Abstract
This is a prospective observational study comparing cases with retrospective controls. The aim of the study is to compare rib regeneration with a scaffold placed intra-periosteally against no scaffold, after costectomy in adolescent idiopathic scoliosis. A prospective study was conducted at Amrita Institute of Medical Sciences on 16 consecutive patients (51 ribs) with adolescent idiopathic scoliosis who underwent costectomy and application of gel foam in the rib bed as a scaffold. These patients were compared with a retrospective group of 15 patients (33 ribs) who did not have the scaffold. All prospective and retrospective patients were followed up for a minimum period of 6 months and were analyzed radiographically for rib regeneration and morphology. A classification system was devised to include all possible morphologies of regenerate. The resulting data, when analyzed showed that majority of ribs re-grew to normal morphology in 3–6 months in the trial group. In comparison the regeneration in the retrospective controls was slower and poorer in quality. Ribs treated by placement of gel foam scaffold in the bed regenerate to a near normal radiological profile within 6 months of costectomy compared to a slower regeneration in those without gel foam scaffold.
Keywords: Adolescent idiopathic scoliosis, Costectomy, Rib regeneration
Introduction
The rib hump, rather than the spinal deformity, is the major cosmetic deformity in scoliosis and success in treating the lateral curve is not always matched by reduction in the rib deformity [6]. Numerous procedures have been described to address the rib deformity. Schollner’s costoplasty, anterior thoracoplasties, and posterior costectomies are some of the more frequently used techniques [2, 4]. Most studies dealing with these procedures have analyzed the cosmetic correction obtained as well as the complications associated with it but none have objectively analyzed the regeneration pattern of these excised ribs after costectomies and its implications on the functional outcome in detail [1, 4, 5].
Although bone formation and regeneration after corticotomy of long bones, has been studied extensively and classification systems established [3], studies of rib regeneration following costectomy for idiopathic scoliosis have been scarce. (The authors did a Pubmed and Medline search using key words costectomy, costoplasty, thoracoplasty and rib regeneration). Due to the high incidence of donor site morbidity, and the limited availability of bone in small children, many alternate materials like allograft, synthetic bone graft substitutes and mixtures of artificial and autologous bone grafts etc. have been studied for fusions in spinal deformity. There is unanimous agreement that autologous bone graft is the gold standard. As rib is an excellent source of autologous cancellous graft, costectomy can be used as a procedure for correction of the rib hump in scoliosis as well as a source of autologous cancellous graft. Costectomy and use of rib as graft for fusion is routine in our institution for adolescent idiopathic scoliosis. This study was undertaken to classify and quantify rib regeneration following costectomy for adolescent idiopathic scoliosis. It was presumed that bone growth is faster when there is a scaffold for the cells to grow over and the quality of the regenerate is better than when they grow in an empty periosteal tube.
Material and methods
The patients were divided into 2 groups. The trial group consisted of 16 consecutive patients (51 ribs) of adolescent idiopathic scoliosis, with an average age of 14 yrs (11–16 yrs). All the patients underwent costectomy and intra-periosteal gel foam application in the rib bed. They were followed up for 1 yr with radiographs taken at 3 monthly intervals. The control group consisted of patients who had had costectomy as a part of their scoliosis correction surgery but did not have gel foam implanted into the rib bed. Fifteen consecutive patients (33 ribs), in the age range of 10–16 yrs (average14.5 yrs) fell into this group. They were analyzed retrospectively by serial radiographs taken at similar intervals for a minimum of 1 year. The X-rays of both groups were assessed to determine the quantity and quality of the regenerate.
