Abstract
The total costs for patients who are sick-listed due to back and neck problems have not previously been determined prospectively on an individual basis. This study aimed to determine the total cost to a society, based on individually assessed costs of health services and loss of production in people who are sick-listed 28 days or more for back or neck problems. Detailed data on individuals’ health-care consumption due to back or neck problems was collected through prospectively entered diaries and questionnaires, after 4 weeks, 3 months, 1 and 2 years, in a consecutively selected cohort of 1,822 employed persons aged between 18 and 59 years. Costs for health care and production losses due to work absenteeism were determined individually and combined to render total costs to society. The costs for all medical services during the 2-year study were 6.9% of total costs for back and neck problems. The single most expensive medical service was surgery. Transferred to a national level, annual total costs for back and neck problems corresponded to 1% of GNP. In conclusion, direct health-service costs were a small fraction of the total costs, consequently indirect costs offer the greatest potential for savings.
Keywords: Back pain, Neck pain, Cost of illness, Disability, Sick-listing
Introduction
Low back and neck problems are especially frequent during the most productive years of a person’s life, causing a large number of lost workdays and production losses [29, 30, 31, 43, 45]. Studies in the UK [6] and the USA [13] have shown that chronic back and neck ailments (duration >3 months) contribute to more than two-thirds of the total costs for this type of problem. Back-pain costs in the Netherlands have been estimated at 1.7% of its GNP [22, 41]. In Sweden, annual costs for those sick-listed due to low back or neck problems have been estimated at 3.5 billion euros, corresponding to nearly one-third of the nation’s total health-care costs (1995) [27]. Around 80% of people with back problems are pain-free within 2 weeks, and over 90% are within 3 months [5]. Nevertheless, the extremely high prevalence translates into a substantial number of people in absolute figures, with high demands for health services and consequent costs, especially for loss of production [1, 28, 33, 38, 42].
Treatment, or direct, costs for back problems are generated in many different therapeutic environments. These and other circumstances make an accurate determination of frequencies and magnitudes difficult. In Sweden, for example, recording data about an individual’s diagnoses, certifying physician and health consumption, etc., has not been allowed or is not done [37]. Because of this, epidemiological studies of the treatment costs of back and neck problems must rely on top-down estimates [16].
A study initiated in 1994 by the Swedish National Insurance Board provided a unique opportunity to gain access to individual diagnoses and thus determine individual costs for low back or neck problems in a “bottom-up” approach [2]. The main objective of the present study was to determine society’s costs (“cost-of illness”) for low back and neck problems in a cohort of initially sick-listed, employed men and women, during a 2-year period. Additional objectives were to determine the relation between direct and indirect costs, to extrapolate those costs to an annual, national level, and to use the results as a baseline for further economic evaluations.
Material and methods
Participants
The participants in the study were consecutively selected from five (of 21) Swedish regional, social insurance offices, located in the northern, middle and southern parts of Sweden and in the two largest cities. Inclusion took place between November 1994 and October 1995. Eligibility required full work incapacity for a minimum 28 days, due to physician-certified low back or neck problems (ICD 10: M 47, 48, 50, 51, 53, 54 or 79). The participants, who were followed for 2 years, had to be employees 18–59 years of age. The study was a combined questionnaire and registry with postal, self-administered questionnaires after 28 and 90 days, 1 and 2 years. Special diaries were also used.
The questionnaire study
The questionnaires covered background information such as the individual’s finances (the first questionnaire) and included questions about examinations, treatments or rehabilitation activities due to the present spine problems. In complement, every person was asked to note all contacts, referrals, appointments, visits, type of examinations, and treatments, etc., in the special diary [12].
The registry study
All information about subjects’ working status (e.g., sick-listing or other benefits) was obtained through the National Social Insurance Board’s central registers. Each participant’s informed consent was obtained, and the Ethics committee at Göteborg University approved the study.
Exclusion criteria
The following exclusion criteria were used:
Unemployment
Self employment
Back or neck problems related to pregnancy, fracture(s), tumour, infection or generalised inflammatory disorders
Back surgery during the preceding year
The cohort
The 1,822 included individuals were asked about interventions that had occurred starting from the first day of sick-listing, by questionnaire at 90 days, then at 1 and 2 years, and also asked to enter this information in the diaries. Thus, the analysis is based on responses of the 1,146 (63%) individuals who completed the 90-day questionnaire. Complete sick-listing information for the entire study period was obtained for all 1,822 (100%).
