Abstract
Background: Infections of the musculoskeletal system are tuberculous in nature in 1–5% of cases. The sacroiliac joint is involved in 3–9.7%. We describe the case of a 32-year-old man with tuberculous sacroiliitis presented as a growing mass on the lateral aspect of his right proximal and mid-thigh. Open biopsy, histology, cultures and PCR established the diagnosis of tuberculosis. Results: After surgical drainage of the abscess, the patient was administrated a triple antibiotic regimen for 12 months. Seven years postoperatively, the patient is disease-free with no functional limitation. This case report highlights the importance of continued awareness for early detection and treatment of a tuberculous sacroiliac joint infection.
Keywords: Skeletal tuberculosis, Abscess, Tuberculous sacroiliitis, Tuberculosis of the greater trochanter
Introduction
Tuberculosis affects worldwide one-third of the population, being the most common infectious cause of death [1]. In contrast, a decreased incidence in the United States is reported [10] after an almost 2 decade interval of increased rates [9]. In urban areas, the incidence of the disease is comparable to that of developing countries, as a result of the high-risk population segregation, and the emergence of drug-resisting bacilli due to the injudicious use of antibiotics and the lack of patient compliance [39].
In the 1950s, because of the optimism succeeding the development of antibiotics, tuberculosis was often overlooked as a cause of musculoskeletal infections [40]. The lack of suspicion and the scant experience of the medical community accounts for the average delay of 17 months between the initial symptoms and the definite diagnosis of skeletal tuberculosis [39, 40].
Infections of the musculoskeletal system are tuberculous in nature in 1–5% of cases [8, 14]. The sacroiliac joint is involved in 3–9.7% [2, 6, 14, 20, 30]. Of note is the fact that the reported incidence of sacroiliac joint tuberculosis is negligible in developing countries [26].
Sacroiliac joint infections represent a diagnostic dilemma for their vague and non-specific clinical presentation [17]. Herein, the authors report a patient with sacroiliac joint tuberculous infection that was undiagnosed for several years, until the infection spread to the greater trochanter and an ipsilateral thigh abscess developed.
Case report
In July 1997, a 32-year-old man, a schoolteacher in a rural area, was admitted to the authors’ institution complaining of right buttock pain and an enlarging mass over the lateral aspect of his right hip and mid-thigh.
His pain originated in 1992 after a fall. At that time, plain radiographs of the pelvis showed no fractures; however, there were extensive erosions at the right sacroiliac joint and faint calcifications at the ipsilateral ischial tuberosity (Fig. 1). Tc99 -bone scintigraphy demonstrated increased radioisotope uptake at the right sacroiliac joint and the ipsilateral greater trochanter (Fig. 2). His local physician attributed the sacroiliac joint lesion to a previous Brucella mellitensis infection and the increased radioisotope uptake at the region of the greater trochanter to his fall. The patient refused any further investigation because his pain was adequately relieved with non-steroid anti-inflammatory drugs.
Fig. 1.

Anteroposterior radiograph of the pelvis in a 27-year-old man, showing erosions of the right sacroiliac joint and demarcation of the cortex of the right ischial tuberosity
Fig. 2.

Bone scintigraphy with 99mTc MDP exhibiting increased radioisotope uptake at the right sacroiliac joint, the right trochanteric area and ischial tuberocity
In December 1996, the patient’s buttock pain had worsened and an enlarging thigh mass emerged. The pain radiated to the ipsilateral calf, especially during climbing stairs and intense walking. The patient had sporadic systemic episodes of low-grade fever and night sweats. Past medical history included positive agglutination tests for brucellosis, for which the patient had received oral tetracyclines. Interestingly, before the definite diagnosis of brucellosis, a 3-week course of intramuscular streptomycin had been administered with improvement of his symptoms. Family history was negative for tuberculosis.
At his admission, the patient was walking with an antalgic gait. Clinical examination revealed a painless mass over the lateral aspect of his right hip and mid-thigh and moderate swelling at the inner thigh and the ipsilateral perineal area. The right sacroiliac joint was tender in deep palpation and stretching maneuvers, including lateral pelvic compression test, Patrick and Gaenslen’s tests. Right hip joint motion was painful at the extremity. Right straight leg raising test was positive at 50°. There were no motor or sensitivity neurologic deficits in the lower extremities.
