Abstract
Cervical spine fractures in patients with ankylosing spondylitis are serious and potentially lethal injuries with high complication rates. Treatment obstacles include long lever arms that generate large forces on any fixation device, osteoporosis, and, usually, kyphotic deformity. The Olerud Cervical Fixation System (OC), with cervical pedicle screws and rods, offers an opportunity to create a biomechanically stable posterior fixation in these complicated cases. The present study is a retrospective chart review and a radiological follow-up of patients with this diagnosis, treated at our department between 1995 and 2000. Nineteen patients (two women) with a mean age of 60 years (32–78 years) were included. The fracture levels were predominantly C5–C6 (five patients) and C6–C7 (five patients). All patients were treated with a long posterior fixation with the OC, and in four patients this was combined with an anterior plate fixation. One patient with severe lordosis also received a short posterior plate fixation. The patients’ notes and plain radiographs have been reviewed. Five patients died during the post-operative follow-up period; the others had a mean follow-up time of 24 months (10–55 months). Eleven patients had no neurological deficits preoperatively. One of them developed moderate weakness in his right arm, postoperatively, due to a misplaced pedicle screw in the right pedicle of C5. However, after extraction of the screw he almost totally recovered in 6 months. Eight patients had neurological deficits. Two were paraplegic; two had motor weakness combined with sensory deficiency, and four had a sensory deficiency. Two of the patients with neurological deficits improved postoperatively, but the others were unchanged. Peroperative problems were recorded in five patients; one C6 pedicle was perforated, and two patients had pedicles on one or more levels that the surgeon was not able to probe. In one of the latter patients, transfacet screws were chosen, instead, for one of the levels. Extensive peroperative bleeding was encountered in two patients. One deep-wound infection was noted, postoperatively, and required surgical drainage, but no patients have been re-operated due to loosening of the instrument or to healing problems. In conclusion, the results of the present study indicate that the OC—and possibly other similar long-fixation systems that allow using both pedicle screws and lateral mass screws rigidly connected to a rod—is suited for treating subaxial cervical spine fractures in patients with ankylosing spondylitis, allowing high healing rates.
Keywords: Spinal fusion, Spinal fracture, Fracture fixation, Cervical vertebrae, Ankylosing spondylitis
Introduction
Subaxial cervical spine fractures in patients with ankylosing spondylitis rarely come up in general discussions of cervical spine fractures, but they are quite common in patients with this disease. These fractures are serious and potentially lethal injuries [3, 5]. Trauma to the ankylosed cervical spine carries a poorer prognosis than similar injuries in cervical spines without ankylosis [25]. Fractures of the cervical spine in patients with ankylosing spondylitis were first described by Stiasny in 1933 [39]. The underlying disease process in ankylosing spondylitis transforms the vertebral column and its ligamentous attachments into a solid column of tubular bone through which the spinal cord passes [30]. The creation of a rigid spinal column, with the associated osteoporosis as the disease progresses, results in a brittle, rigid structure poorly suited to withstand stress. Thus, even minor trauma can result in a fracture [3, 5, 9, 10, 22, 30, 32, 35, 41]. The cervical spine, especially the lower cervical spine, is the most common site of fractures in these patients [22, 30, 32, 35, 41].
Treatment obstacles include marked instability in all planes [5], long lever arms generating large forces on any fixation device [3], osteoporosis [8], and, usually, kyphotic deformity [4, 14]. There have been several reports about associated higher complication rates [5, 14, 19, 30, 35] and higher rates of neurological deficit, compared with cervical spine fractures in patients without ankylosing spondylitis [10, 19, 30, 35]. Associated morbidity rates of 50% or more [10, 26] and high mortality rates of 20–50% are found in the literature [10, 14, 16, 22, 26, 30, 35, 42, 43].
Suggested methods for treatment of these fractures include non-surgical methods, such as axial traction [10], cervicothoracic bracing or halo vest treatment [5, 7, 22, 25, 35, 40, 43], and surgical methods such as anterior plating, posterior wiring techniques [18] and posterior plates fixed with lateral mass screws [41]. However, disadvantages and complications have been demonstrated with all these methods [8, 12, 22, 40].
