Abstract
Forty-nine patients with low-back pain referred for flexion-extension radiographs due to suspicion of lumbar instability were studied to examine the relationship between the clinical presentation and the presence of radiographic instability of the lumbar spine. Patients had a mean age of 39.2 (±11.3) years, with a mean Oswestry score of 20.4% (±13.3). The median duration of symptoms was 78 days. All patients underwent both a radiographic and clinical examination. The reliability of the radiographic variables was high, while the reliability of clinical variables ranged from moderate to good. Twenty-eight patients (57%) had radiographic instability based on published norms. Clinical variables related to the presence of radiographic instability were age, lumbar flexion range of motion, total extension range of motion, the Beighton scale for general ligamentous laxity, and segmental intervertebral motion testing. The presence of at least 53° of lumbar flexion or a lack of hypomobility with intervertebral motion testing resulted in a positive likelihood ratio of 4.3 (95% CI: 1.8, 10.6), for predicting radiographic instability. The results of this study indicate that various factors from the clinical examination are useful for predicting radiographic instability. If the findings of this study can be replicated, these clinical factors could be used to inform treatment decision-making without a sole reliance on radiographic assessment.
Keywords: Low-back pain, Instability, Diagnosis, Radiographic assessment
Introduction
Despite technological advances, the identification of a specific structural cause remains elusive in the majority of individuals with low-back pain (LBP) [1]. Notwithstanding the lack of success to date, the pursuit of relevant subgroups of individuals with LBP remains a research priority [6, 7, 9, 12]. Lumbar spine instability has been considered by many to represent an important subgroup of those experiencing LBP [23, 43]. Numerous definitions and perspectives on lumbar instability have been proffered [23, 44, 61], yet many questions persist regarding the clinical presentation and diagnosis of the condition.
Specific surgical and non-surgical treatment approaches have been proposed for patients thought to have lumbar instability, and preliminary evidence suggests that individuals with LBP due to instability may preferentially respond to these specific interventions. Lumbar fusion is presumed to be the surgical treatment of choice for individuals with LBP due to instability [52], while non-surgical management has focused on stabilization exercises [27, 29, 43]. Research evidence suggests that patients with instability may respond better to these treatments than alternative approaches [10, 26, 42, 62, 63]. Directing patients towards these specific interventions relies on an accurate method of detecting lumbar instability [19].
Knuttson [32] originally described a method for diagnosing segmental instability using lateral radiographs with the patient performing maximum lumbar flexion and extension. The amount of sagittal plane translation and rotation occurring at individual spinal motion segments are calculated from the radiographs, and comparisons are made with studies defining normal magnitudes of rotational and translational movement [15, 16, 46, 47]. White and Panjabi [61] defined criteria for diagnosing instability from flexion-extension radiographs as sagittal plane translation greater than 4.5 mm or greater than 15% of the vertebral body width, or sagittal plane rotation of greater than 15° at L1/L2, L2/L3 or L3/L4, greater than 20° at L4/L5, or greater than 25° at L5/S1 [61].
Although concerns about the validity of flexion-extension radiographs have been raised [5, 25, 53], this method has become the standard by which lumbar instability is diagnosed [15, 16, 40, 47]. Other proposed “gold standards” for diagnosing instability include intra-operative spinal stiffness measures or external fixation; however, these methods may not be practical for routine use in patients managed non-surgically [2, 8]. Numerous clinical findings are proposed to indicate instability, but the validity of these findings remains largely unreported. History variables suggested to be diagnostic of instability include frequent recurrent episodes of LBP, short-term relief from manipulation, a history of trauma, or improvement of symptoms with a rigid brace or external fixation [20, 37, 55]. Others have recommended palpation for the presence of a “step-off” between adjacent spinous processes, aberrant motions such as an “instability catch” [30, 41], or increased mobility with passive intervertebral motion testing [45]. The purpose of this study was to examine the relationship between clinical findings and a flexion-extension radiographic examination. Specific variables from the history and physical examination were examined for their accuracy in predicting lumbar instability on the radiographic examination.
Materials and methods
Study population
This study examined a prospective cohort of patients referred for flexion-extension radiographs based on suspicion of instability. Inclusion criteria were a chief complaint of LBP with or without radiation into the lower extremities, and less than 60 years of age. Patients were excluded if there was a contraindication to radiographic assessment (e.g., current pregnancy), previous lumbar fusion surgery, or the inability to actively flex and extend the spine adequately to permit an assessment of segmental motion due to pain or muscle spasm. The study protocol was approved by the Institutional Review Board of the University of Pittsburgh and all participants signed an informed consent document.
Experimental protocol
Study participants underwent both a radiologic and clinical examination, performed by separate examiners, who were blinded to the results of the other examination. For 40 patients the examinations were performed on the same day. The other 13 patients had no longer than 2 weeks between examinations.
Radiologic examination
Flexion-extension radiographs of the lumbar spine were taken using previously described methodology [48]. The patient first sat at the edge of a tall stool with feet flat on the floor and arms folded across the chest. The patient was instructed to flex forward as far as possible for the flexion radiograph. For the extension radiograph, the patient stood with arms folded, and was asked to extend as far as possible. Performing flexion in sitting and extension in standing has been found to produce optimum segmental spinal movements and can be measured with high intra- and inter-rater reliability.
