Abstract
Atlantoaxial (C1–C2) facet joint osteoarthitis is a distinct clinical syndrome that often goes unrecognized. Severe pain resistant to conservative treatment that is corroborated by the radiographic findings represents the indication for surgery. The aim of this study was to retrospectively examine the long-term outcome [after an average 6.5 years (SD 4.0)] of C1-2 fusion for osteoarthritis of the atlantoaxial segment in 35 consecutive patients [25 male, 10 female; aged 62 (SD 15) years]. At follow-up, clinical outcome and radiological status was examined in 27/35 (77%) patients, and self-rated pain and disability (Neck Pain and Disability Scale; NPDS) in 29/35 (83%) patients. In 27/35 patients (77%), 2 screws were inserted; in 7 patients (20%), only 1 screw; and in 1 patient (3%), no screws. 11% of the patients had late complications requiring revision surgery. All patients showed solid fusion at the long-term follow-up. 26% patients showed an improvement in sensory disturbances, 63% no change, and 11% a worsening. 89% were pain-free or had markedly reduced pain. The average score on the NPDS (0–100) was 34 (SD 27), representing ‘mild’ neck problems, and the average pain intensity (0–5 VAS) was 1.5 (SD 1.5). Eighty-five percent of the patients declared that they would make the same decision again to undergo surgery. In conclusion, in a group of patients with a painful and debilitating degenerative disorder of C1-2, posterior transarticular atlantoaxial fusion proved to be an effective treatment with a low rate of serious complications.
Keywords: Degenerative changes, Atlantoaxial segment diagnostics, Surgical technique, Fusion
Introduction
Atlantoaxial (C1–C2) facet joint osteoarthitis (Fig. 1) is a distinct clinical syndrome with a natural history that differs from that of degenerative disorders of the lower cervical spine [19, 27]. It represents a neglected entity that often goes unrecognized for a long time. In part, this might be due to the limitations of conventional radiographs: in lateral and anteroposterior views, the articulation between the first and second vertebrae is obscured by the overlying structures of the maxilla and the base of the cranium. Furthermore, the symptoms associated with degenerative changes of the atlantoaxial facets are somewhat unspecific, expressed mostly as severe unilateral pain in the suboccipital area. Physical examination typically reveals marked restrictions in rotation towards the affected side and localized unilateral tenderness at the occipitocervical junction [27]. The diagnosis is confirmed by plain radiographs of the C1–C2 articulation (transoral view; see Fig. 2), on the basis of unilateral joint-space narrowing or obliteration, osteophyte formation and subchondral sclerosis.
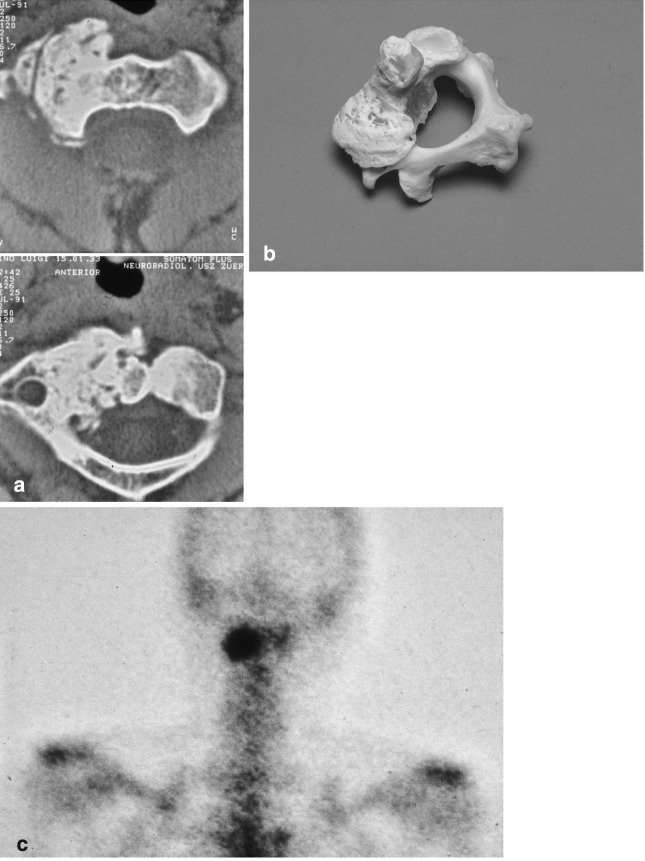
Fig. 1.
