Abstract
Bone bruising associated with long bone injury is a defined entity with known radiological, pathologic and clinical features. Vertebral bone bruise (VBB) has been described through magnetic resonance imaging (MRI) of the injured spine, but to date the consequences of this entity are unknown. The objective of this retrospective study was to describe the plain radiographic outcome of MRI-defined VBB associated with thoracic and lumbar spine fracture in adults, and to assess whether VBBs caused abnormalities of the bone–implant interface at instrumented levels. Levels of VBB were identified through analysis of the full spine MRI in a consecutive series of adult patients admitted to a spinal injuries unit for thoracic and lumbar spine fractures. The anterior wedge angles (AWAs) of thoracic and lumbar vertebrae demonstrating VBB were measured on radiographs taken at time of injury and at follow-up. Abnormalities of the bone–implant interface were recorded at instrumented levels associated with VBB on follow-up radiographs. Thirty VBBs were identified in 18 adult patients who had suffered 21 vertebral fractures. At an average follow-up of 19 months (range, 12–30 months), the mean AWAs of the VBB vertebrae at the time of injury and at the most recent follow-up were 3.5° and 3.8°, respectively (p=0.33, paired t-test). A total of 12 out of 30 (40%) bruised levels were instrumented in 13 out of 18 (72%) operated patients. No bone–implant interface failure was observed at these levels. It is concluded that VBB associated with thoracic and lumbar vertebral fracture in adult patients does not appear to cause significant progressive vertebral deformity or bone–implant interface failure.
Keywords: Bone bruise, Trabecular microfracture, Spinal injury, MRI
Introduction
Bone bruises, also known as trabecular microfractures, are defined on magnetic resonance imaging (MRI) as band-like or diffuse zones of high signal intensity on T2-weighted sequences and decreased signal intensity on T1-weighted sequences, without associated fracture of the cortex [2]. In the knee, the most frequent mechanism of generation of bone bruises is an axial compression load. Signs of subchondral damage resolve on MRI within 2–4 months from injury, but their long-term effect on joint function is not clear [11]. Bone bruises affecting the vertebral bodies can be associated with spinal injury [5]. However, to our knowledge, the plain radiographic sequelae of vertebral bone bruises (VBB) have not been described yet.
Histological analysis of bone bruises identified in the knee has shown that microfractures occur in the cancellous bone [13]. Trabecular microfractures have also been observed at autopsy in 67% of thoracic spine specimens retrieved after blunt trauma fatalities [16]. In theory, similar findings in spinal trauma patients could render a vertebral body liable to deformity and compromise the fixation if a bone-bruised vertebra were instrumented.
MRI of the injured spine offers the benefit of examining all potentially traumatised structures, namely the vertebrae, the intervertebral disc, the ligaments and the neural tissue [14, 17]. This helps in determining the management of these patients and, if chosen, the appropriate method of surgical stabilisation [12, 14, 17]. All patients admitted to our spinal injuries unit undergo full spine MRI, enabling us to identify those who have sustained VBB in addition to their thoracic or lumbar fractures.
This study was designed to establish the plain radiographic outcome of bone-bruised vertebrae in terms of segmental deformity, by comparing the anterior wedge angle (AWA), [4, 8] at injury and follow-up, in adult patients who have sustained thoracic and/or lumbar spine fractures. Secondly, we wished to assess if the presence of bone bruise compromised the use of surgical instrumentation within affected vertebral levels, by recording any abnormality at the bone–implant interface on follow-up radiographs.
