Abstract
Today, posterior stabilization of the cervical spine is most frequently performed by lateral mass screws or spinous process wiring. These techniques do not always provide sufficient stability, and anterior fusion procedures are added secondarily. Recently, transpedicular screw fixation of the cervical spine has been introduced to provide a one-stage stable posterior fixation. The aim of the present prospective study is to examine if cervical pedicle screw fixation can be done by low risk and to identify potential risk factors associated with this technique. All patients stabilized by cervical transpedicular screw fixation between 1999 and 2002 were included. Cervical disorders included multisegmental degenerative instability with cervical myelopathy in 16 patients, segmental instability caused by rheumatoid arthritis in three, trauma in five and instability caused by infection in two patients. In most cases additional decompression of the spinal cord and bone graft placement were performed. Pre-operative and post-operative CT-scans (2-mm cuts) and plain X-rays served to determine changes in alignment and the position of the screws. Clinical outcome was assessed in all cases. Ninety-four cervical pedicle screws were implanted in 26 patients, most frequently at the C3 (26 screws) and C4 levels (19 screws). Radiologically 66 screws (70%) were placed correctly (maximal breach 1 mm) whereas 20 screws (21%) were misplaced with reduction of mechanical strength, slight narrowing of the vertebral artery canal (<25%) or the lateral recess without compression of neural structures. However, these misplacements were asymptomatic in all cases. Another eight screws (9%) had a critical breach. Four of them showed a narrowing of the vertebral artery canal of more then 25%, in all cases without vascular problems. Three screws passed through the intervertebral foramen, causing temporary paresis in one case and a new sensory loss in another. In the latter patient revision surgery was performed. The screw was loosened and had to be corrected. The only statistically significant risk factor was the level of surgery: all critical breaches were seen from C3 to C5. Percutaneous application of the screws reduced the risk for misplacement, although this finding was not statistically significant. There was also a remarkable learning curve. Instrumentation with cervical transpedicular screws results in very stable fixation. However, with the use of new techniques like percutaneous screw application or computerized image guidance there remains a risk for damaging nerve roots or the vertebral artery. This technique should be reserved for highly selected patients with clear indications and to highly experienced spine surgeons.
Keywords: Cervical spine, Pedicle screw fixation, Complication, Posterior fusion
Introduction
Cervical spine fixation by pedicle screws is a established technique for C2 and C7 [7, 16]. Radiological and anatomical investigations have shown that the pedicles of C3 to C6 are frequently small. It is therefore difficult to place transpedicular screws at these levels without cortical violation [6, 8–12, 14, 17, 18]. Therefore it has been recommended to perform stabilization of this region via the ventral approach. In cases of major instability it may be necessary to combine the ventral stabilization with a dorsal instrumentation such as sublaminar wiring, spinous process wiring or lateral mass screws [4, 20]. If the dominant pathology is situated dorsal to the spinal cord, decompression and bone onlay by a posterior approach alone may be appropriate. However, especially a short distance posterior stabilization is not considered sufficiently stable [5, 13]. Solving this dilemma requires additional anterior stabilization or multi-level posterior fixation with reduction of cervical spine mobility. Both solutions are not ideal.
The recent literature describes the use of transpedicular screws in all cervical segments [1–3, 8]. Pedicle screws in the cervical spine have been shown to have significantly higher pullout strength and higher primary stability than lateral mass screws [10, 15]. With the use of pedicle screws it is possible to create sufficient short distance dorsal instrumentation and fusion without the need for ventral stabilization. The advantage is twofold: it is a one-stage procedure and leads to minimal reductionof cervical spine mobility. This concept is well established for the lumbar and thoracic spine.
Abumi et al. [1] stated that the use of pedicle screws in the cervical spine is not as risky as has been thought before. They reported successful insertion of cervical pedicle screws in a large number of patients with low risk.
The purpose of this prospective study is to evaluate the risk of placing cervical pedicle screws with the aid of computerized imaged guidance and newly developed implants.
