Abstract
The main objective of the present study is to evaluate biomechanically a newly designed expansive pedicle screw (EPS) using fresh pedicles from calf lumber vertebrae in comparison with conventional pedicle screws, (CDH) CD Horizon, Universal Spine System pedicle screw (USS) and Tenor (Sofamor Denek). Pull-out and turning-back tests were performed on these pedicle screws to compare their holding strength. Additionally, revision tests were undertaken to evaluate the mechanical properties of EPS as a “rescue” revision screw. A fatigue simulation test using a perpendicular load up to 1,500,000 cycles was also carried out. The results showed that the turning back torque (Tmax) and pull-out force (Fmax) of EPS screws were significantly greater than those of USS, Tenor and CDH screws (6.5×40 mm). In revision tests, the Fmax of both types of EPS screws (6.5×40 mm; 7.0×40 mm) were significantly greater than that of CDH, USS, and Tenor screws (P<0.05). Furthermore, no screws were broken or bent at the end of fatigue tests. The findings from the current study suggest that expansive pedicle screws can significantly improve the bone purchase and the pull-out strength compared to USS, Tenor and CDH screws of similar dimensions before and after a failure simulation.
Keywords: Spine-Internal fixators, Bone screws, Biomechanics, Osteoporosis
Introduction
The transpedicular screw system pioneered by Boucher [3] has been widely used in treating degenerative disorders, unstable fractures and tumors of the spine in the past two decades [1, 6, 7, 14, 29]. However, the loosening and failure of the screws develops in cases of inadequate fixation strength of the screw or a mechanical overload of the repaired spine, especially in patients with osteoporosis [6, 8, 11, 17–19, 25], which may lead to the non-union or sagittal collapse of the construct and painful kyphosis [6], often necessitating surgical revision. Surgical remedies currently in practice include increasing the diameter and/or length of the pedicle screw [15] or, in cases of severe bone loss, filling in the void with such materials as polymethyl-methacrylate (PMMA) or calcium phosphate cement (CPC) [2, 7, 16, 20, 22, 31, 36].
These various strategies, however, have their various drawbacks such as increased risks of pedicle fracture with resultant neural injury for larger screws, or anterior body penetration with ensuing vascular or visceral injury for longer screws [13], or potential problems associated with a non-absorbable foreign body in the spinal canal [14, 27, 33]. To address these issues, several investigators have attempted to develop expansive pedicle screws that expand radially at the screw tips to render greater bone contact without a concurrent increase in the pedicle insertion diameter or screw length [23, 28]. However, little or no systemic biomechanical evaluation has been performed of these expansive pedicle screws concerning the mechanical properties that may contribute to screw purchase in the vertebral pedicles.
The principal purposes of this study were to compare the mechanical pull-out force, turning-back torque and fatigue strength of a newly designed expansive pedicle screw (EPS) with those of the conventional screws including Universal Spine System pedicle screw (USS), CD Horizon (CDH) and Tenor (Sofamor Denek) and to evaluate the mechanical properties of EPS as a “rescue” revision screw.
