales from 28% to 59%.122
Efforts to bring healthier foods into corner stores in low-income and underserved communities around the country are supported by networking in the national Healthy Corner Store Network (HCSN). One of the few corner store programs with robust evaluation results is Baltimore Healthy Stores (BHS). That program, developed based on extensive formative research on social and cultural context, works with store owners to increase healthy food options, conduct food demonstrations and taste tests, change the physical location of food items, offer price incentives, and identify healthy products. The program resulted in significantly higher sales of promoted foods. Six months after the program, at-home healthy food cooking was significantly increased in the intervention area, and nonsignificant results suggested continued healthy food stocking and changes in store owner expectations and self-efficacy.123
Direct to consumer marketing. Direct-to-consumer marketing, including farmers’ markets and community-supported agriculture, is growing rapidly in the United States. The number of farmers’ markets grew from 1755 in 1994 to 4685 in 2008, making it one of the fastest growing alternative food sale venues.124 Efforts to improve access to healthy and sustainably produced food through farm to consumer marketing have generally not been well evaluated; there are few references in the peer-reviewed literature.125,126 Below, we describe 3 main types of intervention.
First, interventions to establish farmers’ markets in areas convenient to low-income and minority consumers have been implemented in numerous areas. These projects are often challenged by high startup costs and, unfortunately, they frequently fail.127 Community engagement in the process, community financial ability to start a market, and strategic location choice appear to be important. One successful example is the Food Trust in Philadelphia, which runs 14 farmers’ markets around the city, mostly in low-income areas. Costs are subsidized by markets in other areas with higher-income clientele. In their 2007 evaluation, 49% of respondents reported increased FV intake since shopping at the markets, and of that group, 30% stated that their FV consumption increased by one to two daily servings.120
Second, interventions to make farmers’ market produce more affordable are also proliferating. For example, the farmers’ market nutrition programs (WIC and seniors) provide coupons to incentivize consumers to use these markets and were further expanded in the 2008 Farm Bill.128 One evaluation found that participants in the farmers’ market nutrition program consumed more vegetables than WIC participants.129 Another recent study found that subsidizing fruit and vegetable purchases for WIC participants increased the number of servings by 1.4 compared to the control group and those changes were sustained 6 months after the intervention ended.130,131 A similar increase (1.4 servings) in fruit and vegetable consumption was found in a program that used home delivery for the seniors’ farmers’ market nutrition program.132 Two earlier evaluations found that the markets were used extensively but did not increase FV consumption; further evaluations are ongoing.121 One key limitation is the small amount of monthly funding provided to consumers; some states are supplementing the federal funds to increase the amounts provided.
Finally, initiatives around the country are working to provide (costly) machines to farmers’ markets to enable them to accept electronic benefits, a benefit both to SNAP and to other community members who use debit or credit cards.133
Restaurants
Compared to food prepared at home, typical fast food restaurant meals have higher energy density, calories, fat, sugars, sodium, and portion size and are relatively low in fruits and vegetables.62,134,135 Heavy consumption of fast food that is high in energy but low in nutrients is associated with higher BMI.136 Though “away” and pre-prepared foods are generally more costly than those prepared at home, they are still consumed at high rates among those with lower incomes134,135,137 and, some evidence suggests, minorities.137
Larson et al found that overall most US studies find more fast food restaurants in low-income and minority areas and healthier restaurants in wealthier areas, although results are not consistent.104,135 Further, the literature generally shows that consuming more restaurant food, especially fast food, is associated with obesity and weight gain. However, findings are mixed regarding the impact of geographic proximity to certain types of restaurants, because living nearby does not equate with eating the food.104
We found few evaluations of interventions to address possible connections between restaurants and health disparities. Only one disparities-specific food environment intervention was identified for this article: the city of Los Angeles placed a year-long moratorium on any new fast food restaurants locating in low-income, high-fast food-density areas. An evaluation is currently underway. The literature does include interventions aiming to change consumer awareness of nutritional and caloric content of restaurant food, primarily through policy. We note, however, that that such changes are positive, they may be of the greatest help to those with higher nutrition literacy and those who are already inclined to seek out such options—and thus that such interventions might even increase disparities. Further research is needed on both the role restaurants may play in health disparities—and on impacts on disparities from restaurant interventions designed to improve the availability or identification of healthy foods.
Schools
School food is significant for providing nutrition and improving food security. Schools are also an important venue to set an example about healthy food and nutrition behaviors. Many schools provide two meals a day. These are subject to federal nutrition standards, although low reimbursement levels constrain the ability to meet them. Particular challenges include reducing fat levels and the levels of fresh FV and whole grains offered.138 Competitive foods (foods sold outside school meal programs) are typically low in nutrient value and highly processed and are not subject to federal regulation.139 Given that competitive foods bring in additional revenue that is especially appealing to struggling school districts, the financial incentives may increase resistance to change in these districts especially and thus exacerbate health disparities.
When the school food environment is altered to promote healthier foods, is there an impact on health? Results are mixed. It is challenging at best to find positive results when distal outcome measures such as BMI are used, due to the many intervening and confounding factors and the fact that students are in school only a portion of the day. Impacts on knowledge, attitudes, and behaviors are often more realistic targets of research.140 One recent paper examined the evidence regarding farm-to-school programs.141 Of the 15 evaluations reviewed, only one examined direct health outcomes using BMI as a measure, and that evaluation found no significant change. Eleven studies looked at dietary behavior changes and 10 of those reported an increase in eating more fresh produce in school. Of the 5 programs that measured consumption outside of the classroom, 4 found that there was an increase. Two programs incorporated classroom nutrition education but only one found that it increased the amount of produce consumption. Two studies found that students were making positive lifestyle changes such as greater physical activity, improved self-esteem, and improved work ethic. Knowledge and attitudes were measured in 4 of the studies and found an increase in students’ understandings of where their food comes from, how to read nutritional labels, and recommendations for daily produce consumption. Overall, there is a need for more evidence about connections between farm-to-school programs and health. Many are viewing these programs as a promising option for increasing children's exposure to fresh produce, a strategy that can have particular benefits among those who otherwise would have relatively little such exposure. School gardens also have a role to play in health promotion and disease prevention and can affect children's relationships with food in a positive way such as increasing willingness to taste new FV.142
To the extent that school-based interventions are positioned to address health disparities, it is generally a matter of implementing programs in schools or areas with many low-income or minority children and engaging culturally appropriate strategies. It is important to recognize that some of the most effective and progressive interventions addressing food in schools also involve the most substantial and costly change and thus can be challenging or unaffordable for many schools in poor neighborhoods. To avoid increasing disparities among schools, across-the-board implementation (following pilot projects) within districts might be recommended.143
Beyond in-school food, the environment surrounding many schools also offers easy access to unhealthy choices. Zenk and Powell144 found that one third of US public secondary schools had fast food restaurants and/or convenience stores within a half mile. Schools in lower-income (vs higher) and predominately white (vs predominantly African American) neighborhoods were particularly likely to be located near food outlets.
