Abstract
Sufficient bone decompression of osteophytes is essential for functional long-term outcome in surgery for spondylotic cervical myelopathy. Postoperative CT scans clearly show that decompression is sometimes insufficient. Intraoperative CT scanning has been used to monitor sufficient decompression. Instead of standard intraoperative fluoroscopy, we used an isocentered three-dimensional (3D) flouroscopy with 3D image reconstruction to evaluate the extent of bone decompression. From October 2003 to April 2004, we have used intraoperative 3D fluoroscopy on seven patients with anterior cervical spine surgery due to cervical spondylotic myelopathy. Five patients were operated on in one level, two patients had surgery in two segments. If surgery was performed in two levels or preoperative cinetic MRT showed cervical instability, internal plate fixation was done additionally. All patients were positioned on a radiolucent operating table, made of carbon fibers. Three-dimensional fluoroscopy was always performed before wound closure to evaluate sufficient bone removal. The scanning time was 120 s and the whole procedure from scanning to evaluation is approximately 5 min. In all patients we were able to evaluate the extent of bone decompression. Additionally, placement of cage, plates and screws can be evaluated intraoperatively. In one patient, 3D fluoroscopy showed insufficient decompression, especially on the right side. Further bone removal was performed before the end of the procedure. Intraoperative 3D fluoroscopy is a valuable tool for imaging bone decompression and implant location in anterior cervical spine surgery. The technique is safe, reliable and should help us to avoid incomplete decompression or misplacement of implants and therefore improve long-term functional outcome in cervical spine surgery in the future.
Keywords: Anterior cervical spine surgery, Decompression, Threedimensional fluoroscopy, Intraoperative imaging, CFK equipment
Introduction
Robinson and Smith in 1955 and 1958 [14,17], along with Cloward in 1958 [4], introduced the direct anterior approach to the cervical spine to treat herniated cervical discs and spinal cord compression. Since then, anterior cervical decompression and interbody fusion has probably become the most often performed surgical procedure in cervical spondylotic myelopathy [5]. Various techniques have been described, ranging from discectomy to complete corpectomy with fusion and internal plate fixation [3,12,13,15,16] .
A review of the literature clearly indicates that the extent of bone decompression correlates with outcome [5,13,16]. It may be difficult to determine the extent of bone resection during surgery in the craniocaudal direction, and also on the lateral side. If the surgeon drifts away from the midline, decompression may be excellent at one side, but insufficient at the contralateral side. Postoperative CT scans clearly showed that decompression is sometimes incomplete. Intraoperative CT scanning has been performed to monitor the adequacy of sufficient decompression [8].
We used isocentered three-dimensional (3D) flouroscopy with 3D image reconstruction to evaluate the extent of bone decompression.
Routinely, a lateral X-ray is taken prior to wound closure. Postoperative X-rays with anterior-posterior and lateral view are taken as standard follow-up. The anterior and posterior border of the implant can be seen, but we cannot evaluate the extent of bone decompression. Postoperative CT scans in patients with remaining symptoms show that bone decompression may be incomplete.
Intraoperative imaging is limited to 2D images in most centers. Intraoperative 3D imaging can be done by using an isocentric mobile C arm, like the Iso-C 3D fluoroscopy system (Siremobil Iso-C 3D; Siemens Medical Solutions, Erlangen, Germany). This system allows intraoperative 3D imaging without repositioning of the patient. The Iso-C arm provides multiple flouroscopic images aquired by rotation around an isocentric point. By providing axial plane tomographic images, an accurate 3D volume is reconstructed. Axial, sagittal and coronal planes are rendered, and user-defined axes may be used in different planes. This new technique has been used in spinal surgery to support navigation for screw placement [11,18] and in the beginning was used mostly in foot and ankle surgery [7].
We have used this system since October 2003 in anterior cervical spine surgery for intraoperative evaluation of bone decompression, and placement of cages, plates and screws.
Method and patient selection
Technical equipment
For intraoperative 3D fluoroscopy, we have used the Siremobil Iso-C 3D C-arm (Siemens Medical Solutions, Erlangen, Germany). The system consists of a motorized C-arm with an image intensifier and orbital drive (Fig. 1). For image acquisition, an orbital rotation of 190° in 120 s is performed. During rotation 100 images are aquired in fixed angular steps and subsequently a high resolution 3D data set is reconstructed. Immediately after orbital rotation, a 256 axial-slice DICOM compliant data set is available. The images are displaced in multiplanar reconstruction therafter and user-defined axes can be used to evaluate the intervertebral space and the placement of implants. The rendered 3D image can be shown rotating as film or in single pictures, so the location of the implants are viewed from different angles.