Materials and methods
Implant description
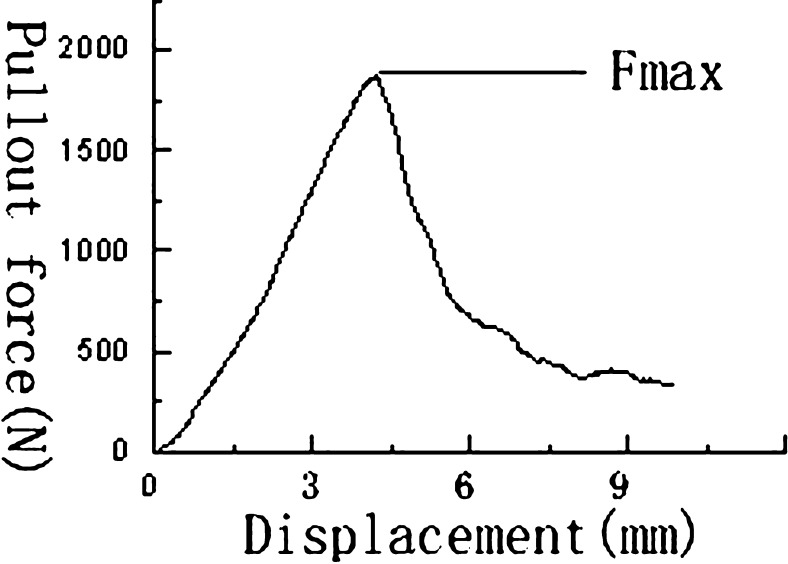
The newly designed EPS was barrel-shaped, with an outer diameter of 6.5 mm (and 7.0 mm), a 2.5-mm bore and a 3-mm pitch. The anterior half of the screw is split lengthwise by two perpendicular grooves to form four anterior fins. A smaller gauge screw is inserted into the threaded interior of EPS and opens the fins concentrically as it is advanced. This system increases the diameter of the expanding screw tip by approximately 2.5 mm (Fig. 1). The diameter of the posterior portion of the screw remains constant in order to prevent the fracture of the pedicle during the expansion of the screw. The main design features of all the screws investigated in the current study including EPS, USS and Tenor are listed in Table 1.
Fig. 1.
The structure of the EPS. No 1 is the smaller gauge screw, No 2 is the external part of the EPS and No 3 is the expanding EPS
Table 1.
The main design features of the screws tested
| Screw type | Diameter (mm) | Length of thread (mm) | Pitch (mm) |
|---|---|---|---|
| USS | 6.5 and 7.0 | 40 | 2.0 |
| CDH | 6.5 and 7.0 | 40 | 2.5 |
| Tenor | 6.5 and 7.0 | 40 | 2.5 |
| EPS | 6.5 and 7.0 | 40 | 3.0 |
Cadaveric specimens
One hundred fresh, unembalmed vertebrae were harvested from 20 calf lumbar spines. The specimens were double-bagged and frozen at −76°C within 1 h of being harvested for further use. On the day of testing, the specimens were thawed at room temperature and cleared of all soft tissue. Each vertebra was disarticulated at the intervertebral disc space and individual vertebrae were mounted in a standard bench-top vise to provide specimen stability during pedicle screw hole preparation. All the procedures involving animal use conform to the ethics guidelines established by the Xijing Hospital.
Bone mineral density (BMD)
For the determination of the quality and density of the bones within the vertebral body, the vertebral BMD was measured using a dual energy X-ray absorption meter (Lunar Corp., Madison, WI, U.S.A.) and reported in g/cm2. Lateral scans were taken after each vertebra was isolated and labeled.
Screw placement technique
The pedicle screws were inserted into the lumbar pedicles using surgical techniques and instruments specifically designed for EPS. Extra care was taken to avoid the penetration of the anterior cortex. All the pedicles were drilled manually using a 5.0-mm drill bit. After the insertion of EPS, a conus is screwed in the central hole to provide the expansion for EPS. Plain radiographs were obtained to verify correct screw placement and measure the diameters of the EPS tip. Each vertebra received one control screw in one pedicle and one EPS in the contralateral pedicle. After the pullout of EPS, the diameters of the EPS tips were re-measured by a Vernier caliper.
Grouping
One hundred fresh calf lumber vertebrae with a total of 200 pedicles were harvested from 20 calf lumber spine and randomized into 12 groups with 20 pedicles each in group A1, A2, A3, B1, B2, B3, C5 and C6 and 10 pedicles each in group C1, C2, C3 and C4 (Table 2). Turning back tests were performed in group A1–A3. Axial pull-out tests of non-salvage screws were performed in group B1–B3 and axial pull-out tests of salvage screws were performed in group C1–C3.
Table 2.