Workplaces
Workplace interventions have grown in popularity in part because employers who provide health insurance have seen a significant increase in costs related to diet-related diseases. Progressive companies, primarily larger in size, offer on-site healthy cafeteria choices or interventions such as lowering the cost of healthy foods, improving vending choices, providing nutrition information for cafeteria foods, and e-mailing nutrition education.145 Workplaces can play a key role in reaching at-risk populations that have poor access to healthier foods in their neighborhoods, and poor access to health providers. A supportive environment augmented with coworkers or family also seeking change can serve to increase health-promoting behaviors146,147 and help establish healthier food consumption norms. The vast majority of workplaces, particularly those in low-wage industries, do not have cafeterias or such nutrition-oriented programs, however. Thus—as in the case of school interventions—these interventions may exacerbate disparities. Though the evaluation literature lags behind the state of practice, those reviews that have been conducted have generally found that work-site health promotion activities that modify food environments are effective.105,145,147,148 Most papers and review articles do not disaggregate findings based on demographic categories of workers.
It is important to approach workplace interventions with the recognition that employees may resist and/or resent nutrition interventions that appear to attribute health problems to individual behavior, when similar attention is not also paid to improving the environment by providing healthier food choices or reducing workplace hazards.149 In addition, some employer incentives for healthy behavior or weight loss, such as added costs in insurance premiums or social pressures, can be counterproductive and discriminatory; given demographic trends in obesity, these may fall disproportionately on minority and low-income workers.
Community-level policy approaches
Though multiple program efforts focus on changing the physical environment in which food is offered, in the absence of fundamental food system change, those efforts at best have limited potential and, at worst, might be conducted in vain. One effective strategy for addressing food systems more comprehensively has been establishing state-, county-, or city-level food policy councils—groups of governmental and nongovernment food system stakeholders that would otherwise have little interaction, joining to shape local policy and programs related to food, agriculture, and/or hunger.89,150,151 Most of the approximately 50 food policy councils in the United States include addressing food system disparities in their missions.151
Communities addressing food system health disparities—whether through councils or otherwise—are developing a variety of innovative approaches including changes to legal codes and policies for zoning, development, taxation, food assistance, and public health. Some of these local decisions have been challenged by food industry and industrial agriculture interest groups, with varying results. These challenges highlight the benefit of stakeholder engagement and inclusive processes of policy development in many cases, as well as the benefits of additional legal and policy research to assure that proactive policies may employ the strongest possible legal grounding. As well, evaluation is needed to glean lessons from these policies and eventually enable scaling up of the most promising initiatives.
Other Social Factors
The social and cultural factors discussed in the following section are not primary targets of action for the majority of those focused on improving food systems, because they are commonly seen as involving individual-level behavior and responsibility. We include them here because the insight that derives from a food systems framework is one of interrelationship and multifaceted spheres of influence. Working on supply without addressing demand can have limited impact. If social factors combine so that individuals in specific communities buy and consume low amounts of healthy food, disparities in food access may be worsened. These community-level disparities are also aggregated upward to affect the overall shape of the food system and societal food supply, price, availability, and so on.
Tradition and culture
The determinants of demand for food vary by cultural group. Space constraints do not allow us to delineate relevant cultural factors group by group in this article. It is, however, critical to consider 4 cross-cutting issues.
First, culture and personal history affect food consumption via the pathway of preferences. Beyond the obvious direct connections to particular food preferences, these exposures also affect openness to try new foods, food preparation knowledge, and comfort levels regarding new or different cooking methods and ingredients. Further, as cultures interact with poverty, higher-fat foods and meats are often particularly valued because they are filling, and extra weight may be seen by some as offering security.152,153 Several studies found meats (which are associated with obesity154) including red meat (associated with negative health outcomes including cardiovascular disease, some cancers, and diabetes155) to be top preferred foods among different groups of low-income women, both for cultural and personal history reasons. Low budgets may push meat purchases toward higher-fat, more processed, and less-expensive cuts.73,156
Second, food is often seen as a means of connecting to or holding onto cultural identity and distinguishing oneself from the mainstream.157–159 Foods promoted as “healthy” are sometimes viewed as foreign to a given culture or can be perceived as culturally inappropriate.157 Several qualitative studies describe food, including “comfort” foods (ie, foods that are high in fat, sweetness, and/or filling), as a way to nurture and provide something positive and culturally significant to children and others in the face of poverty and stress.92,158
Third, acculturation within the overall and/or perceived norms of US society has been found to predict numerous unhealthy behaviors across multiple immigrant and ethnic groups. In terms of diet, intake among those with greater acculturation tends to become more processed, with increased fats and sugars.160,161
Finally, though culture can support unhealthy diets, we emphasize that cultures are not static. In some cultures, and across populations, there have been apparent cultural shifts in preferences based on knowledge of health impacts of certain preferred foods—such as the shift away from full-fat milk.36,162
It would be beneficial to expand the largely qualitative literature on connections between cultural identity and food choice and to complement it with more quantitative investigations.
Time
The phrase time is money may be a cliché. However, the fungibility of the two is important when it comes to people's relationships with food and may significantly explain why some people on low budgets choose to buy more expensive pre-prepared foods versus cooking from scratch. Single parents in particular tend to have more “poverty” when time is factored into the equation.163 To increase healthy food feasibility for low-income families, there is need for further innovation to identify ways the food system can reduce the time cost of healthy foods while keeping prices low, including through prepackaged items, funds to families to purchase cooking equipment, and recipe sharing.
Perceptions of “good food”
Several investigations have examined how low-income individuals and minorities perceive “good food”—food that is healthy, green, fair, and affordable—particularly organic and sustainably produced foods. According to Zepeda et al, research findings have been mixed regarding predictors of organic food consumption by age, gender, income, and education.164 Recent qualitative investigations have attempted to dig deeper.
one qualitative study found that lower-income participants valued many of the same attributes advocated by proponents of sustainable food systems, including an emphasis on local control, participatory process, ethics and equitability, and health.165 In another involving focus groups with African American and white participants, the former tended to be more positive toward and more willing to pay more for organic produce; further, they were more aware of broad food system and social factors, more frequently had dietary restrictions, and were more likely to read food labels for that reason.164 Though finding this potential openness to sustainable produce, both studies also identified financial, geographic, and knowledge barriers. Despite these barriers, a 2004 national study using Nielsen Homescan data found that African Americans spent the most per capita of any ethnic group on organic produce and, further, that families earning less than $25,000 per year spent more per capita than any other income group.52
Food production and processing exposures
Finally, outside the eating pathway in the food system, exposures associated with agriculture and food processing methods can directly affect health, contributing to health disparities.
