Abstract
Study Design: Three cases of osteoid osteomas of the spine, adjacent to neural elements, were treated with CT-guided thermal coagulation. Objective: To present an alternative method to conventional treatment of spinal osteoid osteoma. Summary of Background Data: Percutaneous CT-guided radiofrequency coagulation has been succesfully used for osteoid osteoma of the extremities. The conventional management of spinal osteoid osteoma is by surgical resection. Method: Three patients with osteoid osteoma of the spine, adjacent to neural structures, were treated by percutaneous radiofrequency ablation. The procedure was performed in the CT room under general anesthesia and CT guidance. The thermocoagulation electrode was heated at 90°C for 4 min. Results: Two patients left the hospital the same day; the third one was kept 24 h for observation. All of them had total pain relief within 48 h following the procedure. No complications were recorded. There was no evidence of recurrence after a mean follow-up period of 17 months. Conclusion: Osteoid osteoma of the spine, adjacent to neural structures, can effectively and safely be treated by minimally invasive percutaneous CT guided radiofrequency coagulation.
Keywords: Spinal osteoid osteoma, Percutaneous treatment, Radiofrequency coagulation
Introduction
Osteoid osteoma is a benign painful bone tumor usually found in the lower extremities of children and young adults, but it can also occur in the spine In 10% of cases [7, 13]. The largest part of osteoid osteomas of the spine occur in the lumbar area (59%), but the cervical (27%), thoracic (12%), and sacral (2%) spines may as well be involved [9, 10, 17]. They are usually located in the posterior elements of a vertebra, but may also occur in the vertebral body. They rarely involve the spinal canal [12].
Although they bear the criticism of lacking the histologic proof for diagnosis of osteoid osteoma, minimally invasive techniques, such as CT-guided percutaneous radiofrequency thermal ablation and laser photocoagulation have become the methods of choice for the treatment of all localisations except those in contact with neural structures [12, 14], provided that the diagnosis is based on a typical clinical and imaging data. Advanced radionuclide imaging have facilitated the accurate diagnosis of osteoid osteoma, although a negative bone scan does not preclude the diagnosis of this tumor in the presence of a high index of clinical and CT scan suspicion [1, 2, 5, 15].
In a series of 40 consecutive patients of osteoid osteoma treated in our institution by radiofrequency ablation since 1997, four were localized to the spine, three of which were very close to the spinal canal or in direct contact with the nerve roots. In order to categorize them better, we defined the “Neural Spinal Ring”(NSR) as the “container” formed by the inner border of all bony structures that form the spinal canal and lateral recesses, in close contact with the spinal cord and/or the nerve roots: the posterior wall of the vertebral body, the inner and inferior aspects of the pedicles, as well as the inner cortex of the laminae, pars interarticularis and superior facets.
It is the purpose of the present paper to report on the data and results of these osteoid osteomas of the NSR treated by percutaneous thermal ablation.
Case reports
Case 1
A 42-year-old man, presented to our institution for persistent back pain predominating at night. He confirms having this pain for 12 years, and that he is partially relieved by conventional non-steroidal anti-inflammatory drugs (NSAIDs). His physical examination was unremakable. Technetium 99 bone scan with early acquisitions and pinhole magnification on the area of maximum pain did not show any significant uptake. The MRI of the thoracic spine revealed the presence of a well-defined 7 mm round lesion within the vertebral body of the eighth thoracic vertebra (T8), tangential to the posterior wall, separated from the spinal canal by a very thin rim, and containing a central signal, low and intermediate to low on T1 and T2 images, respectively (Fig.1a). On axial CT images of T8, the lesion was lytic, surrounded by a thin sclerotic rim, and containing a 2– 3 mm density (Fig.1b). The overall picture was compatible with the diagnosis of osteoid osteoma of the vertebral body, and surgical treatment was decided. Owing to the particular morbidity of any open surgical approach to this lesion and the difficulty to localize it intraoperatively, it was decided to treat it by percutaneous CT-guided thermal ablation.The procedure was undertaken in the CT room under general anesthesia. The patient was draped in a prone position, and the lesion approached percutaneously under CT guidance following the same technical steps described and used for osteoid osteoma of the limbs (4, 8). After CT verification of the accurate position of the electrode in the center of the nidus, the temperature of its tip was risen to 90°C for 4 min (Fig.1c). The pain disappeared immediately after the procedure. The patient was discharged from the hospital within few hours, and he resumed his daily activities the following day. Two years later, the patient is asymptomatic. The CT Scan shows bony healing of the lesion in contiguity to the electrode tract (Fig.1d).