Fig. 1.
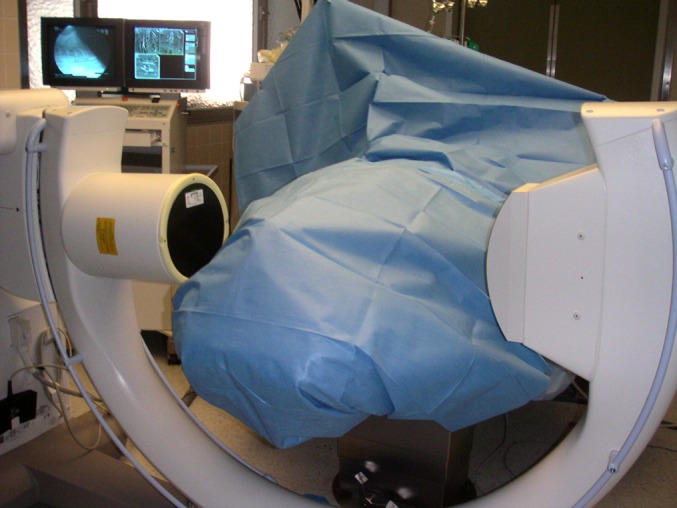
Intraoperative scanning with Iso-C 3D
Patient and treatment characteristics
In a 6-month period, from October 2003 to April 2004, we treated seven patients (four female, three male) with cervical spondylotic myelopathy by an anterior cervical approach.
The median age of the patients was 59 years, ranging from 46 to 81 years.
Five patients were operated on in one segment; two patients had surgery in two segments. Level C5/6 was involved in six and C6/7 in three cases. In two patients, preoperative cinetic functional MRT showed significant instability of the involved segment.
All patients had neurological signs of cervical myelopathy and neuroimaging showed significant bone compression on the cervical myelon. Four patients had radicular signs additionally.
Overall, nine segments were decompressed.
Treatment protocol
A radiolucent operating table made of carbon was used in all patients.
The procedure was performed by an anterior approach to the cervical spine. After excision of the intervertebral disc and resection of the posterior ligament, dorsal osteophytes were removed using the diamond bur with rongeurs and currettes. To ensure sufficient distraction of the intervertebral space, an intervertebral spreader was used. The goal was to achieve maximum decompression without comprising spinal stability. After the surgeon believed that decompression was adequate, the interlaminar spreader was removed and 3D fluoroscopy was performed using the Iso-C 3D after draping the patient (Fig. 1). The reconstructed images were reviewed to evaluate the extent of bone decompression. If bone decompression was incomplete, corrections were done at once.
A rectangular cage made of poly-ether-ether-keton (Cervios, Mathys Medical, Bettlach , Switzerland) was inserted. Internal plate fixation (Mathys Medical, Bettlach, Switzerland) was performed in patients with bisegmental interbody fusion or in patients with monosegmental disease, if preoperative functional MR imaging of the patient showed instability of the cervical spine.
After wound closure, a postoperative X-ray was no longer performed.
Results
At follow-up, 6 weeks postoperatively, signs of myelopathy were improved in all patients. Radicular pain diminished in all patients during postoperative course. There was no additional morbidity or progression of symptoms in any patient treated.
Intraoperative 3D scanning was done successfully in all patients.
Scanning time for the 190° was 120 s and the whole procedure from scanning to evaluation of the pictures never exceeded 5 min. All spinal segments were visualised with good image quality.
The extent of bone decompression could have been evaluated in every segment operated on. Scanning through the axial and sagittal images made sufficient bone removal visible.