Plain anteroposterior radiograph of the pelvis showed a sacroiliac joint lesion and significant erosions of the right greater trochanter (Fig. 3). Computed tomography (CT) of the pelvis also showed the right sacroiliac joint erosions, in addition to scattered calcifications and extensive destruction of the ipsilateral greater trochanter and ischium (Fig. 4). Magnetic resonance imaging (MRI) demonstrated a large soft tissue mass at the right mid-thigh, with signal abnormalities suggesting an abscess (Fig. 5). Chest radiographs, and CT and MRI of the lumbar spine were negative.
Fig. 3.

Preoperative anteroposterior radiograph of the pelvis showing destructive lesion of the right trochanter and right ischial tuberosity
Fig. 4.
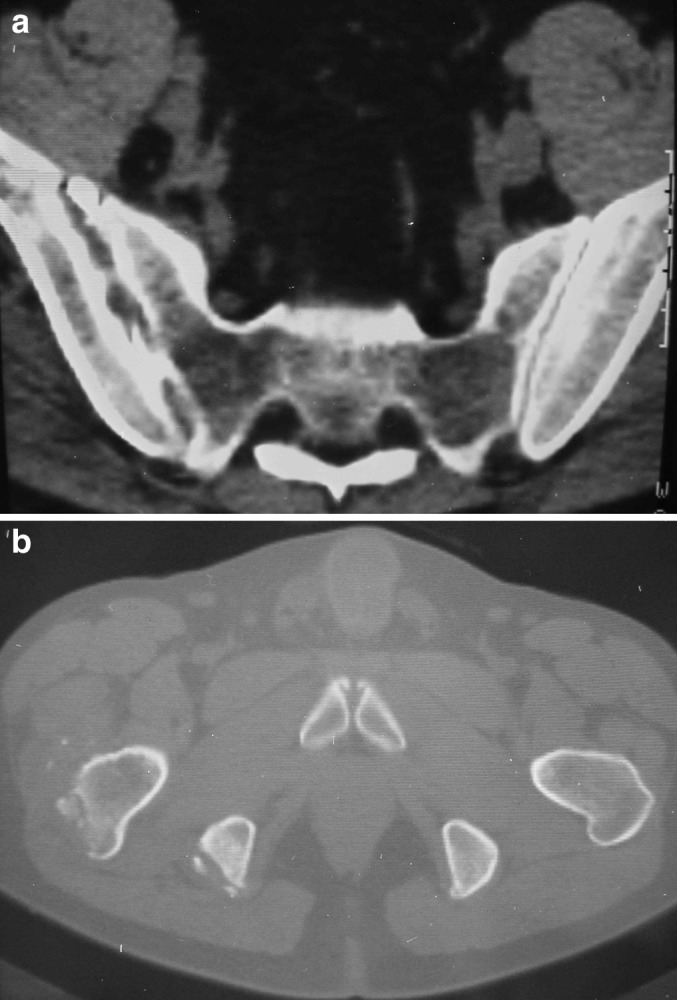
a Axial computer tomography image showing erosions of the articular surface of the right sacroiliac joint. b Axial CT-image depicting destruction at the right trochanter and ischial tuberocity. Soft tissue calcifications are delineated in both sites
Fig. 5.

aCoronal T-2 weighted magnetic resonance image of the pelvis showing a soft tissue mass at the right hip and proximal thigh, associated with destruction and significant edema of the right trochanter. b Axial T-2 weighted magnetic resonance image showing a soft tissue mass of the right proximal thigh
Erythrocyte sedimentation rate (ESR) was 5 mm/h and C-reactive protein (CRP) was 0.9 mg/dl (normal value, <0.5 mg/dl). There was a mild hypochromic and microcytic anemia; hematocrit was 39.5%. Slide agglutination tests with Brucella antiserum were negative. Tuberculin skin test was positive (10 mm); however, the patient had a history of BCG vaccination 10 years previously.
Open biopsy was performed through a lateral approach over the right greater trochanter and extensive debridement was performed. The gross specimen was soft, friable, whitish-gray clumped cheese-like material. Direct smear and stain of the material showed acid-fast bacilli. Histological examination was consistent with a granulomatous infection. Polymerase chain reaction (PCR) showed amplification of the M. tuberculosis genome. Cultures in Löwestein–Jensen culture medium isolated M. tuberculosis, and the diagnosis of tuberculosis was confirmed.