Workers engaged in food production, processing, distribution, warehousing, and other aspects of the US food system report exceptionally high rates of occupational injuries, illnesses, and fatalities.29,166 Hazards include musculoskeletal strains and other injuries and exposures to chemicals, dust, endotoxins, and pathogens including antibiotic-resistant microbes.29,167 The US food system relies heavily on workers who are low-income, minority, and immigrant; due to social power differentials and other factors, these workers often experience difficulty exercising their rights to workplace safety and health and obtaining compensation when adverse events occur.24–29,168 It is a cruel irony that due to the low wages in food production, processing, distribution, and sales jobs, many of these workers providing our food are unable to afford and/or access healthy foods for themselves and their families.
Many rural communities are directly involved in and/or proximal to agriculture and food production and processing operations; studies have documented environmental injustice in the siting of industrial food animal production (IFAP) facilities, including disproportionate frequency in areas with high proportions of low-income and African American residents.30,31,169,170 There is a growing body of research on the public health impacts of living near IFAP facilities. In particular, there is evidence suggesting associations with respiratory conditions and mental health concerns.30
CONCLUSIONS
This review has shown how food systems and their components are key loci of and contributors to magnifying existing health disparities. The products and externalized costs of our food production system are inequitably distributed throughout society, as a result of supply, demand, and other social and economic factors. The determinants of disparities are like a prism, refracting the elements of our food system and making them differentially available, accessible, and even preferred by various sectors of society.
The UN has defined food security as a situation whereby “all people, at all times, have physical, social and economic access to sufficient, safe and nutritious food that meets their dietary needs and food preferences for an active and healthy life.”171 This article has emphasized the gaps in such access, identified key determinants of such gaps within US food systems, and described a set of interventions that can address them. We have reviewed the strong, complex, dynamic, and multifaceted relationships between food systems and health disparities and described existing policy and programmatic interventions that reflect an understanding of how food systems can address and reduce health disparities. We have reviewed literature and discussed research and policy needs relevant to the broad food system, community food systems, other social factors, and food production/processing exposures.
Finally, we have shared an original conceptual model explaining these relationships. The model also emphasizes the social factors that, though separate from the food system, interface with the food system in affecting health disparities. The model provides a structure that can be useful in conceiving interventions, by providing a set of variables and sites of interventions to consider. At least as importantly, though any single intervention may primarily focus on a single one of the model's levels, the model highlights the need to approach interventions with an understanding of the systemic nature of food systems and of the interactions between components at multiple levels. For example, in order to address Baltimore City's nutritional disparities, the city's farm-to-school program primarily aims to serve healthier food to children. But to do so, the program extends to address a broad range of needs including local food production and distribution networks, institutional contracts, food preparation infrastructure, food education, and demand-building strategies.
From this review, the following points emerge.
To address public health disparities, a key goal is to shift away from the current mainstream food supply, to food encouraged as part of the Dietary Guidelines for Americans5 as well as more environmentally sustainable foods. These foods should become those most available and affordable through basic food outlets. Key tactics in this shift may include realignment of farm policy incentives that promote overproducing selected commodity crops and altering food processor incentives. Increased incentives should support fruit and vegetable production, until the label “specialty crops” becomes the anachronism it should be.
A second key goal is to alter food environments to support access to and affordability of healthier foods. An extensive research and review literature examines relationships between food environments and health and evaluates interventions to address the impacts.
Some groups may lag in adopting innovations (such as new approaches to diet or new venues for obtaining food) due to inequalities in financial resources, geographic access, time, education, and other factors. Population strategies must be balanced with efforts specifically aimed at removing barriers that create and/or perpetuate disparities.
The converging environmental crises we face will have powerful effects on food security; those with the least economic, social, and political power may bear the brunt of the harms. Greater recognition of this phenomenon and more purposeful planning including development of resilient, localized agricultural production may help mitigate the situation.
There is great need for study of the nutritional public health impacts of sustainably produced food and for evaluation of practice work in alternative food systems, including the disparities impacts.
Community engagement and participatory approaches are essential in the search for and development of effective solutions that will not be experienced as punitive, stigmatizing, unrealistic, or missing key components— and also to make sure the right questions are asked.
There is much need for programs to develop careers of researchers and local, state, and federal leaders who appreciate health in all policies from within the populations experiencing health disparities.
Food systems advocates and public health advocates seeking to address health disparities must join forces with those working to address underlying social inequities, including poverty and racism, that interact with food system factors to influence disease risk.
We cannot effectively address food-related health disparities or the ecologic harms of the food system without also working to make access to healthy and more sustainably produced food a right, not a privilege. All these relationships are inextricably linked, and critical synergies of impact can be accessed by jointly pursuing public health, equity, and “good food” goals. Improved political alliances between anti-hunger advocates and those supporting healthy food and sustainable food can also change the political calculus of agricultural policy. The United States has set a national goal to eliminate health disparities.12 Effective progress will depend partly on a broader recognition of the breadth of food system factors that contribute to these disparities—community-level factors, other social factors, and agricultural exposures. In all these areas, this review documents a need for more evidence and evaluation, more innovation, more scaling up and policy change, and more action.
Acknowledgments
This article was produced with funds from the Healthy Eating Research program and from the Center for a Livable Future, Johns Hopkins Bloomberg School of Public Health. It was originally developed as a background paper for the Food Systems and Public Health: Linkages to Achieve Healthier Diets and Healthier Communities workshop. The authors gratefully acknowledge the conference organizers for the opportunity to develop this article, reviewers for their helpful edits, and Brent Kim and other colleagues at the Center for a Livable Future for their research assistance.
REFERENCES
- 1.US Dept of Health and Human Services. Healthy People 2010. 2nd ed. Washington, DC: US Government Printing Office; 2000. [Google Scholar]
- 2.Sobal J, Khan LK, Bisogni C. A conceptual model of the food and nutrition system. Soc Sci Med. 1998;47:853–863. doi: 10.1016/s0277-9536(98)00104-x. [DOI] [PubMed] [Google Scholar]
- 3.von Bertalanffy L. An outline of general system theory. Br J Philos Sci. 1950;1:134–165. [Google Scholar]
- 4.Leischow SJ, Milstein B. Systems thinking and modeling for public health practice. Am J Public Health. 2006;96:403–405. doi: 10.2105/AJPH.2005.082842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Dept of Health and Human Services, US Dept of Agriculture. Dietary Guidelines for Americans, 2005. 6th ed. Washington, DC: US Government Printing Office; 2005. [Google Scholar]
- 6.Kellogg Foundation WK. Overview: good food. Available at: http://www.wkkf.org/default.aspx?tabid=75&CID=19&NID=61&LanguageID=0. Accessed March 11, 2009.