The biomechanical tests performed in each experimental group
| Tests performed | Group | Pedicles | Screw type |
|---|---|---|---|
| Turning-back test | A1 | 20 | EPS vs USS |
| A2 | 20 | EPS vs Tenor | |
| A3 | 20 | EPS vs CDH | |
| Pull-out test | B1 | 20 | EPS vs USS |
| B2 | 20 | EPS vs Tenor | |
| B3 | 20 | EPS vs CDH | |
| Revision test (6.5×40 mm) | C1 | 10 | CDH |
| C2 | 10 | USS | |
| C3 | 10 | Tenor | |
| C4 | 10 | EPS | |
| Revision test (7.0×40 mm) | C5 | 20 | EPS vs CDH |
| C6 | 20 | EPS vs USS |
Turning-back tests
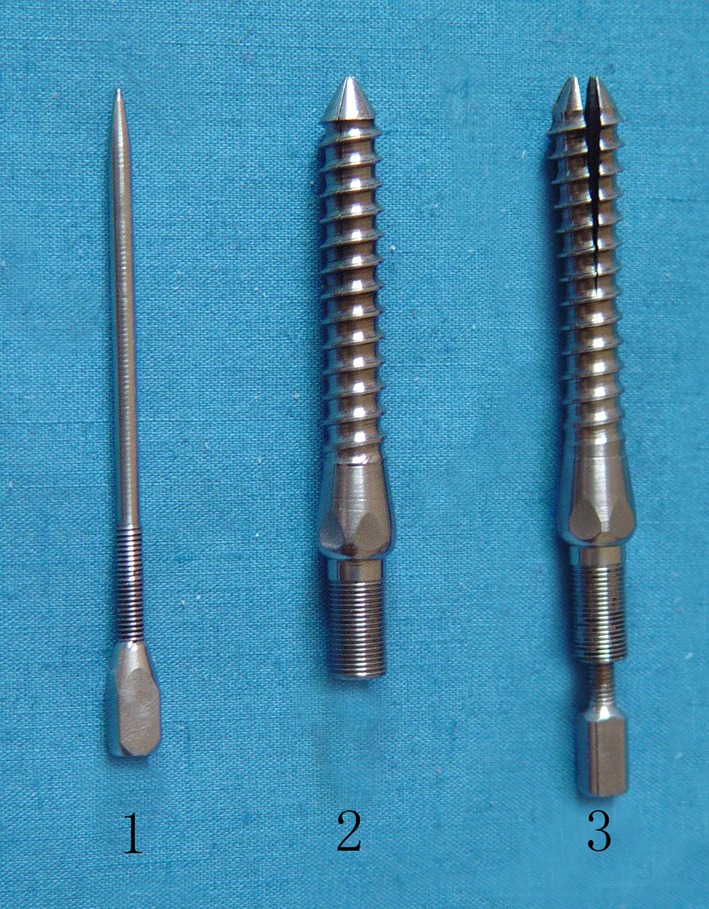
Turning-back tests were performed in group A1, A2 and A3. The vertebra and pedicle screw unit was placed in a custom jig. The specimens were placed in a material test machine (MTS 858 System Inc., Minneapolis, USA), which was vertically aligned along the screw axis (Fig. 2). The free end of the screw was attached by a hydraulic grip to the testing machine. Each screw was turned back from the pedicle at a constant angular velocity of 240°/min until purchase failure, which is defined as the maximum torque reached before the load decreased abruptly.
Fig. 2.