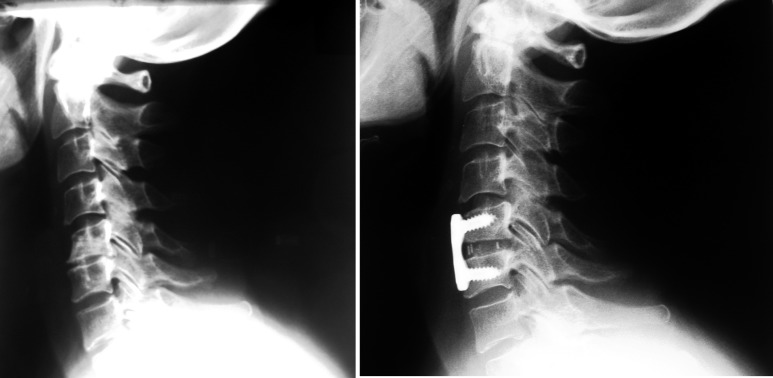
Figure 2 shows a patient with dorsal osteophytes in segment C5/6 and the postoperative film scan with sufficient decompression and the implants in place.
Fig. 2.
Degenerative osteophytes in segment C5/6 and postoperative picture
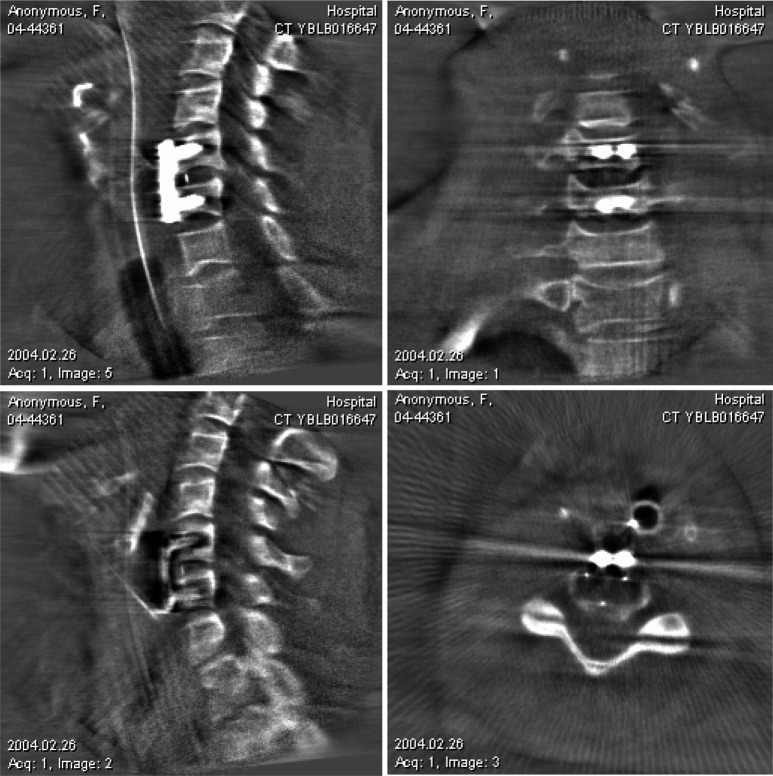
In one patient, intraoperative evaluation of the axial reconstruction clearly demonstrated insufficient removal of the osteophytes on the right side and bone removal was further accomplished before the end of the procedure (Fig. 3).
Fig. 3.
Reconstruction showing incomplete bone removal, especially on the right side
It is often difficult to evaluate adequate bone decompression intraoperatively. We do not have a direct view with the operating microscope of the epidural space, which has to be decompressed. Evaluation of the epidural space with dissectors and nerve hooks is often inadequate and makes the surgeon believe that decompression is complete, although postoperative films clearly show significant osteophytes still in place.
In patients with additional internal plate fixation the location not only of the cage but also of the plate and screws were identified in all segments. There were some minor artefacts, but the quality of the images to evaluate screw positioning was sufficient in any case. Figure 4 shows the position of the cage, plate and screws at the segment C5/6.
Fig. 4.
Intraoperative cage and plate position in segment C 5/6 after adequate decompression
Overall operative strategy was changed in one out of the seven patients treated (14.3%).
The radiation dose associated with this technique is measured continuously. A standard 100-image Iso-C capture is equivalent in radiation to 40 s of standard fluoroscopy. The amount of radiation received by the body ranged between 60 and 110 kV (3–5mA).
Radiation dose for 3D scanning is between 220 and 250cGy per cm2.
In most cases only one Iso-C spin was performed. If decompression was incomplete, an additional scan was taken to proove efficacy of decompression. After wound closure we did not perform routine additional X-rays, neither was postoperative CT scanning necessary in any patient.