- 7.Beydoun MA, Gary TL, Caballero BH, Lawrence RS, Cheskin LJ, Wang Y. Ethnic differences in dairy and related nutrient consumption among US adults and their association with obesity, central obesity, and the metabolic syndrome. Am J Clin Nutr. 2008;87:1914–1925. doi: 10.1093/ajcn/87.6.1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dubowitz T, Heron M, Bird CE, et al. Neighborhood socioeconomic status and fruit and vegetable intake among whites, blacks, and Mexican Americans in the United States. Am J Clin Nutr. 2008;87:1883–1891. doi: 10.1093/ajcn/87.6.1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kant AK, Graubard BI, Kumanyika SK. Trends in black-white differentials in dietary intakes of US adults, 1971–2002. Am J Prev Med. 2007;32:264–272. doi: 10.1016/j.amepre.2006.12.011. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blisard N, Stewart H, Jolliffe D. Low Income Households’ Expenditures on Fruits and Vegetables. Washington, DC: Economic Research Service, US Dept of Agriculture; 2004. [Google Scholar]
- 11.Bleich SN, Wang YC, Wang Y, Gortmaker SL. Increasing consumption of sugar-sweetened beverages among US adults: 1988–1994 to 1999–2004. Am J Clin Nutr. 2009;89:372–381. doi: 10.3945/ajcn.2008.26883. [DOI] [PubMed] [Google Scholar]
- 12.Department of Health & Human Services. Healthy People 2010 Midcourse Review. 2009.
- 13.Miech RA, Kim J, McConnell C, Hamman RF. A growing disparity in diabetes-related mortality: US trends, 1989–2005. Am J Prev Med. 2009;36:126–132. doi: 10.1016/j.amepre.2008.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiologic Reviews Advance Access. 2007. [DOI] [PubMed]
- 15.Pan L, Galuska DA, Sherry B, et al. Differences in prevalence of obesity among Black, White, and Hispanic adults—United States, 2006–2008. MMWR. 2009;58:740–744. [PubMed] [Google Scholar]
- 16.National Center for Health Statistics. Health, United States, 2008. 2009. [PubMed]
- 17.Nord M, Andrews M, Carlson S. Household Food Security in the United States, 2007. 2008. Economic Research Report No. (ERR-66).
- 18.Dinour LM, Bergen D, Yeh MC. The food insecurity-obesity paradox: a review of the literature and the role food stamps may play. J Am Diet Assoc. 2007;107:2071–2076. doi: 10.1016/j.jada.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 19.Huang TT, Glass TA. Transforming research strategies for understanding and preventing obesity. JAMA. 2008;300:1811–1813. doi: 10.1001/jama.300.15.1811. [DOI] [PubMed] [Google Scholar]
- 20.Lawrence RG. Framing obesity: the evolution of news discourse on a public health issue. Harvard Int J Press/Polit. 2004;9:56–75. [Google Scholar]
- 21.Adler NE, Stewart J. Reducing obesity: motivating action while not blaming the victim. Milbank Mem Fund Q Health Soc. 2009;87:49–70. doi: 10.1111/j.1468-0009.2009.00547.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Progressive Grocer. ACNielsen Study: parents blame selves for kids’ obesity. Available at: http://www.allbusiness.com/retail-trade/food-stores/4255602-1.html.
- 23.Pomeranz JL. A historical analysis of public health, the law and stigmatized social groups: the need for both obesity and weight bias legislation. Obesity. 2008;16(2):S93–S103. doi: 10.1038/oby.2008.452. [DOI] [PubMed] [Google Scholar]
- 24.Gouveia L, Juska A. Taming nature, taming workers: constructing the separation between meat consumption and meat production in the U.S. Sociol Ruralis. 2002;42(4) [Google Scholar]
- 25.Lipscomb HJ, Argue R, McDonald MA, et al. Exploration of work and health disparities among black women employed in poultry processing in the rural south. Environ Health Perspect. 2005;113:1833–1840. doi: 10.1289/ehp.7912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cooper M. The heartland's raw deal: how meatpacking is creating a new immigrant underclass. In: Arrighi BA, editor. Understanding Inequality: The Intersection of Race/Ethnicity, Class, and Gender. 2nd ed. Rowman and Littlefield; 2007. pp. 137–142. [Google Scholar]
- 27.McCauley LA, Lasarev MR, Higgins G, et al. Work characteristics and pesticide exposures among migrant agricultural families: a community-based research approach. Environ Health Perspect. 2001;109:533–538. doi: 10.1289/ehp.01109533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lipscomb HJ, Loomis D, McDonald MA, Argue RA, Wing S. A conceptual model of work and health disparities in the United States. Int J Health Serv. 2006;36:25–50. doi: 10.2190/BRED-NRJ7-3LV7-2QCG. [DOI] [PubMed] [Google Scholar]
- 29.Frank AL, McKnight R, Kirkhorn SR, Gunderson P. Issues of agricultural safety and health. Annu Rev Public Health. 2004;25:225–245. doi: 10.1146/annurev.publhealth.25.101802.123007. [DOI] [PubMed] [Google Scholar]
- 30.Donham KJ, Wing S, Osterberg D, et al. Community health and socioeconomic issues surrounding concentrated animal feeding operations. Environ Health Perspect. 2007;115:317–320. doi: 10.1289/ehp.8836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mirabelli MC, Wing S, Marshall SW, Wilcosky TC. Race, poverty, and potential exposure of middle-school students to air emissions from confined swine feeding operations. Environ Health Perspect. 2006;114:591–596. doi: 10.1289/ehp.8586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Food and Agriculture Organization, United Nations. Voluntary Guidelines to Support the Progressive Realization of the Right to Adequate Food in the Context of National Food Security. 2004.
- 33.Gittelsohn J, Franceschini MCT, Rasooly IR, et al. Understanding the food environment in a low-income urban setting: implications for food store interventions. J Hunger Environ Nutr. 2008;2(2):33. [Google Scholar]
- 34.Real Food Challenge. All participating schools. Available at: http://db.realfoodchallenge.org/. Accessed August 18, 2009.
- 35.Farmer P. Pathologies of power: structural violence and the materiality of the social. The 8th Annual Sidney W. Mintz Lecture in Anthropology, Johns Hopkins University. November 2001.
- 36.Variyam JN, Golan E. New health information is reshaping food choices. Food Rev. 2002;25:13–18. [Google Scholar]
- 37.Wells HF, Buzby JC. Dietary Assessment of Major Trends in US Food Consumption, 1970–2005. 2008. Economic Information Bulletin-33.
- 38.Wallinga D, Schoonover H, Muller M. Considering the contributions of US agricultural policy to the obesity epidemic: overview and opportunities. J Hunger Environ Nutr. 2009;4:3–19. [Google Scholar]
- 39.Putnam J, Allshouse J, Kantor LS. US per capita food supply trends: more calories, refined carbohydrates, and fats. Food Rev. 2002;25:2–15. [Google Scholar]
- 40.Buzby J, Wells HF, Vocke G. Possible Implications for US Agriculture From Adoption of Select Dietary Guidelines. 2006. USDA Economic Research Report No. ERR-31.
- 41.Hendrickson M, Wilkinson J, Heffernan WD, Gronski R. The Global Food System and Nodes of Power. 2008.