Materials and methods
Cases were obtained from a prospective database of whole spine MRI for patients presenting to a regional spinal injuries unit with a spinal fracture. The total number of patients on this database was 127. The findings on whole spine MRI in this patient group have been published separately. From this study, the overall incidence of VBB was 57% [3]. Inclusion criteria were defined as follows: patients were adults referred to our spinal injuries unit with a thoracic and/or lumbar vertebral fracture, plus one or more vertebral bone bruises identified in the thoracic and/or lumbar spine on a full spine MRI obtained at the time of admission. VBB levels were defined according to the criteria described in the introduction. The sequences used were: sagittal T1-weighted spin echo; sagittal fat-saturated T2-weighted fast spin echo (which highlight bone oedema) and axial T1-weighted spin echo sequences at, above and below the vertebral fracture level [4, 14, 17]. The remainder of the spine was imaged with a sagittal fat-suppressed T2-weighted fast spin echo sequence, in order to identify occult non-contiguous injuries. Patients had to have completed a minimum follow-up of 1 year and undergone plain radiography of both the fractured and bone-bruised levels at the time of injury and latest follow-up.
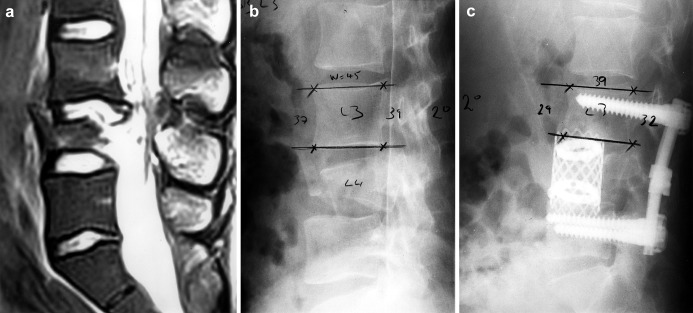
From the database we identified a consecutive series of 18 patients matching these criteria. An orthopaedic trainee, a spinal fellow and a consultant radiologist who had not been involved in the treatment of the patients reviewed the imaging of each patient. We assessed the MRI from the time of injury to identify the appropriate level or levels of bone bruise (Fig. 1a). With a pocket goniometer, we then measured the AWA of the bone-bruised vertebrae on lateral spinal radiographs taken at the time of the injury and erect lateral radiographs from the most recent follow-up (Fig. 1b and c).
a.
Fig. 1 a Sagittal fat-suppressed T1 W fast spin echo MRI showing vertebral bone bruise at L3, associated with an A3 (burst) fracture at L4 (Patient No. 17). b Lateral radiograph at time of injury showing an AWA of 2° at level of bone bruise. c Lateral radiograph at 30 months follow-up showing an AWA of 2° at level of bone bruise. No detectable bone–implant interface abnormality
Measurements of AWA were made independently by two observers and interobserver reliability assessed using the kappa statistic. A paired Student’s t-test was performed to compare the mean AWA at the time of injury with that of the most recent follow-up. The sagittal index (SI-ratio of posterior vertebral body height to anterior vertebral body height) was also calculated for each of the bone-bruised vertebrae at presentation and at final follow-up. The difference in mean SI at time of injury and at time of follow-up was assessed using a paired Student’s t-test. Finally, we analysed the outcome of the instrumentation. Failure of the bone–implant interface was defined as the presence of screw or hook change of position (back-out, dislodgement) or any bone abnormality (radiolucency, fracture) around the instrumentation on follow-up radiographs (Fig. 1a–c).
Results
Eighteen patients who had been admitted consecutively to our spinal injuries unit for thoracic and lumbar spine fractures over a period of 3 years (from 1998 to 2000) matched the inclusion criteria of the study. These patients, 15 men and three women, were aged 38 years on average (range, 19–75). The mean interval from the time of injury to the most recent follow-up was 19 months (range, 12–30 months). None of these patients was lost to follow-up.
Table 1 displays the number, type and levels of vertebral fractures and vertebral bone bruises (VBBs) in the corresponding patients. Patients had sustained a total of 21 fractures of the thoracic and lumbar spine, associated with 30 bone-bruised vertebrae overall. Therefore, 30 of 285 non-fractured thoracic and lumbar vertebrae displayed VBB, giving a frequency of 10.5%. According to the comprehensive classification [9], A3 fracture types (burst fractures) were most common, being observed in 15 out of 21 cases (12 patients). While fractures prevailed at L1 (seven out of 21 levels), VBBs were equally predominant at T9, T10 and T12 (four per each level) but were distributed throughout the entire thoracic and lumbar spine, with the exception of T3, T7 and L5. A single VBB was observed in most of the patients (seven out of 18), two in five patients, three in two patients and four in one patient only.