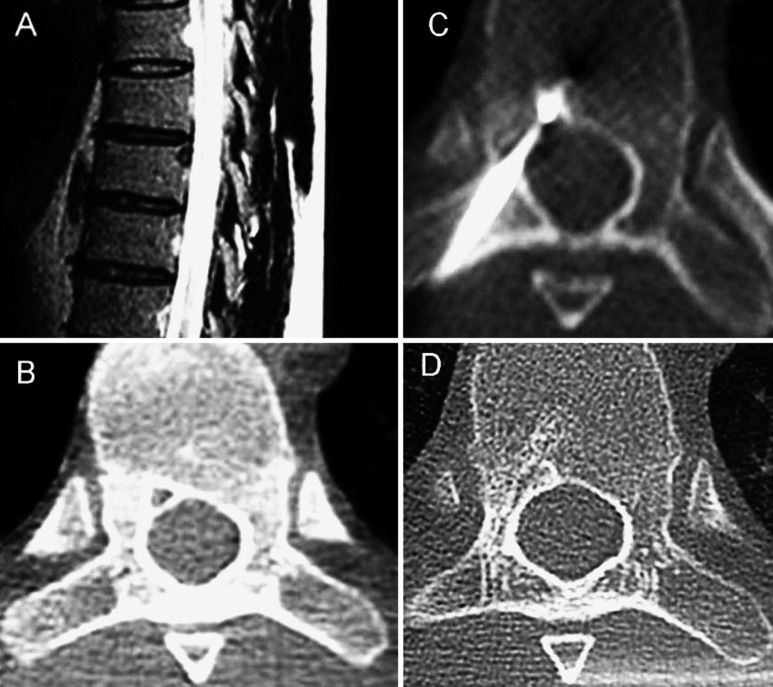
Fig. 1.
A The MRI of the thoracic spine on T2 weighted image sagittal slice, showing a 7-mm low T2 intensity round lesion, located in the neural spinal ring of T8 vertebra. B Axial CT Scan image of T8, showing a small lytic lesion surrounded by a thin sclerotic ring. C Axial CT Scan image of T8, showing the tip of the electrod in the center of the nidus during the percutaneous radiofrequency coagulation procedure. D Axial CT Scan image of T8, 24 months later showing spongious bony healing of the lesion contiguous to the electrode tract
Case 2
A 44-year-old patient presented with a history of neck pain of gradual onset and six months duration. The pain increased at night and responded well to salicylates. His physical examination did not show any abnormality. Radiographs of the cervical spine showed mild degenerative changes. Technetium bone scan with early acquisitions showed increased uptake at the right side of the sixth cervical vertebra (C6). On CT scan and MRI, there was a heterogenous 8-mm lesion of C6’s right superior articular facet just behind the right C7 nerve root. This was interpreted as osteoid osteoma and percutaneous ablation using radiofrequency coagulation was contemplated. Under general anesthesia, the lesion was approached percutaneously in a prone position under CT guidance, through the inferior right facet of C6. Coagulation of its center was performed according to the same principles and following the same steps as previously reported. The pain subsided few hours later and the patient resumed his work the following day. At a follow-up of eight months he is still asymptomatic despite a persistent mild limitation of cervical mobility, possibly due to degenerative changes found on radiographs.
Case 3
A 32-year-old patient complains of low back pain of 18 months duration, predominating at night and partially releived by conventional NSAIDs. His physical examination was unremarkable. Radiographs of the lumbosacral spine were normal. Technetium bone scan with early acquisitions and pinhole magnification showed increased uptake at the right aspect of the posterior arch of the fifth lumbar vertebra (L5). The CT scan revealed the presence of an 8-mm hypodense lesion of L5’s right superior articular facet, surrounded by a thin and irregular dense ring, just behind the right L4 nerve root, compatible with the diagnosis of osteoid osteoma.
Radiofrequency thermal coagulation of this lesion was undertaken using a standard technique, in a prone position under general anesthesia. Recovery was immediate and the patient was discharged the same day. He is still asymptomatic one year later.
Discussion
This paper highlights the possibility to extend the use of percutaneous radiofrequency coagulation to osteoid osteomas of the spine even those adjacent to neural structures.
In an in vitro experiment using the femurs of living dogs, Tillotson et al. [16] showed that thermal coagulation using a radiofrequency generator and a probe causes necrosis in a sphere of tissue approximately 1 cm in diameter, the center of which is the probe’s tip. This method became rapidly one of the first line methods currently used for the treatment of osteoid osteomas of the limbs [6, 12, 14]. Osti and Sebben reported on the first case of lumbar osteoid osteoma of the spine treated successfully by radiofrequency coagulation [11]. Other reports were less enthusiastic about the use of this technique in vertebral osteoid osteomas adjacent to neural elements, because of the potential risk of neurologic complications [3, 8, 12, 14]. In an ex-vivo study measuring temperature changes in the adjacent spinal canal while applying radiofrequency to vertebral bodies in pigs, Dupuy et al. [4] stated that there was no cytotoxic temperature elevations recorded in the spinal canal. They explained this phenomenon by the possibility that local heat decreases because of the presence of a rich epidural venous plexus and the cerebrospinal fluid circulation. They treated successfuly a 1-cm intra spinal osteoid osteoma located at the junction of the T11 right pedicule and lamina, very close to the thecal sac with no complications [4]. Other authors reported in the litterature there experience on a few cases, with a success rate of 50% for spinal lesions. Recurrent or unhealed tumors were surgically treated later on [18].