Osteoarthritis of the C1/2 facet joint: a Male, 85 years. Severe, unilateral neck pain for 4 years; CT shows typical unilateral arthritis of the C1/2 joint, b anatomical specimen depicting the situation as seen in the CT of a, c osteoarthritis of the atlantoaxial joint revealed by a well defined “hot spot” in the bone scan. This investigation may be useful as an unspecific tracer in cases with chronic neck pain. The positive result indicates the need for more specific diagnostic tests
Fig. 2.
Patient B.L. (71 years, female). The patient suffers from intractable unilateral suboccipital neck pain. Radiological investigation with transoral AP-view of the atlas reveals instability and osteoarthritis of the right C1/2 facet joint
As is the case for degenerative changes of the extremities, the cause of osteoarthritic changes of the atlantoaxial segment remains largely unknown. Previous experience of trauma is often reported [8], but a direct correlation with the atlantoaxial problem can seldom be established. Some studies have suggested a connection between atlantoaxial arthritis and anatomical anomalies, systemic disease or rheumatoid arthritis [12, 16, 22].
There are no conclusive figures in the literature regarding the prevalence of atlantoaxial arthritis. Halla et al. [19] reported on 27 cases with C1–C2 osteoarthritis, which represented 4% of all patients with osteoarthritis of the spine. Zapletal et al [34] reported a radiologic prevalence of 4.8% in patients undergoing radiographic investigation of the paranasal sinuses. In their series of 355 examinations, the prevalence of atlantoaxial osteoarthritis increased with age, ranging from 5.4% in the sixth decade to 18.2% in the ninth decade of life [34].
The basic indication for surgery is severe pain that is resistant to conservative treatment and that corresponds with radiographically recorded changes of the atlantoaxial joints [16]. Atlantoaxial fusion is typically the treatment of choice.
Internal fixation of the atlantoaxial segment represents a surgical challenge, as the anatomic area is not very accessible and the bony structures are small. This renders the insertion of surgical implants and the achievement of bony fusion somewhat difficult. For a long time, the traditional method of fixation was the posterior wiring technique [3, 10], but this was subsequently shown to result in a high rate of pseudarthrosis due to the isolated posterior fixation [5, 9]. The superior biomechanical stability of atlantoaxial transarticular screw fixation [17, 25] typically results in fusion rates of 90–100% [5, 9, 16, 28]. Studies in which the two techniques have been directly compared reveal solid fusion rates of 86% for posterior wiring compared with 98% for transarticular screw fixation [5], and 58% versus 100% respectively [9].
The aim of the present study was to examine clinical, radiological and patient-orientated outcomes in a group of 35 patients who had undergone C1–C2 fusion on average 6.5 years ago. The study was primarily retrospective, but the standard pre-operative clinical data were also available for comparison with the long-term follow-up data.
Patients and methods
Patients
Thirty-five patients took part in the study; these represented all the patients from the authors’ Spine Unit who had undergone C1-2 fusion for painful osteoarthritis of the atlantoaxial segment between January 1986 and October 2000; the procedure constitutes approximately 7% of the authors’ cervical spine caseload. The mean age of the patients at operation was 62 (SD 15, range 28–82) years; there were 25 women and 10 men.
Pre-operative evaluation
Pre-operative evaluation included patient history, imaging, and clinical and neurological evaluation by the treating surgeon.
The primary indication for surgery was atlantoaxial (C1–C2) facet joint osteoarthritis, accompanied by severe pain in the suboccipital area. The diagnosis was established if the clinical findings were corroborated by the radiological investigation. The clinical signs included unilateral tenderness at the atlantoaxial level, with greatest pain at the lateral process of the atlas. Further, cervical spine rotation in the neutral position and in maximum flexion was blocked or restricted (by at least 50%) unilaterally, whereas flexion and extension manoeuvres were less painful. Typically, the patients experienced severe, sharp, unilateral pain when trying to rotate the head; some used their hands to stabilize their head in order to reduce the pain.
The imaging/investigative procedures undertaken prior to surgery included: transoral anteroposterior radiographs in all 35 cases (Fig. 2); CT and MRI in 8 cases (23%); CT only in 25 cases (71%); MRI only in 1 case (3%); no additional imaging in 1 case (3%).
Surgical technique
The surgery was performed using the Magerl transarticular fixation technique [18] (Fig. 3).