Table 1.
Patient details (VBB vertebral bone bruise)
| Patient No. | Gender | Age | Follow-up (months) | Fracture type [8] | Fracture levels (n=21) | VBBs (n=30) |
|---|---|---|---|---|---|---|
| 1 | Male | 26 | 12 | B3 | T8 | T1 |
| 2 | Male | 51 | 21 | B2 | T4 | T2 |
| 3 | Female | 70 | 19 | B2 | T8 | T4 |
| 4 | Male | 24 | 20 | A3 | T7 | T4, T5 |
| 5 | Male | 48 | 17 | A3 | T7, T8 | T6 |
| 6 | Male | 38 | 16 | A3 | T7 | T8 |
| 7 | Male | 21 | 19 | B2 | T12 | T10, T11, L1 |
| 8 | Male | 57 | 21 | A3 | T12, L1 | T9, T10, T11 |
| 9 | Female | 24 | 20 | B1 | L1 | T9, T10, T12 |
| 10 | Male | 48 | 17 | A3 | T11 | T9, T10 |
| 11 | Male | 33 | 19 | A3 | L1 | T9, T11, T12 |
| 12 | Male | 35 | 15 | A3 | L1 | T12, L2 |
| 13 | Male | 19 | 21 | A3 | T11 | T12, L1 |
| 14 | Female | 19 | 20 | A3 | L2 | L1 |
| 15 | Male | 19 | 15 | A3 | L1 | L2 |
| 16 | Male | 33 | 17 | A3 | L1, L4 | L3 |
| 17 | Male | 69 | 30 | B3 | L4 | L3 |
| 18 | Male | 75 | 20 | A3 | L1 | L4 |
Table 2 displays the radiological measurements concerning the bone-bruised levels. Interobserver concordance for AWA measurements between observers 1 and 2 for radiographs at presentation was k=0.957 (excellent agreement) and for radiographs at final follow-up was k=0.939 (excellent agreement). The mean AWA of vertebrae associated with VBB at the time of injury was 3.5° (SD, 2.3°; range, 0–7°). At the time of the most recent follow-up, the mean AWA of the same vertebrae was 3.8° (SD, 2.2°; range, 0–7°). The difference (0.3°) for these normally distributed data was not statistically significant (p=0.33 at t-test). Of the 30 VBB levels, eight (27%) showed an increase in AWA from injury to follow-up averaging 2° (range, 1–3°), 15 (50%) showed no change in AWA and seven (33%) showed a negative difference of −1° to −2°. The mean SI at time of injury was 1.105 and at final follow-up was 1.118. This difference was found to be not significant (p=0.59).
Table 2.