Costs of illness
In this study, society’s costs are the direct and indirect costs associated with low back or neck problems during the 2-year period. They are not related to outcome or so-called intangible costs.
Direct costs
Direct costs include all those for examination, treatment and rehabilitation [14]. Data about resource consumption was collected and each item multiplied by its cost. Prices from a variety of sources were used. For example, nationally determined price lists were consulted to determine the cost of visits to a physician or a physiotherapist [14, 21]. Costs for various interventions requiring hospital care, such as surgery, were obtained from the accounting offices of at least one hospital within the participating region.
Direct non-medical costs, e.g., for transportation to a physician, were not included. All costs are given in 1995 prices. The special price index for Swedish health care was used for adjustments between different years during the study period.
Indirect costs
The human capital method estimates potential production loss or potentially lost income as a consequence of disease [8, 20], based on the assumption that earnings reflect productivity [41]. Using this method, daily production loss on an individual basis was calculated. This was multiplied by the actual number of days lost until the end of the second year, when applicable. Each individual’s number of sick-leave days was obtained from the National Social Insurance Board’s central registers, which contain the latest information of all citizens’ income that qualifies for health benefits (SGI). Production loss was computed as the time units lost, multiplied by a valuation of cost per time unit. The latter equals SGI plus the employer’s payroll taxes (33% of gross income in 1994–95), here converted into a daily cost. For individuals with a partial benefit, production loss was calculated as the number of whole days off work. For individuals granted a permanent disability benefit during the study period due to actual problems, production lost was calculated up until the first day of old-age pension (65 years), based on life expectancy from Statistics Sweden. A 5% discount rate and an assumed annual increase in productivity of 1.5% were used to convert future years’ production loss to present value. Future production losses are discounted with a rate generally corresponding to the long-term real, risk-free interest rate on capital investments [8, 46].
Results
Cost of illness
Direct costs
The number of different examinations and treatments, when and in what order they occurred varied considerably (Table 1). Specified costs for all included medical interventions are presented in Table 2. Total direct costs during the 2-year study for the 1,146 people completing the questionnaire after 90 days were 2,073,837 euros, with an average direct cost per subject of 1,810 euros.
Table 1.
Relative frequencies of visits to various types of physicians, other professionals, and treatments received after 28 days, 90 days, 1 and 2 years (accumulated); and the average number of treatments for each subject
| Treatment | 28 days | 90 days | 1 year | 2 years | Average |
|---|---|---|---|---|---|
| General practitioner | 61 | 66 | 70 | 71 | 4.3 |
| Company physician | 19 | 23 | 27 | 27 | 3.5 |
| Private practitioner | 8 | 10 | 12 | 12 | 3 |
| Orthopaedic surgeon | 18 | 30 | 37 | 64 | 1.9 |
| Neurologist | 2 | 4 | 6 | 7 | 1.9 |
| Psychiatrist | 1 | 3 | 3 | 4 | 2.6 |
| Rehabilitation specialist | 2 | 5 | 8 | 9 | 2.7 |
| Other physician* | 7 | 14 | 18 | 19 | 2.1 |
| Disc surgery | 2 | 4 | 7 | 8 | 1 |
| Physiotherapist** | 52 | 72 | 78 | 79 | 11.8 |
| Chiropractor | 7 | 9 | 12 | 13 | 4.2 |
| X-ray | 38 | 55 | 63 | 64 | 1.4 |
| Computerized tomography (CT) / magnetic resonance imaging (MRI) | 9 | 16 | 25 | 30 | 1.3 |
| Medications*** | 71 | 73 | 57 |
*Specialists of types not listed in questionnaires
**Treatment could consist of physical activity, heat or cold, ultrasound, acupuncture, manipulation, traction, TENS (trans-cutaneous electrical nerve stimulation), massage or zone therapy
***Include analgesics, injections such as nerve blocks, steroids etc. Not accumulated
Table 2.
