Abstract
This case report illustrates three learning points about cervical fractures in ankylosing spondylitis, and it highlights the need to manage these patients with the neck initially stabilised in flexion. We describe a case of cervical pseudoarthrosis that is a rare occurrence after fracture of the cervical spine with ankylosing spondylitis. This went undetected until the development of myelopathic symptoms many months later. The neck was initially stabilised in flexion using tongs, and then slowly extended before anterior and posterior fixation was performed. The myelopathic symptoms resolved, and the patient had a good result at 18 months. We conclude that any increased movement of the spine after trauma in ankylosing spondylitis must be considered suspect and fully investigated.
Keywords: Ankylosing spondylitis, Cervical fracture, Pseudoarthrosis
Introduction
Ankylosing spondylitis (AS) is an inflammatory arthropathy, affecting between one and three per 1000 of the population [17]. The primary effects are stiffness of the spine and sacroiliac joints. In the spine the ligaments and discs become calcified and normal movement is lost, as the spine develops the characteristic flexed posture of spondylitis deformans or Bechterew’s disease, named after the Russian neurologist Vladimir M. Von-Bechterew (1857–1927). It is noted that the neural tissues enclosed within their rigid, bony constraints remain normal.
Fracture of the ankylosed spine is relatively common, with an incidence four times that of spinal fracture in the normal population [4, 27]. Seventy-five percent of these occur in the lower cervical spine[16], but they are described at all spinal levels. Multiple fractures are seen, often with very minor trauma, as the rigid and weakened bones easily fracture, often through the disc space. They are known to be easily missed [11] on initial presentation, especially if there are no neurological symptoms. However, they are often associated with neurological deficits, frequently with fatal complications [6, 19].
Pseudoarthrosis is the term used to describe the appearance of a false joint within the ankylosed spine after a fracture. The developments of these disco-vertebral destructive lesions with bone loss are relatively frequently seen in the thoracolumbar spine[21], but they are rare in the cervical spine[9]. The term pseudo-pseudoarthrosis has been proposed to describe abnormal motion between two ankylosed spinal segments resulting in extensive disco-vertebral destruction without fracture[12].
Case report
A 36-year-old man with a 20 year history of AS presented with the inability to rise from a chair. Each time he tried to do so, he collapsed due to lower-limb weakness. Over the previous 5 weeks, he had been experiencing increasing, although intermittent, symptoms including: sharp pains in the posterior aspect of his neck with head movement, abdominal pain and paraesthesia with numbness of his fingers and toes.
He gave further history of a fall down a flight of stairs, involving two complete backward rolls, some 30 months previously. When picked up from his fallen position he had “self-assessed” himself to be uninjured, as he had no pain, weakness or numbness. However, he did notice that when walking he was able to achieve a more horizontal gaze than usual and that in the car he was able to place his head against the head rest for the first time in years
Examination of upper limb motor function revealed Medical Research Council (MRC) grade 3 power in the hands, and grade 4 in the rest of the upper limbs symmetrically. Reflexes were pathologically brisk and symmetrical with normal sensation to light touch and pin prick. All roots of the lumbosacral plexus had grade 3 power, with hyperreflexia, hypertonia and up-going plantars symmetrically. Patchy areas of sensory loss were noted over both anterior thighs. Anal tone was normal, although perineal sensation was decreased, and he had a palpable bladder which drained 500 ml of residual urine on catheterisation.