Measurements of sagittal plane translation and rotation were made using methods described by White and Panjabi [61]. Sagittal plane rotation for each motion segment was calculated as the difference between the Cobb angle measurements taken in the flexion and extension positions. Sagittal plane translation was assessed for both the flexion and extension radiographs. The magnitude of the translation at each segment was calculated by measuring the displacement of the superior vertebra as a percentage of vertebral body width of the inferior vertebra. This method avoids inaccuracies related to magnification [15]. The criteria of White and Panjabi [61] for determining rotational or translational instability were applied at each motion segment.
All rotation and translation measurements were made directly on the film by one rater, who was blind to the clinical examination results. The intra-rater reliability of the measurements was assessed in the first ten patients. In these patients the rater made measurements of rotation and translation from the patient’s radiographs on one occasion, then repeated the measurements 10–14 days later. The order of the radiographs for the second measurement was randomized, and the patient’s identifying information was masked to minimize the possibility of recall.
Clinical examination
The clinical examination consisted of self-report, history and physical examination variables performed by one physical therapist blind to the radiographic results. Inter-rater reliability of the physical examination was examined in a subset of 38 patients. In these patients, a second physical therapist, blind to the results of the radiographic assessment and the first examination, repeated the examination after approximately 5 min of rest.
Self-report measures included demographic information as well as the Fear Avoidance Beliefs Questionnaire (FABQ) [59] and modified Oswestry disability questionnaire [21]. The FABQ contains two subscales assessing fear-avoidance beliefs about work (seven items), and physical activity (four items). Fear avoidance beliefs have been associated with prolonged disability, work loss, and deconditioning in individuals with LBP [22, 31, 56, 57]. The OSW is a ten-item measure of disability for patients with LBP. The version used in this study was modified from the original [17] by replacing the item on sex life with an item about employment/home-making. Both the original and modified versions have excellent reliability and validity for assessing disability [13, 21, 54].
Historical information obtained included duration and distribution of symptoms, prior history of LBP, and response to previous treatments. The physical examination included the following:
Range of motion (ROM)
Range of motion measures were taken with a single inclinometer using methods described by Waddell et al. [58]. Lumbar, pelvic and total flexion, total extension, side-bending, and straight leg raise (SLR) were assessed. Discrepancies in side-bending and SLR were computed by taking the absolute value of the right-side measurement minus the left-side measurement. The ratio of extension to flexion ROM was computed as well as the ratio of lumbar flexion to total flexion ROM. These variables have been suggested to be indicative of instability [15, 19, 34].
Physical impairment index (PII)
Four ROM tests (total flexion, total extension, average lumbar side-bending, and average straight leg raise), and three other tests (bilateral active straight leg raise, active sit-up, and spinal tenderness) were combined to form the physical impairment index [58]. Each test is scored as impaired (1) or negative (0) based on published cut-off values; resulting in a total impairment score from 0 to 7.
Tests for lumbar instability
Five tests proposed to indicate instability were performed:
Aberrant motion: Any aberrant motions present during flexion-extension ROM were recorded, including an instability catch [42], painful arc of motion, “thigh climbing” (Gower’s sign), or a reversal of lumbopelvic rhythm [14].
Posterior shear test: The test was performed with the patient standing with the hands across the lower abdomen. The examiner placed one arm over the patient’s crossed arms. The heel of the other hand was placed on the patient’s pelvis for stabilization. The examiner produced a posterior shear force through the patient’s abdomen, and an anteriorly-directed stabilizing force with the opposite hand. The test was repeated at each lumbar level. A positive test occurred if familiar symptoms were provoked, and is proposed to indicate lumbar instability [14].
Beighton hypermobility scale: General ligamentous laxity was assessed with the nine-point Beighton scale. One point was given for each of the following: knee hyperextension >10°, elbow hyperextension >10°, fifth finger hyperextension >90°, thumb abduction to contact the forearm, and ability to flex the trunk and place hands flat on the floor with knees extended [3].
Intervertebral motion testing: Intervertebral motion was tested with the patient prone. The examiner contacted the spinous process with the hypothenar eminence and produced a posterior-anterior force. The mobility of each segment was judged as normal, hypermobile, or hypomobile. The presence of pain was recorded as present or absent.
Prone instability test: The prone instability test is performed with the patient prone with the trunk supported on the examining table and feet resting on the floor. With the patient in this position, the examiner performs an intervertebral motion test to each level of the lumbar spine. Any provocation of pain is recorded [38]. The patient then lifts the legs off the floor and the intervertebral motion test is repeated. If pain is present in the resting position but subsides in the second position, the test is positive.