The decreased bone quality due to osteoporosis gives a sub-optimal anchorage for spinal implants. In several series, using anterior plating or lateral mass screws, screw-loosening and screw pull-out have been demonstrated [8, 12]. The Olerud cervical fixation system (OC) (Anatomica AB, Askim, Sweden), with cervical pedicle screws and rods, gives an opportunity to create a more rigid and biomechanically stable osteosynthesis than the previously mentioned methods [33]. Constrained systems using cervical screws and rod fixation—the design of the OC system—have in biomechanical tests been demonstrated to create an increased primary stability [36].
The aim of this study was to retrospectively evaluate the outcome, with special reference to the radiological outcome, and to identify possible complications of posterior fixations with the OC system in patients with subaxial cervical spine fractures and ankylosing spondylitis.
Patients and methods
The study is based on data from all patients with ankylosing spondylitis and subaxial cervical spine fractures who, between 1995 and 2000, underwent a posterior fusion that used the Olerud cervical fixation system with transpedicular screws. The study design is a retrospective chart review and a radiological follow-up with plain radiographs. Nineteen patients were included, 17 men and 2 women, with a mean age of 60 years(32–78 years). Five died during the post-operative follow-up period. The others had a mean follow-up time of 24 months (10–55 months). Five patients were from the primary region around our hospital, but 14 were referred to us from other hospitals in Sweden, because we are a regional spine trauma center. Thirteen patients sustained fractures after falling whilst walking or standing; one fell from a lawn mover, one from a bicycle and one from a snow mobile. One patient sustained a fracture after a minor head trauma, from a falling tree branch; and one patient fell down a staircase. The remaining patient had no identifiable trauma.
The fracture levels were C5–C6 in five patients, C6 in four patients, C6–C7 in five and C7 in two (Table 1). One patient had a C2–C3 fracture, and one had a C4–C5 fracture. The remaining patient had a long and comminuted fracture from C4 to C7. Eight patients had neurological deficits, preoperatively. Two patients had total loss of motor and sensory function below the injured level; two had motor weakness combined with a sensory deficit, and four had a sensory deficit (one of them also had rhizopathic pain). All patients were treated with long posterior fixations with the OC system (Fig. 1 and Fig. 3), but four also had a concomitant anterior fixation with an anterior plate (CSLP cervical spine locking plate, Stratec Medical, Switzerland). One of the latter patients had an extra procedure—a short posterior fixation with a limited-contact-dynamic-compression plate (LCDCP) for fracture stabilisation (Stratec Medical, Switzerland) (Fig. 2). This patient was the only one for whom the occiput was included in the posterior fixation. This more proximal anchorage and the additional posterior plates were employed due to the severe deformity (Fig. 2), the preexisting ankylosis including the occipitocervical and atlantoaxial regions, and the surgeon’s determination that the fracture was extremely unstable. The decision to add an anterior fixation was up to the spine surgeon in charge of the operation, based on his preoperative evaluation of fracture stability.
Table 1.