Operative technique
All patients undergoing posterior instrumentation and fusion for Adolescent Idiopathic Scoliosis at our center routinely undergo costectomies. The surgical technique was identical in both trial and control groups. Excision of 2–3 inches each of 2–6 ribs from the convex side of the apical region of the curve is adequate in most cases. The operative technique in both groups consisted of subperiosteal dissection of the ribs. Through the original midline incision, the plane between Lattissimus Dorsi and the Erector Spinae is developed. The ribs maximally contributing to the hump are exposed from the tip of the transverse process to the posterior axillary line. About 4–6 ribs are then excised subperiosteally. Any accidental pleural tear is repaired immediately in a watertight manner. After excision and meticulous hemostasis the rib bed was reconstructed in the case of the trial group by placing absorbable gelatin sponge gel foam (Pharmacia-Upjohn) or Spongostan (Johnson& Johnson) of the corresponding size as the excised rib. The periosteum was meticulously closed in both groups. The muscle layer was then closed without a drain.
AP radiographs of the spine were taken according to the standard protocol (standing films at 1 m) immediately post op, at 6 weeks, and thereafter at 3 monthly intervals for 1 year. All ribs in both groups were analyzed for the quantity and quality of regeneration. The regenerate was classified according to our rib regenerate classification protocol. The radiological evaluation was done by an independent observer (Orthopaedic Surgeon), and the two senior authors separately, and their observations tabulated. (The intra and inter observer variability of the classification system is currently being studied).
Rib regenerate classification
The rib regenerate classification was formulated after reviewing 99 patients with 360 rib resections performed at this institute between 2001 and 2004. The following grades of regenerate are described.
No regenerate
Diffuse opacity; no corticalization
Corticalized discrete islands of regenerate
Corticalized, but irregular, oligotrophic regenerate, not in continuity
Corticalized, but irregular, oligotrophic regenerate, in continuity
Corticalized, smooth, oligotrophic regenerate, in continuity
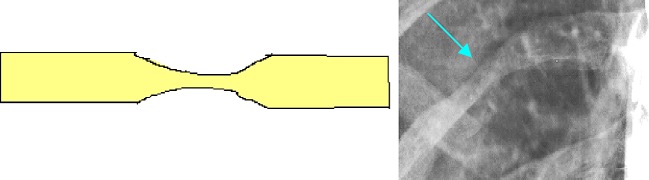
- Normal or hypertrophic regenerate [Fig. 1–7].
Fig. 2.
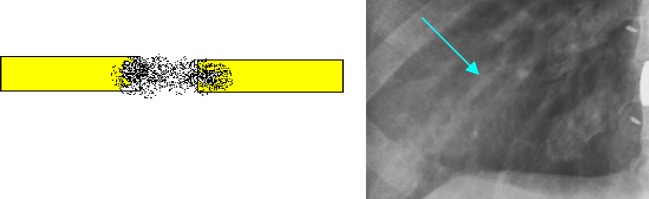
GRADE 2: Diffuse opacity; no corticalizationFig. 3.
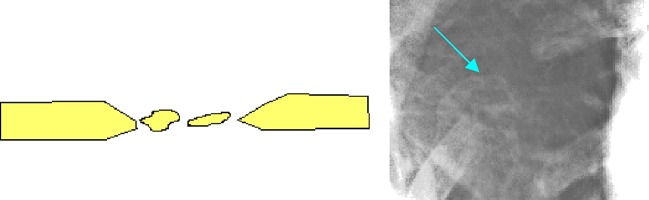
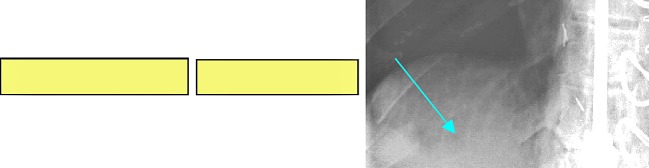
GRADE 3: Corticalized discrete islands of regenerateFig. 4.
GRADE 4: Corticalized, but irregular, oligotrophic regenerate, not in continuityFig. 5.
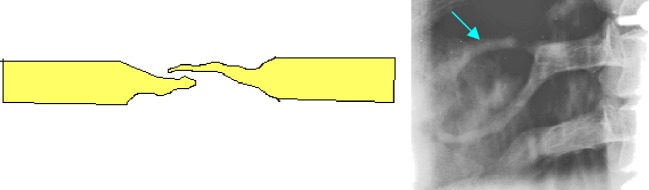
GRADE 5: Corticalized, but irregular, oligotrophic regenerate, in continuityFig. 6.
