Abstract
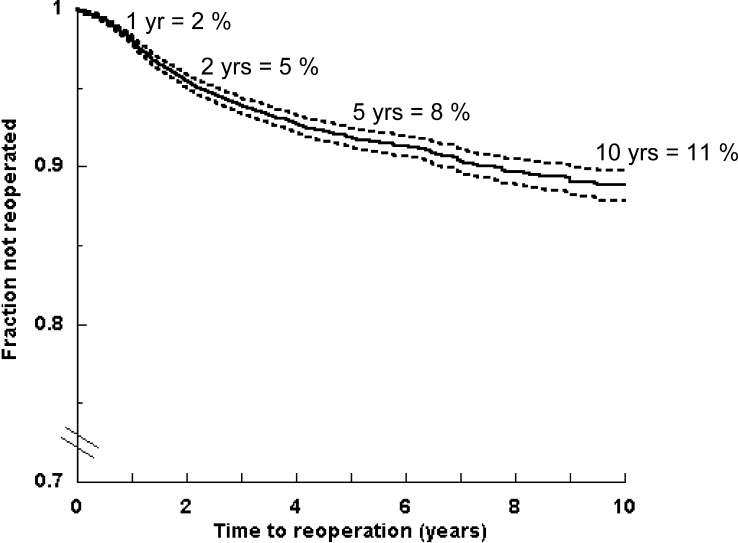
Re-operation rates in spinal stenosis surgery vary between 5 and 23%. Most previous studies have been based on selected patients groups. We analysed the 10-year lumbar spinal stenosis re-operation rate from comprehensive Swedish national data during 1987–1999. The mean length of stay decreased from 2 weeks in 1987 to 1 week in 1999. Of 9,664 patients, 628 (6.5%) were re-operated. Within 30 days after the first spinal stenosis operation, 0.15% of the parients were re-operated. The 1-, 2-, 5-, and 10-year re-operation rates were 2, 5, 8 and 11%, respectively. The rate lowered by 31% over time. Adding a fusion may lower the re-operation risk, an observation which can only be evaluated in randomised trial.
Keywords: Spinal Stenosis, Surgery, Re-operation, Epidemiology, Length of stay
Introduction
Lumbar spinal stenosis is a common cause of low-back pain, radiating pain in the legs, decreased walking ability, and disability [16, 23, 27].
Studies comparing conservative and surgical treatment are rare, and few of them report long-term results. Most studies favor operative over non-operative treatment [1, 2, 15].
National data of the incidence of spinal stenosis, the subsequent development of symptoms, characteristics of the patients, and mortality have been reported [8, 14].
The rates of re-operation after decompressive spinal stenosis surgery vary from 5 to 23% [5, 12, 13, 18]. Most previous studies of the re-operation rate of spinal stenosis surgery have been based on selected patient groups, either from different regions, hospitals, or patients belonging to certain healthcare insurance programs. National longitudinal data of the re-operation rate have rarely been reported [14].
The aim of the current study is to report the 10-year lumbar spinal stenosis re-operation rate, based on comprehensive national data from Sweden during the years 1987–1999.
Materials and methods
Patients
We used the same selection criteria as in a previous study [14]. Briefly, all patients discharged from hospital care from the year 1987 through to December 1999 and operated on for spinal stenosis were retrieved from the National Inpatient Registry by procedure codes. Since these procedure codes were applicable for several conditions, only patients having a primary diagnosis of thoracic or lumbar spinal stenosis were included. We further categorised these discharges according to the complexity of the procedure. Fusion surgery with or without instrumentation was characterised as complex and procedures without fusion surgery as non-complex. This left a study base with 11,283 operations on 10,494 patients.
In order to minimise the risk that the index operation was actually a re-operation of an index operation performed before 1987, only operations from January 1, 1989 through to December 31, 1999 were included. This secondary analysis left 9,664 (86%) of the patients who had undergone surgery for spinal stenosis. The risk of a re-operation was calculated, considering age, gender, type of surgery, time period, and length of stay (LOS). The LOS was calculated from the day of admission to the day of discharge, and categorised by quartiles into four different groups 0–3, 4–7, 8–14, and >14 days, respectively. The calendar year of discharge was categorised into three different time periods, 1989–1991, 1992–1995, and 1996–1999.
Data analysis and statistics
Descriptive analyses of patients characteristics, considering age, gender, discharge diagnoses, LOS, and time period was performed.