Posterior fixation of subaxial cervical spine fractures: patient data. LCDCP limited-contact-dynamic-compression plate; CLSP cervical locking plate
| Pat-ient No. | Gender | Age (years) |
Fracture level |
Surgical method |
X-ray follow up (months) |
X-ray follow up status |
Death (months) | Cause of death |
|---|---|---|---|---|---|---|---|---|
| 1 | F | 54 | C6–C7 | OC C4–T3 | 15 | No healing disturbances | - | - |
| 2 | M | 67 | C6 | OC C2–T2 | 13 | Healed | - | - |
| 3 | M | 58 | C5–C6 | OC C2–T2 | 37 | Healed | - | - |
| 4 | M | 56 | C5–C6 | OC C1–T3 | 25 | No healing disturbances | - | - |
| 5 | M | 53 | C6–C7 | OC C3–T2 | 44 | Healed | - | - |
| 6 | M | 55 | C6 | OC C2–T3 | 23 | Healed | - | - |
| 7 | M | 76 | C6–C7 | OC C2–T5 | 45 | No healing disturbances | - | - |
| 8 | M | 49 | C7 | OC C4–T2 | 12 | No healing disturbances | - | - |
| 9 | M | 51 | C4–C7 | OC Occiput–T2+LCDCP+CLSP C6–C7 | 14 | Healed | - | - |
| 10 | M | 32 | C6 | OC C2–T1 | 55 | Healed | - | - |
| 11 | M | 60 | C6–C7 | OC C4–T2+CLSP C6–C7 | 10 | Healed | - | - |
| 12 | M | 69 | C4–C5 | OC C2–C7 | 6 | No healing disturbances | 18 | Pneumonia |
| 13 | M | 58 | C6–C7 | OC C3–T1+CLSP C6–C7 | 2 | No healing disturbances | 21 | Pneumonia and chronic respiratory insufficiency |
| 14 | M | 48 | C6 | OC C3–T1 | 9 | Healed | 33 | Pneumonia and chronic alcohol abuse |
| 15 | M | 76 | C5–C6 | OC C2–T1 | 3 | No healing disturbances | 53 | Lung edema |
| 16 | M | 78 | C2–C3 | OC C2–C4 | 14 | Healed | - | - |
| 17 | M | 54 | C5–C6 | OC C4–C7 | 11 | No healing disturbances | - | - |
| 18 | M | 64 | C5–C6 | OC C2–T2+CLSP C4–C7 | 5 | No healing disturbances | 11 | Intestinal obstruction and peritonitis |
| 19 | F | 78 | C7 | Decompression C7+OC C4–T3 | 17 | No healing disturbances | - | - |
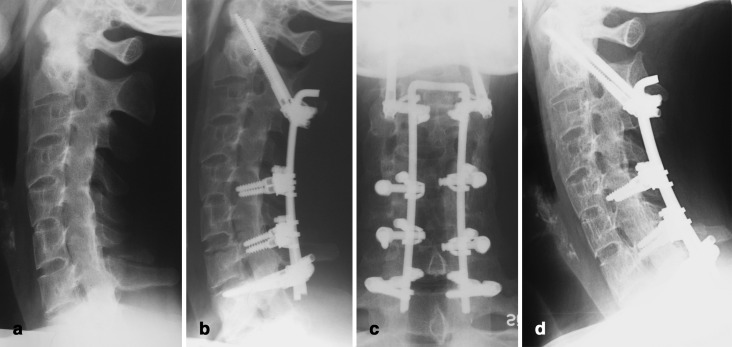
Fig. 1.
Radiographs of a 32-year-old man (No. 10 in Table 1) with ankylosing spondylitis. After a C6-fracture in a bicycle accident, he was stabilized with OC from C2 to T1, using transarticular screws in C2, pedicle screws in T1, and lateral mass screws at levels C5 and C7. a preoperative lateral; b postoperative lateral; c postoperative antero-posterior; and d lateral at follow-up at 55 months
Fig. 3.