GRADE 6: Corticalized, smooth, oligotrophic regenerate, in continuity
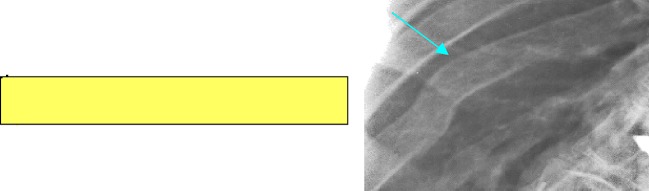
Fig. 1.
GRADE 1: No regenerate
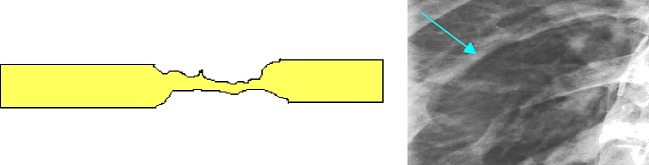
Fig. 7.
GRADE 7: Normal or hypertrophic regenerate
Results and analysis
Control group (15 patients, 33 ribs)
In the control group (without gel foam scaffold) 33 rib resections in 15 patients were analyzed for rib regeneration morphology. At 3 months most of the control group ribs (27/33) fell between grades 2–3 in the regenerate classification. (Table 1). At 6 months there was marginal improvement with majority of the ribs falling in between grades 3 and 5 (22/27). By 1 yr almost all ribs (26/27) on which data was available regenerated to more than grade 4. At 6 months and 1 y 2 patients with a total of 6 rib resections were not available for follow up. There was no significant improvement in the regenerate beyond 1 yr in 21 ribs that were followed up for a period of 2 yrs.
Table 1.
Control group (15 patients, 33 ribs) No: of ribs
| Classification | 3 months | 6 months | 1 yr | 2 yrs |
|---|---|---|---|---|
| 1 | 1 | |||
| 2 | 22 | 1 | ||
| 3 | 5 | 12 | 1 | 1 |
| 4 | 2 | 4 | 14 | 5 |
| 5 | 3 | 6 | 2 | 4 |
| 6 | 0 | 4 | 6 | 5 |
| 7 | 0 | 0 | 4 | 6 |
| Total | 33 | 27 | 27 | 21 |
Trial group (16 patients, 51 ribs)
In the trial group (with gel foam scaffold) 16 patients with 51 rib resections were analyzed for regeneration morphology and time. At 3 months 33/51 ribs regenerated to grade 5 or more. On follow up at 6 months 42 out of 51(82%) had achieved grade 6 or 7 of regeneration and no rib followed up fell below grade 4 (Table 2). Although only 13 ribs were followed up at 1 yr, this drop out was not significant, as 42/51 ribs had already achieved maximum regeneration grades at 6 months.
Table 2.
Trial group (16 patients, 51 ribs) No: of ribs
| Classification | 3 months | 6 months | 1 yr |
|---|---|---|---|
| 1 | 3 | ||
| 2 | 4 | ||
| 3 | 5 | ||
| 4 | 6 | 1 | |
| 5 | 17 | 8 | |
| 6 | 8 | 11 | 5 |
| 7 | 8 | 31 | 8 |
| Total | 51 | 51 | 13 |
It was observed that in the trial cases, (in which gel foam was used as a scaffold) the ribs regenerated faster and to near normal morphology. Almost all ribs in the trial group reached grade 4 or above at 6 months whereas in the control group the regenerate was poor with most regeneration falling below grade 4 at the same period. The data was analyzed using the Fischer exact test and was found to be statistically significant with P values of >0.0001 at 3 months, >0.0001 at 6 months and >0.0005 at 1 y.