- 42.Hendrickson M, Heffernan WD. Concentration of Agricultural Markets. Columbia, Mo: Dept of Rural Sociology, University of Missouri; 2007. [Google Scholar]
- 43.Miller JC, Cobles KH. Cheap food policy: fact or rhetoric. Food Policy. 2007;32:98–111. [Google Scholar]
- 44.Beghin JC, Jensen HH. Farm policies and added sugars in US diets. Food Policy. 2008;33:480–488. [Google Scholar]
- 45.Alston JM, Sumner DA, Vosti SA. Are agricultural policies making us fat? Likely links between agricultural policies and human nutrition and obesity, and their policy implications. Rev Agric Econ. 2006;28:313–322. [Google Scholar]
- 46.Hunt DB, Schaffer HD, Ray DE. US Agricultural commodity policy and its relationship to obesity—draft. Wingspread conference. 2007.
- 47.Harvie A, Wise TA. Sweetening the Pot: Implicit Subsidies to Corn Sweeteners and the US Obesity Epidemic. GDAE Policy Brief No. 09-01. Available at: http://www.ase.tufts.edu/gdae/Pubs/rp/PB09-01SweeteningPotFeb09.pdf.
- 48.Benbrook C, Zhao X, Yanez J, Davies N, Andrew P. New evidence confirms the nutritional superiority of plant-based organic foods: state of science review. Available at: http://www.organic-center.org/reportfiles/5367_Nutrient_Content_SSR_FINAL_V2.pdf.
- 49.Dangour AD, Dodhia SK, Hayter A, Allen E, Lock K, Uauy R. Nutritional quality of organic foods: a systematic review. Am J Clin Nutr. 2009. [DOI] [PubMed]
- 50.Clancy K. Greener Pastures: How Grass-Fed Beef and Milk Contribute to Healthy Eating. Union of Concerned Scientists; 2006. [Google Scholar]
- 51.Hamm MW. Linking sustainable agriculture and public health: opportunities for realizing multiple goals. J Hunger Environ Nutr. 2008;3:169–185. [Google Scholar]
- 52.Stevens-Garmon J, Huang CL, Lin B. Organic demand: a profile of consumers in the fresh produce market. Choices: The Magazine of Food, Farm and Resource Issues. 2007;22:110–116. [Google Scholar]
- 53.Banse M, Nowicki P, van Hans M. Why are current food prices so high? 2008. pp. 2008–2040.
- 54.Organisation for Economic Co-operation and Development, Food and Agriculture Organization of the United Nations. OECD-FAO Agricultural Outlook: 2008–2017. 2008.
- 55.Trostle R. Global Agricultural Supply and Demand: Factors Contributing to the Recent Increase in Food Commodity Prices. 2008. p. WRS-0801.
- 56.Institute for Agriculture and Trade Policy. Commodities Market Speculation: The Risk to Food Security and Agriculture. 2008.
- 57.United States Senate Permanent Subcommittee on Investigations. Excessive Speculation in the Wheat Market. 2009.
- 58.Blair D, Giesecke CC, Sherman S. A dietary, social and economic evaluation of the Philadelphia urban gardening project. J Nutr Educ. 1991;23(4):161–167. [Google Scholar]
- 59.Alaimo K, Packnett E, Miles RA, Kruger DJ. Fruit and vegetable intake among urban community gardeners. J Nutr Educ Behav. 2008;40(2):94–101. doi: 10.1016/j.jneb.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 60.Horovitz B. Recession grows interest in seeds, vegetable gardening. USA Today. 2009.
- 61.Drewnowski A, Specter S. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79(1):6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- 62.Glanz K, Basil M, Maibach E, Goldberg J, Snyder D. Why Americans eat what they do: taste, nutrition, cost, convenience, and weight control concerns as influences on food consumption. J Am Dent Assoc. 1998;98:1118–1126. doi: 10.1016/S0002-8223(98)00260-0. [DOI] [PubMed] [Google Scholar]
- 63.Leibtag ES, Kaufman PR. Exploring Food Purchase Behavior of Low Income Households. Agriculture Information Bulletin No. 747-07. Available at: http://www.ers.usda.gov/Publications/AIB747/aib74707.pdf.
- 64.Kaufman PR, Macdonald JM, Lutz SM, Smallwood DW. Do the Poor Pay More for Food? Item Selection and Price Differences Affect Low-income Household Food Costs. 1997. Economic Report No. 759.
- 65.Chung C, Myers S. Do the poor pay more for food?: An analysis of grocery store availability and food price disparities. J Consum Aff. 1999;33:276–296. [Google Scholar]
- 66.Andreyeva T, Blumenthal DM, Schwartz MB, Long MW, Brownell KD. Availability and prices of foods across stores and neighborhoods: the case of New Haven, Connecticut. Health Aff. 2008;27:1381–1388. doi: 10.1377/hlthaff.27.5.1381. [DOI] [PubMed] [Google Scholar]
- 67.Fellowes M. From Poverty, Opportunity: Putting the Market to Work for Lower Income Families. The Brookings Institution; 2006. [Google Scholar]
- 68.Putnam J, Allshouse J, Scott Kantor L. US per capita food supply trends: more calories, refined carbohydrates, and fats. Food Rev. 2002;25(3) [Google Scholar]
- 69.Monsivais P, Drewnowski A. The rising cost of low-energy-density foods. J Am Diet Assoc. 2007;107:2071–2076. doi: 10.1016/j.jada.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 70.Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr. 2005;82:265S–273S. doi: 10.1093/ajcn/82.1.265S. [DOI] [PubMed] [Google Scholar]
- 71.Drewnowski A, Darmon N. Food choices and diet costs: an economic analysis. J Nutr. 2005;135:900–904. doi: 10.1093/jn/135.4.900. [DOI] [PubMed] [Google Scholar]
- 72.Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;87:1107–1117. doi: 10.1093/ajcn/87.5.1107. [DOI] [PubMed] [Google Scholar]
- 73.Wiig K, Smith C. The art of grocery shopping on a food stamp budget: factors influencing the food choices of low-income women as they try to make ends meet. Public Health Nutr. 2008. [DOI] [PubMed]
- 74.Reed J, Frazão E, Itskowitz R. How much do Americans pay for fruits and vegetables? 2004. p. 790. Available at: http://www.ers.usda.gov/publications/aib790/aib790fm.pdf.
- 75.American Medical Association, Council on Science and Public Health. Report of the Council on Science and Public Health: Sustainable Food. 2009. Resolution 405, A-08.
- 76.Powell LM, Chaloupka FJ. Food prices and obesity: evidence and policy implications for taxes and subsidies. Milbank Q. 2009;87:229–257. doi: 10.1111/j.1468-0009.2009.00554.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dong D, Lin BH. Fruit and Vegetable Consumption by Low-income Americans: Would a Price Reduction Make a Difference? 2009. Economic Research Report No. (ERR-70).