Screw axial pullout test. The pull-out force is coaxial with the screw
Pull-out tests
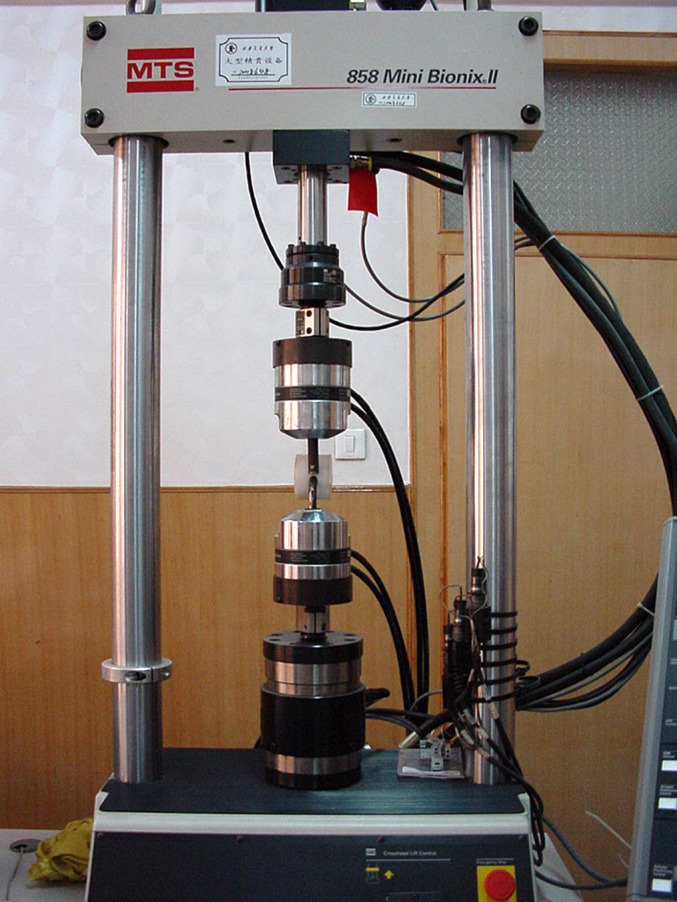
Axial pull-out tests were conducted in group B1, B2 and B3. After the removal of the posterior elements, the vertebra and pedicle screw unit was placed in the jig. Through a hole in the top plate of the jig adjacent to the vertebral body, a straight axial pull-out force was applied using the MTS 858. Each screw was extracted from the pedicle at a constant rate of 18 mm/min until purchase failure, which is defined as the maximum pull-out strength reached before the load decreased abruptly (Fig. 3).
Fig. 3.
Loading-displacement curve for pedicle screw obtained during pull-out test
Revision tests
Revision tests were performed in group C1, C2, C3 and C4. CDH, USS, Tenor, and EPS screws (6.5×40 mm) were of the same diameter and length (6.5×40 mm) and were inserted into group C1, C2, C3 and C4, respectively. The screws were subsequently pulled out to simulate screw failures and CDH, USS, Tenor or EPS screws were re-inserted into the holes as salvage screws. In group C5 and C6, the above screws were inserted into the pedicles. After the pull-out of the screws to simulate screw failures, EPS screws were inserted into one side of the vertebrae while CDH or USS screws were inserted into the other side of the vertebrae.
Fatigue tests
Ultrahigh molecular weight polyethylene (UHMWP) blocks were used as vertebral elements and each block was precisely prepared to enable the symmetrical placement of pedicle screws and iron rods (Fig. 4). Cyclic compressive loading was performed at 200–250 N with a frequency of 5 Hz until the development of implant failures or 1.5 million cycles. The implant failure was defined as breakage of the screw or displacement of bending more than 5 mm.
Fig. 4.
Fatigue test. Cyclic compressive loading was performed vertically aligned along the screw axis
Statistical analysis
Statistical comparisons were carried out using SPSS 10.0. Descriptive statistics were calculated for the entire population and each subset of screw type. First, the data was screened to detect outliers. The Student-Newman-Keuls multiple-range tests were used to compare subgroup means. Paired t tests were also performed to further evaluate the effect of screw design on the turning-back torque and pull-out force. One-way analysis of variance (ANOVA) was performed to examine the effect of the revision screws. The effect of BMD on the pull-out force was determined based on linear regression with stepwise analysis of variance and the partial F test. The coefficients for the regression line were also calculated.
Results
The diameters of EPS tips measured by radiographs ranged from 1.5 to 2.5 mm with a mean of 1.6 mm. After the pull-out of EPS, the diameters ranged from 1.8 to 2.5 mm with a mean of 2.1 mm. The vertebral BMD ranged from 1.341 to 2.634 (mean, 1.822; SD, 0.385) and no significant differences in BMD were observed among the experimental subgroups based on a one-way analysis of variance (P >0.05). The turning-back torque was significantly higher in EPS than that in the other three types of pedicle screws (Table 3).
Table 3.