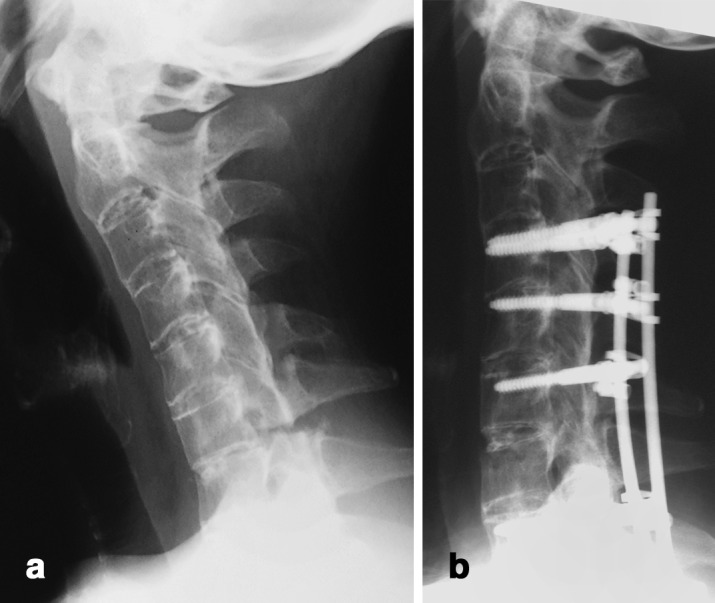
Radiographs of a 54-year-old woman (No. 1 in Table 1) with ankylosing spondylitis. A fall against a bookcase at home fractured level C6–C7. She was stabilised with OC from C4 to T3 using cervical pedicle screws and rods. a preoperative lateral; b postoperative lateral
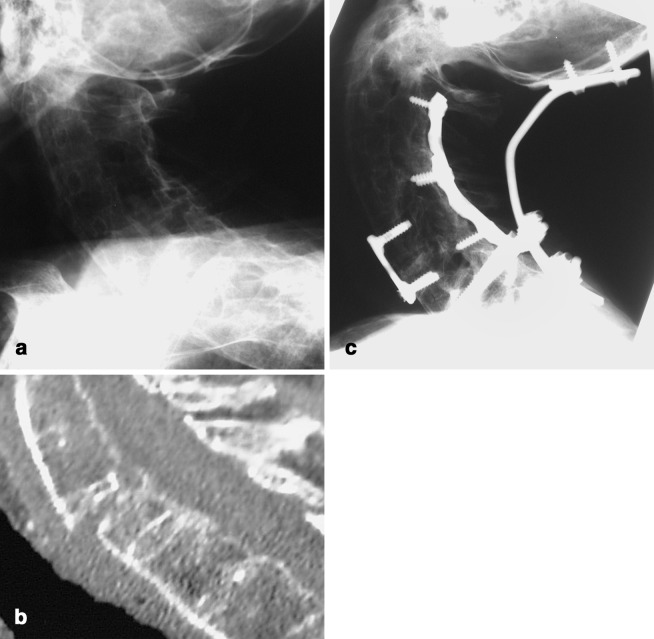
Fig. 2.
Radiographs of a 51-year-old man (No. 9 in Table 1) with ankylosing spondylitis. He fell indoors on his pelvic area, with an indirect axial compression of the spine. X-rays showed a C7-fracture. However, when the cervical spine was exposed surgically through a posterior approach, the fracture system was visible all the way up to the C4 level, posteriorly. Due to severe hyperlordosis in his cervical spine, and related problems in fixating long rods to the mid-cervical spine, he was stabilized with OC from occiput to T2, but also with an anterior plate at C6–C7 and posterior limited-contact-dynamic-compression plates (LCDCP) at C3–T1. a preoperative lateral; b preoperative CT (sagittal reformation); and c lateral at follow-up at 14 months
Pedicle screws were routinely used for fixation in C2 and C7 and the upper-thoracic spine. In the region between C3 and C6, lateral mass screws or transarticular screws (Fig. 1) were sometimes used instead of pedicle screws (Fig. 3). The decision between these alternative techniques was made by the operating surgeon, based on the demands of fracture stabilisation for each patient. To place cervical pedicle screws, a modified Abumi technique was employed, using a lateral C-arm view, anatomic landmarks, creating a large hole in the lamina at the pedicle entrance and gently probing the pedicle before screw insertion. Altogether, 109 pedicle screws were placed, 25 in C2 pedicles, 42 between C3 and C7 and 52 in the upper-thoracic pedicles. Additionally, 16 lateral mass screws and two transarticular screws were used in the region between C3 and C7. There was no primary aim of the surgeon to reduce a pre-traumatic spine deformity when stabilising the cervial spine fracture. The anterior fixations were performed before the posterior fixations in all patients with 360° fixations. Computer-assisted surgery was available for the last patient in the series (VectorVision, BrainLab AG, Germany).
Mean operation time was 3 h 25 min (2 h 05 min–6 h 10 min) and mean blood loss for the surgical procedure was 2,119 ml (450–6,800 ml). Postoperatively, patients were mobilized in a semi-flexible plastic collar of Aspen or Philadelphia type for the first 8 weeks. The patients have been followed with plain radiographs.