Data analysis
Reliability was assessed for the radiographic and physical examination variables using kappa coefficients for dichotomous variables [11], intraclass correlation coefficients (ICC model 3,1) for radiographic variables, and ICC (2,1) for continuous physical examination variables [50]. Patients were dichotomized based on the presence or absence of radiographic instability. The translation and rotation values of each lumbar segment were compared with published thresholds defining instability [61]. Each segment was graded as normal (no instability), unstable in translation, unstable in rotation, or unstable in rotation and translation. Because studies have reported large variability and high false positive rates with flexion-extension radiographs [5, 16, 25], we required a patient to meet one of the following criteria to be categorized as having instability: (1) two segments with either rotational or translational instability, or (2) one segment with both translational and rotational instability.
Clinical variables were examined for univariate relationships with radiographic instability. Continuous variables were compared using independent samples t-tests and categorical variables with Pearson chi-square tests. A significance level of P<0.05 was used for all tests. Variables with significant univariate relationships were examined further. A cut-off value maximizing the prediction of radiographic instability was established for retained continuous variables by calculating sensitivity, specificity, positive and negative likelihood ratio (LR) values [51] for all possible cut-off points. Because the goal was to predict instability, the cut-off score producing the largest value for the lower bound of the 95% confidence interval (CI) for the positive LR was selected [49]. Sensitivity, specificity, and positive and negative LR values were also calculated for each retained categorical variable. All retained variables were entered into a step-wise logistic regression equation (P=0.05 to enter and 0.10 to remove) to determine the most parsimonious set of predictors for instability. Sensitivity, specificity, positive and negative LR values were calculated at each step of the final regression model. The optimal classification criteria for instability were determined from the set of variables maximizing the positive LR for predicting radiographic instability.
Results
Between December 2001 and October 2002, 53 patients were recruited. Four were excluded because the radiographs were insufficient to permit the determination of stability at all lumbar levels. Mean age of the 49 patients was 39.2 (±11.3) years, 28 (57%) were female, and 41 (84%) reported a prior history of LBP. Further characteristics are outlined in Tables 1, 2.
Table 1.
History and demographic variables
| All subjects (n=49) | Radiographic instability present (n=28) | Radiographic instability absent (n=21) | Significance | |
|---|---|---|---|---|
| Age (years) | 39.2 (11.3) | 35.7 (11.5) | 44.0 (9.3) | 0.01 |
| Gender (% female) | 57.1% | 60.7% | 52.4% | NS |
| Duration of current symptoms (median days) | 78 | 123 | 49 | NS |
| Distribution of symptoms | ||||
| Back/buttock only (%) | 63.3% | 60.7% | 66.7% | NS |
| Symptoms distal to the knee (%) | 30.6% | 32.1% | 28.6% | NS |
| Prior history of LBP (%) | 83.7% | 82.1% | 85.7% | NS |
| LBP Episodes becoming more frequent (%) | 30.6% | 39.3% | 19.0% | NS |
| Percent of those with prior bracing treatment who experienced improvement | 66.7% (n=15) | 42.9% (n=7) | 87.8% (n=8) | NS |
| Percent of those with prior manipulation treatment reporting improvement | 75.7% (n=37) | 75.0% (n=20) | 76.5% (n=17) | NS |
| Percent of those with prior extension exercise treatment reporting improvement | 55.6% (n=18) | 55.6% (n=9) | 55.6% (n=9) | NS |
| Percent of those with prior traction treatment reporting improvement | 50.0% (n=20) | 40% (n=10) | 60% (n=10) | NS |
| Oswestry disability score | 20.4 (13.3) | 18.9 (11.9) | 22.4 (15.1) | NS |
| FABQ work subscale | 12.9 (11.8) | 13.0 (10.6) | 12.8 (13.4) | NS |
| FABQ physical activity subscale | 15.0 (6.5) | 14.3 (5.6) | 15.9 (7.6) | NS |
Values represent mean (standard deviation) unless otherwise indicated
Table 2.
