Abstract
Solitary osteochondroma of the cervical spine is a rare manifestation of a common bony tumour. It can create symptoms, depending on the adjacent compressed structures. In this report, a patient suffering solitary osteochondroma on the anterolateral aspect of the C7 vertebral body is presented and the literature is reviewed. A 46-year-old female presented with dysphagia and pain at the anterolateral surface of her neck during cervical movements or application of local pressure. The clinical and imaging assessment ascertained that the above complaints were due to a local tumour in the neck firmly attached to the spine at the anterolateral aspect of the C7 and which resembled an osteochondroma. Surgical treatment was chosen due to the persistence of the symptoms. The lump was resected using an anterolateral cervical approach and it was sent to the pathology department for confirmation of the lesion’s histological character. The patient was completely relieved of her symptoms. Resection of the osteochondroma seems to be the only reliable solution for definitive relief from the clinical complaints. This surgical treatment, as it is reported, has no major complications and gives good functional results. One to four per cent of the osteochondromas are located at the spine. At the cervical spine, they can cause neurological symptoms and more rarely, dysphagia. Reviewing the literature, no case of solitary osteochondroma located in the anterior aspect of the C7 body was found. Two cases suffering from dysphagia were reported due to external compression by anterior hyperostosis of the cervical spine, but not due to osteochondroma.
Keywords: Benign tumour, Solitary osteochondroma, Cervical spine, C7, Dysphagia
Case Report
A 46-year-old female presented with a history of dysphagia due to a lump at the left side of her neck that had been there for a period of almost a year. Pain developed when the neck was turned to the right and it deflected to her left arm, or when local pressure was applied. Examining the lump by palpation, an osseous protuberance, a firmly attached to the cervical spine, was noticed at the base of the neck, over the left anterolateral aspect. Imaging assessment involved anteroposterior and lateral plain radiographs (Figs. 1 and 2), Computer Tomograpy (CT), (Fig. 3) and Magnetic resonance imaging (MRI) scans of the cervical spine. Whole body bone scintigraphy completed the study.
Fig. 1.

Preoperative antero - posterior plain radiograph of the cervical spine.
Fig. 2.

Preoperative lateral plain radiograph of the cervical spine.
Fig. 3.
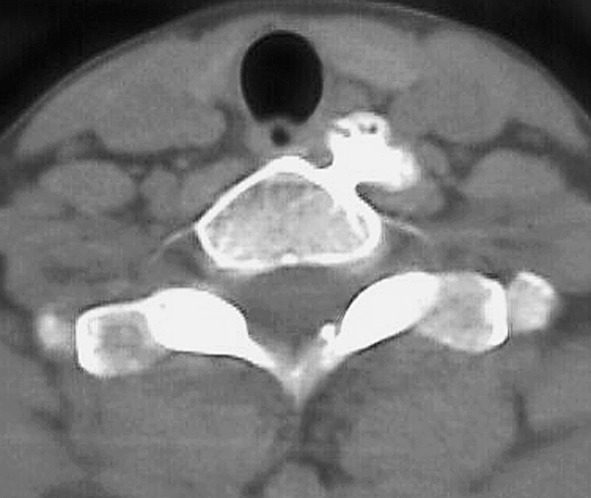
Preoperative CT, showing the osteochondroma of C7.
On completion of the patient’s clinical and radiological investigation, we were led to believe that her complaints were due to a local tumour in the neck that was firmly attached to the spine at the anterolateral aspect of the C7 and that had the characteristics of a solitary osteochondroma.
Surgical treatment
Results
Due to the persistence of the symptoms, surgical treatment was chosen and performed soon after. Under general anaesthesia, and through an anterolateral cervical approach, the lump was clearly visualized. It was of the size of a large chick-pea, with a smooth top surface, and with a thin cartilaginous cap. It was prepared and resected from its pedicle, using a Louer rounger. The resected piece was sent to the pathology department for confirmation of the lesion’s histological character. A drain was applied for 24 h. After 4 days of hospitalization the patient was discharged. Postoperative CT was carried out (Fig. 4). The patient was completely relieved of her symptoms and remained symptomless until her latest follow up, conducted 3 years postoperatively.
Fig. 4.
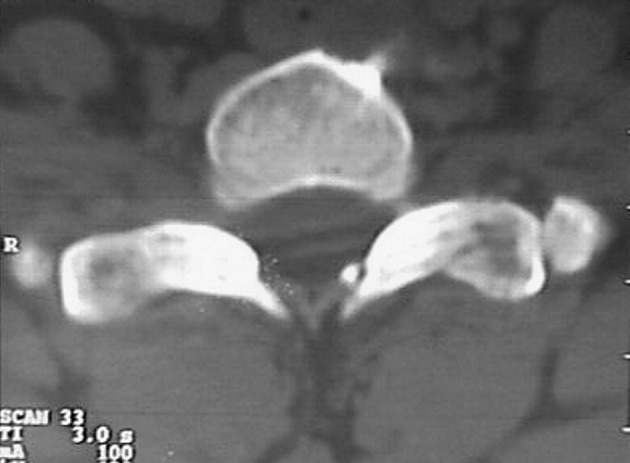
Postoperative CT documenting the resection of the tumour.