Postoperatively, the patient was administered a triple anti-tuberculous chemotherapy regimen including isoniazid (5 mg/kg body weight), rifampicin (10 mg/kg body weight), and pyrazinamide (35 mg/kg body weight) for 12 months. Within this year, clinical symptoms resolved completely, and MRI showed complete regression of the abscess. Seven years later, the patient is pain-free with no functional limitations. Plain radiograph of the pelvis demonstrates spontaneous ankylosis of the sacroiliac joint (Fig. 6).
Fig. 6.

Postoperative anteroposterior radiograph of the pelvis 5 years after the treatment. The sacroiliac joint is spontaneously ankylosed; there are residual changes of the right trochanter and ischial tuberocity
Discussion
The diagnosis of sacroiliac joint infection is often delayed. In the current patient, the short-term administration of streptomycin masked the clinical presentation of tuberculous sacroiliac joint infection, which has been spread in continuity to the ipsilateral greater trochanter. A delayed diagnosis may also be attributed to the inaccessibility of the sacroiliac joint while the patient is examined in the supine position [17], as well as to the physicians’ failure to perform the sacroiliac joint pain provocation maneuvers [12].
Frequently, mycobacterial infections of the sacroiliac joint may present as a psoas abscess, and may not be diagnosed until spontaneous drainage occurs in the groin [16, 21, 31, 32, 34]. The enlarging thigh abscess was the presenting symptom in the present case, ensuing from pus released after the rupture of the anterior sacroiliac joint capsule.
Buttock pain is invariably present in tuberculous sacroiliitis [11, 15–17, 21, 31, 32, 34, 38]. The sacroiliac pain can be referred to the groin, posterior thigh, and occasionally below the knee, mimicking pain originating from the lumbar spine, the hip and the lower abdominal quadrant [4, 5, 12, 15, 16, 32, 37]. There may be signs of femoral or sciatic nerve root irritation if the distended anterior joint capsule comes in contact with the lumbosacral plexus [3]. In a series, Richter et al. [34] reported that 92% of patients were misdiagnosed and were initially treated for lumbosacral radiculopathy, or underwent useless lumbar spine surgery.
Pain is usually reproduced or aggravated when the sacroiliac joint is mechanically strained during physical examination [23], weight bearing, bending, sitting, or riding [7, 11, 12, 21, 25, 32, 34], and is frequently alleviated by standing or walking. Rarely are these associated neurologic symptoms of weakness, paresthesias, or dysthesias [3, 11]. Tenderness on rectal examination is possible [17, 24]. The trochanteric lesion is usually not associated with local pain [7, 22, 25].
Routine laboratory tests such as elevated ESR and CRP are not significant in the diagnosis of tuberculosis, but are considered useful in the assessment of the response to anti-tuberculous therapy [20]. The ESR of the current patient was significantly lower than normal, suggesting a non-pyogenic infection.
Plain radiographs may not show any abnormality in the early stage of sacroiliac tuberculosis. Haziness or loss of joint line may be an early radiographic finding. Bone scan is helpful for early recognition of the condition [35]. However, CT or MRI are more helpful for early detection of sacroiliac tuberculosis [20, 21]. CT scan shows clearly the extent of joint destruction and MRI delineates the abscess in the soft tissues [20, 21, 24, 32, 38]. MRI may also contribute to the differential diagnosis from a soft tissue tumor or pyogenic arthritis [19].
Tuberculous sacroiliitis should be differentiated from degenerative and post-traumatic arthritis; pyogenic infection of the sacroiliac joint; inflammatory diseases such as sero-negative spondyloarthropathies, ankylosing spondylitis, psoriatic arthritis, Reiter’s and Behçet’s syndromes and inflammatory bowel diseases; connective tissue disorders such as rheumatoid arthritis and systemic lupus erythematosus; familial Mediterranean fever with multisystem involvement including arthritis; osteitis condensans ilii; metabolic conditions such as gout pseudogout and hyperparathyroidism; tumors and tumorlike conditions, and pigmented villonodular synovitis [3, 13, 20, 24, 29, 33].