Results
Eleven patients had no neurological deficits preoperatively. One of them developed a moderate weakness in his right arm postoperatively (No. 15 in Table 1), due to a misplaced pedicle screw in the right pedicle of C5. However, after extraction of the screw he almost totally recovered to the 6-month follow-up. Out of the eight patients with neurological deficits preoperatively, two improved postoperatively during their hospital stay, but the others were unchanged. In five patients peroperative problems were recorded; one C6 pedicle was perforated, and two patients had pedicles on one or more levels that the surgeon was not able to probe. In one of the latter patients, transfacet screws were chosen, instead, for one of the levels. Extensive peroperative bleeding was noted in two patients. The postoperative radiological evaluation demonstrated that one cervical pedicle screw was superiorly misplaced, and this screw required extraction, as mentioned above. Two cervical pedicle screws were laterally misplaced in the pedicles, and one was caudally misplaced. Three thoracic pedicle screws were laterally misplaced, and one was slightly medially misplaced. None of the latter seven screws were found to induce any symptoms, and they did not require surgical extraction. However, all the misplaced cervical pedicle screws were evaluated with a postoperative CT scan to determine their position. In summary, four of the 67 cervical pedicle screws (6%) and four of the 52 (8%) thoracic pedicle screws were misplaced.
The radiological follow-up has not shown any signs of disturbed healing, non-unions or loosening of implants. As the follow-up has been performed using plain radiographs, definitive healing can be hard to determine. Still, in nine of the patients, bone trabeculae were seen bridging the fracture, all the way from the vertebra above the fracture to the vertebra below the fracture, without any discontinuity (classified as “healed” in Table 1). In the remaining 10 patients, it was not possible to visualise new bone trabeculae bridging the fracture all the way from the vertebra above to the one below, but there were no signs of mechanical failure of the implant or a radiolucent zone across the fracture level (classified as “no healing disturbances” in Table 1).
Except for the extraction of the misplaced C5 pedicle screw, inducing neural compromise as mentioned above, no re-operations due to implant-related problems have been performed. However, one patient developed a deep-wound infection requiring surgical drainage with insertion of local antibiotics in the form of gentamicin balls (No. 13 in Table 1).
Five patients have died from unrelated causes: at 11 months (intestinal obstruction and peritonitis), 18 months (pneumonia), 21 months (pneumonia and chronic respiratory insufficiency), 33 months (pneumonia combined with chronic alcohol abuse) and at 53 months (lung edema) postoperatively. These five were the only ones not followed for at least 10 months.
Discussion
The treatment of this selected group of patients with ankylosing spondylitis and cervical spine fractures is challenging. Several treatment obstacles have to be surmounted. The ossified spine in ankylosing spondylitis is more easily susceptible to fractures than non-ossified spines, due to changed biomechanics with long lever arms, pre-existing kyphotic deformity and often severe osteoporosis [12, 32]. The cervical spine is the most common site of spine fractures in patients with ankylosing spondylitis, accounting for about 75% of the spinal fractures in these patients [22]. The fractures mainly occur in the lower cervical spine, predominantly C5–C7 [10, 20, 22, 26, 35, 39]. Imaging problems, due to the deformity and osteoporosis, and the fact that these fractures often occur after minimal trauma, frequently delay the diagnosis [4, 22, 25, 26]. Patients with cervical spine fractures and ankylosing spondylitis have a high incidence of neurological injuries at admission and appear to be more susceptible to develop large epidural hematomas [4, 10, 13, 15, 35]. Rehabilitation is also a problematic field—increased difficulty in rehabilitating cord-injured patients with pre-existing ankylosing spondylitis has been demonstrated [31].