Average bone mineral density (BMD) and turning-back torque (Tmax) for the screws 6.5×40 mm 
| Group | Type | Tmax, Nm (SD) | BMD, g/cm2 (SD) | P |
|---|---|---|---|---|
| A1 | EPS | 3.355±0.908 | 1.684±0.426 | 0.001 |
| USS | 1.606±0.300 | |||
| A2 | EPS | 3.569±1.054 | 1.734±0.454 | 0.001 |
| Tenor | 2.258±0.374 | |||
| A3 | EPS | 3.785±0.810 | 1.768±0.462 | 0.002 |
| CDH | 2.371±0.348 |
Furthermore, the highest pull-out strength was seen in EPS, which is consistent with the findings in other studies (Tables 4, 5). The mean pull-out force was calculated for each subgroup and the results showed that EPS improved the pull-out force by 137, 143 and 134% over USS, Tenor and CDH, respectively (Table 4). Paired t tests and ANOVA analysis of Tmax and Fmax in EPS and USS, EPS and Tenor, and EPS vs CDH revealed no statistically significant difference on Tmax between the Tenor group and CDH group (P=0.466). However, the Tmax of Tenor and CDH were significantly larger than that of USS. Furthermore, no statistically significant difference in Fmax was observed among the Tenor, CDH and USS (P=0.810).
Table 4.
Average bone mineral density (BMD) and pull-out force for the screws 6.5×40 mm 
| Group | Type | Fmax, N(SD) | BMD, g/cm2 (SD) | P |
|---|---|---|---|---|
| B1 | EPS | 2 872.7±855.9 | 2.219±0.566 | 0.001 |
| USS | 1 929.9±484.9 | |||
| B2 | EPS | 2 604.6±946.3 | 2.009±0.380 | 0.005 |
| Tenor | 1 849.8±575.9 | |||
| B3 | EPS | 2 480.0±637.2 | 1.979±0.242 | 0.008 |
| CDH | 1 980.9±836.4 |
Table 5.
The initial and salvage pull-out force of screws 6.5×40 mm 
| Group | Type | Initial Fmax, N(SD) | Salvage Fmax, N(SD) | BMD, g/cm2 | Decrease |
|---|---|---|---|---|---|
| C1 | CDH | 2 563±923.5 | 431±229.6 | 1.884±0.171 | 83.1% |
| C2 | USS | 1 549±509.5 | 329±168.8 | 1.605±0.208 | 79.8% |
| C3 | Tenor | 2 702±609.6 | 538±198.9 | 1.583±0.137 | 80.1% |
| C4 | EPS | 960±559.3 | 1.731±0.212 |
Although we found no significant differences in BMD among the subgroups, we noted a significant linear correlation between pull-out strength and vertebral body bone mineral density for all 30 EPS screws (r= 0.344; P =0.032). The average pull-out force in both revision tests was significantly greater for the EPS screw fixation than the control screw fixation (P < 0.01) (Tables 5, 6). However, there was no significant difference in the pull-out force for the control screws (P>0.05).
Table 6.
Salvage pull-out force of screws 7.0×40 mm 
| Group | Type | Salvage Fmax, N(SD) | BMD, g/cm2 (SD) | P |
|---|---|---|---|---|
| C5 | CDH | 1 207±597.4 | 1.826±0.337 | 0.018 |
| EPS | 2 183±316.7 | |||
| C6 | USS | 1 522±392.1 | 1.597±0.416 | 0.029 |
| EPS | 2 140±759.7 |
The results from the fatigue tests demonstrated no failures in the control screws or EPS occurred after 1,500,000 cycles with a system fatigue strength at 1.5 million cycles of 200–250 N, which was identical to that determined for the 6.5-mm control screws. There was no predisposition to failure of the expansive screw or anterior fins.
Discussion
The use of pedicle screws in lumbar spine fixation has been well accepted. Pedicle screw fixations depend on the abilities of pedicle screws to retain the bone purchase until the fusion mass is stable. Osteoporosis has been identified as an important factor in poor screw fixation and subsequent screw loosening and fixation failure [4, 6, 9, 19, 25]. Similarly, the removal and replacement of a pedicle screw in a revision procedure substantially decreases the mechanical fixation strength of the screw [20, 21, 36]. Furthermore, the turning back of the screws becomes necessary when surgeons cannot successfully insert screws into the proper position during the first attempt, which reduces the holding strength [12].