Materials and methods
From July 1999 to October 2002, 26 patients who needed cervical, occipitocervical or cervicothoracic stabilization, were treated with transpedicular screw fixation. One occipitocervical fusion (C0–C3) was performed, the other cases were stabilization procedures of the subaxial cervical spine including five cases of cervicothoracal fusion and two cases with transarticular C1/C2 fusion. The number of instrumented levels ranged from 0 in two cases (C2-fractures) to 7 (C1 to Th1 in rheumatoid arthritis) with a mean number of 3.
Cervical disorders included multisegmental degenerative instability with cervical myelopathy in 16 patients (61%), segmental instability caused by rheumatoid arthritis in three cases (12%), trauma in five patients (19%) and instability caused by infection in two patients (8%). There were 17 males and 9 females. Mean age at surgery was 60 years (range 31–86 years, standard deviation 14 years).
Presurgical management
All patients underwent a CT scan of the cervical spine to depict the exact anatomy of the cervical vertebrae and pedicles and a MRI for exact planning of decompression and stabilization. All patients except the trauma patients were examined with standard functional X-rays (inclination and reclination). Prior to surgery, the patients were evaluated clinically for the neurologic status and for pain.
Because the inherent risk to violate the vertebral artery during surgery, all patient were angiologically tested before surgery by duplex sonography [19]. In cases of vertebral artery hypoplasia or relevant stenosis no pedicle screws were used to avoid vertebrobasilar ischaemia and concurrent stroke.
Surgical management
Nineteen patients were operated upon in the sitting position, and seven in the prone position. Because of the risk of air embolism in the sitting position, all patients were tested for a patent foramen ovale. If the test was positive, surgery was done in the prone position.
A dorsal median approach was utilized in all cases. Lateral fluoroscopy was mandatory during the entire procedure. For screw positioning anatomical landmarks were used. We used computerized image guidance in 18 patients to optimize screw placement. In the remaining procedures no system was available or there were technical problems. From 1999 to 2000 we used the STN 4.0 System (Zeiss Company, Oberkochen Germany), and since 2001 the Vectorvision System (BrainLAB Company, Heimstetten, Germany). The STN-system is a CT-based navigation system including the possibility of surface matching for registration. For this system, no suitable tool adaptor for a drilling machine is available. So we used mainly a pointer for navigation. The Vectorvision System is also CT-based. Furthermore there is an image-fusion with fluoroscopic images possible. But, for the use in cervical spine this technique is too inaccurate. So we used surface-matching for registration in all procedures. A tool adaptor for the Neon cervical system allows here drilling under control of real time computer navigation.
In the first 11 patients, the Cervifix system with non-cannulated 3.5-mm screws (Stratec Medical, Oberdorf, Switzerland) was implanted. This system is not developed for cervical pedicle screws and is not angle stable [15]. The system can be combined with transarticular screws for C1/C2, occiput plates for occipitocervical fusion and with thoracic pedicle screws and hooks via a connector to a 6-mm rod.
In all other patients the newly developed Neon cervical system (Ulrich Co., Ulm, Germany) for cervical pedicle screws was used with cannulated 4.0-mm screws and an angle stable instrumentation [15]. This system includes also lateral mass screws, transarticular screws for C1/C2, different occiput plates and an connector for thoracic instrumentation. Figure 1 shows an example of a stabilization with the Neon cervical system from C4 to Th1.
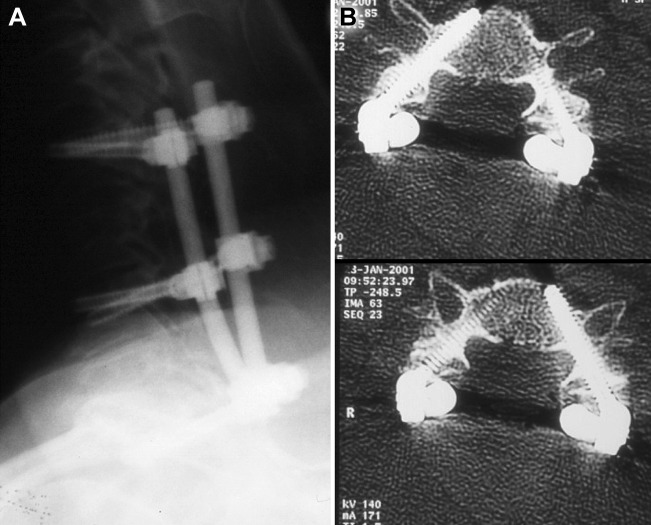
Fig. 1.