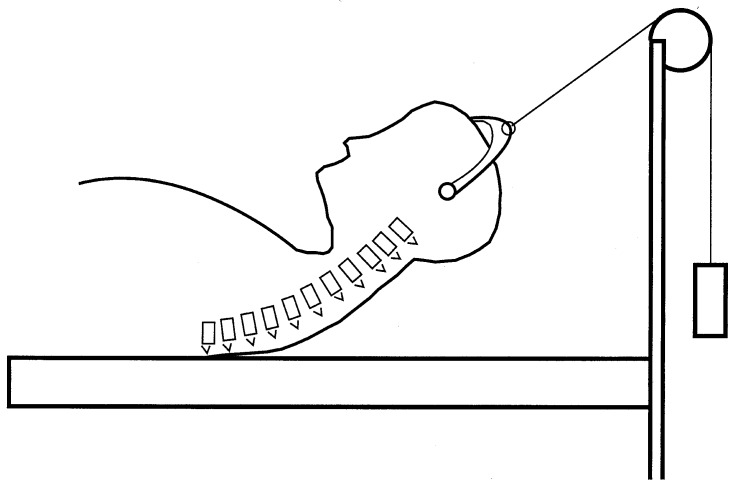
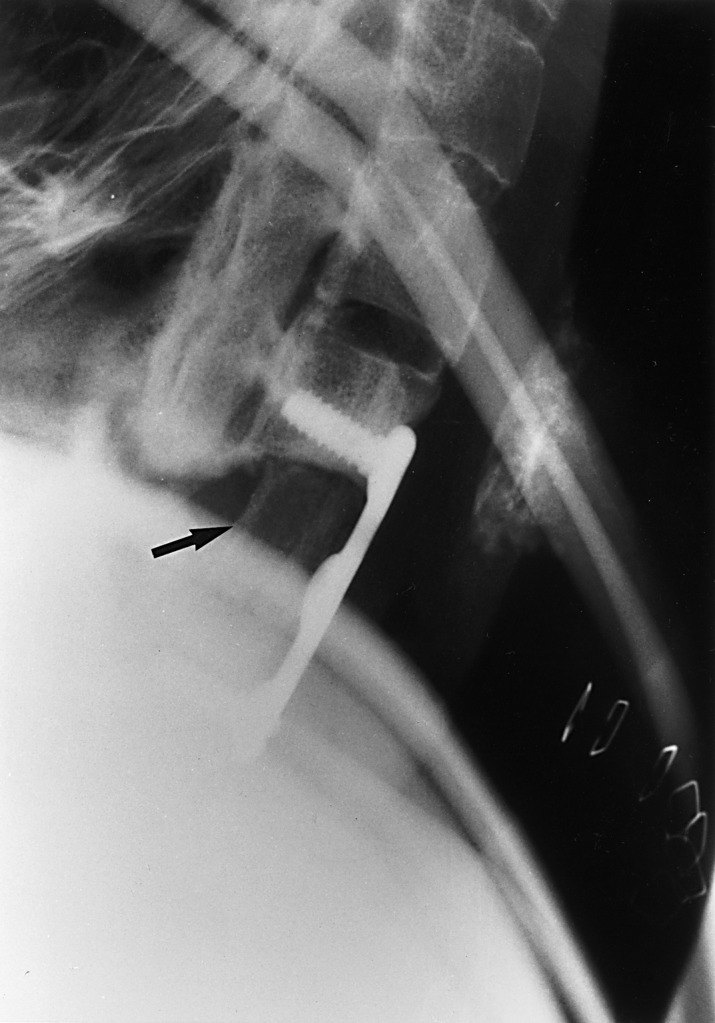
The patient’s lateral cervical spine radiograph (Fig. 1) showed an ankylosed spine, with fusion across all the facet joints. There was a destructive, cystic lesion in the body of C7, with erosion of the posterior aspects of the bony arch. The cervical spine was articulating on a pseudoarthrosis formed from the lateral masses, with an abnormal extension of approximately 45°. Gardener-Wells tongs with 2 k of traction were applied with the pulley positioned to give the applied force in line with his normally flexed cervical spine (Fig. 2), and he was treated with intravenous methylprednisolone.
Fig. 1.

Lateral radiograph of the cervical spine showing pseudoarthrosis with destruction of the body of C7
Fig. 2.
Diagrammatic representation of traction applied with the cervical spine in flexion
There was a dramatic improvement over the next 24 h with this immobilisation and steroid therapy, regaining grade 4 power in all four limbs, with a decrease in his sensory abnormalities. Magnetic resonance imaging (Fig. 3) showed widespread changes of AS, with squaring-off of all vertebral bodies and loss of disc-space height. The body of C7 was replaced by fluid attenuation surrounded by a rim, with the spinal cord relatively normal. His neck was serially and progressively extended in small increments over the next 2 weeks, whilst maintaining axial traction. A lateral, cervical spine radiograph confirmed that a normal alignment had been obtained, but the body of C7 was still absent. After 2 weeks all motor function had improved to 4-plus, with normal sensory and autonomic function.