In the present study, fresh calf spines, which are regarded as a reasonable substitute for human spines in biomechanical testing [5, 24, 32] because of their geometric properties and BMD comparable to those of humans [26, 30, 35], were employed for biomechanical evaluation of a newly designed pedicle screw EPS. The findings from the current study demonstrate that the mean pull-out force and turn-back torque are higher in EPS than those in the control screws. Pedicle screws with larger diameters have been shown to provide greater holding strength [10, 34]. Our results indicated that, with an increase of 2.1 mm in the diameter of EPS, the pull-out force in EPS increased by 48.8, 40.8 and 25.3% more than that of USS, Tenor and CDH screws, respectively, with a mean of 38.3%. Moreover, the results from the pull-out tests showed a positive correlation between the pull-out force and BMD (P<0.05). The pull-out force (2924.3±713.1 N) in the high BMD group (2.3±0.211 g/cm2) was significantly greater than that (2189.3±136.7 N) in the low BMD group (1.706±0.207 g/cm2). In the salvage of the 6.5-mm screw sites with 6.5-mm screws, the pull-out force for EPS was significantly larger than that of the control screws: USS, CDH and Tenor (P=0.002, 0.001, and 0.013, respectively). Likewise, using bigger salvage screws, the pull-out force for EPS was greater than that for USS and CDH screws (P=0.018, 0.029, respectively). In addition, the results of fatigue testing indicated that there was no predisposition to failure of EPS. These biomechanical findings suggest that EPS is ideal in problematic situations where the bone integrity is compromised by either osteoporosis or pedicle screw revision by providing biomechanical parameters similar to those expected for normal bone and in primary surgery. However, as calf spines have a greater pedicle diameter and a higher BMD, further biomechanical evaluation of EPS is needed in human vertebral bodies.
Conclusion
In summary, the use of an expansive screw design significantly improved the biomechanical fixation strength of the screw compared with conventional pedicle screws. The expansive screw design can reduce the risk of pedicle penetration in situations of compromised bone integrity caused by osteoporosis or pedicle screw revision.
Acknowledgements
The authors express their thanks to Dr. Bo Cui, Department of Surgery, Duke University Medical Center, Durham, North Carolina, USA for his assistance in the preparation of this manuscript.
References
- 1.Abumi K, Kaneda K. Pedicle screw fixation for nontraumatic lesions of the cervical spine. Spine. 1997;22(16):1853–1863. doi: 10.1097/00007632-199708150-00010. [DOI] [PubMed] [Google Scholar]
- 2.Bai B, Kummer FJ, Spivak J. Augmentation of anterior vertebral body screw fixation by an injectable, biodegradable calcium phosphate bone substitute. Spine. 2001;26(24):2679–2683. doi: 10.1097/00007632-200112150-00009. [DOI] [PubMed] [Google Scholar]
- 3.Boucher HH. A method of spinal fusion. J Bone Joint Surg Am. 1959;41:248–259. doi: 10.1302/0301-620X.41B2.248. [DOI] [PubMed] [Google Scholar]
- 4.Coe JD, Warden KE, Herzig MA, McAfee PC. Influence of bone mineral density on the fixation of thoracolumbar implants: a comparative study of transpedicular screws, laminar hooks, and spinous process wires. Spine. 1997;9:902–907. doi: 10.1097/00007632-199009000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Cotterill PC, Kostuik JP, D’Angelo G, Fernie GR, Maki BE. An anatomical comparison of the human and bovine thoracolumbar spine. J Orthop Res. 1986;4:298–303. doi: 10.1002/jor.1100040306. [DOI] [PubMed] [Google Scholar]