Physical examination variables. Values represent mean (standard deviation) unless otherwise indicated. (Discrepancy values were calculated as the absolute value of the left-side measurement minus the right-side measurement)
| All subjects (n=49) | Radiographic instability present (n=28) | Radiographic instability absent (n=21) | Significance | |
|---|---|---|---|---|
| Total flexion (°) | 101.5 (21.2) | 108.9 (18.7) | 91.6 (20.7) | 0.004 |
| Pelvic flexion (°) | 53.2 (16.5) | 54.2 (18.3) | 51.9 (13.9) | NS |
| Lumbar flexion (°) | 48.2 (13.6) | 54.6 (9.0) | 39.7 (14.3) | <0.001 |
| Percent of total flexion from lumbar spine (%) | 47.6% (12.5) | 51.4% (11.4) | 42.5% (12.3) | 0.012 |
| Total extension (°) | 25.0 (6.8) | 26.7 (7.4) | 22.8 (5.2) | 0.047 |
| Extension to flexion ratio | 0.25 (0.08) | 0.25 (0.08) | 0.26 (0.07) | NS |
| Average side-bending (°) | 34.8 (15.3) | 33.8 (14.1) | 36.3 (16.9) | NS |
| Side-bending discrepancy (°) | 4.3 (5.5) | 5.1 (6.8) | 3.2 (2.7) | NS |
| Average straight leg raise (°) | 85.3 (13.2) | 87.6 (11.9) | 82.2 (14.4) | NS |
| Straight leg raise discrepancy (°) | 3.1 (2.9) | 3.7 (3.2) | 2.4 (2.1) | NS |
| Physical impairment index | 1.1 (1.4) | 0.86 (1.2) | 1.5 (1.6) | NS |
| Aberrant motion during lumbar range of motion (% yes) | 14.3% | 17.9% | 9.5% | NS |
| Beighton scale | 1.5 (1.9) | 1.9 (2.1) | 0.90 (1.4) | 0.048 |
| Posterior shear test (% positive) | 55.1% | 57.1% | 52.4% | NS |
| Prone instability test (% positive) | 53.1% | 60.7% | 42.9% | NS |
| Lack of hypomobility present during intervertebral motion testing (% yes) | 73.5% | 57.1% | 95.2% | 0.003 |
| Any hypermobility present during intervertebral motion testing (% yes) | 34.7% | 46.4% | 19.0% | 0.046 |
| Any pain during intervertebral motion testing (% yes) | 79.6% | 76.2% | 82.1% | NS |
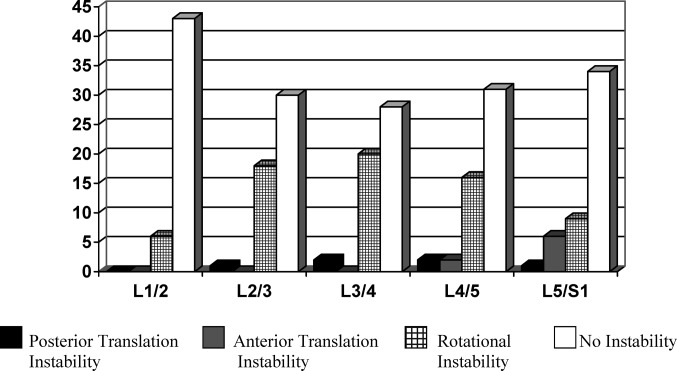
Intraclass correlation coefficients values for radiographic variables ranged from 0.84 to 0.99 for translation measures and 0.81 to 0.96 for rotation measures. Reliability coefficients for physical examination variables are listed in Table 3. The presence of rotational and translational instability at each lumbar level are displayed in Fig. 1. Overall, 28 patients (57%) were classified as having instability.
Table 3.
Reliability coefficients for physical examination variables (n=38 unless otherwise indicated)
| ICC (95% CI) | Percent agreement | Kappa (95% CI) | |
|---|---|---|---|
| Total flexion (°) | 0.91 (0.72, 0.96) | ||
| Pelvic flexion (°) | 0.85 (0.73, 0.92) | ||
| Lumbar flexion (°) | 0.60 (0.33, 0.79) | ||
| Total extension (°) | 0.61 (0.37, 0.78) | ||
| Average side-bending (°) | 0.53 (0.27, 0.72) | ||
| Average straight leg raise (°) | 0.70 (0.42, 0.84) | ||
| Physical Impairment Index (n=35) | 0.75 (0.48, 0.88) | ||
| Beighton scale | 0.72 (0.50, 0.85) | ||
| Aberrant motion during lumbar range of motion | 87% | −0.07 (−0.45, 0.31) | |
| Posterior shear test | 64% | 0.27 (0.14, 0.41) | |
| Prone instability test | 85% | 0.69 (0.59, 0.79) | |
| Hypomobility during intervertebral motion testing | 77% | 0.38 (0.22, 0.54) | |
| Hypermobility during intervertebral motion testing | 77% | 0.48 (0.35, 0.61) | |
| Any pain during intervertebral motion testing | 82% | 0.57 (0.43, 0.71) |
Fig. 1.
Frequency of rotational and/or translational instability at each lumbar segment (n=49)
From the history and demographics, only age showed a significant relationship with instability. Seven variables from the physical examination were significantly different between groups. Three of these variables related to flexion ROM (total flexion ROM, lumbar flexion ROM, and percentage of total flexion from the lumbar spine). Because of the high correlations among these variables, we examined the point-biserial correlations between each flexion variable and the radiographic classification. Lumbar flexion had the highest correlation with the radiographic classification and therefore only this variable was retained for further analysis to avoid multicolinearity. Accuracy statistics for retained variables are given in Table 4. The lack of hypomobility during intervertebral motion testing had the highest positive LR value for predicting radiographic instability.
Table 4.