Radiographic measurements (observer 1) (VBB vertebral bone bruise, AWA anterior wedge angles)
| VBB No. | Injury AWA | Follow-up AWA | Difference |
|---|---|---|---|
| 1 | 7 | 7 | 0 |
| 2 | 0 | 0 | 0 |
| 3 | 3 | 5 | 2 |
| 4 | 4 | 3 | −1 |
| 5 | 2 | 2 | 0 |
| 6 | 1 | 1 | 0 |
| 7 | 6 | 6 | 0 |
| 8 | 6 | 6 | 0 |
| 9 | 2 | 0 | −2 |
| 10 | 5 | 5 | 0 |
| 11 | 5 | 4 | −1 |
| 12 | 0 | 0 | 0 |
| 13 | 0 | 3 | 3 |
| 14 | 5 | 6 | 1 |
| 15 | 8 | 7 | −1 |
| 16 | 5 | 5 | 0 |
| 17 | 3 | 2 | −1 |
| 18 | 2 | 5 | 3 |
| 19 | 3 | 2 | −1 |
| 20 | 7 | 5 | −2 |
| 21 | 6 | 6 | 0 |
| 22 | 3 | 5 | 2 |
| 23 | 0 | 0 | 0 |
| 24 | 2 | 3 | 1 |
| 25 | 3 | 5 | 2 |
| 26 | 3 | 3 | 0 |
| 27 | 5 | 5 | 0 |
| 28 | 4 | 4 | 0 |
| 29 | 0 | 2 | 2 |
| 30 | 6 | 6 | 0 |
Of the 18 patients studied, 13 (72%) underwent surgical stabilisation, all with pedicle screws. In addition, four patients had anterior reconstruction with a titanium cage. Of these 13 patients, nine (69%) had instrumentation placed into a bone-bruised level. In total, 12 of the 30 (40%) assessed bruised vertebrae were instrumented. On follow-up radiographs, a Steffee plate was noted to have fractured in a 21-year-old male patient, 12 months after he had sustained a B2 (flexion-distraction) fracture of T12. This fracture had been treated by posterior instrumentation via placement of pedicle screws at T10, T11 and L1. On the MRI scan taken on admission to hospital, all of these levels were noted to have been affected by VBB, but on follow-up radiographs none of the implanted screws showed signs of change of position, nor was any radiolucency detected around the screws.
On examination of the follow-up spine radiographs of all the patients, we detected no evidence of failure of the bone–implant interface according to the above-described criteria.
Discussion
Bone-bruise following trauma has been well described in MRI studies of the knee [11] and ankle [6]. The radiological outcome of bone bruise is that the abnormality resolves within 2–4 months [1, 11], with a good clinical outcome, provided no other articular structures have been injured [18]. We aimed to investigate the effects of bone bruises on the bony spine, although we suffered the limitations typical of any retrospective study. In particular, in our public health-based institution we could not obtain funding to perform follow-up MRI scans, which might have helped to define a time frame for the evolution of bone bruises in the vertebral marrow, as it has been the case for the knee [11, 18].
In the present study, a minimum follow-up of 12 months was thought to be sufficient for the consequences of VBB to reach a steady state, based on the above-reported findings in long bone trauma. At the final follow-up, 27% of bone-bruised vertebrae did show a 2° increase and 33% a 1–2° decrease in the average AWA from injury to follow-up, but the mean difference of +0.3° in AWA from injury to follow-up was not significant at t-test. It is, therefore, likely that the positive and negative differences in AWAs from injury to follow-up fall within the accuracy range of radiographic measurement described in the Materials and methods section above.
Patients were all skeletally mature with a broad age range, ranging from young adults to elderly individuals. It was not possible to speculate on the effects of age and correlated morbidities on wedging of the bruised levels, because bone mineral density is not routinely studied in patients admitted for spinal trauma. Also, the effect of bone bruise on the immature vertebra remains to be investigated.
Post-traumatic kyphosis, the main parameter correlating with the clinical outcome of thoracic and lumbar fractures in both conservatively and surgically treated patients, is a multifactorial event depending on degree of vertebral body comminution, posterior ligament complex injury [12] and possibly disc injury [14]. Because this study aimed to define the segmental radiographic outcome of vertebral bone bruise, we avoided investigating any variation in the sagittal plane deformity of our patients from injury to follow-up.
As all patients treated within our unit are tertiary referrals, the majority of patients in this series were surgically stabilised, having sustained predominantly type A3 (burst) fractures, along with a number of type B1 and B2 (flexion-distraction) and type B3 (hyperextension-shear) fractures [9]. Surgery was performed by anterior, posterior or combined approaches, depending on the severity of the injury and the structures involved [10]. A single implant failure occurred in the above-described patient, who suffered a type-B2 fracture of T12 and was treated by posterior instrumentation via insertion of pedicle screws at three adjacent bone-bruised levels and interconnecting plates. One of the Steffee plates fractured, but the pedicle screws remained intact. Such a failure mode has been described by the designers of the implant [15], and we believe it is not attributable to the instrumentation of bone-bruised vertebrae.