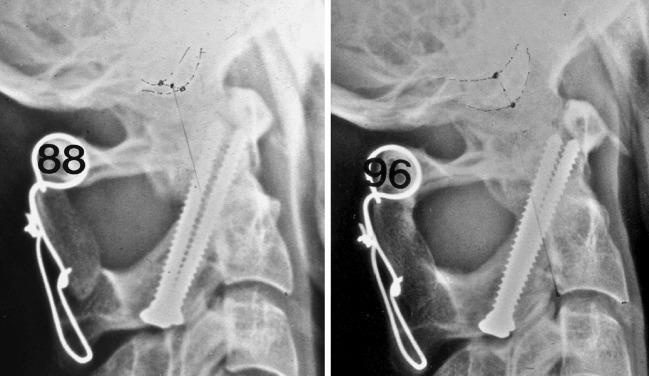
Fig. 3.
Solid atlantoaxial fusion using the transarticular screw fixation technique
Short-term radiological follow-up
Atlas anteroposterior and lateral radiographs were taken 3 months after surgery and analysed in terms of the presence or absence of fusion (no fusion = no spongiosa bridge to graft; partly-fused = line visible between graft and vertebra C1; complete fusion = complete spongiosa fixation).
Clinical and questionnaire follow-up assessment
In October 2001, all the patients were contacted by letter and invited to come for a follow-up examination at the hospital. This assessment comprised imaging (atlas anteroposterior and lateral radiographs) and a clinical and neurological evaluation carried out by an independent physician. Active range of motion of the cervical spine was measured with a simple goniometer and measuring tape in all three planes of movement (values recorded to the nearest 5 degrees and whole cm respectively) [6]. The patients were requested to complete the Neck Pain and Disability Scale (NPDS; score 0–100) [30], adapted for the German language by Bremerich et al. [2]. The patients were also asked whether they would, in retrospect, make the same decision to undergo surgery, if they had known then, what they know now, about the outcome of the operation (possible answer options: “yes” (=“satisfied” patients) and “no” (=”dissatisfied” patients)).
Data analysis
Descriptive and frequency analyses were used to describe the baseline patient characteristics and categorical outcomes. Relationships between categorical variables were examined using contingency tables with Chi-square/Fisher’s exact text (for 2×2 categories). Student’s t tests or Mann-Whitney tests (depending on normality of the data) were used to examine differences between the outcome groups “good” and “poor”, in respect of various continuous variables. Statistical significance was accepted at the P<0.05 level.
Results
Preoperative clinical status
Pre-operatively, severe and disabling pain was experienced by all 35 (100%) patients. Neurological disturbances (dysaesthesia of the head and face) were evident in 16 (46%) patients (6 constantly, 10 intermittently), and subjectively decreased motor function (strength deficits in the upper extremity) in 2 (6%) patients.
Surgery details
The average duration of the operation was 88 min; blood-loss was 307 ml (SD 190, range 50–800); and duration of hospital stay was 11.9 (SD 3.9, range 8–22) days.
Each of these variables showed a significant reduction with increasing operative experience over the 14 year period examined (P< 0.006 in each case).
Intraoperative complications
In 1/35 patients (3%), a lamina fracture with screw breakage occurred during insertion on one side. There were no other intraoperative complications.
Screw fixation
In 27/35 patients (77%), two bilaterally placed transarticular screws were inserted; in 7 cases (20%), the CT revealed doubtful anatomical dimensions of the isthmus of C2 and only one screw was inserted; and in one case (3%), no screws could be inserted as the patient had a short and bulky neck with increased cervicothoracic kyphosis preventing correct positioning of the drill holes (in this patient, posterior wiring and bone graft was used).
In one patient, a washer had to be used due to an intraoperative fissure of the cortex of the interarticular part of C2 (see above; intraoperative complications).
Postoperative complications
4/35 (11%) of the patients had postoperative complications: there was 1 case (3%) of infection, requiring superficial wound revision without removal of the screws; 1 case (3%) of excessive calcification of the spinous process of C2 causing pain; and two cases of pdeudarthrosis with persistent neck pain requiring re-fixation and additional grafting within the first year after surgery.
Radiographic data at first clinical follow-up (3 months after surgery)
Radiographs were available for 34/35 (97%) patients 3 months after surgery: 14 (41%) showed complete fusion; 19 (56%) partial fusion and 1 (3%) no fusion.