Stabilization with the Neon cervical system from C4 to Th1. A Lateral X-ray and B screw position in C4
A technical problem for pedicle screw implantation in the cervical spine is the marked convergence of the screws which ranges from 30° to 50° [9, 14, 18]. Therefore a wide lateral approach is needed for optimal screw insertion. To minimize neck muscle dissection, we developed a trokar system for percutaneous application of the screws with the Neon device (Fig. 2a, b). This can be used in combination with image guidance (Fig. 3). Our last seven procedures were carried out with this Neon trokar system.
Fig. 2.
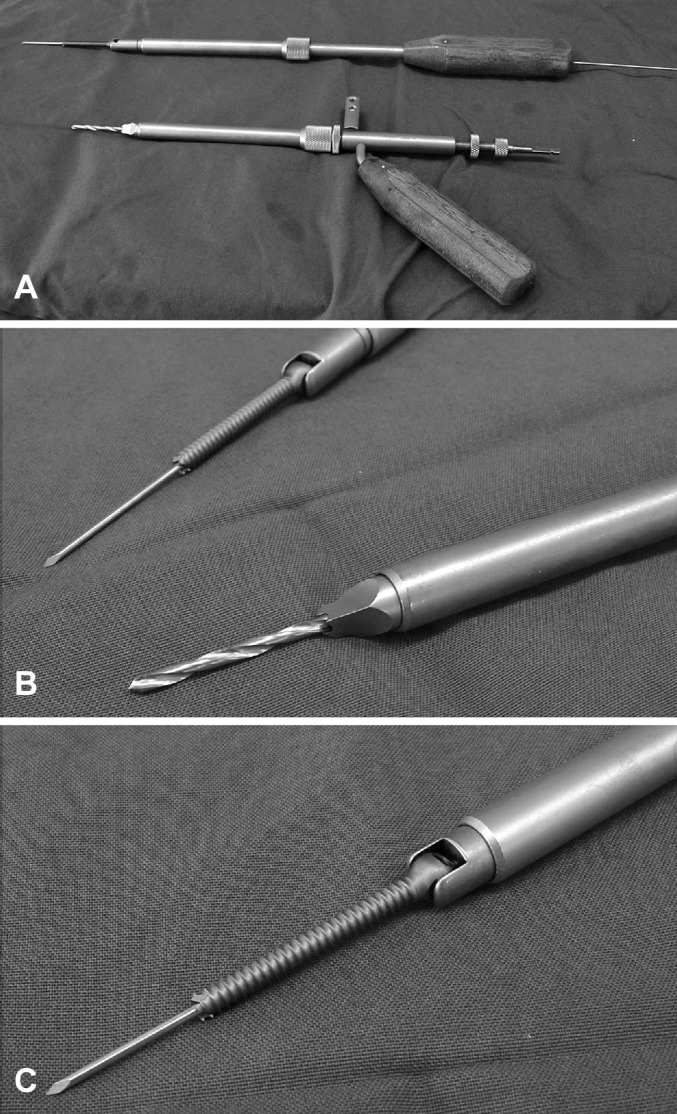
The Neon cervical system with use of trokar application for percutaneous screw insertion (A). First a drill (2.3-mm) is used for pediculation (B), than a k-wire is put into the drill hole, and a self-tapping cannular screw is inserted (C)
Fig. 3.

The navigated use of the Neon trokar system during pediculation with a drill
In all procedures except the two patients with C2 fractures who got only C2 pedicle screws according to Judet et al. [7], bone onlay in the facet joints was done. For this, we harvested bone chips during the decompression. Only in the case of occipitocervical fusion we used additional corticospongious bone from the iliac crest.