Murray and Persellin have discussed fracture mechanisms in ankylosing spondylitis [30]. According to them, hyperextension is the most common mechanism of fracture in patients with ankylosing spondylitis, due to the rigidity of the spine and the position of the head and neck in relationship to the thoracic spine. They asserted that flexion injuries do occur, but less frequently, and they are often induced by forces directed anteriorly against the posterior aspect of the head [30]. In our opinion, this is a misconception. It is true that the majority of patients present with an extension deformity on the primary radiographs, but this is probably an acquired deformity, secondary to the radiographs, usually obtained with the patients in supine position. In the typical patient, before the spine is fractured, the spine has a C-shaped deformity. When supine, the contact area between the back of the patient and the supporting surface of the bed will be at a point somewhere in the middle of the spine, whereas the back of the head and the pelvic area are unsupported (i.e., hanging in free air). The entire spine will be subjected to a three-point bending moment. After a fracture, the spine has a limited amount of supporting soft tissues, and the forces on the fracture site are great due to the long lever arms. Consequently, both the back of the head and the pelvis will tend to seek contact with the bed. The previous C-shaped spine will turn into a “double C-shape”, with a hyperextended fracture site. Thus, any type of fracture mechanism may produce a hyperextension deformity of the fracture, as long as the patient is examined in supine position. This mechanism is probably also a major contributing factor to the development of late neurological symptoms, even weeks after a seemingly trivial injury, that have been reported in ankylosing spondylitis [5, 14, 16, 22, 32]. The soft tissues around the spine may suspend the fracture initially, but as time passes, the periosteal envelope fails, with secondary deformity in hyperextension, which may result in neurological compromise.
Cervical spine fractures in patients with ankylosing spondylitis are often highly unstable [17, 30, 32] and invariably transverse the entire width of the spine, inducing a multidirectional instability. Non-surgical treatment—axial cervical traction and cervicothoracic bracing—cannot be recommended, due to an unacceptably high frequency of complications [3, 7], including death [7]. Halo vest treatment, advocated by some authors as the optimal treatment method [25], is also associated with complications [18, 22, 25, 34, 40, 43]. Even if the majority of patients placed in a halo vest achieve spinal fusion, there are reports of dislocations, non-unions or increased neurological deficits during the treatment [10, 22, 32, 40]. Due to the above-mentioned features, surgical treatment of cervical spine fractures in patients with ankylosing spondylitis is appealing, because it produces immediate stability without the need for cervical traction with prolonged bed rest or a demanding immobilisation in a halo vest. Internal fixation is the only possible means to stabilise the spine with preserved “pre-trauma” deformity, avoiding a local hyperextension, which could have devastating consequences for neural structures. Several operative techniques have been described [8, 41].
For cervical spine stabilisation in general, both biomechanical and clinical studies have demonstrated better primary stability with posterior stabilisation techniques, compared with stand-alone anterior plating [6, 11, 36, 38]. Constrained pedicle-screw and rod systems have been proposed to give a better stability than non-constrained systems [36]. The pull-out strength of various screw-placement techniques in the cervical spine has been analysed. Pedicle screws have been demonstrated to offer the best pull-out resistance of all available posterior fixation techniques, with an 88% increase in pull-out strength, compared with lateral mass screws [23]. Transfacet screws, another screw-placement method, have been reported to have a 30% better pull-out strength than lateral mass screws [27]. Possible differences in the pull-out resistance of bicortical and unicortical types of lateral mass screws have also been evaluated [21, 29, 37]. No significant increase in screw purchase was demonstrated using the bicortical technique, as compared with the unicortical.
The special problems associated with ankylosing spondylitis require special considerations when choosing the internal fixation technique. Due to the long lever arms and weak bone stock, short anterior or posterior fixations will not work. Long posterior fixation with screws and plates may also fail due to screw loosening [8]. The combination of anterior and posterior “360°” fixations is reported to stabilize the spine [32] but to require very extensive surgery.
The OC system allows rigid connection between the screws and the longitudinal rods of the construct, thus eliminating the possibility that screws will back out. The versatility of the device also allows optimal screw positioning to be chosen in osteoporotic bone. The constructs can be adapted to a preexisting deformity, which would make them suitable for treating cervical spine fractures in ankylosing spondylitis patients. In a biomechanical study the OC results in initial stability that is equal to that of a posterior screw-plate construction. However, contrary to the screw-plate construct, the OC stability is preserved during cyclic loading (Dr Brian Cunningham, data on file). It is our opinion that, in order to allow a comparison with the results reported in the present study, other posterior fixation systems need to have the possibility of using both freely placed cervical pedicle screws and/or lateral mass screws, and a successive rigid connection to a rod.