Pyogenic infection of the sacroiliac joint is usually hematogenously spread from cutaneous sources. Predisposing factors including pregnancy, trauma, endocarditis, intravenous drug use, and immunosuppression are usually discovered. Because blood circulation is sluggish in the ilium, infections in this area may begin as osteomyelitis and then extend into the sacroiliac joint [3]. However, in the present case CT and MRI of the lumbar spine were negative. The multiplicity of the lesions, the rounded sclerotic osteolysis of the greater trochanter and the scattered calcifications in the soft tissue suggested of a low-grade infectious arthritis, such as tuberculosis, brucella or fungal infection [13].
Sacroiliitis occurring early in the course of the disease is usually the hallmark of ankylosing spondylitis [3, 20]. However, a bilateral and symmetric distribution is observed in ankylosing spondylitis, whereas unilateral abnormalities and the absence of additional manifestations from the spine are most typical in infection, as in the present case. Generally, inflammatory and sero-negative arthritis of the sacroiliac joints is usually bilateral. Peripheral joints manifestations and the other stigmata of the diseases including urithritis, uveitis, rashes and bowel dysfunction are usually observed [3, 24, 33].
Osteitis condensans ilii is usually identified on radiographs in young multiparous women following pregnancy. It has been proposed to be the aftermath of ligamentous disruption during pregnancy or parturition. It is a self-limiting condition, rarely leading to chronic sacroiliac joint pain [3]. Metabolic conditions usually affect the sacroiliac joints bilaterally, and are always associated with peripheral manifestations in other joints [3].
Definitive diagnosis is obtained by fine needle aspiration or open biopsy [18, 28]. Acid-fast bacilli in direct smears and stains, the growth of the bacilli in the Löwestein-Jensen culture or the granulomatous lesion identified in the histologic specimen will confirm the diagnosis of tuberculosis. Positive culture results and an antibiogram are highly desirable, because fungal infection and brucellosis often yield similar histologic findings [24, 32]. However, false negative results should be anticipated in long standing tuberculosis, due to the paucibacillary nature of the disease [34].
Before the advent of chemotherapy, sacroiliac joint arthrodesis was considered of value in hastening the end result, which, regardless of the treatment, was the spontaneous ankylosis of the joint [37]. Kim et al. [21] described two options of operative intervention; joint curettage at the early stages of the disease, or curettage combined with arthrodesis when joint instability is anticipated. Operative results are excellent [20, 34] in terms of residual disease and pain relief.
Currently, multiagent anti-tuberculous chemotherapy is used is the treatment of choice for tuberculosis [36, 39]. In the present patient, the authors elected to treat the sacroiliac joint lesion conservatively and to operate directly on the tuberculous abscess to prevent spreading to the hip joint [27]. The patient had an excellent outcome, according to the healing criteria of Kim et al. [21]. Analogous response to either conservative or surgical treatment has also been reported [2, 6, 11, 20, 21, 24, 34, 37, 38]. Recurrences are generally not anticipated [21, 34].
References
- 1.Babhulkar SS. Editorial comment. Clin Orthop. 2002;398:2–3. [Google Scholar]