The costs for every intervention, and total costs (in euros) during the 2-year period
| Treatment | Cost per unit | Total direct costs (2 years) |
|---|---|---|
| General practitioner* | 93 | 316,744 |
| Company physician | 93 | 99,168 |
| Private practitioner | 93 | 35,225 |
| Orthopaedic surgeon | 153 | 231,706 |
| Neurologist | 135 | 21,412 |
| Psychiatrist | 153 | 17,282 |
| Rehabilitation specialist | 93 | 40,988 |
| Other physician | 93 | 69,129 |
| Back surgery (Disc surgery)** | 3,671 | 490,588 |
| Physiotherapist | 38 | 389,045 |
| Chiropractor | 38 | 35,680 |
| X-ray*** | ||
| Computerized tomography (CT) / magnetic resonance imaging (MRI)**** | 412 | 153,882 |
| Medications***** | 0.80 | 172,988 |
| Total | 2,073,837 |
*Costs obtained through nationally determined price lists
**An average from five hospitals including all costs before and after surgery. Costs were obtained from the accounting offices in at least one hospital within the participating region
***Cost of a plane X-ray examination was included in the cost for an outpatient visit to a physician and, thus, included in direct costs
****An average from five hospitals. MRI or CT was not differentiated in the questionnaires
*****Based on information from a group of spine physicians. Actual prices were obtained from the national price list (FASS). Drug costs were calculated as an average daily cost for each individual
Indirect costs
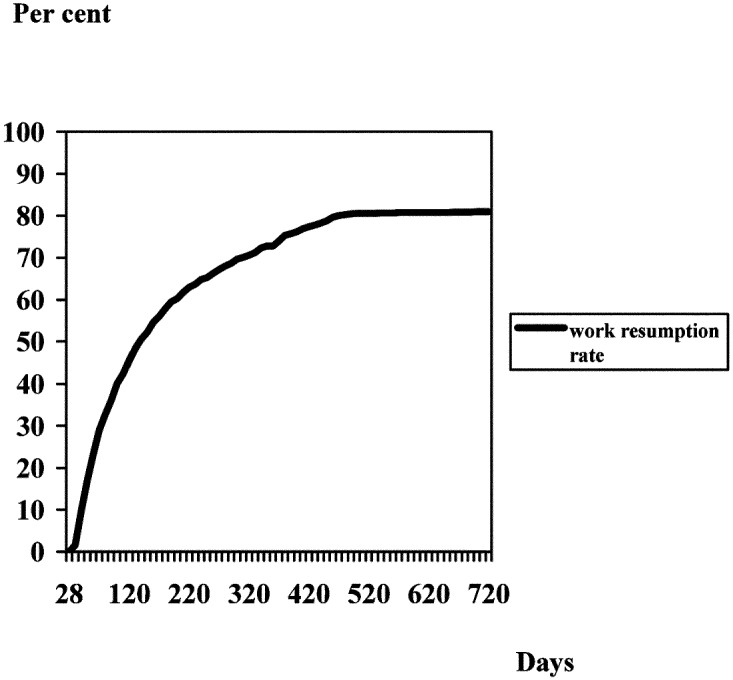
The average and median monthly salaries (SGI) for the study participants were 1,190 euros (mean) and 1,137 euros (median), excluding wage taxes. After 3 months, counted from the first day of sick-listing, 36% of the participants had returned to work. After 1 year the corresponding figure was 72% (Fig. 1). At completion of data collection after 2 years, 225 people had not resumed work. One hundred and thirty-seven were still sick-listed; 40 had been granted full (100%) or partial permanent disability benefits, and 48 received temporary full or partial disability benefits. The total indirect cost during the 2 years was 21,135,927 euros.
Fig. 1.
Participants’ relative work-resumption rates during the 2 years of the study
Estimation of production loss due to permanent disability
SGI plus wage taxes were also used to estimate production loss for the 40 people granted a full (14 people) or partial (26) permanent disability benefit during the study period. Production loss due to permanent disability mounted when calculated with a discount factor of 5% and an annual, estimated increase in productivity of 1.5%, to 7,692,297 euros.
The effect of various discount factors and estimated productivity increases are presented in Table 3.
Table 3.