Report of the Pathology
Histologically, the small pieces of trabecular bone were covered with a thin rim of hyaline cartilage cap. The deeper portions of the bone seemed to spread gradually into the cortex and spongiosa of the small pieces of the resected host bone.
Discussion-conclusions
Osteochondromas are usually benign symptomless tumours, diagnosed in the second or third decade of life. About 1–4% of them occur in the spine [1, 7].
Spinal osteochondromas can be of two types: (1) spinal osteochondromas in patients with multiple osteochondromas, and (2) solitary osteochondromas occurring in the spine [1, 12, 15]. It is reported that the age of patients in the first group is 21.6 ± 1.8 years compared to 30.0 ± 2.1 years for those in the second group and that there is a significant male predominance overall (m:f = 2.5:1) [1].
They can be located anywhere in the cervical spine, as solitary osteochondroma, confluent with marrow of the C6 articular pillar [8], or arising from the spinous process of the C1 [4], C2 [5], C6 [22] and the C7 vertebra [10], from the C2 neural arch [4], from the anterior aspect of the C2 body [18], or as hereditary multiple exostoses as in the case of a 12-year-old girl with an exostosis in the C5 [23].
A variety of signs and symptoms can show up, including those of spinal cord or spinal root compression [7, 19, 20]. Symptoms may be due to compressive myelopathy, from intraspinal osteochondroma [14], or from the very rare osteochondroma of costal origin [21]. Radiculopathy can exist [2], or can dysphagia due to external compression by rare anterior solitary hyperostosis of the cervical spine [9], or hereditary multiple exostosis with cervical ventral protuberance [3]. It is reported that hereditary multiple exostoses can cause acute cervical myelopathy, tetraplegia, and apnea [24], or a spastic quadriplegia or tetraparesis [6, 23].
Spinal cord compression is reported more than twice as frequently in the multiple osteochondroma group as is in the single osteochondroma group (77% vs 33%)[1].
Reviewing the literature, no case of solitary osteochondroma located in the anterior aspect of the C7 body was found. Regarding our patient’s main symptom, it was dysphagia; the two cases that have been previously reported were due to external compression by anterior hyperostosis of the cervical spine, but were not due to osteochondroma [9].
Although unusual, osteochondroma should be considered in the differential diagnosis (dd) of benign appearing tumours in the cervical spine [11]. The dd also includes the large anterior osteophytes formation in Forestiers’ disease [9], or other bony overgrowths and abnormal calcifications about the spine, and know as syndesmophytes, which are vertically oriented outgrowths of trabecular bone forming in the outer margins of the annulus fibrosus and related to repeated episodes of inflammation and repair [13]. Syndesmophytes are classically seen in ankylosing spondylitis and colonic spondyloarthropathy. Bulky paravertebral excrescences are more likely to be found in psoriatic arthritis and Reiter’s syndrome. In cases with neurologic findings, OPLL, which is a progressive disease that can result in severe radicular and myelopathic symptoms, must be considered in dd.
Though CT has been reported to be the preferred imaging procedure for the study of osteochondromas [1], more recent papers report that cervical osteochondromas are best evaluated with routine MRI and noncontrast CT scans [2]. In our case, the MR images demonstrated adequately the relationship of the tumour, the spinal cord, and the adjacent soft tissue. CT played an important role in demonstrating the exact origin and nature of the tumour [16, 17].
In patients suffering from solitary intraspinal vertebral osteochondroma with compressive myelopathy, clinical histories, CT studies, MRI studies, routine radiographs, and/or myelographic studies of the lesions must be carried out. In these patients, although MRI is the preferred method for localizing the lesion, CT can be more specific, because of its sensitivity, when the diagnosis is in doubt [14].
Resection of the osteochondroma seems to be the only reliable solution for definitive relief from the clinical complaints. The surgical treatment, as it is also reported, has no major complications and gives good functional results [7, 9, 14].