- 2.Benchakroun M, El Bardouni A, Zaddoug O, Kharmaz M, Lamrani MO, El Yaacoubi M, Hermas M, Wahbi S, Ouazzani N, El Manouar M. Tuberculous sacroiliitis. Four cases. Joint Bone Spine. 2004;71(2):150–153. doi: 10.1016/S1297-319X(03)00153-2. [DOI] [PubMed] [Google Scholar]
- 3.Bernard TN, Jr, Cassidy JD. The sacroiliac joint syndrome. Pathophysiology, diagnosis, and management. In: Frymoyer JW, editor. The adult spine: principles and practice. Philadelphia: Lippincott-Raven; 1997. pp. 2343–2366. [Google Scholar]
- 4.Bernard TN, Jr, Kirkaldy-Willis WH. Recognizing specific characteristics of nonspecific low back pain. Clin Orthop. 1987;217:266–280. [PubMed] [Google Scholar]
- 5.Bonica JJ. The sacroiliac joint syndrome. Pathophysiology, diagnosis, and management. In: Frymoyer JW, editor. Anatomic and physiologic basis of nociception and pain. Philadelphia: Lea & Febinger; 1990. pp. 18–27. [Google Scholar]
- 6.Brasseur P, Koral E, Sukkarieh F, Vanhaeverbeek M, Bissen L. Tuberculous sacroiliitis: report of a case. Rev Med Brux. 2004;25(2):99–102. [PubMed] [Google Scholar]
- 7.Brown NL. Radiologic case study. Tuberculosis of the greater trochanter and its bursa. Orthopedics. 1986;9(9):1276, 1279–1280. doi: 10.3928/0147-7447-19860901-20. [DOI] [PubMed] [Google Scholar]
- 8.Center Morbidity and Mortality Weekly Report. 1981;30:325. [PubMed] [Google Scholar]
- 9.Center Morbidity and Mortality Weekly Report. 1993;42:696. [PubMed] [Google Scholar]
- 10.CenterMorbidity and Mortality Weekly Report 20025110111892953 [Google Scholar]
- 11.Chen WS. Chronic sciatica caused by tuberculous sacroiliitis. A case report. Spine. 1995;20(10):1194–1196. doi: 10.1097/00007632-199505150-00015. [DOI] [PubMed] [Google Scholar]
- 12.Coy JT JT, 3rd, Wolf CR, Brower TD, Winter WG., Jr Pyogenic arthritis of the sacro-iliac joint. Long-term follow-up. J Bone Joint Surg [Am] 1976;58(6):845–849. [PubMed] [Google Scholar]
- 13.Davidson PT, Horowitz I. Skeletal tuberculosis. A review with patient presentations and discussion. Am J Med. 1970;48(1):77–84. doi: 10.1016/0002-9343(70)90101-4. [DOI] [PubMed] [Google Scholar]
- 14.Davies PD, Humphries MJ, Byfield SP, Nunn AJ, Darbyshire JH, Citron KM, Fox W. Bone and joint tuberculosis. A survey of notifications in England and Wales. J Bone Joint Surg [Br] 1984;66(3):326–330. doi: 10.1302/0301-620X.66B3.6427232. [DOI] [PubMed] [Google Scholar]
- 15.Dunn EJ, Bryan DM, Nugent JT, Robinson RA. Pyogenic infections of the sacro-iliac joint. Clin Orthop. 1976;118:113–117. [PubMed] [Google Scholar]
- 16.Feldmann JL, Menkes CJ, Weill B, Delrieu F, Delbarre F. Infectious sacroiliitis Multicenter study of 214 cases. Rev Rhum Mal Osteoartic. 1981;48(1):83–91. [PubMed] [Google Scholar]
- 17.Gordon G, Kabins SA. Pyogenic sacroiliitis. Am J Med. 1980;69(1):50–56. doi: 10.1016/0002-9343(80)90499-4. [DOI] [PubMed] [Google Scholar]
- 18.Hendrix RW, Lin PJ, Kane WJ. Simplified aspiration or injection technique for the sacro-iliac joint. J Bone Joint Surg [Am] 1982;64(8):1249–1252. [PubMed] [Google Scholar]
- 19.Hong SH, Kim SM, Ahn JM, Chung HW, Shin MJ, Kang HS. Tuberculous versus pyogenic arthritis: MR imaging evaluation. Radiology. 2001;218(3):848–853. doi: 10.1148/radiology.218.3.r01fe27848. [DOI] [PubMed] [Google Scholar]
- 20.Keles Tuberculous. 2003;sacroiliitis:a. [Google Scholar]
- 21.Kim NH, Lee HM, Yoo JD, Suh JS. Sacroiliac joint tuberculosis. Classification and treatment. Clin Orthop. 1999;358:215–222. doi: 10.1097/00003086-199901000-00026. [DOI] [PubMed] [Google Scholar]
- 22.King AD, Griffith J, Rushton A, Metreweli C. Tuberculosis of the greater trochanter and the trochanteric bursa. J Rheumatol. 1998;25(2):391–393. [PubMed] [Google Scholar]