Sensitivity analysis. Calculation of present value of production losses for participants (responders) granted a full or partial, permanent disability benefit during the study period
| Present value (euros) | |||
|---|---|---|---|
| Productivity factors | Discount factor 0% | Discount factor 3% | Discount factor 5% |
| 0% | 10,031,704 | 7,972,305 | 6,935,721 |
| 1.2% | 8,710,900 | 7,531,363 | |
| 1.5% | 8,911,830 | 7,692,297 | |
| 2% | 9,262,777 | 7,972,305 | |
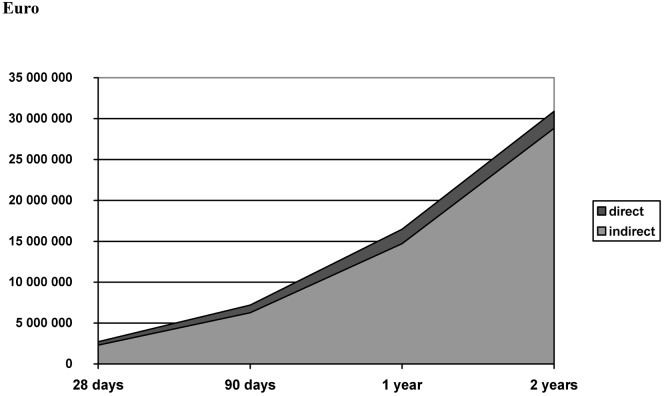
Total costs for the 1,146 people
At study’s end, the direct costs of 2,073,838 euros, indirect costs of 21,135,927 euros, and 7,692,297 euros in lost production (due to permanent disability benefit) totalled 30,902,062 euros for the 1,146 participants. As can be seen in Fig. 2, direct costs were only a minor fraction of total costs. After 28 days, direct costs were 15% of total cost. This declined to 13% at 90 days, 11% at 1 year and 7% at 2 years.
Fig. 2.
Accumulated total costs (direct and indirect) for back and neck patients estimated for the 1,146 participants during the 2-year study period
Non-response analysis
Information available for all 1,822 participants in the study (Table 4) was used in the non-response analysis. A linear relationship existed between the dependent variable (direct cost) and one or several independent variables among responders (1,146), and it was also reasonable to assume a similar relation among non-responders. Consequently, linear-regression analysis was used for the non-response analysis [10]. When linear-regression analysis was performed using direct cost per individual as the dependent variable and taking the variables listed in Table 4 as independent variables, it was found that three of the independent variables (number of days sick-listed, diagnosis, i.e., lower back pain vs neck pain, and working at 90 days) were significantly related to the dependent variable (R2=0.58). Expected values for non-responders were predicted using the corresponding regression relations from responders.
Table 4.
Analysis of non-responders in comparison to responders. Information available for all participants (1,822=100%) in the cohort
| Variable | Non-responders | p value |
|---|---|---|
| Gender | Relatively more men | 0.000 |
| Age | Lower mean age | 0.000 |
| Diagnosis | Relatively more with LBP | 0.000 |
| Days of sick-listing | Relatively more with fewer days on benefits | 0.000 |
| Working at 90 days | Relatively more | 0.000 |
| Working at 1 year | Relatively more | 0.000 |
| Working at 2 years | Relatively more | 0.000 |
| Present income | No difference | n.s |
Direct costs for non-responders
Thus, the predicted direct cost during the 2 years for the 676 non-responders was 1,154,447 euros, with a per-subject mean of 1,708 euros.
Indirect costs for non-responders
Production loss for the 676 non-responders during the study period totalled 9,057,776 euros. Seven non-responders were granted full permanent disability and 18 received partial permanent disability. When production losses—due to permanent disability benefits—were calculated for the non-responders in the same way as for responders (i.e., with a 5% discount factor and 1.5% increase in productivity) they mounted to 5,753,574 euros (Table 5).
Table 5.
Sensitivity analysis. Calculation of present value of production losses for participants who had been granted a full or partial, permanent disability benefit during the study period among non-responders
| Present value (total, in euros) | |||
|---|---|---|---|
| Productivity factors | Discount factor 0% | Discount factor 3% | Discount factor 5% |
| 0% | 6,844,109 | 5,975,283 | 5,157,422 |
| 1.2% | 6,562,521 | 5,626,398 | |
| 1.5% | 6,722,824 | 5,753,574 | |
| 2% | 7,003,323 | 5,975,283 | |
Total costs for non-responders
With direct costs of 1,154,447 euros, indirect costs of 9,057,776 euros and production loss due to permanent disability benefit of 5,753,574 euros, costs for non-responders totalled 15,965,797 euros, of which direct costs were 7.2%.
Total costs for back and neck pain patients
Total costs for all 1,822 participants during the study were 46,867,859 euros. (Table 6.