Discussion
Since the anterior approach for cervical disc herniation and cervical spondylotic myeolopathy was introduced by Smith and Robinson [14, 17] and Cloward [4] in 1955 and 1958, anterior cervical decompression and interbodyfusion has become probably the most frequently performed surgical procedure for the treatment of rdiculopthy and myelopathy due to disc herniation or spondylosis [5].
The goal of surgery is to achieve a maximum of decompression without comprising the spinal stability.
A critical review of the literature indicates that the extent of osteophyte decompression clearly correlates with outcome [5, 16]. Cooper [5] stated that the adequacy of spinal cord decompression is probably the most important factor in determining outcome.
It may be difficult to determine the extent of bone removal during surgery. The surgeon can drift away from the midline. In this case, decompression may be excellent on one side, but insufficient at the contralateral side.
Standard techniques are used to determine the midline of the spine and identify the longus colli muscles and the uncinate process of the vertebrae. Abe [1] recommended a transverse resection of 14–15 mm. Other surgeons have used various techniques to achieve sufficient decompression. Eleraky [6] stopped resection, when nerve root, epidural fat or 18-mm measurment were seen. They obtained a postoperative CT scan immediately, but did not discuss their results seen on CT. Goto [9] used intraoperative ultrasound for confirmation of adequate decompression. Hejazi and Witzmann [10] used intraoperative cervical epidurography for assessing adequacy of decompression during anterior cervical procedures. In 14 out of 39 patients (36%) epidurography proved that the estimation of surgeons regarding resection completeness was incorrect.
Albert [2] addressed this problem by using a navigation system to monitor the adequacy of corpectomy. Kojima [12] described an anterior trench of 12–15 mm to widen the posterior aspect.
Freidberg et al. [8] used intraoperative CT scanning to evaluate extent of resection, and 17 out of 31 patients required further bone removal before wound closure.
Cooper [5] warned that the surgeon‘s line of sight might prevent adequate removal of bone on the side of the approach. In these cases the implanted cage would be positioned oblique instead of rectangular.
Postoperative CT scans often show inadequate bone removal, but the indication of reoperation is seldom discussed and still controversial.
Intra- and mostly also postoperative imaging for anterior cervical spine surgery has been confined to 2D radiography. Inadequate decompression and also misplacement of implants is seen if a CT scan is aquired because of persistent clinical symptoms or recurrent pain postoperatively.
For our patient series, intraoperative 3D fluoroscopy demonstrated insufficicient bone removal in one out of seven (14.3%) patients with cervical spondylotic myelopathy.
Siremobil Iso-C 3D is the first mobile C-arm with true isocentricity. In comparison with standard C-arms, the central beam always remains in the point of rotation of the C-arm, regardless of the orbital angle. Three-dimensional imaging is made possible with true isocentricity and 190° orbital rotation. The region of interest always remains in the same position, regardless of the actual projection angle, so that a data volume can be generated around an isocenter.
The Iso-C 3D provides an unique ability to aquire and view multiplanar 3D images of intraoperative anatomy and their relationship to implants. Real time feed-back is obtained and the data can be integrated into a conventional navigation system for screw placement [11,18].
The size and handling of the system differ little from that of normal C-arm systems.
In anterior cervical spine surgery the technique can be used to confirm bone resection and cage placement, as well as the location of plate and screws before the end of the operative procedure.
Reviewing the literature and our own results, 3D fluoroscopy, if available, should be used in any patient operated on of spondylotic myeolpathy. Further clinical follow-up of our patients is needed to evaluate the influence of adequate decompression and exact cage placement on long-term outcome. Prospective studies in anterior cervical spine surgery on outcome or comparing different grafts spine should also try to document the extent of bone decompression and standardise cage placement.
Conclusion
Intraoperative 3D fluoroscopy is superior compared with the standard technique for imaging postoperative bony decompression and implants in anterior cervical spine surgery. The system allows quick and accurate data acquisition for intraoperative imaging with or without navigation. Additional radiation dose is minimal and clearly outweighed by complete resection and thus better long-term outcome. The technique is safe, reliable and can be quickly adapted in any operating room and should help us to avoid incomplete decompression or misplacement of implants and therefore improve long-term functional outcome in cervical spine surgery.