Absolute risks of re-operation were assessed using the Kaplan–Meier estimator. Cox-regression was performed for the multivariable analysis of time to a first re-operation. The variables included in these models, and their categorisations, are displayed in Table 2. Results are presented as hazard ratios with 95% confidence intervals and likelihood ratio tests for the overall significance for each of the variables included in the model are given. All analyses were performed using the Statistical Analysis (SAS) package system [24].
Table 2.
Lumbar spinal stenosis surgery in Sweden, 1987–1999. The risk of a re-operation as a function of age, gender, type of operation, period, and length of stay (n=628 re-operations in 9,664 patients)
| Hazard ratio | 95% confidence interval | |
|---|---|---|
| Age (years) | ||
| <59 | 1.13 | 0.961–1.319 |
| 60–64 | 0.88 | 0.702–1.103 |
| 65–69 | 0.99 | 0.768–1.284 |
| 70–74 | 1.00 | Ref. |
| 75–79 | 0.75 | 0.557–1.001 |
| >80 | 0.47 | 0.295–0.759 |
| Gender | ||
| Male | 1.00 | Ref. |
| Female | 1.13 | 0.961–1.319 |
| Period | ||
| 1989–1991 | 1.00 | Ref. |
| 1992–1995 | 0.85 | 0.702–1.033 |
| 1995–1999 | 0.69 | 0.537–0.876 |
| Complexity of surgery | ||
| Low (non-fusion) | 1.00 | Ref. |
| High (fusion) | 0.79 | 0.608–1.024 |
| Length of stay | ||
| 0–3 | 1.52 | 1.093–2.104 |
| 4–7 | 1.00 | Ref. |
| 8–14 | 1.03 | 0.859–1.234 |
| >15 | 0.94 | 0.709–1.232 |
Results
The study cohort consisted of 9,664 patients; among these, 628 (6.5%) were re-operated. The patients were followed cumulatively for 40,078 years, with a median 3.76 years (QR1.71–6.24).
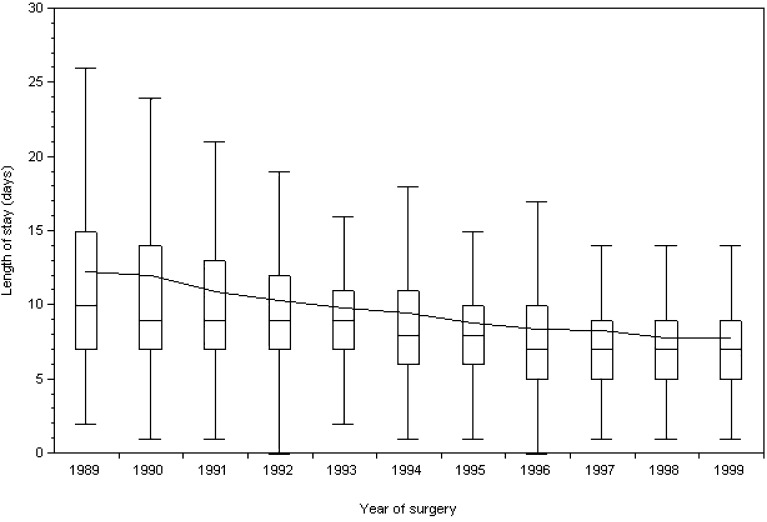
Decompression surgery (laminectomy) was performed in 89% of the patients, and decompression with additional fusion in the remaining 11% (Table 1). The mean age at surgery was 64 years. The mean LOS after spinal stenosis surgery decreased from almost 2 weeks in 1989 to 1 week in 1999 (Fig. 1). Within 30 days after the first spinal stenosis operation, 14 patients (0.15%) were re-operated. The 1-, 2-, 5-, and 10-year re-operation rates were 2, 5, 8, and 11%, respectively (Fig. 2).
Table 1.