Discussion
There is very little information available in medical literature on rib regeneration. H.H. Steele studied 1840 ribs in 392 patients and found that the ribs regenerated in an average time of 3 months. Barret, D.S. et al. in a study of 55 patients (no: of ribs not mentioned) has quoted the average time for regeneration as 3.6 months after costectomy. (Steele did not use X-rays for his analysis of rib regeneration. In Barrett’s study the author has not mentioned what technique of analysis was used.) The discrepancy in the regeneration times may be due to difference in methodology of evaluation of results. The method of confirmation of regeneration in the series of Steele. was by palpation. The surgical technique in his series and the present study were different. Steele used a separate incision for rib dissection and excision but placed a scaffold in the rib bed before closure. Barret et al. did not use a scaffold in the rib bed after excision but the surgical technique was similar to the present study. He radiologically evaluated the regenerate without a classification. In the present study 16 patients (51 ribs), with application of gel foam as a scaffold in the rib bed were evaluated against a retrospective control group of 15 patients (33 ribs) without placement of gel foam in the rib bed. The regeneration time in the gel foam group was found to be comparable to the above studies but the consolidation to near normal radiological profile based on the new classification, took an average of 6 months. This study has objectively documented faster and better regeneration of ribs by using a scaffold of gel foam in the rib bed as opposed to the controls without gel foam placement. The study also demonstrated normal radiological consolidation of regenerate at 6 months compared to subjective assessment of regeneration in 3 and 3.6 months by Steele and Barret et al. respectively. The retrospective control group in the present series had slower rate of regeneration compared to the above-mentioned studies. The regeneration time averaged 6 months.
This study does not, however, look into the cosmetic and functional implications of the regenerate. Does a good radiological regenerate necessarily mean a good cosmetic outcome? Does the good regenerate correlate clinically with good pulmonary function? These are issues not addressed by this paper. Prospective and retrospective studies are currently ongoing at our centre to ascertain such a correlation. The applicability of information regarding regeneration of ribs to other areas of bony regeneration can be pursued through further studies (though rib being a membranous bone its regeneration characteristics may differ substantially from endochondral bone). It would also be interesting to postulate the effect of scaffolding in cortical bone defects.
Conclusions
Ribs regenerate to a near normal radiological profile within 6 months of costectomy when gel foam scaffold is placed in the rib bed.
Rib regeneration in patients without gel foam scaffold is slower and poorer in quality.
It seems that the classification system allows an objective radiological assessment of the quality and quantity of rib regeneration.
References
- 1.Barret DS, MacLean JGB, Bettany J, Ransford AO, Edgar MAJ. Costoplasty in adolescent idiopathic scoliosis. Objective results in 55 patients. J Bone Joint Surg Br. 1993;75:881–885. doi: 10.1302/0301-620X.75B6.8245076. [DOI] [PubMed] [Google Scholar]
- 2.Broome G, Simpson AHRW, Catalan J, Jefferson RJ, Houghton GR. The modified Schollner costoplasty. J Bone Joint Surg Br. 1990;72:894–900. doi: 10.1302/0301-620X.72B5.2211779. [DOI] [PubMed] [Google Scholar]
- 3.Cattaneo R, Catagni MA, Villa A, Maiocchi AB, Aronson J, Paley D, Bendetti GB (1991) In: Maiocchi AB, Aronson J (eds) Operative Principles of Ilizarov, 1st edn. Williams and Wilkins, Italy, pp 52–55
- 4.Owen R, Turner A, Bamforth JSG, Taylor J, Jones RS. Costectomy as the first stage of surgery for scoliosis. J Bone Joint Surg Br. 1986;68:91–95. doi: 10.1302/0301-620X.68B1.3941148. [DOI] [PubMed] [Google Scholar]
- 5.Steele HH. Rib resection and spine fusion in correction of convex deformity in scoliosis. J Bone Joint Surg Am. 1983;65:920–925. [PubMed] [Google Scholar]
- 6.Weatherly CR, Draycott V, O’Brien JF, Benson DR, Gopalakrishnan KC, Evans JH, O’Brien JP. The rib deformity in adolescent idiopathic scoliosis, a prospective study to evaluate changes after Harrington distraction and posterior fusion. J Bone Joint Surg Br. 1987;69:179–182. doi: 10.1302/0301-620X.69B2.3818745. [DOI] [PubMed] [Google Scholar]