On examination of the follow-up radiographs of all patients, there was no evidence of screw or hook back-out or dislodgement, nor of radiolucency or fracture around the instrumentation. Thus, at follow-up, no bone-implant failure appeared to have occurred at instrumented bruised levels. We believe the absence of a follow-up computed tomography (CT) scan did not limit the accuracy of this analysis, as CT does not seem to provide higher accuracy than plain radiographs in detecting abnormalities of the bone–implant interface in spinal trauma patients [7].
Conclusions
Based on the results of this study, we suggest that bone bruises within a thoracic or lumbar vertebral body in adult patients do not cause significant vertebral wedging and so are not, in isolation, a risk factor for post-traumatic deformity. We also feel that bone bruises do not compromise placement of instrumentation within affected vertebrae. Therefore, the benign outcome of bone bruise in the vertebral body seems to replicate the outcome described in long bones, despite the peculiar anatomic and biomechanical features of the bony spine.
Acknowledgement
We thank Marco Brayda-Bruno MD, Senior Consultant, Spinal Deformity Unit, Galeazzi Orthopaedic Institute, Via Galeazzi 4, 20161, Milan, Italy, for his advice regarding this manuscript
Footnotes
An erratum to this article can be found at http://dx.doi.org/10.1007/s00586-006-1076-x
References
- 1.Crotty Clin Orthop. 1996;330:288. doi: 10.1097/00003086-199609000-00037. [DOI] [PubMed] [Google Scholar]
- 2.Eustace Clin Radiol. 2001;56:4. doi: 10.1053/crad.2000.0585. [DOI] [PubMed] [Google Scholar]
- 3.Green RAR, Saifuddin A (2004) Whole spine MRI in the assessment of acute vertebral body trauma. Skeletal Radiol 33; 129–135 [DOI] [PubMed]
- 4.Hedlund Bone Miner. 1988;5:59. doi: 10.1016/0169-6009(88)90006-2. [DOI] [PubMed] [Google Scholar]
- 5.Kulkarni Radiology. 1987;164:837. doi: 10.1148/radiology.164.3.3615885. [DOI] [PubMed] [Google Scholar]
- 6.Labovitz Foot Ankle Int. 1998;19:661. doi: 10.1177/107110079801901003. [DOI] [PubMed] [Google Scholar]
- 7.Larsen J Spinal Disord. 1996;9:117. [PubMed] [Google Scholar]
- 8.Leferink Eur Spine J. 2001;10:517. doi: 10.1007/s005860100319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Magerl Eur Spine J. 1994;3:184. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 10.McCormack Spine. 1994;19:1741. doi: 10.1097/00007632-199408000-00014. [DOI] [PubMed] [Google Scholar]
- 11.MillerAm J Sports Med 199826159474396 [Google Scholar]
- 12.Oner Spine. 2002;27:629. doi: 10.1097/00007632-200203150-00012. [DOI] [PubMed] [Google Scholar]
- 13.Rangger Acta Orthop Scand. 1998;69:291. doi: 10.3109/17453679809000933. [DOI] [PubMed] [Google Scholar]
- 14.Saifuddin Skeletal Radiol. 2001;30:237. doi: 10.1007/s002560100354. [DOI] [PubMed] [Google Scholar]
- 15.SteffeeClin Orthop 1986203453955996 [Google Scholar]
- 16.Taylor J Bone Joint Surg Br. 2001;83:S84. doi: 10.1302/0301-620X.83B2.11419. [DOI] [PubMed] [Google Scholar]
- 17.Tracy Spine. 1989;14:292. doi: 10.1097/00007632-198903000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Wright Am J Sports Med. 2000;28:663. doi: 10.1177/03635465000280050701. [DOI] [PubMed] [Google Scholar]