Accuracy statistics for the variables retained for further analysis
| Variable associated with radiographic instability | Sensitivity | Specificity | Positive LR | Negative LR |
|---|---|---|---|---|
| Age <37 years old | 0.57 (0.39, 0.74) | 0.81 (0.60, 0.92) | 3.0 (1.2, 7.7) | 0.53 (0.33, 0.85) |
| Lumbar flexion >53° | 0.68 (0.49, 0.82) | 0.86 (0.65, 0.94) | 4.8 (1.6, 14.0) | 0.38 (0.21, 0.66) |
| Total extension >26° | 0.50 (0.33, 0.67) | 0.76 (0.55, 0.89) | 2.1 (0.90, 4.9) | 0.66 (0.42, 1.0) |
| Beighton scale >2 | 0.36 (0.21, 0.54) | 0.86 (0.65, 0.94) | 2.5 (0.78, 8.0) | 0.75 (0.54, 1.0) |
| Lack of hypomobility during intervertebral motion testing | 0.43 (0.27, 0.61) | 0.95 (0.77, 0.99) | 9.0 (1.3, 63.9) | 0.60 (0.43, 0.84) |
| Any hypermobility present during intervertebral motion testing | 0.46 (0.30, 0.64) | 0.81 (0.60, 0.92) | 2.4 (0.93, 6.4) | 0.66 (0.44, 0.99) |
The logistic regression model contained two variables; lumbar flexion ROM and lack of hypomobility with intervertebral motion testing. Naglekerke’s R2 for the model was 0.51. If the classification criteria for instability required both findings to be present (i.e., lumbar flexion ROM>53°, and a lack of hypomobility), there were no false positive results (Table 5). The positive LR value associated with this criterion was estimated by adding 0.5 to each cell to avoid division by zero [60]. A value of 12.8 was obtained, although the 95% CI was wide (0.79, 211.6). If the criterion for instability was defined as having either one or two of these findings present, the positive LR was smaller (4.3) but the 95% CI was narrower (1.8, 10.6).
Table 5.
Accuracy statistics for combinations of the two variables (lack of hypomobility during intervertebral motion testing and lumbar flexion ROM>53°) in the logistic regression model
| Sensitivity | Specificity | Positive LR | Negative LR | |
|---|---|---|---|---|
| At least one variable present | 0.82 (0.64, 0.92) | 0.81 (0.60, 0.92) | 4.3 (1.8, 10.6) | 0.22 (0.10, 0.50) |
| Both variables presenta | 0.29 (0.13, 0.46) | 0.98 (0.91, 1.0) | 12.8 (0.79, 211.6) | 0.72 (0.55, 0.94) |
m aNo false positive results were present in this analysis, 0.5 was added to each cell to avoid division by zero error
Discussion
Although numerous examination findings are proposed to be indicative of lumbar segmental instability, few studies have examined the relationship between these findings and stability during flexion-extension radiographic assessment. Our findings support some previously-hypothesized relationships and fail to support others. We found patients with radiographic instability were younger, supporting the theorized etiological sequence of stabilization following a period of instability in patients with LBP [37]. Lumbar flexion ROM measures were also predictive of instability, which is not surprising given previous research demonstrating good correlation between inclinometer and radiographic measurements of lumbar ROM [33]. We found greater ligamentous laxity as measured with the Beighton scale in patients with instability, supporting the proposed relationship between generalized laxity and spinal mobility [35]. The literature does not suggest that individuals with generalized laxity are at greater risk for developing LBP,[24, 33] or to experience greater pain and disability due to an episode of LBP[36]. Several variables, such as aberrant motions or a favorable response to prior immobilization, did not show the expected relationship with instability. Further research is needed to explore if these variables are actually useful for diagnosing instability.
An important finding for predicting instability was lumbar intervertebral motion testing. Patients judged to have hypomobility were unlikely to have instability, while those judged to have hypermobility were more likely to have instability; further supporting the construct validity of intervertebral motion testing. Lundberg and Gerdle [35] found good correlations between segmental assessment of intervertebral motion and sagittal plane lumbar ROM. Flynn et al. [18] found patients with LBP judged to have hypomobility were more likely to respond to a manipulation intervention than those without hypomobility. The findings of the current study suggest that patients with LBP without hypomobility may be more likely to respond to a program of lumbar stabilization exercises; however, this hypothesis requires further research.
Logistic regression retained two variables: lumbar flexion ROM>53°, and a lack of hypomobility with intervertebral mobility testing, explaining about half of the variability in the radiographic classification. We did not obtain oblique or standing neutral radiographs, and were therefore unable to identify a spondylolytic lesion or spondylolesthesis. These abnormalities or other measures of bony morphology of the lumbopelvic region may have explained further variability in the radiographic classification [4, 28]. In addition, differences in the passive properties of soft tissue have been identified in individuals with greater articular mobility[39], but no assessments were made in this study. Our purpose was to examine clinical variables, and therefore these variables were not included in the study.
Likelihood ratios provide the best assessment for diagnostic tests [44]. In this study we focused on the positive LR because it expresses the change in odds favoring the presence of instability given a positive test. The positive LR of 9.0 for a lack of hypomobility with intervertebral motion testing was the best individual test for instability. Based on this LR, if a clinician suspected a patient with LBP of having instability with 50% certainty (roughly the prevalence of instability in this study), a lack of hypomobility would increase the probability of instability to 90%. The best positive LR (12.8) was achieved when both lumbar flexion ROM>53°, and a lack of hypomobility were found. With both present, the probability of instability increases from 50 to 93%. The negative LR of 0.22 is also useful. Among patients who do not have either finding, the probability of having radiographic instability decreases from 50 to 18%. It is important to note that the confidence intervals around these LR statistics were noticeably wide, and therefore replication of these findings is needed.