Table 6.
Total costs (direct and indirect) for back and neck patients, estimated for all 1,822 patients during the 2-year study period
| Direct cost | Indirect cost | Indirect cost including future years’ production loss for permanent disability benefit | Total costs | |
|---|---|---|---|---|
| Participants | 2,073,838 | 21,135,927 | 28,828,224 | 30,902,062 |
| Non-responders | 1,154,447 | 9,057,776 | 14,811,350 | 15,965,797 |
| Total | 3,228,285 | 30,193,703 | 43,639,574 | 46,867,859 |
Low back and neck problems and the Swedish GNP
The average, annual total cost mounted to 17,780 euros (1995) for each individual in our study. For the year 2001, that corresponded to an average total cost per person of 18,666 euros. According to the National Swedish Social Insurance Board (RFV), the total number of persons sick-listed 30 days or longer during 2001 was 694,000. ICD10 back or neck diagnoses (M 47, 48, 50, 51, 53, 54 or 79) caused 19%, or 131,860 people, to be sick-listed. During 2001, 11,558 people received new temporary or permanent disability benefits for those diagnoses, corresponding to 20% of all such benefits awarded that year (RFV). The total number of sick-listed people and people granted temporary or permanent disability for back or neck problems in 2001 was 143,418 persons. This figure multiplied by the average total cost per person determined by this study mounted to 2.7 billion euros. Thus, costs for back and neck problems amounted to about 1% of Sweden’s 2001 GNP of 262 billion euros. The 143 418 persons generating those costs corresponded to 3.3% of the available work force (4,414,000) that year.
Discussion
To our knowledge, this is the first time that all costs for the sick-listing of workers due to back or neck problems have been determined prospectively based on individual data (“bottom up”). Since the selection mechanism seemed to imply that the included people were typical neck and back patients, it is reasonable to assume that the results reflected everyday treatment of these types of patients, at least in Sweden. Striking similarities between the treatments of Swedish patients and those included in simultaneously studied cohorts, with the same inclusion criteria, in Germany, Denmark, the Netherlands, Israel and USA suggest that direct costs, at least relatively, are quite comparable in those countries [4, 15]. By only including employed people the same health-insurance rules applied for all participants throughout the country. For employed people, public health insurance replaces income starting the second day. A physician’s certificate is required for compensated absence after 7 days, and 80% (plus, in most cases 10% from collective insurance) of income is replaced, up to a ceiling of about 7.5 × an average full-time salary. The self-employed were not included, because they can choose individual health-insurance policies with varying lengths of coverage and compensation levels, factors known to be incentives (or disincentives) for the insured’s propensity to utilize benefits [4, 7]. In comparison with the Swedish census report, the present study cohort included a greater number than expected of people with lower education levels and those employed especially in the service, care, merchandise and construction sectors. These sectors are known to be over-represented as recipients of health-insurance benefits [7, 40]. The average and median monthly salaries for the study participants was substantially lower than the mean of the corresponding age groups of the entire Swedish population, something also noticed in other studies of similar groups [2, 16, 31]. Those findings also suggest that the study cohort was at least fairly representative when it comes to trade, employment and income. Currently, the estimation of Swedish society’s costs (top-down) for back and neck problems is only based on results from local populations [32, 35]. Direct health-care costs are typically estimated using census figures, but based on limited or no direct information on treatments [14, 21]. In other words, there are no results in Sweden based on costs generated by the individual back or neck patient (bottom-up), regionally or nationally. There are, however, studies reporting the costs of back or neck problems in evaluating effects of various specified treatments [11, 34, 35]. In contrast, our study was designed to capture all treatments and costs of the typical Swedish back or neck patients.