Spinal stenosis surgery in Sweden 1987–1999. Patient and re-operation characteristics (n=9,664)
| Number of operations | Number of re-operations | Number of re-operations/person years of follow-up (n) | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Age (years) | |||||
| <49 | 1,219 | 12.6 | 97 | 15.4 | 0.015 |
| 50–54 | 842 | 8.7 | 70 | 11.1 | 0.019 |
| 55–59 | 1,037 | 10.7 | 60 | 9.6 | 0.013 |
| 60–64 | 1,194 | 12.4 | 77 | 12.3 | 0.014 |
| 65–69 | 1,490 | 15.4 | 108 | 17.2 | 0.018 |
| 70–74 | 1,775 | 18.4 | 126 | 20.1 | 0.018 |
| 75–79 | 1,419 | 14.7 | 70 | 11.1 | 0.014 |
| >80 | 688 | 7.1 | 20 | 3.2 | 0.009 |
| Total | 9,664 | 100 | 628 | 100 | 0.016 |
| Gender | |||||
| Male | 4,786 | 49.5 | 302 | 48.1 | 0.015 |
| Female | 4,878 | 50.5 | 326 | 51.9 | 0.016 |
| Type of surgery | |||||
| Laminectomy | 8,676 | 89.2 | 559 | 89.0 | 0.016 |
| Fusiona | 988 | 10.2 | 69 | 11.0 | 0.012 |
| Year of operation | |||||
| 1989–1991 | 1,678 | 17.4 | 182 | 29.0 | 0.015 |
| 1992–1995 | 3,918 | 40.5 | 311 | 49.5 | 0.016 |
| 1996–1999 | 4,068 | 42.1 | 135 | 21.5 | 0.018 |
aWith or without instrumentation and with or without laminectomy
Fig. 1.
Length of stay for spinal stenosis surgery in Sweden 1989–1999. Box plot of age, each box including the central 50% of all length of stay each year. The whiskers show 1.5-times the in-time quartile range. Lines in boxes indicate median values
Fig. 2.
Survival curve after lumbar disc herniation surgery in Sweden 1989–1999. Kaplan–Meier plot showing re-operation over time
The risk of being re-operated was higher among women although not significantly (Table 2). Age brought a decreased risk but only among patients older than 80 years of age. The risk was slightly although not significantly lower after a high complexity operation (fusion with or without instrumentation). The risk of re-operation lowered significantly during each time period, and was 31% lower at the end of the study period.
The risk seemed to vary with the LOS of the index operation. A short stay of less than 3 days brought a higher risk of being re-operated. This risk was only found in the patients who were re-operated on within 30 days.
Discussion
This Swedish national study shows that patients having undergone surgery for spinal stenosis have a risk of being re-operated after 1-, 2-, 5-, and 10-years of 2, 5, 8, and 11%, respectively.
Our study is the largest population-based analysis on repeated spinal stenosis surgery. The study design has the advantage of including all patients discharged after spinal stenosis surgery in Sweden during a period of 13 years. It also enables a complete follow-up of re-operations, even after the patients were discharged from hospital. We based our analysis on a national database, and register studies have several advantages, notably virtually complete coverage and unbiased prospective collection of data.
Re-operation rates for decompressive laminectomy have been reported to vary from 5 to 23% [5, 12, 13, 18]. We found an 11% re-operation rate after 10 years compared with a US study by Katz et al. [18] that presented a 23% re-operation rate 8 years after surgery. This high rate may be due to different indications for surgery or that the operations were performed with other techniques. The patients in the Katz et al. cohort were operated on during 1983–1986, compared with our study period of 1987–1999. During the same period as the study by Katz and co-workers, Caputy and Luessenhop [5] also reported a comparable high re-operation rate of 18% after 5 years. In a cohort from 1991 to 1992, Hanraj et al. [12] found only 5% re-operations after 5 years.
During our study period, the re-operation rate decreased by almost a third. This may be due to several factors. The knowledge about the etiology of spinal stenosis disease has been more or less established, which may have influenced the indications for surgery [20, 25]. Awareness has increased about the different mechanisms behind persistent radicular pain, i.e., neuropathic pain [21, 22]. A third factor is improved diagnostic tools; i.e., CT and also MRI [19]. MRI especially is today a more accurate way to detect and visualise postoperative scar tissues, which in turn has become a more questionable indication for a re-operation [17]. Last but not least in the development of improved standardised operative techniques may have an impact on the re-operation rates [3, 4].
In our study, 11% of the patients had a fusion added to the decompression surgery, and there was a tendency towards a lower risk of being re-operated on if the patient had undergone fusions. This may be compared with a Swedish hospital-based case series of 96 patients operated on for spinal stenosis surgery [6]. A high proportion, 61% had undergone fusion surgery. Among patients with instrumental fusions, 25 patients had undergone a re-operation to remove the osteosynthes material. The indication for removing the hardware was, however, not mentioned, but the clinical outcome in patients who were operated on by fusion and those who were operated but not fused did not differ statistically significantly.