Conclusions
Certain findings from the history and physical examination were predictive of radiographic instability. The two most predictive factors were lumbar flexion ROM and a lack of hypomobility during lumbar intervertebral motion testing. The presence of both findings increased the probability of instability from 50 to 93%. Further research is needed to determine if patients with LBP who have these findings will respond preferentially to lumbar stabilization exercises or fusion interventions.
Acknowledgements
This work was supported by Central Research Development Grant, University of Pittsburgh
Footnotes
The opinions and assertions contained herein are the private views of the author and are not to be construed as official or as reflecting the views of the Department of the Air Force or the Department of Defense
A comment to this article can be found at http://dx.doi.org/10.1007/s00586-004-0828-8
References
- 1.Abenhaim L, Rossignol M, Gobeille D, Bonvalot Y, Fines P, Scott S. The prognostic consequences in the making of the initial medical diagnosis of work-related back injuries. Spine. 1995;20:791–795. doi: 10.1097/00007632-199504000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Bednar DA. Failure of external spinal skeletal fixation to improve predictability of lumbar arthrodesis. J Bone Joint Surg Am. 2001;83-A:1656–1659. doi: 10.2106/00004623-200111000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Beighton P, Horan F. Orthopedic aspects of Ehlers-Danlos syndrome. J Bone Joint Surg Br. 1969;51:444–453. [PubMed] [Google Scholar]
- 4.Berlemann U, Jeszenszky DJ, Buhler DW, Harms J. Facet joint remodeling in degenerative spondylolisthesis: an investigation of joint orientation and tropism. Eur Spine J. 1998;7:376–380. doi: 10.1007/s005860050093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boden SD, Wiesel SW. Lumbosacral segmental motion in normal individuals. Have we been measuring instability properly? Spine. 1991;15:571–575. doi: 10.1097/00007632-199006000-00026. [DOI] [PubMed] [Google Scholar]
- 6.Borkan JM, Cherkin DC. An agenda for primary care research on low back pain. Spine. 1996;21:2880–2884. doi: 10.1097/00007632-199612150-00019. [DOI] [PubMed] [Google Scholar]
- 7.Borkan JM, Koes B, Reis S, Cherkin DC. A report from the second international forum for primary care research on low back pain: reexamining priorities. Spine. 1998;23:1992–1996. doi: 10.1097/00007632-199809150-00016. [DOI] [PubMed] [Google Scholar]
- 8.Brown MD, Wehman KF, Heiner AD. The clinical usefulness of intraoperative spinal stiffness measurements. Spine. 2002;27:959–961. doi: 10.1097/00007632-200205010-00015. [DOI] [PubMed] [Google Scholar]
- 9.Bouter LM, Tulder MW, Koes BW. Methodologic issues in low back pain research in primary care. Spine. 1998;23:2014–2020. doi: 10.1097/00007632-199809150-00019. [DOI] [PubMed] [Google Scholar]
- 10.Buttermann GR, Garvey TA, Hunt TF, et al. Lumbar fusion results related to diagnosis. Spine. 1998;23:116–127. doi: 10.1097/00007632-199801010-00024. [DOI] [PubMed] [Google Scholar]
- 11.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46. [Google Scholar]
- 12.Coste J, Paolaggi J, Spira A. Classification of non-specific low back pain II. Clinical diversity of organic forms. Spine. 1992;17:1038–1042. doi: 10.1097/00007632-199209000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Davidson M, Keating JL. A comparison of five low back disability questionnaires: reliability and responsiveness. Phys Ther. 2002;82:8–24. doi: 10.1093/ptj/82.1.8. [DOI] [PubMed] [Google Scholar]
- 14.Delitto A, Erhard RE, Bowling RW. A treatment based classification approach to low back syndrome: identifying and staging patients for conservative treatment. Phys Ther. 1995;75:470–489. doi: 10.1093/ptj/75.6.470. [DOI] [PubMed] [Google Scholar]
- 15.Dupuis PR, Yong-Hing K, Kassidy JD, Kirkaldy-Willis WH. Radiographic diagnosis of degenerative lumbar spinal instability. Spine. 1985;10:262–276. doi: 10.1097/00007632-198504000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Dvorak J, Panjabi M, Novotny JE, Chang DG, Grob D. Clinical validation of functional flexion extension roentgenograms of the lumbar spine. Spine. 1991;16:943–950. doi: 10.1097/00007632-199108000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 18.Flynn T, Fritz J, Whitman J, et al. A clinical prediction rule for classifying patients with low back pain who demonstrate short term improvement with spinal manipulation. Spine. 2002;27:2835–2843. doi: 10.1097/00007632-200212150-00021. [DOI] [PubMed] [Google Scholar]