The rate of misplaced cervical pedicle screws in the present study, four out of 67 (6.0%), must be considered quite low, especially considering the problem of finding normal anatomic landmarks in patients with ankylosing spondylitis. In a large clinical series, Abumi and co-workers reported 45 misplaced screws out of 669 evaluated screws (6.7%) [2]. The same group of authors reported 6.3% of the pedicles perforated and two out of the 142 evaluated screws inducing radiculopathy, using a pedicle screw system for fixation after correction of cervical kyphotic deformities [1]. In a cadaver study [28], Ludwig and co-workers, using the Abumi insertion technique in 67 cervical pedicles, demonstrated a 12% misplacement rate, described as “critical breaches” and in another 50 pedicles, using CAOS (Stealth Station, Sofamor Danek, Memphis, TN), reported 18% “critical breaches”. They concluded that, “The use of a computer-assisted image guidance system did not enhance safety or accuracy in placing pedicle screws, compared with Abumi’s technique”. In another cadaver study evaluating 120 cervical pedicle screws, 16.8% perforations were demonstrated, 7.1% classified as critical and 9.7% as non-critical [24].
The average blood loss of 2,119 ml recorded for the surgical procedures in the present study is quite high, compared with most surgical procedures in the cervical spine. However, this must be compared with other surgical procedures, keeping in mind that patients with ankylosing spondylitis have an increased tendency to bleed from their fractures, compared with patients without this disease [13]. Also, stabilising these fractures is time-consuming due to the special biomechanical problems already mentioned.
In the present study there were no re-operations for mechanical failure, and no patient sustained an increased neurological injury due to secondary displacement. The only neurological worsening was due to a misplaced screw, which is a non-implant related complication. All fractures healed or were without signs of healing disturbances at follow-up.
Conclusions
The results of the present study indicate that the OC—and possibly other long fixation systems that, like the OC, allow using both pedicle screws and lateral mass screws rigidly connected to a rod—is suited for treating subaxial cervical spine fractures in patients with ankylosing spondylitis, allowing high healing rates. The complication rate was found to be acceptable and no higher than in other non-surgical or surgical series.
References
- 1.Abumi Spine. 1999;24:2389. doi: 10.1097/00007632-199911150-00017. [DOI] [PubMed] [Google Scholar]
- 2.Abumi Spine. 2000;25:962. doi: 10.1097/00007632-200004150-00011. [DOI] [PubMed] [Google Scholar]
- 3.Amamilo Orthop Rev. 1989;18:339. [PubMed] [Google Scholar]
- 4.Bohlman J Bone Joint Surg Am. 1979;61:1119. [PubMed] [Google Scholar]
- 5.Broom Spine. 1988;13:763. doi: 10.1097/00007632-198807000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Coe Spine. 1989;14:1122. doi: 10.1097/00007632-198910000-00016. [DOI] [PubMed] [Google Scholar]
- 7.CooperJ Neurosurg 197951603430154 [Google Scholar]
- 8.Cooper Neurosurgery. 1988;23:300. doi: 10.1227/00006123-198809000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Cooper J Rheumatol. 1994;21:1877. [PubMed] [Google Scholar]