Long-term follow-up (radiographic, clinical, and patient self-rated outcome)
Participation rate for long-term follow-up examinations
A total of 27/35 (77%) patients agreed to attend the hospital for the follow-up assessment and to complete the Neck Pain and Disability scale. Two patients, aged 81 and 82 at the time of surgery, had died in the meantime, and the reasons given for non-attendance by the remaining 6 patients were: “living abroad” (n=3), “no interest in attending” (n=1), and “too old, not very mobile and living quite a distance from the hospital” (n=2). The latter 2 patients nonetheless agreed to complete the questionnaire, such that the self-rated outcome measures were available for 29/35 (83%) patients).
The patients who did not attend for follow-up were significantly older than those who did attend (P=0.04), but otherwise did not differ significantly in relation to gender, pre-operative symptoms, and fusion status at the first post-operative check-up.
The average duration of the follow-up for the 29 patients that completed at least the questionnaire was 6.5 years (SD 4.0, range 1.0–14.5).
Radiographic data
26/27 patients who attended for the long-term follow-up underwent radiography (1 patient underwent clinical investigation only and brought with him his latest radiographs from the GP, which were used for the assessment of fusion status only). In the lateral radiographs, all 27 patients showed solid fusion i.e. continuity of the bone trabeculae from the graft to the adjacent bony structures of the atlas and axis.
Clinical data
Neurological examination
At the long-term follow-up, 14/27 patients (52%) were completely pain-free. Pain was reduced in 10/27 patients (37%) and the same in 3/27 patients (11%) compared with the status before the operation.
Of the two patients with strength deficits before surgery, 1had less marked deficits at follow-up and the other experienced the same deficits as before the operation.
21/27 patients (78%) showed no sensory disturbances at follow-up; a further 5/27 patients (19%) showed intermittent disturbances, and 1/27 patient (4%) constant sensory disturbances. Compared with the pre-operative situation, this represented an improvement in 7/27 patients (26%), no change in 17/27 patients (63%) and a worsening in 3/27 patients (11%).
Re-operation rate
3/27 patients (11%) had undergone further surgical procedures on the cervical spine since the index surgery (2 patients had had one further operation; and 1 patient had had two further operations).
Range of motion
The ranges of motion for each of the three cardinal planes of movement were as follows: axial rotation, 58° (SD 23); chin to chest distance from full flexion to full extension, 9 cm (SD 3); lateral flexion, 20° (SD 8). Compared with normal values [6], these results indicate a restriction of motion, predominantly in terms of rotation.
The values for the range of flexion/extension correlated highly significantly with the self-ratings in response to the question in the Neck Pain and Disability Scale “how much trouble do you have looking up and down” (R=0.66, P=0.0002). Similarly, the range of rotation showed a significant correlation with the answers to the question “how much trouble do you have turning your neck” (R=0.60, P=0.001). Thus, there was good agreement between the patient’s self-rated “disability” and the objectively measured ranges of motion.
Patient self-rated outcome
Of the 29 patients who completed the patient-orientated questionnaire, 24 (83%) reported that they would undergo the procedure again, if they had known then, what they knew now, about the outcome. 5 patients (17%) declared that they would not make the same decision to undergo surgery, if they found themselves in the same situation again.
The average score on the NPDS scale (best possible=0, worst possible=100) at the time of the follow-up was 34.2 (SD 27.2, range 0–89) points. According to the categories described by Wheeler et al [30], the degree of pain and disability shown by this group of patients at the time of follow-up was minimal for 13/29 (45%) patients, mild for 6 (21%) patients, moderate for 1 (3%) patient, moderate to severe for 6 (21%) patients and severe for 3 (10%) patients.
The average VAS pain intensity (on a 0–5 scale) from the five pain questions in the NPDS (how bad is your pain today; pain on average; pain at worst; pain whilst standing; pain whilst walking) was 1.5 (SD 1.5, range 0.0–4.5).
Although only few of the patients (5/29 (17%)) declared being dissatisfied with the procedure, i.e. they would not make the same decision again to undergo surgery, bivariate analyses were still able to reveal a number of factors that were significantly associated with outcome. The variables that differentiated between the two groups (“satisfied” and “dissatisfied”) are shown in Table 1. Briefly, the more positive outcome group had: a higher mean age, fewer post-operative complications, a higher objectively-measured ROM in the sagittal plane, less trouble “looking up and down” (an item from the NPDS), less pain (as reported during the clinical assessment, and as rated on the five pain questions of the NPDS), and less overall disability (from NPDS). Of all of these factors, pain was the one that distinguished most significantly and consistently between the two outcome groups. Factors that did not differentiate between the two outcome groups included gender, length of follow-up, and fusion status at 3 months.