Previous studies have reported that fusion operations have more complications than non-fusion operations [8, 26]. In our study an added fusion seemed to lower the risk of a re-operation. We could not ascertain the reason for fusions in the study, and therefore this finding must be interpreted with caution. A few controlled prospective randomised trials comparing fusion to non-fusion operations have been performed [9–11]. However, long-term analyses of the differences in re-operation rates are still lacking.
There was a tendency for women to have more re-operations. The same has also been noticed for disc herniation surgery [7]. The reasons are not known. The LOS after spinal stenosis surgery decreased from 2 weeks in 1987 to 1 week in 1999. Atraumatic surgery and improved perioperative care, more effective hospital routines, together with a decreased number of hospital beds may explain this.
We defined a re-operation as a new operation for spinal stenosis not considering the exact level of the spinal stenosis. The level of the encroachment in the spinal vertebrae could not be extracted from the inpatient register, which is a limitation in our study. Another limitation in our study is that we could not assume that all operations performed after 1987 were first-time operations. In order to minimise the risk that the assumed first operation was actually a re-operation of a first operation, we did not include the first two years (1987–1989) available in the data base. By doing this, the risk of misclassification of first operations is reduced, because the majority of re-operations appear early (5% in 2 years in our study). Still there could be a few patients who were operated on before 1987, who we actually defined as first time operations during 1989–1999.
Our results of the re-operation rate in the current study are on a group level (all spinal stenosis patients). However, in clinical decision making one has only the individual patient to consider. Thus, results of the reported re-operation rates should be put in the current patient’s perspective with respect to present individual factors.
We have no data of health-related quality of life. Instruments like SF-36 and Euroqol (EQ5D) measure the quality of life. These are, however, now prospectively collected in The Swedish National Register for Lumbar Spine Surgery and will be possible to study in the future [26].
Conclusion
Our Swedish national-based study shows that one out of ten spinal stenosis patients will be re-operated after 10 years. The re-operation rate lowered over time and was almost one-third lower at the end of the study. Adding a fusion may lower the re-operation risk, an observation which can only be evaluated in randomised trial.
Acknowledgements
K.-Å. Jansson was partly funded by the Karolinska Institute and the Karolinska University Hospital. Ethical approval is accepted from the Ethics Committee North at Karolinska Hospital.
References
- 1.Amundsen T, Weber H, Lilleas F. Lumbar spinal stenosis. Clinical and radiologic features. Spine. 1995;20:1178–1186. doi: 10.1097/00007632-199505150-00013. [DOI] [PubMed] [Google Scholar]
- 2.Atlas S, Deyo R, Keller R, et al. The Maine Lumbar Spine Study, Part III. One-year outcomes of surgical and non-surgical management of lumbar spinal stenosis. Spine. 1996;21:1787–1794. doi: 10.1097/00007632-199608010-00012. [DOI] [PubMed] [Google Scholar]
- 3.Benini A. Clinical aspects, pathophysiology and surgical treatment of lumbar spinal stenosis. Schweiz Rundsch Med Prax. 1992;81:395–404. [PubMed] [Google Scholar]
- 4.Benini A, Magerl F. Selective decompression and translaminar articular facet screw fixation for lumbar canal stenosis and disc protrusion. Br J Neurosurg. 1993;7:413–418. doi: 10.3109/02688699309103497. [DOI] [PubMed] [Google Scholar]
- 5.Caputy AJ, Luessenhop AJ. Long-term evaluation of decompressive surgery for degenerative lumbar stenosis. J Neurosurg. 1992;77:669–676. doi: 10.3171/jns.1992.77.5.0669. [DOI] [PubMed] [Google Scholar]
- 6.Cornefjord M, Byröd G, Brisby H, Rydevik BJ (2000) A long-term (4- to 12-year) follow-up study of surgical treatment of lumbar spinal stenosis. Eur Spine 563–570 [DOI] [PMC free article] [PubMed]
- 7.Dedering (2002) An analysis of electromyography, endurance time and subjective factors in patients with lumbar disc herniation and healthy subjects. Thesis/Dissertation, Department of Surgical Sciences, Section of Orthopedics Karolinska Institutet, Stockhom, Sweden