- 23.Laslett M, Williams M. The reliability of selected pain provocation tests for sacroiliac joint pathology. Spine. 1994;19(11):1243–1249. doi: 10.1097/00007632-199405310-00009. [DOI] [PubMed] [Google Scholar]
- 24.Ludmerer KM, Kissane JM. Clinicopathologic conference. Severe right hip pain in a 73-year-old woman. Am J Med. 1986;81(1):117–124. doi: 10.1016/0002-9343(86)90192-0. [DOI] [PubMed] [Google Scholar]
- 25.Lynch AF. Tuberculosis of the greater trochanter. A report of eight cases. J Bone Joint Surg [Br] 1982;64(2):185–188. doi: 10.1302/0301-620X.64B2.7068738. [DOI] [PubMed] [Google Scholar]
- 26.Martini M, Ouahes M. Bone and joint tuberculosis: a review of 652 cases. Orthopedics. 1988;11(6):861–866. doi: 10.3928/0147-7447-19880601-04. [DOI] [PubMed] [Google Scholar]
- 27.McNeur JC, Pritchard AE. Tuberculosis of the greater trochanter. J Bone Joint Surg [Br] 1955;37(2):246–251. doi: 10.1302/0301-620X.37B2.246. [DOI] [PubMed] [Google Scholar]
- 28.Miskew DB, Block RA, Witt PF. Aspiration of infected sarco-iliac joints. J Bone Joint Surg [Am] 1979;61(7):1071–1072. [PubMed] [Google Scholar]
- 29.Moujtahid M, Essadki B, Lamine A, Fikry T, Bennouna D, Dkhissi M, Zryouil B. Tuberculous osteitis in limbs. Twenty five case-reports. Rev Rheum Engl Ed. 1996;63(5):344–348. [PubMed] [Google Scholar]
- 30.Nicholson RA. Twenty years of bone and joint tuberculosis in Bradford. A comparison of the disease in the indigenous and Asian populations. J Bone Joint Surg [Br] 1974;56(B(4)):760–765. doi: 10.1302/0301-620X.56B4.760. [DOI] [PubMed] [Google Scholar]
- 31.Papadopoulos ECh, Papagelapoulos PJ, Savvidou OD, Falagas ME, Sapkas GS, Fragkiadakis EG. Tuberculous sacroiliitis. Orthopedics. 2003;26(26(6)):653–657. doi: 10.3928/0147-7447-20030601-18. [DOI] [PubMed] [Google Scholar]
- 32.Pouchot J, Vinceneux P, Barge J, Boussougant Y, Grossin M, Pierre J, Carbon C, Kahn MF, Esdaile JM. Tuberculosis of the sacroiliac joint: clinical features, outcome, and evaluation of closed needle biopsy in 11 consecutive cases. Am J Med. 1988;84(3 Pt 2):622–628. doi: 10.1016/0002-9343(88)90146-5. [DOI] [PubMed] [Google Scholar]
- 33.Resnick D, Niwayama G. Osteomyelitis, septic arthritis, and soft tissue infection: organisms. In: Resnick D, editor. Diagnosis of bone and joint disorders. Philadelphia: Saunders; 1995. pp. 2461–2485. [Google Scholar]
- 34.Richter R, Nubling W, Kobler G, Iljinski A. Tuberculosis of the iliosacral joints. Treatment, results, prognosis and differential diagnosis. Z Orthop Ihre Grenzgeb. 1983;121(5):564–570. doi: 10.1055/s-2008-1053278. [DOI] [PubMed] [Google Scholar]
- 35.Salomon CG, Ali A, Fordham EW. Bone scintigraphy in tuberculous sacroiliitis. Clin Nucl Med. 1986;11(6):407–408. doi: 10.1097/00003072-198606000-00009. [DOI] [PubMed] [Google Scholar]
- 36.Shembekar A, Babhulkar S. Chemotherapy for osteoarticular tuberculosis. Clin Orthop. 2002;398:20–26. doi: 10.1097/00003086-200205000-00004. [DOI] [PubMed] [Google Scholar]
- 37.Soholt ST. Tuberculosis of the sacro-iliac joint. J Bone Joint Surg [Am] 1951;33(1):119–130. [Google Scholar]
- 38.Vaiopoulos G, Sfikakis PP, Velikas E, Kittas C, Kaklamanis P. Tuberculosis of the sacroiliac joint. Eur Spine J. 1997;6(5):330–331. doi: 10.1007/BF01142680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Watts HG, Lifeso RM. Tuberculosis of bones and joints. J Bone Joint Surg [Am] 1996;78(2):288–298. doi: 10.2106/00004623-199602000-00019. [DOI] [PubMed] [Google Scholar]
- 40.Yao DC, Sartoris DJ. Musculoskeletal tuberculosis. Radiol Clin North Am. 1995;33(4):679–689. [PubMed] [Google Scholar]