Direct costs
The cost of all medical examinations and treatment (direct costs) during the 2-year study period amounted to only 6.9% of total costs. Although no direct cost comparisons are possible for a similar time period, health-care consumption for this type of patient seems quite similar in various countries [4, 15]. Other studies have also noted that length of disability is associated with an increased utilization of, e.g., specialist referrals, provider visits, spinal imaging and medication [23]. One apparent difference between this Swedish cohort and several other countries was the rate of surgery. In particular, it was five times higher in the USA and three times higher in the Netherlands than in Sweden [15]. In this study, 8% of cohort members underwent back surgery, for which the average cost of one procedure represented 24% of total direct cost, a somewhat higher figure than that estimated in a recent Swedish evidence report (17%)[27]. Almost 25% of direct costs were generated the first month, which seems just as reasonable as the finding that very few medical interventions occurred after 1 year [14]. One exception was that as many as 42% of the first visits to an orthopaedic specialist took place after the first year. This might also explain the relatively high number of magnetic resonance imaging (MRI) or computerized tomography (CT) examinations (frequently initiated by orthopaedic surgeons) during the second year. Effective medical treatment or intervention could reduce the period of sickness absence and, hence, the indirect costs [3]. The very low return-to-work rate, especially during the second year (8 %), indicates that sick-listing, although apparently quite ineffective in returning people to work, was the only “therapy” left during the second year, when all others have been tried [9]. The only medical intervention that the present study found distinctly able to return people to work was disc surgery for those with a lumbar disc herniation, an effect not noted in countries with, e.g., much higher surgical rates [15].
Indirect costs
Indirect costs of a disease are defined as production losses due to morbidity and mortality. In the case of low back and neck pain, production losses are restricted to those caused through absenteeism and disablement. In our study cohort, long-lasting back problems and work absenteeism predominated in low-income people. This finding was recently confirmed in a national report [31], in which the average daily reimbursement for people sick-listed due to back pain was 17% lower than for those sick-listed due to a myocardial infarction. The average reimbursement for those sick-listed for back pain was almost 6% higher than for those sick-listed due to non-specific pain problems. The low average income in our cohort kept production losses relatively low for given lengths of absence. When the human-capital method is used to determine production losses, the unemployment rate in the society is disregarded in the analysis [8]. The Swedish unemployment rate from 1994 to 1997 was around 8%. At such a high rate it can be assumed, at least hypothetically, that an unemployed person would “immediately” be able to replace someone on sick leave. However, if that had been the case, the total level of production would have been unaffected, and there would have been limited production losses. Other methods that take into account the unemployment rate, e.g., the so-called friction cost method, have also been presented in the literature [17, 19, 20]. The friction cost method is suitable when there is an adequate and immediate supply of substitutes with the necessary education and work experience to replace sick-listed employees. Today, unemployment is around 5%; the sick-listing rate is extremely high, especially because of back and neck problems, and frequency of long sick-leave absences has risen especially among persons with longer education. Consequently, it is less realistic to find suitable substitutes easily. Recurrences—known to be frequent in subjects with back and neck problems—were not included in this study; so both direct and indirect costs, if anything, are underestimated [1, 36]. For all participants, except those granted a permanent disability pension, indirect costs were only estimated until the end of the study, i.e., 2 years, when applicable. For those awarded a permanent disability benefit (3.5%) because of health problems, production loss until their mandatory old-age pension was estimated. It is theoretically possible for someone granted a permanent disability benefit to return to work. However, that happens rarely.
Discount factor
Future production losses due to permanent disability benefit could vary considerably, depending on the discount factor used. To make comparisons easier, we chose the 5% discount rate. Table 3 shows how different discount rates affect the costs for production loss due to permanent disability benefits [25].
Non-responders
Postal-questionnaire surveys are known to have low response rates [10]. In spite of vigorous reminding procedures, including telephone calls, only 63% of participants responded to the second questionnaire. That meant that direct costs for 676 people could not be calculated. With complete registry information, indirect costs for all 1,822 could be determined, however. The completeness of registry information made a relatively comprehensive non-response analysis possible. It is reasonable to assume that direct costs for non-responders were relatively similar to those for the rest of the cohort. However, indirect costs for non-responders were lower because of their shorter sick-listing periods. The non-response analysis showed that the relation between direct and indirect costs after 2 years largely corresponded to the relation between these costs for responders.
To reduce costs for long-lasting back and neck problems
Although direct costs were only a small fraction of indirect costs, they could be reduced by better adherence to treatments that have an evidence-based effect [26]. The greatest potential for cost reduction is lowering production losses. Recent, comprehensive evidence reviews confirm the present study’s findings (Fig. 1) that sick-listing in itself as a treatment for long-lasting back or neck problems has questionable and probably counterproductive effects [39, 44]. To minimize sick-listing would, therefore, not only reduce indirect costs but also contribute to faster improvement of pain and function, by helping and supporting patients to return to physical activity that is as normal as possible. This strategy has been shown to be effective for both acute and chronic back problems [18, 24]. Surgery for the relatively few people who have appropriate symptoms of herniated discs improved not only pain and function but also work ability. Consequently, avoidance of unnecessary waiting in those cases would also reduce indirect costs [15].