The 94 cervical transpedicular screws were combined with an occiput plate in one patient, with 33 lateral mass screws, with 5 transarticular screws in C1/C2 and with 12 thoracic transpedicular screws.
Postoperative management
After surgery all patients underwent a.p. and lateral X-rays and CT scans to determine the quality of decompression, the screw positions and the spinal alignment. Pain status and neurological findings were documented as well. All patients were mobilized the day after surgery. The trauma patients were mobilized in a semirigid collar for the first six weeks.
Follow up
Patients were re-examined clinically and radiologically (a.p. and lateral standard radiography) six weeks and three month after surgery. Finally, after one year the degree of bony fusion was controlled by X-ray examination and/or CT scans.
Results
Complications directly attributable to surgery
During surgery slippage of the drill caused in one patient a dural tear, without lesion of neural structures. The defect was closed with fibrin glue. There was no lesion of the vertebral artery or relevant air embolisms during surgery.
One patient had a temporary weakness of the deltoid muscle after surgery. Postoperative CT scan showed a screw misplacement at C4 with caudal pedicle perforation (Fig. 4). Complete recovery occurred following treatment with dexamethasone. The screw did not need to be corrected surgically.
Fig. 4.
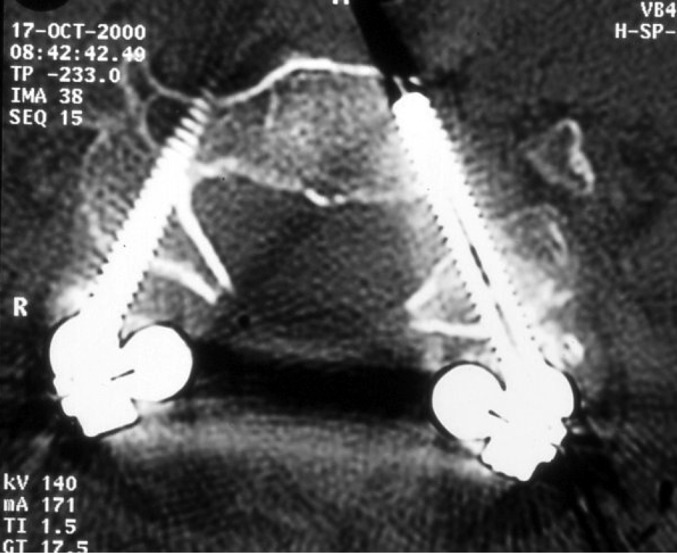
Patient with screw displacement C4 with caudal pedicle perforation and clinical symptoms (left screw) and narrowing of the vertebral channel more than 25% (right screw): both are major breaches
Another patient with severe cervical myelopathy developed a new sensory loss in the hand. CT examination also revealed a screw misplacement at C4 with caudal pedicle perforation. Even though the dermatome of sensory loss did not correspond to the distribution of C5, revision surgery was done, because there was no other reason found for this new deficit. During revision surgery it was found that the screw in C4 was loosened and it was replaced transpedicularly. Symptoms resolved only incompletely during follow-up. No other patient deteriorated postoperatively. There was no infection, and during follow up there was no implant failure and no pseudarthrosis. Summarizing, 2 of 26 patients (8%) showed clinical signs directly attributable to surgery and revision surgery was indicated in one of them.
Radiological assessment of screw placement
All patients underwent a high resolution CT of the instrumented levels after surgery. Based on these examinations, correct placement of the 94 transpedicular screws was assessed. We defined three categories for quality of placement:
Correct screw position
Screws either completely within the cortical walls of the pedicle (46 screws) or with a cortical perforation of maximal 1 mm as seen on CT (20 screws). This group comprised 66 screws (70%) of implanted pedicle screws (Table 1).
Table 1.