Table 1.
Associations between global outcome and various potential “explanatory” factors (demographic, clinical, and patient self-assessment variables)
| Variable | Global outcome | P valuea | |
|---|---|---|---|
| Satisfied (n=24) | Dissatisfied (n=5) | ||
| Demographic/medical variables | |||
| Age at operation (years) | 63.1 (13.2) | 44.8 (16.1) | 0.01 |
| Gender | 75% female | 60% female | 0.60 |
| Length of follow-up (years) | 6.3 (4.2) | 7.0 (2.7) | 0.74 |
| Fusion at 3 months | 33% fused | 80% fused | 0.15 |
| Late complications/revision op | 96% no | 60% no | 0.015 |
| Range of motion at follow-up | |||
| Rotation, degrees | 59.6 (24.3) | 51.3 (11.1) | 0.51 |
| Flexion-extension, cm | 9.4 (3.2) | 5.3 (1.0) | 0.02 |
| Lateral bending, degrees | 19.3 (7.9) | 21.3 (10.3) | 0.67 |
| Clinical assessment | |||
| Pain | 0% not improved | 75% not improved | 0.0001 |
| Neck Pain and Disability at follow-up | |||
| Average pain intensity (0–5 VAS)b | 1.2 (1.3) | 3.4 (0.9) | 0.001 |
| Neck Pain Disability Scale | 27.1 (24.0) | 68.1 (11.4) | 0.001 |
| Difficulties “looking up and down” (0–5 VAS)c | 2.2 (1.7) | 4.1 (0.6) | 0.02 |
aSignificance of difference between the groups (“satisfied” and “dissatisfied” patients), as assessed by the global outcome question “Would you, in hindsight, make same decision to undergo the operation?”. Values in bold P<0.05
bFrom five questions in the neck pain and disability scale (see text for details)
cFrom single question in the neck pain and disability scale (see text for details)
Discussion
Pathologies that often involve the atlantoaxial segment include rheumatoid arthritis, tumour, trauma, and congenital anomalies. As shown in Fig. 1a, the appearance of massive degenerative changes may be difficult to diagnose. The possible presence of a bone tumour such as an osteoblastoma should not be overlooked, and in case of doubt a biopsy should be performed.
Despite the presence of joints that allow a wide range of motion and are constantly used for orientation and head movements, degenerative changes in the C1/C2 segment are not common. The relatively unconstrained motion, controlled only by the dens and capsulo-ligamentous structures, might contribute to the longevity of the atlantoaxial facets. Nonetheless, these joints have an anatomical architecture that is identical to that of other joints in the human body and are therefore also susceptible to degenerative change. In line with the general symptoms of osteoarthritis, the main manifestations of atlantoaxial degeneration are pain and restricted motion. The pain itself is not specific except in its localisation [27]; headache, occipital neuralgia and neck pain—often unilateral—are typical. The restriction in motion manifests itself as reduced and painful head rotation, most apparent when tested in maximum flexion. In this position, the capsulo-ligamentous structures of the subaxial cervical spine are under maximal tension and lock the facet joints of C2–C7 [7]; accordingly, a manoeuvre with passive head rotation produces rotation only in the atlantoaxial joint. In the presence of osteoarthritis of the atlantoaxial joints, the examiner often feels a dry stop that blocks head rotation to one side and produces a sharp and acute pain sensation in the suboccipital area.
This clinical test is also useful to localize the source of pain and to differentiate it from pain originating from the occipito-cervical area or the subaxial spine. Since patients with atlantoaxial arthritis are often elderly and also have generalized osteoarthritis involving the whole cervical spine, this differentiation—important as it is—can sometimes be difficult. Manifestation of radiological osteoarthritis of the subaxial spine does not necessarily result in pain [15], but can mislead the diagnostic procedure. The radiological investigation for osteoarthritis of the subaxial spine is only performed up to the segment C2/3, which can lead to further delay in identifying the true pain source [27]. If there is any doubt, diagnostic test infiltrations of facets and discs are recommended [1, 21]. Elimination or provocation of pain during these procedures may reveal a specific painful area in the subaxial spine. In our series, 17% of patients declared being dissatisfied with the results of surgery; it is possible that this group had symptoms from degenerative changes of the subaxial cervical spine that were not fully appreciated at the time of the preoperative evaluation.