Conclusion
The current report of three cases of osteoid osteoma of the NSR, adjacent to neural structures and treated successfully by thermal ablation without neurologic complications is encouraging. Larger series are needed to evaluate the long term efficacy off his method and to support it’s use in the management of all osteoid osteomas.
References
- 1.jonboCampanacci M (1999) Osteoid osteoma. In: Bone and soft tissue tumors. Piccin Nuova Libraria, Padova and Springer Verlag, Wien, New York pp391–414
- 2.Campanacci M, Mercuri M, Gasbarrini A, Campanacci L. The value of imaging in the diagnosis and treatment of bone tumors. Eur J Radiol. 1998;27(Suppl 1):S116–22. doi: 10.1016/S0720-048X(98)00052-7. [DOI] [PubMed] [Google Scholar]
- 3.Cove JA, Taminiau AH, Obermann WR, Vanderschueren GM. Osteoid osteoma of the spine treated with percutaneous computed tomography-guided thermocoagulation. Spine. 2000;25:1283–6. doi: 10.1097/00007632-200005150-00014. [DOI] [PubMed] [Google Scholar]
- 4.Dupuy DE, Hong R, Oliver B, Goldberg SN. Radiofrequency ablation of spinal tumors : temperature distribution in the spinal canal. Am J Roentgenol. 2000;175:1263–6. doi: 10.2214/ajr.175.5.1751263. [DOI] [PubMed] [Google Scholar]
- 5.Fehring TK, Green NE. Negative radionuclide scan in osteoid osteoma. A case report. Clin Orthop. 1984;185:245–9. [PubMed] [Google Scholar]
- 6.Ghanem I, Collet LM, Kharrat K, et al. Percutaneous radiofrequency coagulation of osteoid osteoma in children and adolescents. J Pediatr Orthop B. 2003;4:244–52. doi: 10.1097/00009957-200307000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Greenspan A. Benign bone-forming lesions: osteoma, osteoid osteoma, and osteoblastoma. Skeletal Radiol. 1993;22:485–500. doi: 10.1007/BF00209095. [DOI] [PubMed] [Google Scholar]
- 8.Hadjipavlou AG, Lander PH, Marchesi D, Katonis PG, Gaitanis IN. Minimallly invasive surgery for ablation of osteoid osteoma of the spine. Spine. 2003;28:472–7. doi: 10.1097/01.BRS.0000092386.96824.DB. [DOI] [PubMed] [Google Scholar]
- 9.Kroon HMJA. Radiologic aspects of neoplasms and tumor-like lesions of bone. Karstens, The Netherlands, pp. 1994;25(-49):25–49. [Google Scholar]
- 10.Mirra JM, Gold RH, Picci P. Osseous tumors of intramedullary origin. Beckenham, UK: Lea & febiger; 1989. [Google Scholar]
- 11.Osti OL, Sebben R. High-frenquency radio-wave ablation of osteoid osteoma in the lumbar spine. Eur Spine J. 1998;7:422–5. doi: 10.1007/s005860050101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pinto GH, Taminiau AH, Vanderschueren GM, et al. Technical considerations in CT-guided radiofrequency thermal ablation of osteoid osteoma:tricks of the trade. Am J Roentgenol. 2002;179:1633–42. doi: 10.2214/ajr.179.6.1791633. [DOI] [PubMed] [Google Scholar]
- 13.Raskas DS, Graziano GP, Hensinger RN. Osteoid osteoma and osteoblastoma of the spine. J Spinal Disord. 1992;5:204–11. doi: 10.1097/00002517-199206000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Rosenthal DI, Hornicek FJ, Torriani M, et al. Osteoid osteoma:percutaneous treatment with radiofrequency energy. Radiology. 2003;229:171–5. doi: 10.1148/radiol.2291021053. [DOI] [PubMed] [Google Scholar]
- 15.Tanburelli F, Bucca C, Caldarozzo L. Negative results of the scintigraphic examination in osteoid osteoma. Arch Putti Chir Organi. 1989;37:193–8. [PubMed] [Google Scholar]
- 16.Tillotson CI, Rosenberg AE, Rosenthal DI. Controlled thermal injury of bone: report of a percutaneous technique using radiofrequency electrode and generator. Invest Radiol. 1989;24:888–92. doi: 10.1097/00004424-198911000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Unni KK (ed) (2001) Osteoid osteoma. In: Dahlin’s bone tumors. lippincott-Raven, Philadelphia, pp 121–130
- 18.Vanderschueren GM, Taminian AH, Obermann WR, Bloem JL. Osteoid osteoma: clinical results with thermocoagulation. Radiology. 2002;224:82–86. doi: 10.1148/radiol.2241011135. [DOI] [PubMed] [Google Scholar]