Radiological assessment of cervical pedicle screw placement (94 screws)
| Correct position: 66 screws=70% | |
|---|---|
| Screw completely within cortical walls of the pedicle | 46 screws |
| Cortical perforation maximum of 1 mm in CT | 20 screws |
| Minor breach: 20 screws=21% | |
|---|---|
| Lateral or ventral perforation of the vertebral body | 5 screws |
| Slightly affecting the lateral recess without dural contact | 10 screws |
| Narrowing of the vertebral channel less than 25% | 5 screws |
| Major breach: 8 screws=9% | |
|---|---|
| Medial perforation of the pedicle with dural tear | 0 screws |
| Medial perforation with radicular/medullar compression | 0 screws |
| Caudal perforation with potential nerve root injury | 3 screws |
| Narrowing of the vertebral channel more than 25% | 5 screws |
Minor breach
Lateral or ventral perforation of the vertebral body (5 screws) or slight affection of the lateral recess without dural contact (10 screws) or narrowing of the vertebral artery canal less than 25% of its diameter (5 screws).
Summarizing, 20 screws or 21% of all screws showed a minor breach radiologically (Table 1).
Major breach
Encroachment of the vertebral artery canal of more than 25% (five screws; levels: one screw C3, two screws in C4 and C5 each) or caudal perforation of the pedicle with potential nerve root compression or injury (three screws; levels: one in C3 and two screws in C4). Further possibilities of major breaches like medial pedicle perforation with dural laceration and risk of radicular or medullar compression or injury were not observed in this series.
The group of major breaches comprises eight (9%) of implanted transpedicular screws (Table 1).
It is of notice, that only two misplaced screws had clinical relevance, 26 of 28 misplaced screws (=93%) were clinically silent.
Risk factors for relevant screw misplacement
The only statistically significant risk factor in this series was the level of screw implantation. Most screws were inserted into C3 (26 screws or 27%) and C4 (19 screws or 20%). All nine major breaches occurred at the levels C3 to C5 (Table 2). Minor breaches occurred at all levels with a slight preference at C3 and C4. The risk for screw misplacement for the levels C3 to C5 is significantly higher then for the other cervical levels (P=0.01, fishers exact test).
Table 2.
Level of screws
| Screw position | Correct (n) (%) |
Minor breach (n) (%) |
Major breach (n) (%) |
Total (n) (%) |
|---|---|---|---|---|
| C1 | 1 (100) |
0 (0) |
0 (0) |
1 (100) |
| C2 | 7 (87) |
1 (13) |
0 (0) |
8 (100) |
| C3 | 16 (61) |
8 (31) |
2 (8) |
26 (100) |
| C4 | 9 (48) |
6 (32) |
4 (21) |
19 (100) |
| C5 | 11 (79) |
1 (7) |
2 (14) |
14 (100) |
| C6 | 11 (91) |
1 (9) |
0 (0) |
12 (100) |
| C7 | 11 (79) |
3 (21) |
0 (0) |
14 (100) |
| Total | 66 (70) |
20 (21) |
8 (9) |
94 (100) |
The learning curve of the surgeon and the screw insertion technique had no statistical significance. To analyze the effects of the learning curve we compared the accuracy of the first 20 screws, inserted by three experienced spine surgeons, with all consecutive screws placed by the same surgeons (Table 3). All surgeons were well experienced in instrumentation of the whole spine including lateral mass screws and transarticular screws of the cervical spine. The risk of major breaches was markedly higher for the first 20 screws (13%) then in consecutive screw insertions (4%).
Table 3.
Learning curve
| Screw position | Correct (n) (%) |
Minor breach (n) (%) |
Major breach (n) (%) |
Total (n) (%) |
|---|---|---|---|---|
| First 20 screws (%) | 32 (66) |
10 (21) |
6 (13) |
48 (100) |
| Following screws (%) | 34 (74) |
10 (22) |
2 (4) |
46 (100) |
| Total (%) | 66 (70) |
20 (21) |
8 (9) |
94 (100) |
Furthermore we analyzed the effect of the newly developed trokar system for percutaneous screw insertion on the quality of screw position. We compared the results of seven surgeries using the trokar system and percutaneous screw application with all other procedures performed as standard open surgery. Major breaches occurred only in the group of standard procedures (Table 4).
Table 4.