For a long time, the treatment of atlantoaxial osteoarthritis was somewhat controversial; in 1987, Halla et al stated that there is no specific therapy for atlantoaxial OA [19]. Others concentrated on conservative, non-operative treatment with symptomatic pain therapy, such as steroid injections into the affected joint [4, 13]. Only after the study of Star et al [27], in which excellent results were reported for all eight patients treated surgically for painful osteoarthritis of the atlantoaxial joint, did fusion become a more popular alternative. Anterior transoral curettage of the degenerative lesions was published as an alternative by Harata et al [20]. Today, fusion of the painful joint seems to be the accepted way of treatment, although the number of reported cases remains small due to the relatively low prevalence of the disorder. To the best of our knowledge, our study with 35 patients is the largest series reported in the literature to date.
The issue regarding the safe placement of transarticular screws is still the subject of much controversy. In other series, serious complications have been reported in association with screw misplacement and consequent injury to the vertebral artery [23]. A survey amongst members of the American Association of Neurological Surgeons/Congress of Neurological Surgeons revealed that, including both known and suspected cases, the risk of vertebral artery injury was 4.1% per patient or 2.2% per screw inserted. The risk of neurological deficit from vertebral artery injury was 0.2% per patient or 0.1% per screw, and the mortality rate was 0.1% [33]. It is essential to carefully study the anatomy and dimensions of the isthmic part of the axis, as this entity is crucial for correct screw placement due to its close proximity to the vertebral artery.
Confirming previous studies [16, 26], the present series showed that solid fusion can be achieved even if only one screw is placed ideally (e.g. following the inadvertent misplacement of the screw on the opposite side) and is combined with appropriate midline bone grafting. As such, if one side is shown on preoperative CT or MRI scans to be of an inadequate shape, instrumentation of just one side may still represent an acceptable solution. Newer technologies involving computer assistance [29] or other intraoperative assistive devices [14, 24] will surely be useful for preoperative planning and safer screw placement. The absence of severe complications due to screw placement on one side only, and the generally good clinical outcome in the group as a whole, appears to support the use of transarticular screw fixation in atlantoaxial osteoarthritis.
A salient feature of the present study was the inclusion of patient-orientated outcome measures as part of the follow-up assessment. This an important issue that has not been addressed in previous studies of outcome after atlantoaxial fusion [5, 9, 16, 28] or indeed in many studies of cervical spine fusion. In the present study, the Neck Pain and Disability Scale of Wheeler et al. [30] was used, a condition-specific questionnaire that purportedly displays the best construct validity [31] and greatest sensitivity [32] of all the commonly used neck pain disability questionnaires. Using the sub-categories described by Wheeler et al [30], the degree of pain and disability reported at the long-term follow-up was equivalent to “minimal to mild” in nearly 70% of the patients. A slightly highly proportion (83%) indicated that they would make the same decision to undergo surgery if they had known then, what they know now, about the long-term outcome. As mentioned above, few patient-orientated data are available in the literature with which one can make comparisons, but the outcomes presented in the current study appear to be at least as good as, if not slightly better, than, those reported for the long-term follow-up of patients undergoing fusion of the cervical spine for neck pain (summarized in Garvey et al. [11]).
The restriction in overall head rotation as a result of C1/2 fusion was relatively marked. However, the resulting disability in everyday activities associated with such a dysfunction did not appear to be of any great significance to the patients: the range of motion in rotation (measured either clinically or indicated subjectively) was no different between the patients reporting a “good” outcome and those reporting a “poor” outcome. It seems that the restriction in rotation is perceived by the patient to be an acceptable “price to pay” for the pain relief obtained; most likely, increased trunk rotational movements compensate adequately for the reduced head rotation. Interestingly, one of the factors that appeared to be moderately associated with a poor long-term outcome was the movement limitation in the sagittal plane (both clinically-measured and self-rated). This may reflect ongoing impairment due to concomitant degenerative changes of the subaxial spine, which are then erroneously attributed to “failure” of the original surgical procedure. Overall, the most significant factor governing satisfaction with treatment was the alleviation of pain; as unremitting pain is one of the main indications for the procedure, it is fitting that this variable should manifest itself as the major determinant of a positive long-term outcome.
Conclusion
In a group of patients with a painful and debilitating degenerative disorder of C1/2, posterior transarticular atlantoaxial fusion proved to be an effective treatment with a very low rate of serious complications. The majority of patients had only mild levels of neck pain and disability at the long-term follow-up, the fusion rate was high and the patients’ self-rated outcome indicated a high degree of satisfaction with the procedure.