Fig. 3.

Mid-sagittal MRI scan of the cervical spine showing fluid attenuation in the cyst replacing the body of C7
In the operating theatre, whilst maintaining the exact head position that had been obtained with traction, the cervical spine was exposed through an anterior approach. The body of C7 was found to have been replaced with a cyst, lined by fibrous tissue and containing altered blood. The sclerotic bone around the margins was prepared with a high speed burr and a tri-cortical bone graft, harvested from the iliac crest, tightly introduced forming a press-fit. An AO cervical plate was applied using four screws, two each into the bodies of C6 and T1 (Fig. 4). The fixation was felt to be solid and the neck immobilised in a Philadelphia collar post-operatively. Two weeks later (due to logistical difficulties), a posterior approach was made to the lower cervical spine, the intention being to augment the anterior fixation with posterior stabilisation if required. However, the lower cervical spine was found to be sufficiently rigid to consider further fixation unnecessary, so the levels C6 to T1 were fused using bone graft alone. Again, the neck was immobilised using a Philadelphia collar for a further 10 weeks.
Fig. 4.
Lateral radiograph of the cervical spine showing the plate, with screw fixation into the body of C6, and the block of bone graft (arrow)
Post-operatively there was no deterioration in the patient’s neurological state, and his general condition and mobility slowly improved over the coming weeks, with physiotherapy and hydrotherapy. At 3 months he had normal upper limb function. Although the symmetrical lower limb weakness remained, he could walk unaided. At 4 months, the weakness persisted although it had improved, and plain X-ray showed consolidation of the patient’s bone graft into a solid fusion. He felt that his head position was generally improved and that he had a better line of sight! He remains well 18 months after his surgery.
Discussion
Pseudoarthrosis of the cervical spine in AS is rare, with two other cases described in the literature[9], and none reported in the Fang’s [10] series of 40 cases in 1988. These disco-vertebral destructive lesions were described by Anderson in 1937 [5], and classified by Cawley et al. in 1972 [7]. Imaging is difficult, as they may be confused with malignancy, infection or necrosis [2]. They commonly present with localised pain that is worse on exercise and resolves with rest [7], or with neurological complications from spinal stenosis.
The pathogenesis of the lesion has been questioned, as to whether it has a mechanical or inflammatory origin [23]. However, Wu et al. [26], from a dissection study, concludes that the pathological observations strongly implicate mechanical trauma as initiating and perpetuating pseudoarthrosis. Certainly significant trauma to a rigid and osteoporotic spine will cause fracture, and then the effect of instability at the fracture site (the fused spinal segments can be thought of as a long bone) will produce a pseudoarthrosis. An alternative view is that inflammatory changes from the intervertebral disc may progress towards the posterior arch and induce microtrauma stress fractures, thus generating the pseudoarthrosis [9]. This may also account for the lesions seen without trauma.
The management of spinal fractures in AS is controversial, with good results reported from operative and non-operative means. The current trend with cervical fractures seems to favour fixation, be it anterior, posterior or combined, with collars or halo-vests for aftercare[14, 24, 25]. Local expertise and familiarity will probably dictate the outcome. However, the treatment of pseudoarthrosis is generally agreed to be surgical [9, 14], as the instability that is generated needs to be addressed. A longer fixation is generally desired on these osteoporotic bones, as mobility is not a key consideration.
Anterior cervical fusion with screw-plate fixation, although originally a treatment for degenerative disc disease, has now been well-proven in the treatment of fractures. The need for additional posterior stabilisation is debatable. The anterior technique provides a greater surface area for bony fusion and is also considered safer when transferring patients with cervical fractures. Several clinical series have reported excellent results from anterior plating alone after cervical fractures [1, 13]. The stability achieved is so good that even distraction-flexion injuries [15] or rotationally unstable fractures [18] have also been treated in this way.
It must be appreciated that the overall management of patients with fixed cervical kyphosis is different from that of normal patients having undergone blunt trauma. The usual “safe practice” of holding the neck in extension may worsen the presenting condition. A patient’s neurological condition may be made worse by extension of the neck, as the spinal cord may be compromised by the angle that is formed between the upper and lower rigid bony segments of the cervical spine. The development of paraesthesia [22] and death [20] are reported. Damage to the spinal cord with extension of the neck has also resulted from stabilising the cervical spine in those with rheumatoid arthritis [17] and also in children [8].