Screw implant technique
| Screw position | Correct (n) (%) |
Minor breach (n) (%) |
Major breach (n) (%) |
Total (n) (%) |
|---|---|---|---|---|
| conventional (%) | 52 (71) |
13 (18) |
8 (11) |
73 (100) |
| Use of Neon trokar-system (%) | 14 (67) |
7 (33) |
0 (0) |
21 (100) |
| Total (%) | 66 (70) |
20 (21) |
8 (9) |
94 (100) |
We also investigated the influence of an image guidance system. Seventy two from 94 screws were placed with the aid of neuronavigation. The proportional quantity of major screw misplacements was higher in the navigated group then in the others. Comparing the characteristics of these groups, there were relevant differences. The critical levels from C3 to C5 (see Table 2) were preferably treated using neuronavigational assistance, whereas the other levels often were operated without image guidance. Statistical comparison of these groups is impossible because of obvious bias (Table 5).
Table 5.
Use of neuronavigation
| Screw position | Correct (n) (%) |
Minor breach (n) (%) |
Major breach (n) (%) |
Total (n) (%) |
|---|---|---|---|---|
| Without neuronavigation (%) | 17 (77) |
4 (18) |
1 (5) |
22 (100) |
| With neuronavigation (%) | 49 (68) |
16 (22) |
7 (10) |
72 (100) |
| Total (%) | 66 (70) |
20 (21) |
8 (9) |
94 (100) |
Discussion
Previous reports on the use of cervical pedicle screws have focused on anatomical specialties of the cervical spine [6, 9, 14, 17, 18], biomechanical issues [6, 10, 15] and surgical techniques [8, 11, 12]. Few publications dealt with the complications attributed to this surgical technique [1, 8]. In this prospective study, we analyzed the risks of transpedicular screw placement in the cervical spine since its introduction in our department.
Two of 26 patients had clinical signs attributable to surgery (8%) and revision surgery was indicated in one of them (4%). The largest series dealing with transpedicular screw application in the cervical spine is published by Abumi et al. [1], including 180 patients with 712 screw insertions. These authors reported two cases of nerve root injury, one case of vertebral artery injury and two cases of infection, corresponding to an overall complication rate of 2.7%. Revision surgery was done in 1% of the cases (Table 6).
Table 6.
Complications related to posterior cervical screw fixation in four studies
| Present study | Abumi [1] | Kamimura [8] | Heller [5] | |
|---|---|---|---|---|
| Type of screws | Pedicle | Pedicle | Pedicle | Lateral mass |
| No. of patients | 26 | 180 | 9 | 78 |
| No. of screws | 94 | 712 | 36 | 654 |
| Compression or injury of neural structures | 2 | 2 | 0 | 6 |
| Vascular complications | 0 | 1 | 0 | 0 |
| Mechanical complications | 0 | 0 | 0 | 3 |
| Infection | 0 | 2 | 0 | 1 |
| Total | 2 (7.6%) | 5 (2.7%) | 0 (0%) | 10 (12.8%) |
| No. of revision surgery | 1 (3.8%) | 2 (1.1%) | 0 (0%) | 8 (10.3%) |
Compared to their experience, our preliminary series is small and a learning curve must be considered with our results. However, we feel that reporting these results of applying a new technique that is considerably demanding is useful information to others who will add this technique to their repertoire in the future.
Comparing our results with the use of lateral mass screws [5], there are no obvious differences in complication rates concerning vascular or nervous injury of neural structures. Mechanical complications such as implant failure, screw loosening or avulsion and loss of reduction occurred eventually more often with the use of lateral mass screws. The reason for this is the higher pullout strength and higher primary stability of pedicle screws in the cervical spine as compared to lateral mass screws [10, 15].
Radiological assessment of screw placement
In our series, 70% of implanted screws were positioned correctly and further 21% of the screws caused a minor breach of the pedicle wall. This corresponds to the results of Ludwig et al. [12] in their study on cadavers. They found a 76% rate of correct cervical screw placement using computer assisted surgery compared to 13% when using surface landmarks and to 45% correct placement when performing laminoforaminotomies for direct visualization of the pedicles.