References
- 1.Bogduk N, Marsland A. The cervical zygapophysial joints as a source of neck pain. Spine. 1988;13:610–617. [PubMed] [Google Scholar]
- 2.Bremerich FH, Mannion AF, Baumgartner H, Grob D (2002) Transkulturelle Anpassung des “Neck Pain and Disability” Fragebogens für deutschsprachige Patienten. Jahreskongress der schweizerischen Gesellschaft für Orthopädie
- 3.Brooks AL, Jenkins EG. Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg. 1978;60-A:279–284. [PubMed] [Google Scholar]
- 4.Chevrot A, Cermakova E, Vallee C, Chancelier MD, Chemla N, Rousselin B, Langer-Cherbit A. C1-2 arthrography. Skelet Radiol. 1995;24:425–429. doi: 10.1007/BF00941238. [DOI] [PubMed] [Google Scholar]
- 5.Dickman Neurosurgery. 1998;43:275. doi: 10.1097/00006123-199808000-00056. [DOI] [PubMed] [Google Scholar]
- 6.Dvorak J, Antinnes JA, Panjabi MM, Loustalot D, Bonomo M. Age and gender related normal motion of the cervical spine. Spine. 1992;17:S393–S398. doi: 10.1097/00007632-199210001-00009. [DOI] [PubMed] [Google Scholar]
- 7.Dvorak J, Dvorak V (1991) Manuelle Medizin. 4. Auflage (Thieme Verlag, Stuttgart, New York
- 8.Ehrat C, Grob D, Dvorak J. Die posttraumatische atlantoaxiale arthrose. Der Orthopäde. 1996;25:542–545. doi: 10.1007/s001320050058. [DOI] [PubMed] [Google Scholar]
- 9.Farey ID, Nadkarni S, Smith N. Modified Gallie technique versus transarticular screw fixation in C1–C2 fusion. Clin Orthop. 1999;359:126–135. doi: 10.1097/00003086-199902000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Gallie WE. Fractures and dislocations of the cervical spine. Am J Surg. 1939;46-A:495–499. doi: 10.1016/S0002-9610(39)90309-0. [DOI] [Google Scholar]
- 11.Garvey Spine. 2002;27:1887. doi: 10.1097/00007632-200209010-00015. [DOI] [PubMed] [Google Scholar]
- 12.Gerster JC, Doenz F. Unusual destructive and hypertrophic arthropathy of the atlanto-axial joint in calcium pyrophosphate dihydrate deposition disease. Osteoarthritis Cartil. 1994;2:275–279. doi: 10.1016/s1063-4584(05)80079-2. [DOI] [PubMed] [Google Scholar]
- 13.Glemarec J, Guillot P, Laborie Y, Berthelot JM, Prost A, Maugars Y. Intraarticular glucocorticosteroid injection into the lateral atlantoaxial joint under fluoroscopic control. A retrospective comparative study in patients with mechanical and inflammatory disorders. Joint Bone Spine. 2000;67:54–61. [PubMed] [Google Scholar]
- 14.Goffin J, Van Brussel K, Martens K, Vander Sloten J, Van Audekercke R, Smet MH. Three-dimensional computed tomography-based, personalized drill guide for posterior cervical stabilization at C1–C2. Spine. 2001;15:1343–1347. doi: 10.1097/00007632-200106150-00017. [DOI] [PubMed] [Google Scholar]
- 15.Gore DR. Roentgenographic findings in the cervical spine in asymptomatic persons: a ten-year follow-up. Spine. 2001;26:2463–2466. doi: 10.1097/00007632-200111150-00013. [DOI] [PubMed] [Google Scholar]
- 16.Grob D. Surgery in the degenerative cervical spine. Spine. 1998;23:2674–2683. doi: 10.1097/00007632-199812150-00005. [DOI] [PubMed] [Google Scholar]
- 17.Grob D, Crisco J, Panjabi M, Wang P, Dvorak J. Biomechanical evaluation of four different posterior atlantoaxial fixation techniques. Spine. 1992;17:480–490. doi: 10.1097/00007632-199205000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Grob D, Magerl F. Surgical stabilization of C1 and C2 fractures. Orthopade. 1987;16:46–54. [PubMed] [Google Scholar]
- 19.Halla JT, Hardin JG., Jr Atlantoaxial (C1–C2) facet joint osteoarthritis: a distinctive clinical syndrome. Arthritis Rheum. 1987;30:577–582. doi: 10.1002/art.1780300514. [DOI] [PubMed] [Google Scholar]