- 78.Brownell KD, Frieden TR. Ounces of prevention—the public policy case for taxes on sugared beverages. N Engl J Med. 2009;360:1805–1808. doi: 10.1056/NEJMp0902392. [DOI] [PubMed] [Google Scholar]
- 79.US Dept of Agriculture Food and Nutrition Service. Reaching Those in Need: State Food Stamp Participation Rates in 2006. Available at: http://www.fns.usda.gov/ora/MENU/Published/SNAP/FILES/Participation/Reaching2006.pdf.
- 80.US Dept of Agriculture, Office of Analysis, Nutrition, and Evaluation. WIC Program Coverage: How Many Eligible Individuals Participated in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC): 1994 to 2003? Available at: http://www.fns.usda.gov/ora/MENU/Published/WIC/FILES/WICEligibles.pdf.
- 81.Bartlett S, Burstein N. Food Stamp Program Access Study: Eligible Nonparticipants. 2004. E-FAN-03-013-2.
- 82.Basiotis PP, Kramer-LeBlanc CS, Kennedy ET. Maintaining nutrition security and diet quality: the role of the Food Stamp Program and WIC. Fam Econ Nutr Rev. 1998;11:2–16. [Google Scholar]
- 83.Fox MK, Hamilton W, Lin B. Effects of food assistance and nutrition programs on nutrition and health. 2004. p. 3. Available at: http://www.ers.usda.gov/publications/fanrr19-3/fanrr19-3.pdf. [DOI] [PubMed]
- 84.Ralston K. Nutrient adequacy of children participating in WIC. Available at: http://www.ers.usda.gov/publications/EB8/EB8.pdf.
- 85.Rosenbaum D. Food Stamp benefits falling further behind rising food prices. Available at: http://www.cbpp.org/7-22-08fa.pdf. Accessed March 6, 2009.
- 86.Golden C. Reaching the heights. Edible San Diego. 2008.
- 87.Food Research and Action Center. Commodity foods and nutritional quality of the national school lunch program: historical role, current operations, and future potential. Available at: http://frac.org/pdf/commodities08.pdf.
- 88.Glauber J. US food policy and recent food price increase. Paper presented at: Johns Hopkins Bloomberg School of Public Health; March 13, 2009.
- 89.Winne M. Fresh from the city. Yes! Magazine. 2009.
- 90.Poppendieck J. Sweet Charity?: Emergency Food and the End of Entitlement. New York, NY: Penguin Books; 1999. [Google Scholar]
- 91.Berg J. All You Can Eat: How Hungry Is America? New York, NY: Seven Stories Press; 2008. [Google Scholar]
- 92.Kaufman L, Karpati A. Understanding the sociocultural roots of childhood obesity: food practices among Latino families of Bushwick, Brooklyn. Soc Sci Med. 2007;64:2177–2188. doi: 10.1016/j.socscimed.2007.02.019. [DOI] [PubMed] [Google Scholar]
- 93.Chilton M, Booth S. Hunger of the body and hunger of the mind: African American women's perceptions of food insecurity, health and violence. J Nutr Educ Behav. 2007;39(3):116–125. doi: 10.1016/j.jneb.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 94.Kempson KM, Palmer Keenan D, Sadani PS, Ridlen S, Scotto Rosato N. Food management practices used by people with limited resources to maintain food sufficiency as reported by nutrition educators. J Am Diet Assoc. 2002;102:1795–1799. doi: 10.1016/s0002-8223(02)90385-8. [DOI] [PubMed] [Google Scholar]
- 95.Advertising Age. Special Report Supplement: 50th Annual 100 Leading National Advertisers. Available at: http://adage.com/images/random/lna2005.pdf.
- 96.Advertising Age. 100 Leading national advertisers 2009. Advertising Age. 2009.
- 97.Harris J, Pomeranz J, Lobstein T, Brownell KD. A crisis in the marketplace: how food marketing contributes to childhood obesity and what can be done. Annu Rev Public Health.; p. 30. [DOI] [PubMed]
- 98.Glanz K, Resnicow K, Seymour J, et al. How major restaurant chains plan their menus: the role of profit, demand, and health. Am J Prev Med. 2007;32:383–388. doi: 10.1016/j.amepre.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 99.Yancey AK, Cole BL, Brown R, et al. A cross-sectional prevalence study of ethnically targeted and general audience outdoor obesity-related advertising. Milbank Q. 2009;87:155–184. doi: 10.1111/j.1468-0009.2009.00551.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tirodkar MA, Jain A. Food messages on African American television shows. Am J Public Health. 2003;93:439–441. doi: 10.2105/ajph.93.3.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Henderson VR, Kelly B. Food advertising in the age of obesity: content analysis of food advertising on general market and African American television. J Nutr Educ Behav. 2005;37(4):191–196. doi: 10.1016/s1499-4046(06)60245-5. [DOI] [PubMed] [Google Scholar]
- 102.Kumanyika S, Grier S. Targeting interventions for ethnic minority and low-income populations. Future Child. 2006;16:187–207. doi: 10.1353/foc.2006.0005. [DOI] [PubMed] [Google Scholar]
- 103.FTC. Marketing Food to Children and Adolescents: A Review of Industry Expenditures, Activities, and Self-Regulation: A Report to Congress. 2008.
- 104.Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the US. Am J Prev Med. 2009;36:74–81. doi: 10.1016/j.amepre.2008.09.025. e10. [DOI] [PubMed] [Google Scholar]
- 105.Story M, Kaphingst KM, Robinson-O'Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- 106.US Dept of Agriculture, Economic Research Service. Access to Affordable and Nutritious Food: Measuring and Understanding Food Deserts and Their Consequences: Report to Congress. 2009.
- 107.Beaulac J, Kirstjansson E, Cummins S. Food deserts: a systematic review, 1966–2007. Prev Chronic Dis. [PMC free article] [PubMed]
- 108.Shaffer A. The Persistence of L.A.’ s Grocery Gap: The Need for a New Food Policy and Approach to Market Development. Center for Food and Justice, Urban and Environmental Policy Institute, Occidental College; 2002. [Google Scholar]
- 109.Weinberg Z. No place to shop: food access lacking in the inner city. Race, Poverty and the Environment. Winter 2000.