- 8.Deyo R, Cherkin D, Loeser J, Bigos S, Ciol M. Morbidity and mortality in association with operations on the lumbar spine. The influence of age, diagnosis, and procedure. J Bone Joint Surg Am. 1992;74:536–543. [PubMed] [Google Scholar]
- 9.Fischgrund JS, Mackay M, Herkowitz HN, Brower R, Montgomer DM, Kurz LT. 1997 Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospecitive, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal intrumentation. Spine. 1997;22:2807–2812. doi: 10.1097/00007632-199712150-00003. [DOI] [PubMed] [Google Scholar]
- 10.Fox MW, Onofrio, BM, Hanssen AD. Clinical outcomes and radiological instability following decompressive lumbar laminectomy for degenerative spinal stenosis: a comparison of patients undergoing concomitant arthrodesis versus decompression alone. J Neurosurg. 1996;85:793–802. doi: 10.3171/jns.1996.85.5.0793. [DOI] [PubMed] [Google Scholar]
- 11.Grob D, Humke T, Dvorak J. Degenerative lumbar spinal stenosis. Decompression with and without arthrodesis. J Bone Joint Surg Am. 1995;77:1036–1041. doi: 10.2106/00004623-199507000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Hansraj K, Cammisa FP, Jr, O’Leary PF, et al. Decompressive surgery for typical lumbar spinal stenosis. Clin Orthop. 2001;384:10–17. doi: 10.1097/00003086-200103000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Herno A, Airaksinen O, Saari T. Long-term results of surgical tratment of lumbar spinal stenosis. Spine. 1993;18:1471–1474. [PubMed] [Google Scholar]
- 14.Jansson K-Å, Blomqvist P, Granath F, Németh G (2003) Spinal stenosis surgery in Sweden 1987–1999. Eur Spine J 535–541 [DOI] [PMC free article] [PubMed]
- 15.Johnsson K, Uden A, Rosen I. The effect of decompression on the natural course of spinal stenosis. A comparison of surgically treated and untreated patients. Spine. 1991;16:615–619. doi: 10.1097/00007632-199106000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Johnsson K, Uden A, Rosen I. The natural course of lumbar spinal stneosis. Clin Orhop. 1992;279:1982–1986. [PubMed] [Google Scholar]
- 17.Jönsson B, Strömqvist B. Clinical characteristics of recurrent sciatica after lumbar discectomy. Spine. 1996;21:500–505. doi: 10.1097/00007632-199602150-00017. [DOI] [PubMed] [Google Scholar]
- 18.Katz J, Lipson SJ, Chang LC, Levine SA, Fossel AH, Iang MH. Seven- to 10-year outcome of decompressive surgery for degenerative lumbar spinal stenosis. Spine. 1996;21:92–97. doi: 10.1097/00007632-199601010-00022. [DOI] [PubMed] [Google Scholar]
- 19.Kent D, Haynor D, Larson E, et al. Diagnosis of lumbar spinal stenosis in adults. A meta analysis of the accuracy of CT, MR and myelography. AJR Am J Roentgenol. 1992;158:1135–1144. doi: 10.2214/ajr.158.5.1533084. [DOI] [PubMed] [Google Scholar]
- 20.Martinelli T, Wiesel S (1992) Epidemiology of spinal stenosis. Instr Course Lect 179–181 [PubMed]
- 21.Olmarker K, Rydevik B, Norborg C. Autologuos nucleus pulposus inducedes neurophysiological and histological changes in porcine cauda equina nerve roots. Spine. 1994;18:1425–1432. [PubMed] [Google Scholar]
- 22.Rydevik B. Aktuellt om patofysiologi och smärtmekanismer. Nord Med. 1994;109:74–76. [PubMed] [Google Scholar]
- 23.Sanderson PL, Getty CJ. Long term results of patial undercuting facetectomy for lumbar lateral recess stenosis. Spine. 1996;21:1352–1356. doi: 10.1097/00007632-199606010-00015. [DOI] [PubMed] [Google Scholar]
- 24.SAS/STAT software changes and enhancements through release. 6.12. Cary: SAS Institute; 1997. pp. 247–348. [Google Scholar]
- 25.SchönströmNS Bolender NF, Pengler DM. The pathomorphology of spinal stenosis as seen on CT scans of the lumbar spine. Spine. 1985;10:806–811. doi: 10.1097/00007632-198511000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Strömqvist B, Jönsson B, Fritzell P, Hägg O, Larsson B, Lind B. The Swedish National Register for Lumbar Spine Surgery, Swedish Society for Spinal Surgery. Acta Ortop Scand. 2001;72:99–106. doi: 10.1080/000164701317323327. [DOI] [PubMed] [Google Scholar]
- 27.Verbiest H. A radicular syndrome from developmental narrowing of the lumbar vertebral canal. J Bone Joint Surg Br. 1954;36:230–237. doi: 10.1302/0301-620X.36B2.230. [DOI] [PubMed] [Google Scholar]