- 6.Faraj AA, Webb JK. Early complications of spinal pedicle screw. Eur Spine J. 1997;6(5):324–326. doi: 10.1007/BF01142678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gaines RW., Jr The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am. 2000;82-A(10):1458–1476. doi: 10.2106/00004623-200010000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Glaser J, Stanley M, Sayre H, Woody J, Found E, Spratt K. A 10-year follow-up evaluation of lumbar spine fusion with pedicle screw fixation. Spine. 2003;28(13):1390–1395. doi: 10.1097/00007632-200307010-00008. [DOI] [PubMed] [Google Scholar]
- 9.Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS, III, Cook SD. Effects of bone mineral density on pedicle screw fixation. Spine. 1994;19(21):2415–2420. doi: 10.1097/00007632-199411000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Krag MH, Beynnon BD, Pope MH, Frymoyer JW, Haugh LD, Weaver DL. An internal fixator for posterior application to short segments of the thoracic, lumbar, or lumbosacral spine. Design and testing. Clin Orthop. 1986;203:75–98. [PubMed] [Google Scholar]
- 11.Law M, Tencer AF, Anderson PA. Caudo-cephalad loading of pedicle screws: mechanisms of losing and methods of augmentation. Spine. 1993;18:2438–2443. doi: 10.1097/00007632-199312000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Lill CA, Schlegel U, Wahl D, Schneider E. Comparison of the in vitro holding strengths of conical and cylindrical pedicle screws in a fully inserted setting and backed out 180°. J Spinal Disord. 2000;13(3):259–266. doi: 10.1097/00002517-200006000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Lonstein JE, Denis F, Perra JH, Pinto MR, Smith MD, Winter RB. Complications associated with pedicle screws. J Bone Joint Surg Am. 1999;81-A(11):1519–1528. doi: 10.2106/00004623-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Lotz JC, Hu SS, Chiu DF, Yu M, Colliou O, Poser RD. Carbonated apatite cement augmentation of pedicle screw fixation in the lumbar spine. Spine. 1997;22(23):2716–2723. doi: 10.1097/00007632-199712010-00003. [DOI] [PubMed] [Google Scholar]
- 15.McLain RF, Fry MF, Moseley TA, Sharkey NA. Lumbar pedicle screw salvage: pullout testing of three different pedicle screw designs. J Spinal Disord. 1995;8(1):62–68. [PubMed] [Google Scholar]
- 16.Moore DC, Maitra RS, Farjo LA, Graziano GP, Goldstein SA. Restoration of pedicle screw fixation with an in situ setting calcium phosphate cement. Spine. 1997;22(15):1696–1705. doi: 10.1097/00007632-199708010-00003. [DOI] [PubMed] [Google Scholar]
- 17.Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K. Influence of bone mineral density on pedicle screw fixation: a study of pedicle screw fixation augmenting posterior lumbar interbody fusion in elderly patients. Spine. 2001;1(6):402–407. doi: 10.1016/S1529-9430(01)00078-X. [DOI] [PubMed] [Google Scholar]
- 18.Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K. Can insertional torque predict screw loosening and related failures? An in vivo study of pedicle screw fixation augmenting posterior lumbar interbody fusion. Spine. 2000;18(15):858–864. doi: 10.1097/00007632-200004010-00015. [DOI] [PubMed] [Google Scholar]
- 19.Okuyama K, Sato K, Abe E, Inaba H, Shimada Y, Murai H. Stability of transpedicle screwing for the osteoporotic spine. An in vitro study of the mechanical stability. Spine. 1993;18(15):2240–2245. doi: 10.1097/00007632-199311000-00016. [DOI] [PubMed] [Google Scholar]
- 20.Pfeifer BA, Krag MH, Johnson C. Repair of failed transpedicle screw fixation. A biomechanical study comparing polymethylmethacrylate, milled bone, and matchstick bone reconstruction . Spine. 1994;19(3):350–353. doi: 10.1097/00007632-199402000-00017. [DOI] [PubMed] [Google Scholar]
- 21.Polly DW, Orchowski JR, Ellenbogen RG. Revision pedicle screws: bigger, longer shims—what is best? Spine. 1998;12:1374–1375. doi: 10.1097/00007632-199806150-00015. [DOI] [PubMed] [Google Scholar]