References
- 1.Abe H, Tsuru M, Ito T. Anterior decompression for ossification of the posterior longutdinal ligament of the cervical spine. J Neurosurg. 1981;55:108–116. doi: 10.3171/jns.1981.55.1.0108. [DOI] [PubMed] [Google Scholar]
- 2.Albert TJ, Klein GR, Vaccaro AR. Image-guided anterior cervical corpectomy. A feasibility study. Spine. 1999;24:826–830. doi: 10.1097/00007632-199904150-00017. [DOI] [PubMed] [Google Scholar]
- 3.Bohlmann HH. Cervical spondylosis with moderate to severe myelopathy: a report of seventeen cases treated by Robinson anterior cervical discectomy and fusion. Spine. 1977;2:151–162. [Google Scholar]
- 4.Cloward RB. The anterior approach for removal of ruptured cervical discs. J Neurosurg. 1958;15:602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 5.Cooper . Degenerative diseases of the cervical spine. New York: American Association of Neurological Surgeons; 1992. Cervical spondylotic myeolopathy: management with anterior operation; pp. 73–89. [Google Scholar]
- 6.Eleraky MA, Llanos C, Sonntag VK. Cervical corpectomy: report of 185 cases and review of the literature. J Neurosurg Spine. 1999;90:35–41. doi: 10.3171/spi.1999.90.1.0035. [DOI] [PubMed] [Google Scholar]
- 7.Euler E, Wirth S, Pfeifer J, Mutscher W, Hebecker A. 3-D imaging with an isocentric mobile C-arm. Electromedica. 2000;68:122–126. [Google Scholar]
- 8.Freidberg SR, Pfeifer BA, Dempsey PK, Tarlov EC, Dube MA, Day JD, Machado DE. Intraoperative computerized tomography scanning to assess the adequacy of decompression in anterior cervical spine surgery. J Neurosurg Spine. 2001;94:8–11. doi: 10.3171/spi.2001.94.1.0008. [DOI] [PubMed] [Google Scholar]
- 9.Goto S, Mochizuki Kita M Y. Anterior surgery in four consecutive technical phases for cervical spondylotic myelopathy. Spine. 1993;18:1968–1973. doi: 10.1097/00007632-199310001-00008. [DOI] [PubMed] [Google Scholar]
- 10.Hejazi N, Witzmann A, Hassler W. Intraoperative cervical epidurography: a simple modality for assessing the adequacy of decompression during anterior cervical procedures. J Neurosurg Spine. 2003;98:96–99. doi: 10.3171/spi.2003.98.1.0096. [DOI] [PubMed] [Google Scholar]
- 11.Hott JS, Deshmukh VR, Klopfenstein JD, Sonntag VKH, Dickman CA, Spetzler RF, Papadopoulos SM. Intraoperative Iso-C C-arm navigation in craniospinal surgery: The first 60 cases. Neurosurgery. 2004;54:1131–1137. doi: 10.1227/01.neu.0000119755.71141.13. [DOI] [PubMed] [Google Scholar]
- 12.Kojima Waga T S, KuboY Anterior cervical vertebrectomy and interbody fusion for multilevel spondylosis and ossification of the posterior longitudinal ligament. Neurosurgery. 1989;24:864–872. doi: 10.1227/00006123-198906000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Pavlov PW. Anterior decompression for cervical spondylotic myelopathy. Eur Spine J. 2003;12(Suppl 2):S188–S194. doi: 10.1007/s00586-003-0610-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robinson RA, Smith GW. Anterolateral cervical disc removal and interbody fusion for cervical disc sysndrome. Bull John Hopkins Hosp. 1955;96:223–224. [Google Scholar]
- 15.Saunders RL, Bernini PM, Shirreffs TG. Central corpectomy for cervical spondylotic myelopathy: a consecutive series with long term follow-up evaluation. J Neurosurg. 1991;74:163–170. doi: 10.3171/jns.1991.74.2.0163. [DOI] [PubMed] [Google Scholar]
- 16.Seifert V, Stolke D. Multisegmental cervical spondylosis: treatment by spondylectomie, microsurgical decompression and osteosynthesis. Neurosurgery. 1991;29:498–503. [PubMed] [Google Scholar]
- 17.Smith GW, Robinson RA. The treatment of certain cervical spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40:607–624. [PubMed] [Google Scholar]
- 18.Wang MY, Kim KA, Liu CY, Kim P, Apuzzo Reliability of three-dimensional flouroscopy for detecting pedicle screw violations in the thoracic and lumbar spine. Neurosurgery. 2004;54:1138–1143. doi: 10.1227/01.neu.0000119330.70023.8f. [DOI] [PubMed] [Google Scholar]