Total costs and GNP
Our calculated total cost did not include costs for those sick-listed less than 1 month, or those still working but using health services because of back or neck problems. These people most likely consume less health care and definitely generate lower indirect costs than those included in our study. Nonetheless, their high prevalence implies that their costs will add significantly to the total, although how much is uncertain. Based on other assumptions, we suggest that these patient groups stand for one-fourth of the total cost. Added to those sick-listed for longer than 1 month, total costs for all back and neck problems comes to 3.3 billion euros, or 1.3% of GNP. This is lower than was earlier estimated, which is explained mainly by the fact that subjects sick-listed with back and or neck problems have below-average income, something made visible by this study’s bottom-up approach [22, 27].
Conclusion
The total costs for back or neck problems were determined individually and prospectively in a cohort of employed men and women sick-listed 28 days and longer. Direct costs (health-service costs) and indirect costs (production losses) for the group of 1,822 patients followed for 2 years totalled almost 47 million euros. Health-service costs were less than 10% of the total. Nationally, total costs for these patients corresponded to 1% of GNP, while the number who were sick-listed or awarded temporary or permanent disability benefits for these problems corresponded to almost 4% of the entire available workforce.
Acknowledgments
This study was supported by grants from The Medical Faculty, Göteborg University and the Swedish Council for Social Research. We are greatly indebted to Professor Ed Palmer at the Evaluation Department, National Social Insurance Board for his invaluable cooperation, to Associate Professor Robert Jonsson for statistical advice and Professor Alf Nachemson for his great support.
References
- 1.Abenhaim J Occup Med. 1987;29:670. [PubMed] [Google Scholar]
- 2.Bergendorff S, Hansson E, Hansson T et al (1997) Projektbeskrivning & undersökningsgrupp. Rikförsäkringsverket. Sahlgrenska Universitetssjukhuset, Stockholm
- 3.Bigos S (1994) Acute low-back problems in adults. In: Clinical practice guidelines. US Department of Health and Human Services, Rockville, MD, USA
- 4.Bloch F, Prins R (eds) (2000) Who returns to work and why? A six-country study on work incapacity and reintegration. Transaction Publishers, New Brunswick, NJ, USA
- 5.CosteBMJ 19943085778148683 [Google Scholar]
- 6.Coyle D, Richardson G (1994) The cost of back pain. In: Clinical Standards Advisory Group report on back pain. HMSO, London, pp 65–71
- 7.Doorn Acta Orthop Scand Suppl. 1995;263:1. [PubMed] [Google Scholar]
- 8.Drummond M, O’Brien B, Stoddart G et al (1997) Methods for the economic evaluation of health care programmes. Oxford University, Oxford
- 9.Englund L (2000) Sick-listing attitudes and doctors’ practice. Faculty of medicine. Uppsala Universitet, Uppsala
- 10.Eriksson S (1979) Statistisk undersökningsmetodik. Studentlitteraturett förlag inom. Utbildningshuset, Lund, Sweden
- 11.Goossens J Occup Rehabil. 1997;7:15. [Google Scholar]
- 12.Goossens J Clin Epidemiol. 2000;53:688. doi: 10.1016/S0895-4356(99)00177-8. [DOI] [PubMed] [Google Scholar]
- 13.Guo Am J Ind Med. 1995;28:591. doi: 10.1002/ajim.4700280504. [DOI] [PubMed] [Google Scholar]
- 14.Hansson E, Hansson T (1999) Rygg och Nacke 3. Medicinska åtgärder för sjukskrivna med rygg- och nackbesvär. Rfv SU, Stockholm, pp 1–74