- 20.Harata S, Tohno S, Kawagishi T. Osteoarthritis of the alanto-axial joint. Int Orthop. 1981;5:277–282. doi: 10.1007/BF00271083. [DOI] [PubMed] [Google Scholar]
- 21.Kikuchi S, Macnab I, Moreau P. Localisation of the level of symptomatic cervical disc degeneration. J Bone Joint Surg Br. 1981;63(B):272–277. doi: 10.1302/0301-620X.63B2.7217155. [DOI] [PubMed] [Google Scholar]
- 22.Kusakabe N, Tsuzuki N, Sonada M. Compression of the cervical cord due to alcaptonuric arthropathy of the atlanto-axial joint. A case report. J Bone Joint Surg Am. 1995;77:274–277. doi: 10.2106/00004623-199502000-00016. [DOI] [PubMed] [Google Scholar]
- 23.Madawi AA, Casey AT, Solanki GA, Tuite G, Veres R, Crockard HA. Radiological and anatomical evaluation of the atlantoaxial transarticular screw fixation technique. J Neurosurg. 1997;86:961–968. doi: 10.3171/jns.1997.86.6.0961. [DOI] [PubMed] [Google Scholar]
- 24.Neo M, Matsushita M, Yasuda T, Sakamoto T, Nakamura T. Use of an aiming device in posterior atlantoaxial transarticular screw fixation. Technical note. J Neurosurg Spine. 2002;97:123–127. doi: 10.3171/spi.2002.97.1.0123. [DOI] [PubMed] [Google Scholar]
- 25.Reilly TM, Sasso RC, Hall PV. Atlantoaxial stabilization: clinical comparison of posterior cervical wiring technique with transarticular screw fixation. J Spinal Disord Tech. 2003;16:248–253. doi: 10.1097/00024720-200306000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Song GS, Theodore N, Dickman CA, Sonntag VK. Unilateral posterior atlantoaxial transarticular screw fixation. J Neurosurg. 1997;87:851–855. doi: 10.3171/jns.1997.87.6.0851. [DOI] [PubMed] [Google Scholar]
- 27.Star MJ, Curd JG, Thorne RP. Atlantoaxial lateral mass osteoarthritis. A frequently overlooked cause of severe occipitocervical pain. Spine. 1992;17:S71–S76. [PubMed] [Google Scholar]
- 28.Suchomel P, Stulik J, Klezl Z, Chrobok J, Lukas R, Krbec M, Magerl F. [Transarticular fixation of C1-C2: a multicenter retrospective study] Acta Chir Orthop Traumatol Cech. 2004;71:6–12. [PubMed] [Google Scholar]
- 29.Weidner Spine. 2000;25:2668. doi: 10.1097/00007632-200010150-00020. [DOI] [PubMed] [Google Scholar]
- 30.Wheeler AH, Goolkasian P, Baird AC, Darden BV., II Development of the Neck Pain and Disability Scale. Item analysis, face, and criterion-related validity. Spine. 1999;24:1290–1294. doi: 10.1097/00007632-199907010-00004. [DOI] [PubMed] [Google Scholar]
- 31.Wlodyka-Demaille S, Poiraudeau S, Catanzariti JF, Rannou F, Fermanian J, Revel M. French translation and validation of 3 functional disability scales for neck pain. Arch Phys Med Rehabil. 2002;83:376–382. doi: 10.1053/apmr.2002.30623. [DOI] [PubMed] [Google Scholar]
- 32.Wlodyka-Demaille S, Poiraudeau S, Catanzariti JF, Rannou F, Fermanian J, Revel M. The ability to change of three questionnaires for neck pain. Joint Bone Spine. 2004;71:317–326. doi: 10.1016/j.jbspin.2003.04.004. [DOI] [PubMed] [Google Scholar]
- 33.Wright NM, Lauryssen C. Vertebral artery injury in C1-2 transarticular screw fixation: results of a survey of the AANS/CNS section on disorders of the spine and peripheral nerves. American Association of Neurological Surgeons/Congress of Neurological Surgeons. J Neurosurg. 1998;88:634–640. doi: 10.3171/jns.1998.88.4.0634. [DOI] [PubMed] [Google Scholar]
- 34.Zapletal J, Valois JC. Radiologic prevalence of advanced lateral C1–C2 osteoarthritis. Spine. 1997;22:2511–2513. doi: 10.1097/00007632-199711010-00009. [DOI] [PubMed] [Google Scholar]