- 110.Tropp D, Ragland E, Barham J. The Dynamics of Change in the US Food Marketing Environment. US Dept of Agriculture Agricultural Marketing Service; 2008. [Google Scholar]
- 111.Kaufman PR. Rural poor have less access to supermarkets, large grocery stores. Rural Dev Perspec.; 13(3):19–26. [Google Scholar]
- 112.Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson ML. Neighborhood racial composition, neighborhood poverty, and the spatial accessibility of supermarkets in metropolitan Detroit. Am J Public Health. 2005;95:660–667. doi: 10.2105/AJPH.2004.042150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Antin TM, Hora MT. Distance & beyond: Variables influencing conceptions of food store accessibility in Baltimore, MD. Practicing Anthropol. 2005;27(2):15–17. [Google Scholar]
- 114.Sharkey J. Session 1—rural food deserts: perspective from rural Texas. Institute of Medicine Workshop on the Public Health Effects of Food Deserts; [Google Scholar]
- 115.Palmer A, Smith J, Haering SA, McKenzie S. Understanding and Addressing Food Security in Southwest Baltimore. Center for a Livable Future; 2007. [Google Scholar]
- 116.Franco M, Diez Roux AV, Glass TA, Caballero B, Brancati FL. Neighborhood characteristics and availability of healthy foods in Baltimore. Am J Prev Med. 2008;35:561–567. doi: 10.1016/j.amepre.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Franco M, Diez Roux AV, Nettleton JA, et al. Availability of healthy foods and dietary patterns: the multi-ethnic study of atherosclerosis. Am J Clin Nutr. 2009;89:1–7. doi: 10.3945/ajcn.2008.26434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Brunett D. Supermarket access in low-income communities. Available at: http://www.preventioninstitute.org/pdf/CHI_Supermarkets.pdf.
- 119.Wrigley N, Warm D, Margetts B, Whelan A. Assessing the impact of improved retail access on diet in a “food desert”: a preliminary report. Urban Stud. 2002;39:2061–2082. [Google Scholar]
- 120.The Food Trust. Pennsylvania Fresh Food Financing Initiative: providing healthy food choices to Pennsylvania's communities. Available at: http://www.thefoodtrust.org/pdf/FFFI%20Case%20Studies.pdf. Accessed March 16, 2009.
- 121.Glanz K, Yaroch AL. Strategies for increasing fruit and vegetable intake in grocery stores and communities: policy, pricing, and environmental change. Prev Med. 2004;39(suppl 2):75–80. doi: 10.1016/j.ypmed.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 122.Seymour JD, Lazarus Yaroch A, Serdula M, Blanck HM, Khan LK. Impact of nutrition environmental interventions on point-of-purchase behavior in adults: a review. Prev Med. 2004;39(suppl 2):108–136. doi: 10.1016/j.ypmed.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 123.Gittelsohn J, Suratkar S, Song H, et al. Process evaluation of Baltimore Healthy Stores: a pilot health intervention program with supermarkets and corner stores in Baltimore City. Health Promot Pract. 2009. [DOI] [PMC free article] [PubMed]
- 124.US Dept of Agriculture. Farmers market growth: 1994–2008. Available at: http://www.ams.usda.gov/AMSv1.0/ams.fetchTemplateData.do?template=TemplateS&navID=WholesaleandFarmersMarkets&leftNav=WholesaleandFarmersMarkets&page=WFMFarmersMarketGrowth&description=Farmers%20Market%20Growth&acct=frmrdirmkt. Accessed January 2009.
- 125.Flournoy R, Treuhaft S. Healthy food, healthy communities: improving access and opportunities through food retailing. Available at: http://www.policylink.org/pdfs/HealthyFoodHealthyCommunities.pdf.
- 126.Policy Link. Healthy food retailing: getting started. Available at: http://www.policylink.org/EDTK/HealthyFoodRetailing/GettingStarted.html.
- 127.Fisher A. Hot Peppers and Parking Lot Peaches: Evaluating Farmers’ Markets in Low Income Communities. Community Food Security Coalition; 1999. [Google Scholar]
- 128.US Dept of Agriculture. 2008 Farm Bill side by side: nutrition. Available at: http://www.ers.usda.gov/FarmBill/2008/Titles/TitleIVNutrition.htm. Accessed March 16, 2009.
- 129.Kropf M, Holben D, Holcomb J, Anderson H. Food security status and produce intake and behaviors of Special Supplemental Nutrition Program for Women, Infants, and Children and Farmers’ Market Nutrition Program participants. J Am Diet Assoc. 2007;107:1903–1908. doi: 10.1016/j.jada.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 130.Herman DR, Harrison GG, Afifi AA, Jenks E. Effect of a targeted subsidy on intake of fruits and vegetables among low-income women in the Special Supplemental Nutrition Program for Women, Infants, and Children. Am J Public Health. 2008;98:98–105. doi: 10.2105/AJPH.2005.079418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Herman D, Harrison G, Jenks E. Choices made by low-income women provided with an economic supplement for fresh fruit and vegetable purchase. J Am Diet Assoc. 2007;106:740–744. doi: 10.1016/j.jada.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 132.Johnson DB, Beaudoin S, Smith LT, Beresford SAA, LoGerfo JP. Increasing fruit and vegetable intake in homebound elders: the Seattle Senior Farmers’ Market Nutrition Pilot Program. Prev Chronic Dis. 2004;1:A03. [PMC free article] [PubMed] [Google Scholar]
- 133.USDA Food and Nutrition Service. 2008 EBT farmers’ market projects status report. Available at: http://www.fns.usda.gov/FSP/ebt/ebt_farmers_markstatus.htm. Accessed March 16, 2009.
- 134.Guthrie JF, Lin BH, Frazao E. Role of food prepared away from home in the American diet, 1977–78 versus 1994–1996: changes and consequences. J Nutr Educ Behav. 2002;34:140–150. doi: 10.1016/s1499-4046(06)60083-3. [DOI] [PubMed] [Google Scholar]
- 135.Powell LM, Chaloupka FJ, Bao Y. The availability of fast-food and full-service restaurants in the United States: associations with neighborhood characteristics. Am J Prev Med. 2007;33(4, suppl 1):S240–S245. doi: 10.1016/j.amepre.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 136.Pereira MA, Kartashov AI, Ebbeling CB, et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005;365(9453):36–42. doi: 10.1016/S0140-6736(04)17663-0. [DOI] [PubMed] [Google Scholar]
- 137.French SA, Harnack L, Jeffery RW. Fast food restaurant use among women in the Pound of Prevention Study: dietary, behavioral and demographic correlates. Int J Obes. 2000;24:1353–1359. doi: 10.1038/sj.ijo.0801429. [DOI] [PubMed] [Google Scholar]
- 138.Story M, Nanney MS, Schwartz MB. Schools and obesity prevention: creating school environments and policies to promote healthy eating and physical activity. Milbank Q. 2009;87:71–100. doi: 10.1111/j.1468-0009.2009.00548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Greves HM, Rivara FP. Report card on school snack food policies among the United States’ largest school districts in 2004–2005: room for improvement. Int J Behav Nutr Phys Act. 2006;3(1) doi: 10.1186/1479-5868-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Institute of Medicine, Committee on Progress in Preventing Childhood Obesity. Framework for evaluating progress. In: Koplan JP, Liverman CT, Kraak VI, Wisham SL, editors. Progress in Preventing Childhood Obesity: How Do We Measure Up? Washington, DC: National Academies Press; 2007. [Google Scholar]
- 141.Joshi A, Azuma AM, Feenstra G. Do farm-to-school programs make a difference? Findings and future research needs. J Hunger Environ Nutr. 2008. p. 3.