References
- 1.Albrecht S, Crutchfield JS, SeGall GK. On spinal osteochondromas. J Neurosurg. 1992;77(2):247–252. doi: 10.3171/jns.1992.77.2.0247. [DOI] [PubMed] [Google Scholar]
- 2.Arasil Spine. 1996;21:516. doi: 10.1097/00007632-199602150-00021. [DOI] [PubMed] [Google Scholar]
- 3.Barros Spine. 1995;20:1640. doi: 10.1097/00007632-199507150-00015. [DOI] [PubMed] [Google Scholar]
- 4.Cherubino P, Benazzo F, Castelli C. Osteochondroma of the cervical spine. Ital J Orthop Traumatol. 1991;17(1):131–134. [PubMed] [Google Scholar]
- 5.Cohn RS, Fielding JW. Osteochondroma of the cervical spine. J Pediatr Surg. 1986;21(11):997–999. doi: 10.1016/s0022-3468(86)80123-3. [DOI] [PubMed] [Google Scholar]
- 6.Cooke RS, Cumming WJ, Cowie RA. Osteochondroma of the cervical spine: case report and review of the literature. Br J Neurosurg. 1994;8(3):359–363. doi: 10.3109/02688699409029627. [DOI] [PubMed] [Google Scholar]
- 7.deNed Tijdschr Geneeskd 199914352510321262 [Google Scholar]
- 8.Eaton BA, Kettner NW, Essman JB. Solitary osteochondroma of the cervical spine. J Manipulative Physiol Ther. 1995;18(4):250–253. [PubMed] [Google Scholar]
- 9.Grasshoff H, Motsch C, Mahlfeld K. Vertebragenic dysphagia. Zentralbl Chir. 1999;124(11):1041–1044. [PubMed] [Google Scholar]
- 10.Haritidis J, Tsikouriadis P, Tsakonas A. Osteochondroma of the cervical spine. Case report. Chir Organi Mov. 1993;78(4):251–253. [PubMed] [Google Scholar]
- 11.Inglis AE, Rubin RM, Lewis RJ, Villacin A. Osteochondroma of the cervical spine. Case report. Clin Orthop. 1977;126:127–129. [PubMed] [Google Scholar]
- 12.Jackson A, Hughes D, StClair Forbes W, Stewart G, Cummings WJ, Reid H. A case of osteochondroma of the cervical spine. Skeletal Radiol. 1995;24(3):235–237. doi: 10.1007/BF00228935. [DOI] [PubMed] [Google Scholar]
- 13.Jones MD, Pais MJ, Omiya B. Bony overgrowths and abnormal calcifications about the spine. Radiol Clin North Am. 1988;26(6):1213–1234. [PubMed] [Google Scholar]
- 14.Khosla Spine. 1999;24:77. doi: 10.1097/00007632-199901010-00019. [DOI] [PubMed] [Google Scholar]
- 15.Malat J, Virapongse C, Levine A. Solitary osteochondroma of the spine. Spine. 1986;11(6):625–628. doi: 10.1097/00007632-198607000-00017. [DOI] [PubMed] [Google Scholar]
- 16.Morikawa M, Numaguchi Y, Soliman JA. Osteochondroma of the cervical spine. MR findings. Clin Imaging. 1995;19(4):275–278. doi: 10.1016/0899-7071(94)00063-i. [DOI] [PubMed] [Google Scholar]
- 17.N’dri K, Lapra-Lepine C, Colonna C, Tavernier T, Bochu M. Imaging of spinal osteochondroma of neurologic nature. Apropos of 7 cases. J Radiol. 1994;75(8–9):427–431. [PubMed] [Google Scholar]
- 18.Nielsen OG, Gadegaard L, Fogh A. Osteochondroma of the cervical spine. J Laryngol Otol. 1986;100(6):733–736. doi: 10.1017/s0022215100099990. [DOI] [PubMed] [Google Scholar]
- 19.Prasad A, Renjen PN, Prasad ML, Bhatty GB, Madan VS, Buxi TB, Agarwal SP. Solitary spinal osteochondroma causing neural syndromes. Paraplegia. 1992;30(9):678–680. doi: 10.1038/sc.1992.132. [DOI] [PubMed] [Google Scholar]
- 20.Tajima K, Nishida J, Yamazaki K, Shimamura T, Abe M. Case report 545: Osteochondroma (osteocartilagenous exostosis) cervical spine with spinal cord compression. Skeletal Radiol. 1989;18(4):306–309. doi: 10.1007/BF00361214. [DOI] [PubMed] [Google Scholar]
- 21.Tang Spine. 1998;23:1900. doi: 10.1097/00007632-199809010-00021. [DOI] [PubMed] [Google Scholar]
- 22.Traina GC, Massari L, Chiarelli GM. A rare case of solitary exostosis of the cervical spine. Ital J Orthop Traumatol. 1988;14(3):385–387. [PubMed] [Google Scholar]
- 23.Tully RJ, Pickens J, Oro J, Levine C. Hereditary multiple exostoses and cervical cord compression: CT and MR studies. J Comput Assist Tomogr. 1989;13(2):330–333. doi: 10.1097/00004728-198903000-00029. [DOI] [PubMed] [Google Scholar]
- 24.Wen DY, Bergman TA, Haines SJ. Acute cervical myelopathy from hereditary multiple exostoses: case report. Neurosurgery. 1989;25(3):472–475. doi: 10.1097/00006123-198909000-00028. [DOI] [PubMed] [Google Scholar]