- 10.Detwiler J Neurosurg. 1990;72:210. doi: 10.3171/jns.1990.72.2.0210. [DOI] [PubMed] [Google Scholar]
- 11.DoSpine 2001261511148640 [Google Scholar]
- 12.Exner Spinal Cord. 1998;36:377. doi: 10.1038/sj.sc.3100673. [DOI] [PubMed] [Google Scholar]
- 13.FarhatJ Trauma 1973135914715027 [Google Scholar]
- 14.Farmer J Spinal Disord. 1988;11:192. [PubMed] [Google Scholar]
- 15.FooNeurosurgery 198211257110563 [Google Scholar]
- 16.Foo Paraplegia. 1985;23:358. doi: 10.1038/sc.1985.57. [DOI] [PubMed] [Google Scholar]
- 17.Fox J Neurosurg. 1993;78:871. doi: 10.3171/jns.1993.78.6.0871. [DOI] [PubMed] [Google Scholar]
- 18.Gallie Am J Surg. 1939;46:495. doi: 10.1016/S0002-9610(39)90309-0. [DOI] [Google Scholar]
- 19.Graham Spine. 1989;14:803. doi: 10.1097/00007632-198908000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Harding Br J Radiol. 1985;58:3. doi: 10.1259/0007-1285-58-685-3. [DOI] [PubMed] [Google Scholar]
- 21.Harris Spine. 2001;26:2427. doi: 10.1097/00007632-200111150-00006. [DOI] [PubMed] [Google Scholar]
- 22.Hunter Ann Intern Med. 1978;88:546. doi: 10.7326/0003-4819-88-4-546. [DOI] [PubMed] [Google Scholar]
- 23.Jones Spine. 1997;22:9777. doi: 10.1097/00007632-199705010-00009. [DOI] [Google Scholar]
- 24.Karaikovic Spine. 2001;26:2456. doi: 10.1097/00007632-200111150-00012. [DOI] [PubMed] [Google Scholar]
- 25.Kewalramani J Trauma. 1975;15:931. doi: 10.1097/00005373-197510000-00016. [DOI] [PubMed] [Google Scholar]
- 26.Kiwerski Int Orthop. 1985;8:243. doi: 10.1007/BF00266867. [DOI] [PubMed] [Google Scholar]
- 27.Klekamp J Spinal Disord. 2000;13:515. doi: 10.1097/00002517-200012000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Ludwig Spine. 2000;25:2675. doi: 10.1097/00007632-200010150-00022. [DOI] [PubMed] [Google Scholar]
- 29.MuffolettoSpine 200328778. 10.1097/00007632-200304150-0000912698120 [DOI] [Google Scholar]
- 30.Murray Am J Med. 1981;70:1033. doi: 10.1016/0002-9343(81)90860-3. [DOI] [PubMed] [Google Scholar]
- 31.Ohry Paraplegia. 1984;22:291. doi: 10.1038/sc.1984.47. [DOI] [PubMed] [Google Scholar]
- 32.Olerud Eur Spine J. 1996;5:51. doi: 10.1007/BF00307827. [DOI] [PubMed] [Google Scholar]
- 33.Olerud Ups J Med Sci. 1999;104:131. doi: 10.3109/03009739909178957. [DOI] [PubMed] [Google Scholar]
- 34.Papagelopoulos Spine. 2001;26:E463. doi: 10.1097/00007632-200110010-00030. [DOI] [PubMed] [Google Scholar]
- 35.Rowed J Neurosurg. 1992;77:241. doi: 10.3171/jns.1992.77.2.0241. [DOI] [PubMed] [Google Scholar]
- 36.Schmidt Spine. 2003;28:1821. doi: 10.1097/01.BRS.0000083287.23521.48. [DOI] [PubMed] [Google Scholar]
- 37.Seybold Spine. 1999;24:2397. doi: 10.1097/00007632-199911150-00018. [DOI] [PubMed] [Google Scholar]
- 38.Singh Spine. 2003;28:2352. doi: 10.1097/01.BRS.0000085344.22471.23. [DOI] [PubMed] [Google Scholar]
- 39.Stiasny Zentralbibl Chir. 1933;60:998. [Google Scholar]
- 40.Surin Acta Orthop Scand. 1980;51:79. doi: 10.3109/17453678008990772. [DOI] [PubMed] [Google Scholar]
- 41.Taggard Spine. 2000;25:2035. doi: 10.1097/00007632-200008150-00006. [DOI] [PubMed] [Google Scholar]
- 42.Weinstein J Neurosurg. 1982;57:609. doi: 10.3171/jns.1982.57.5.0609. [DOI] [PubMed] [Google Scholar]
- 43.Young Paraplegia. 1977;15:133. doi: 10.1038/sc.1977.19. [DOI] [PubMed] [Google Scholar]