- 19.Fritz JM, Erhard RE, Hagen BF. Segmental instability of the lumbar spine. Phys Ther. 1998;78:889–896. doi: 10.1093/ptj/78.8.889. [DOI] [PubMed] [Google Scholar]
- 20.Fritz JM, George S. The use of a classification approach to identify subgroups of patients with acute low back pain: inter-rater reliability and short-term treatment outcomes. Spine. 2000;25:114–121. doi: 10.1097/00007632-200001010-00018. [DOI] [PubMed] [Google Scholar]
- 21.Fritz JM, Irrgang JJ. A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther. 2001;81:776–788. doi: 10.1093/ptj/81.2.776. [DOI] [PubMed] [Google Scholar]
- 22.Fritz JM, George SZ, Delitto A. The role of fear avoidance beliefs in acute low back pain: relationships with current and future disability and work status. Pain. 2001;94:7–15. doi: 10.1016/S0304-3959(01)00333-5. [DOI] [PubMed] [Google Scholar]
- 23.Frymoyer JW, Selby DK. Segmental instability: rationale for treatment. Spine. 1985;10:280–286. doi: 10.1097/00007632-198504000-00017. [DOI] [PubMed] [Google Scholar]
- 24.Harreby M, Nygaard B, Jessen T, et al. Risk factors for low back pain in a cohort of 1389 Danish school children: an epidemiologic study. Eur Spine J. 1999;8:444–450. doi: 10.1007/s005860050203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hayes MA, Howard TC, Gruel CR, Kopta JA. Roentgenographic evaluation of the lumbar spine flexion-extension in asymptomatic individuals. Spine. 1989;14:327–331. doi: 10.1097/00007632-198903000-00014. [DOI] [PubMed] [Google Scholar]
- 26.Hides JA, Jull GA, Richardson CA. Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine. 2001;26:E243–E248. doi: 10.1097/00007632-200106010-00004. [DOI] [PubMed] [Google Scholar]
- 27.Hides JA, Richardson CA, Jull GA. Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine. 1996;21:2763–2769. doi: 10.1097/00007632-199612010-00011. [DOI] [PubMed] [Google Scholar]
- 28.Jackson RP, Phipps T, Hales C, Surber J. Pelvic lordosis and alignment in spondylolisthesis. Spine. 2003;28:151–160. doi: 10.1097/00007632-200301150-00011. [DOI] [PubMed] [Google Scholar]
- 29.Jull GA, Richardson CA. Motor control problems in patients with spinal pain: a new direction for therapeutic exercise. J Manipulative Physiol Ther. 2000;23:115–117. doi: 10.1016/S0161-4754(00)90079-4. [DOI] [PubMed] [Google Scholar]
- 30.Kirkaldy-Willis WH, Farfan HF. Instability of the lumbar spine. Clin Orthop. 1982;165:110–123. [PubMed] [Google Scholar]
- 31.Klenerman L, Slade PD, Stanley IM, et al. The prediction of chronicity in patients with an acute attack of low back pain in a general practice setting. Spine. 1995;20:478–484. doi: 10.1097/00007632-199502001-00012. [DOI] [PubMed] [Google Scholar]
- 32.Knutsson F. The instability associated with disk degeneration in the lumbar spine. Acta Radiol. 1944;25:593–609. [Google Scholar]
- 33.Larsson LG, Mudholkar GS, Baum J, Srivastava DK. Benefits and liabilities of hypermobility in the back pain disorders of industrial workers. J Indust Med. 1995;238:461–467. doi: 10.1111/j.1365-2796.1995.tb01224.x. [DOI] [PubMed] [Google Scholar]
- 34.Lund T, Nydegger T, Schlenzka D, et al. Three-dimensional motion patterns during active bending in patients with chronic low-back pain. Spine. 2002;27:1865–1874. doi: 10.1097/00007632-200209010-00012. [DOI] [PubMed] [Google Scholar]
- 35.Lundberg G, Gerdle B. The relationships between spinal sagittal configuration, joint mobility, general low back mobility and segmental mobility in female homecare personnel. Scand J Rehabil Med. 1999;31:197–206. doi: 10.1080/003655099444362. [DOI] [PubMed] [Google Scholar]
- 36.Lundberg G, Gerdle B. Correlations between joint and spinal mobility, spinal sagittal configuration, segmental mobility, segmental pain, and disabilities in female homecare personnel. Scand J Rehabil Med. 2000;32:124–133. doi: 10.1080/003655000750045479. [DOI] [PubMed] [Google Scholar]
- 37.MacNab I. Disc degeneration and low back pain. Clin Orthop. 1986;208:3–14. [PubMed] [Google Scholar]
- 38.Magee DJ. Orthopaedic physical assessment. 3. Philadelphia: Saunders; 1997. p. 399. [Google Scholar]
- 39.Magnusson SP, Julsgaard C, Aagaard P, et al. Viscoelastic properties and flexibility of the human muscle-tendon unit in benign joint hypermobility syndrome. J Rheumatol. 2001;28:2720–2725. [PubMed] [Google Scholar]
- 40.Nizard RS, Wybier M, Laredo J. Radiologic assessment of lumbar intervertebral instability and degenerative spondylolisthesis. Radiol Clin North Am. 2001;39:55–71. doi: 10.1016/S0033-8389(05)70263-3. [DOI] [PubMed] [Google Scholar]