- 15.Hansson Spine. 2000;25:3055. doi: 10.1097/00007632-200012010-00013. [DOI] [PubMed] [Google Scholar]
- 16.Henriksson Economic aspects of chronic. 2001;diseases:Multiple. [Google Scholar]
- 17.Hutubessy Pain. 1999;80:201. doi: 10.1016/S0304-3959(98)00204-8. [DOI] [PubMed] [Google Scholar]
- 18.Indahl Spine. 1995;20:473. doi: 10.1097/00007632-199502001-00011. [DOI] [PubMed] [Google Scholar]
- 19.Johannesson J Health Econ. 1997;16:249. doi: 10.1016/S0167-6296(97)00006-4. [DOI] [PubMed] [Google Scholar]
- 20.Koopmanschap J Health Econ. 1995;14:171. doi: 10.1016/0167-6296(94)00044-5. [DOI] [PubMed] [Google Scholar]
- 21.Landstingsförbundet (1995) Kostnad per vårdtillfälle, vårddag, läkarbesök m m 1993. Landstingsförbundet, Stockholm
- 22.Maetzel Best Pract Res Clin Rheumatol. 2002;16:23. doi: 10.1053/berh.2001.0204. [DOI] [PubMed] [Google Scholar]
- 23.Mahmud J Occup Environ Med. 2000;42:1178. doi: 10.1097/00043764-200012000-00012. [DOI] [PubMed] [Google Scholar]
- 24.MalmivaaraN Engl J Med 19953323517823996 [Google Scholar]
- 25.Meltzer Lancet. 2001;358:993. doi: 10.1016/S0140-6736(01)06107-4. [DOI] [PubMed] [Google Scholar]
- 26.Nachemson A, Jonsson E (2000) Neck and back pain. The scientific evidence of causes, diagnosis and treatment. Lippincott, Philadelphia
- 27.Nachemson A, Jonsson E (eds) (2000) Ont i ryggen, ont i nacken. SBU Statens beredning för medicinsk utvärdering, Stockholm, p 417 (vol I), p 389 (vol II)
- 28.Nachemson A, Spitzer W (1987) Scientific approach to the assessment and management of activity-related spinal disorders. A monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Spine [Suppl 1] 12(7S) [PubMed]
- 29.Riksförsäkringsverket RFV Redovisar. 1996;1996:3. [Google Scholar]
- 30.Riksförsäkringsverket (1997) Nybeviljade förtidspensioner/sjukbidrag 1996. RFV Informerar. Statistikinformation Is-I 1997:3. Riksförsäkringsverket, Stockholm
- 31.Riksförsäkringsverket (2002) Vad kostar olika sjukdomar? Sjukpenningkostnaderna fördelade efter sjukskrivningsdiagnos RFV Redovisar 2002:2. Riksförsäkringsverket, Stockholm
- 32.Riksförsäkringsverket (Försäkringskassan i Göteborg) Christer Gustavsson BA (1997) Sjukskrivningsdagar för ryggont i Göteborg 1987 respektive 1992–1996. Göteborgs Universitet, Göteborg
- 33.Rossignol J Occup Med. 1988;30:502. [PubMed] [Google Scholar]
- 34.Skargren Spine. 1998;23:1875. doi: 10.1097/00007632-199809010-00016. [DOI] [PubMed] [Google Scholar]
- 35.Skargren Spine. 1997;22:2167. doi: 10.1097/00007632-199709150-00015. [DOI] [PubMed] [Google Scholar]
- 36.SkovronSpine 1994191298153818 [Google Scholar]
- 37.Socialförsäkringsregisterlag (1997) SFS, Sweden
- 38.Spengler Spine. 1986;11:241. doi: 10.1097/00007632-198604000-00010. [DOI] [PubMed] [Google Scholar]
- 39.Statens beredning för medicinsk utvärdering S (2003) Sjukskrivning—orsaker, konsekvenser och praxis. Stockholm
- 40.Statistiska SOU. 2000;2000:121. [Google Scholar]
- 41.Tulder Pain. 1995;62:233. doi: 10.1016/0304-3959(94)00272-G. [DOI] [PubMed] [Google Scholar]
- 42.Waddell Clin. 1987;Orthop:110. [Google Scholar]
- 43.Waddell Neurosurg Clin N Am. 1991;2:719. [PubMed] [Google Scholar]
- 44.Waddell G, Aylward M, Sawney P (2002) Back pain, incapacity for work and social security benefits: An international literature review and analysis. Royal Society of Medicine, London
- 45.Walker J Spinal Disord. 2000;13:205. doi: 10.1097/00002517-200006000-00003. [DOI] [PubMed] [Google Scholar]
- 46.Weinstein JAMA. 1996;276:1253. [PubMed] [Google Scholar]