- 142.Robinson-O'Brien R, Story M, Heim S. Impact of garden-based youth nutrition intervention programs: a review. J Am Diet Assoc. 2009;109:273–280. doi: 10.1016/j.jada.2008.10.051. [DOI] [PubMed] [Google Scholar]
- 143.Allen P, Guntham J. From “old school” to “farm-to-school”: neoliberalization from the ground up. Agric Human Values. 2006;23:401–415. [Google Scholar]
- 144.Zenk SN, Powell LM. US secondary schools and food outlets. Health Place. 2008;14:336–346. doi: 10.1016/j.healthplace.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 145.Heinen L, Darling H. Addressing obesity in the workplace: the role of employers. Milbank Q. 2009;87:101–122. doi: 10.1111/j.1468-0009.2009.00549.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Sorensen G, Stoddard AM, Dubowitz T, et al. The influence of social context on changes in fruit and vegetable consumption: results of the healthy directions studies. Am J Public Health. 2007;97:1216–1227. doi: 10.2105/AJPH.2006.088120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Pomerleau J, Lock K, Knai C, McKee M. Interventions designed to increase adult fruit and vegetable intake can be effective: a systematic review of the literature. J Nutr. 2005;135:2486–2495. doi: 10.1093/jn/135.10.2486. [DOI] [PubMed] [Google Scholar]
- 148.Engbers LH, van Poppel MNM, Chin A, Paw M, van Mechelen W. Worksite health promotion programs with environmental changes: a systematic review. Am J Prev Med. 2005;29:61–70. doi: 10.1016/j.amepre.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 149.Sorensen G, Stoddard A, Ockene JK, Hunt MK, Youngstrom R. Worker participation in an integrated health promotion/health protection program: results from the WellWorks project. Health Educ Q. 1996;23(2):191–203. doi: 10.1177/109019819602300205. [DOI] [PubMed] [Google Scholar]
- 150.Clancy K, Hammer J, Lippoldt D. Remaking the North American Food System: Strategies for Sustainability. University of Nebraska Press; 2008. Food policy councils: past, present, and future. [Google Scholar]
- 151.Community Food Security Coalition. North American Food Policy Council Web site. Available at: http://www.foodsecurity.org/FPC/index.html. Accessed August 13, 2009.
- 152.Sanchez-Johnson LAP, Fitzgibbon ML, Martinovich Z, Stolley MR, Dyer AR, Van Horn L. Ethnic differences in correlates of obesity between Latin-American and black women. Obes Res. 2004;12:652–660. doi: 10.1038/oby.2004.75. [DOI] [PubMed] [Google Scholar]
- 153.Kumanyika S. Environmental influences on childhood obesity: ethnic and cultural influences in context. Physiol Behav. 2008;94(1, special issue):61–70. doi: 10.1016/j.physbeh.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 154.Wang Y, Beydoun MA. Meat consumption is associated with obesity and central obesity among US adults. Int J Obes. 2009;33:621–628. doi: 10.1038/ijo.2009.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Walker P, Rhubart-Berg P, McKenzie S, Kelling K, Lawrence RS. Public health implications of meat production and consumption. Public Health Nutr. 2005;8:348–356. doi: 10.1079/phn2005727. [DOI] [PubMed] [Google Scholar]
- 156.Hargreaves MK, Schlundt DG, Buchowski MS. Contextual factors influencing the eating behaviors of African American women: a focus group investigation. Ethn Health. 2002;7:133–147. doi: 10.1080/1355785022000041980. [DOI] [PubMed] [Google Scholar]
- 157.James DCS. Factors influencing food choices, dietary intake, and nutrition-related attitudes among African Americans: application of a culturally sensitive model. Ethn Health. 2004;9:349–367. doi: 10.1080/1355785042000285375. [DOI] [PubMed] [Google Scholar]
- 158.Liburd L. Food, identity, and African-American women with type II diabetes: an anthropological perspective. Diab Spectr. 2003;16:160–165. [Google Scholar]
- 159.Horowitz CR, Tuzzio L, Rojas M, Monteith S, Sisk JE. How do urban African Americans and Latinos view the influence of diet on hypertension? J Health Care Poor Underserv. 2004;15:631–644. doi: 10.1353/hpu.2004.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Gordon-Larsen P, Harris KM, Ward DS, Popkin BM. Acculturation and overweight-related behaviors among Hispanic immigrants to the US: the National Longitudinal Study of Adolescent Health. Soc Sci Med. 2003;57:2023–2034. doi: 10.1016/s0277-9536(03)00072-8. [DOI] [PubMed] [Google Scholar]
- 161.Unger JB, Reynolds K, Shakib S, Spruijt-Metz D, Sun P, Johnson CA. Acculturation, physical activity, and fast-food consumption among Asian American and Hispanic adolescents. JECH. 2004;29:467–481. doi: 10.1007/s10900-004-3395-3. [DOI] [PubMed] [Google Scholar]
- 162.Prynne CJ, Paul AA, Mishra GD, Greenberg DC, Wadsworth MEJ. Changes in intake of key nutrients over 17 years during adult life of a British birth cohort. Br J Nutr. 2005;94:368–376. doi: 10.1079/bjn20041404. [DOI] [PubMed] [Google Scholar]
- 163.Rose D. Food stamps, the thrifty food plan, and meal preparation: the importance of the time dimension for US nutrition policy. J Nutr Educ Behav. 2007;39:226–232. doi: 10.1016/j.jneb.2007.04.180. [DOI] [PubMed] [Google Scholar]
- 164.Zepeda L, Chang HS, Leviten-Reid C. Organic food demand: a focus group study involving Caucasian and African-American shoppers. Agric Human Values. 2006;23:385–394. [Google Scholar]
- 165.Webber CB, Dollahite JS. Attitudes and behaviors of low income food heads of households toward sustainable food system concepts. J Hunger Environ Nutr. 2008;3:186–205. [Google Scholar]
- 166.Bureau of Labor Statistics. Table 1: Incidence rates of nonfatal occupational injuries and illnesses by selected industries and case types, 2007. 2008.
- 167.US Occupational Safety & Health Administration. Agricultural operations: hazards and solutions. Available at: http://www.osha.gov/SLTC/agriculturaloperations/recognition.html. Accessed March 16, 2009.
- 168.Azaroff LS, Lax MB, Levenstein C, Wegman DH. Wounding the messenger: the new economy makes occupational health indicators too good to be true. Int J Health Serv. 2004;34:271–303. doi: 10.2190/4H2X-XD53-GK0J-91NQ. [DOI] [PubMed] [Google Scholar]
- 169.Wilson SM, Howell F, Wing S, Sobset M. Environmental injustice and the Mississippi hog industry. Environ Health Perspect. 2002;110:195–201. doi: 10.1289/ehp.02110s2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Wing S, Cole D, Grant G. Environmental injustice in North Carolina's hog industry. Environ Health Perspect. 2000;108:225–231. doi: 10.1289/ehp.00108225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.United Nations Food and Agriculture Organization. The State of Food Insecurity in the World 2001. 2002.