- 41.Ogon M, Bender BR, Hooper DM, et al. A dynamic approach to spinal instability. Part I. Sensitization of intersegmental motion profiles to motion direction and load condition by instability. Spine. 1997;22:2841–2858. doi: 10.1097/00007632-199712150-00007. [DOI] [PubMed] [Google Scholar]
- 42.Ogon M, Bender BR, Hooper DM, et al. A dynamic approach to spinal instability. Part II. Hesitation and giving-way during interspinal motion. Spine. 1997;22:2859–2866. doi: 10.1097/00007632-199712150-00008. [DOI] [PubMed] [Google Scholar]
- 43.O’Sullivan PB. Lumbar segmental “instability”; clinical presentation and specific stabilizing exercise management. Man Ther. 2000;2000(5):2–12. doi: 10.1054/math.1999.0213. [DOI] [PubMed] [Google Scholar]
- 44.Panjabi MM, Lydon C, Vasavada A, Grob D, Crisco JJ, Dvorak J. On the understanding of clinical instability. Spine. 1994;19:2642–2650. [PubMed] [Google Scholar]
- 45.Paris SV. Physical signs of instability. Spine. 1985;10:277–279. doi: 10.1097/00007632-198504000-00016. [DOI] [PubMed] [Google Scholar]
- 46.Pearcy M, Portek I, Shepard J. Three-dimensional x-ray analysis of normal movement in the lumbar spine. Spine. 1984;9:294–297. doi: 10.1097/00007632-198404000-00013. [DOI] [PubMed] [Google Scholar]
- 47.Posner I, White AA, Edwards WT, Hayes WC. A biomechanical analysis of the clinical stability of the lumbar and lumbosacral spine. Spine. 1982;7:389–392. doi: 10.1097/00007632-198207000-00008. [DOI] [PubMed] [Google Scholar]
- 48.Putto E, Tallroth K. Extension-flexion radiographs for motion studies of the lumbar spine: a comparison of two methods. Spine. 1990;15:107–110. doi: 10.1097/00007632-199002000-00011. [DOI] [PubMed] [Google Scholar]
- 49.Sackett DL. A primer on the precision and accuracy of the clinical examination. JAMA. 1992;267:2638–2644. doi: 10.1001/jama.267.19.2638. [DOI] [PubMed] [Google Scholar]
- 50.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–426. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 51.Simel DL, Samba GL, Matchar DB. Likelihood ratios with confidence: sample size estimation for diagnostic test studies. J Clin Epidemiol. 1991;44:763–770. doi: 10.1016/0895-4356(91)90128-V. [DOI] [PubMed] [Google Scholar]
- 52.Slosar PJ. Indications and outcomes of reconstructive surgery in chronic pain of spinal origin. Spine. 2002;27:2555–2562. doi: 10.1097/00007632-200211150-00031. [DOI] [PubMed] [Google Scholar]
- 53.Soini J, Antti-Poika I, Tallroth K, et al. Disc degeneration and angular movement of the lumbar spine: comparative study using plain and flexion-extension radiography and discography. J Spinal Dis. 1991;4:183–187. doi: 10.1097/00002517-199106000-00008. [DOI] [PubMed] [Google Scholar]
- 54.Suarez-Almazor ME, Kendall C, Johnson JA, Skeith K, Vincent D. Use of health status measures in patients with low back pain in clinical settings: comparison of specific, generic and preference-based instruments. Rheumatology (Oxford) 2000;39:783–790. doi: 10.1093/rheumatology/39.7.783. [DOI] [PubMed] [Google Scholar]
- 55.Tokuhashi Y, Matsuzaki H, Sano S. Evaluation of clinical lumbar instability using the treadmill. Spine. 1993;18:2321–2324. doi: 10.1097/00007632-199311000-00031. [DOI] [PubMed] [Google Scholar]
- 56.Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85:317–332. doi: 10.1016/S0304-3959(99)00242-0. [DOI] [PubMed] [Google Scholar]
- 57.Vlaeyen JW, Jong J, Geilen M, Heuts PH, Breukelen G. The treatment of fear of movement/(re)injury in chronic low back pain: further evidence on the effectiveness of exposure in vivo. Clin J Pain. 2002;18:251–261. doi: 10.1097/00002508-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 58.Waddell G, Somerville D, Henderson I, Newton M. Objective clinical evaluation of physical impairment in chronic low back pain. Spine. 1992;17:617–628. doi: 10.1097/00007632-199206000-00001. [DOI] [PubMed] [Google Scholar]
- 59.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 60.Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine. 2003;28:52–62. doi: 10.1097/00007632-200301010-00014. [DOI] [PubMed] [Google Scholar]
- 61.White AA, Panjabi MM. Clinical biomechanics of the spine. 2. Philadelphia: Lippincott; 1990. pp. 23–45. [Google Scholar]
- 62.Yone K, Sakou T. Usefulness of Posner’s definition of spinal instability for selection of surgical treatment for lumbar spinal stenosis. J Spinal Dis. 1999;12:40–44. [PubMed] [Google Scholar]
- 63.Zdeblick TA. A prospective, randomized study of lumbar fusion: preliminary results. Spine. 1993;18:983–991. doi: 10.1097/00007632-199306150-00006. [DOI] [PubMed] [Google Scholar]