- 22.Renner SM, Lim TH, Kim WJ, Katolik L, An HS, Andersson GB. Augmentation of pedicle screw fixation strength using an injectable calcium phosphate cement as a function of injection timing and method. Spine. 2004;29(11):212–216. doi: 10.1097/00007632-200406010-00020. [DOI] [PubMed] [Google Scholar]
- 23.Richter M, Wilke HJ, Kluger P, Claes L, Puhl W. Biomechanical evaluation of a newly developed monocortical expansion screw for use in anterior internal fixation of the cervical spine: in vitro comparison with two established internal fixation systems. Spine. 1999;24(3):207–212. doi: 10.1097/00007632-199902010-00002. [DOI] [PubMed] [Google Scholar]
- 24.Riley LH, III, Eck JC, Yoshida H, Koh YD, You JW, Lim TH. A biomechanical comparison of calf versus cadaver lumbar spine models. Spine. 2004;29(11):E217–E220. doi: 10.1097/00007632-200406010-00021. [DOI] [PubMed] [Google Scholar]
- 25.Sarzier JS, Evans AJ, Cahill DW. Increased pedicle screw pullout strength with vertebroplasty augmentation in osteoporotic spines. J Neurosurg. 2002;96(3 Suppl):309–312. doi: 10.3171/spi.2002.96.3.0309. [DOI] [PubMed] [Google Scholar]
- 26.Skinner R, Maybee J, Transfeldt E, Venter R, Chalmers W. Experimental pullout testing and comparison of variables in transpedicular screw fixation. A biomechanical study. Spine. 1990;15:195–201. doi: 10.1097/00007632-199003000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Soshi S, Shiba S, Knodo H, Murota K. An experimental study on transpedicular screw fixation in relation to osteoporosis of the lumbar spine. Spine. 1991;16:1335–1341. doi: 10.1097/00007632-199111000-00015. [DOI] [PubMed] [Google Scholar]
- 28.Stephen DC, Salkeld SL, Whitecloud TS, III, Barbera J. Biomechanical evaluation and preliminary clinical experience with an expansive pedicle screw design. J Spinal Disord. 2000;13(3):230–236. doi: 10.1097/00002517-200006000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Suk SI, Kim WJ, Lee SM, Kim JH, Chung ER. Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine. 2001;26(18):2049–2057. doi: 10.1097/00007632-200109150-00022. [DOI] [PubMed] [Google Scholar]
- 30.Swartz DE, Wittenberg RH, Shea M, White AA, Hayes WC. Physical and mechanical properties of calf lumbosacral trabecular bone. J Biomech. 1991;24:1059–1068. doi: 10.1016/0021-9290(91)90022-F. [DOI] [PubMed] [Google Scholar]
- 31.Taniwaki Y, Takemasa R, Tani T, Mizobuchi H, Yamamoto H. Enhancement of pedicle screw stability using calcium phosphate cement in osteoporotic vertebrae: in vivo biomechanical study. J Orthop Sci. 2003;8(3):408–414. doi: 10.1007/s10776-003-0639-6. [DOI] [PubMed] [Google Scholar]
- 32.Wilke HJ, Krischak S, Claes L. Biomechanical comparison of calf and human spines. J Orthop Res. 1996;14(3):500–503. doi: 10.1002/jor.1100140321. [DOI] [PubMed] [Google Scholar]
- 33.Wilkes RA, Mackinnon J, Thomas W. Neurologic deterioration after cement injection into a vertebral body. J Bone Joint Surg Br. 1994;76:155. [PubMed] [Google Scholar]
- 34.Wittenberg RH, Lee KS, Shea M, White AA, III, Hayes WC. Effect of screw diameter, insertion technique, and bone cement augmentation of pedicular screw fixation strength. Clin Orthop. 1993;296:278–287. [PubMed] [Google Scholar]
- 35.Wittenberg RH, Shea M, Swartz DE, Lee KS, White AA, III, Hayes WC. Importance of bone mineral density in instrumented spine fusions. Spine. 1991;16:647–652. doi: 10.1097/00007632-199106000-00009. [DOI] [PubMed] [Google Scholar]
- 36.Yerby SA, Toh E, McLain RF. Revision of failed pedicle screws using hydroxyapatite cement. A biomechanical analysis. Spine. 1998;23(15):1657–1661. doi: 10.1097/00007632-199808010-00008. [DOI] [PubMed] [Google Scholar]