This case illustrates three learning points:
Any injury in AS allowing greater movement (even if seemingly desirable) is to be taken seriously, for it probably represents spinal fracture and needs to be investigated and treated as such.
The initial immobilisation and nursing needs to be done with the neck in the normal, flexed position, with consideration for the spinal cord and any swelling that might develop.
A gradual extension of the neck over time can obtain an improved position for the head, which can then be maintained with surgical fixation of the fracture.
References
- 1.Aebi M, Zuber K, Marchesi D (1991) Treatment of cervical spine injuries with anterior plating. Indications, techniques and results. Spine 16 [Suppl 3]:38–45 [DOI] [PubMed]
- 2.Albertsen Acta Radiol. 1996;37:98. doi: 10.1177/02841851960371P119. [DOI] [PubMed] [Google Scholar]
- 3.Althoff Ann Rheum Dis. 1980;39:485. doi: 10.1136/ard.39.5.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Amamilo Orthop Rev. 1989;18:339. [PubMed] [Google Scholar]
- 5.Andersson Nord Med Tidskv. 1939;14:2000. [Google Scholar]
- 6.Broom Spine. 1988;13:763. doi: 10.1097/00007632-198807000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Cawley Ann Rheum Dis. 1972;31:345. doi: 10.1136/ard.31.5.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Curran J Trauma. 1995;39:729. doi: 10.1097/00005373-199510000-00022. [DOI] [PubMed] [Google Scholar]
- 9.Deburge Spine. 1996;21:2801. doi: 10.1097/00007632-199612010-00017. [DOI] [PubMed] [Google Scholar]
- 10.Fang J Bone Joint Surg Br. 1988;70:443. doi: 10.1302/0301-620X.70B3.3372569. [DOI] [PubMed] [Google Scholar]
- 11.Finkelstein Spinal Cord. 1999;37:444. doi: 10.1038/sj.sc.3100837. [DOI] [PubMed] [Google Scholar]
- 12.FurstJ Rheumatol 1990172582319527 [Google Scholar]
- 13.Goffin J Spinal Disord. 1995;8:500. [PubMed] [Google Scholar]
- 14.Graham Spine. 1989;14:803. doi: 10.1097/00007632-198908000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Henriques J Spinal Disord Tech. 2004;17:1. doi: 10.1097/00024720-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Hunter Arthritis Rheum. 1983;26:751. doi: 10.1002/art.1780260608. [DOI] [PubMed] [Google Scholar]
- 17.Lawrence Br J Clin Pract. 1963;17:699. [PubMed] [Google Scholar]
- 18.Lifeso Spine. 2000;25:2028. doi: 10.1097/00007632-200008150-00005. [DOI] [PubMed] [Google Scholar]
- 19.Murray Am J Med. 1981;70:1033. doi: 10.1016/0002-9343(81)90860-3. [DOI] [PubMed] [Google Scholar]
- 20.Papadopoulos BMJ. 1999;319:171. doi: 10.1136/bmj.319.7203.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pettersson Br J Rheumatol. 1996;35:1319. doi: 10.1093/rheumatology/35.12.1319. [DOI] [PubMed] [Google Scholar]
- 22.Podolsky Ann Emerg Med. 1983;12:578. doi: 10.1016/s0196-0644(83)80305-9. [DOI] [PubMed] [Google Scholar]
- 23.Rasker Scand J Rheumatol. 1995;25:52. doi: 10.3109/03009749609082669. [DOI] [PubMed] [Google Scholar]
- 24.Taggard Spine. 2000;25:2035. doi: 10.1097/00007632-200008150-00006. [DOI] [PubMed] [Google Scholar]
- 25.Vaverka Rozhl Chir. 2001;80:5. [PubMed] [Google Scholar]
- 26.WuClin Orthop 19882301543365888 [Google Scholar]
- 27.Young Paraplegia. 1977;15:133. doi: 10.1038/sc.1977.19. [DOI] [PubMed] [Google Scholar]