Among their patients, Abumi et al. [1] had a very high rate of correct screw placements in about 93%. They used a different surgical technique: first they create a screw insertion hole with a high-speed burr, then a small pedicle probe is inserted into the pedicle and before screw insertion a tapping is performed. They never use a drill bit to penetrate the pedicle [1].
Ludwig et al. [11] compared high quality navigation and the so-called “Abumi technique” using human cadavers. Correct screw placement was possible in 60% using the Abumi technique and in 52% using the navigation system. Twenty-eight percent of the screws placed with the Abumi technique and 30% of the navigation group caused a noncritical breach, defined as not encroaching on critical structures such as neural structures or vertebral artery. A critical breach was seen in 12% of the Abumi group and 18% of the navigation group. These distributions of screw misplacements are very similar to our results with a quote of non critical breaches of 21% and major breaches in 9%.
The explanation for this difference between clinical results of Abumi et al. [1] and the cadaver study of Ludwig et al. [11] is unclear, the main reason might be the extraordinary experience of Abumi et al. with their technique.
Risk factors for relevant screw misplacement
The most obvious risk factor for screw misplacement in our series was the level of surgery. Ninety-one percent of the screws in C6 were correctly placed, compared to only 48% of screws in C4. This can be explained by anatomical facts. The diameter of the pedicles C3 and C4 are the smallest within the cervical spine [6, 9, 14, 17, 18]. Karaikovic et al. [9] found that 75% of the pedicles C3 and 36% of the pedicles C4 are smaller than 4 mm. This means, that in these cases it is impossible to place a pedicle screw with a diameter of 4 mm entirely within the cortical walls. For that reason we accepted a maximal cortical breach of 1 mm for correct placement when using the 4-mm screws of the Neon system. Another reason for the higher number of screw misplacements at the levels C3–C5 is the transverse angle of the pedicle, which is largest in C3 and C4 [12].
In our patients there was a remarkable learning curve with a decrease of major screw misplacements falling from 13% for the first 20 screws to 4% for the consecutive screws. Although all screws were inserted by otherwise experienced spine surgeons, we have to confess that there is a high potential for insertion failure at the beginning due to the different anatomy and the considerable transverse pedicle angle in the cervical spine as compared to the thoracic and lumbar spine [6, 9, 14, 17, 18].
The use of the newly developed trokar system for percutaneous screw application had a favorable effect on the quality of screw positioning, although this was not statistically significant.
For correct transpedicular screw placement a marked transverse angulation of the screws is mandatory. This requires a wide lateral approach and causes large soft tissue damage and means a strain situation during surgery. The neck muscles are hindering the maintenance of an adequate insertion angle. Using the trokar system, this problem has been sufficiently solved.
In our series, the additional use of a neuronavigation system had no clear influence to the results. This is in contrast to other authors [8, 12]. As mentioned above, we cannot make clear conclusions concerning the effect of using image guidance due to obvious bias. We believe, however, that this lack of influence is in part due to the technical pitfalls associated with the technique of cervical transpedicular screw insertion and not attributable to any inaccuracy of image guidance itself.
Conclusion
Instrumentation with cervical transpedicular screws results in very stable fixation. However, with the use of new techniques like percutaneous screw application or computerized image guidance there remains a risk for damaging nerve roots or the vertebral artery. This technique should be reserved for highly selected patients with clear indications and to highly experienced spine surgeons.
Acknowledgements
The studies comply with the current laws of the country in which they were performed inclusive of ethics approval.
References
- 1.Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine. 2000;25:962–969. doi: 10.1097/00007632-200004150-00011. [DOI] [PubMed] [Google Scholar]
- 2.Abumi K, Shono Y, Kotani Y, Kaneda K. Indirect posterior reduction and fusion of the traumatic herniated disc by using a cervical pedicle screw system. J Neurosurg (Spine 1) 2000;92:30–37. doi: 10.3171/spi.2000.92.1.0030. [DOI] [PubMed] [Google Scholar]
- 3.Abumi K, Kaneda K. Pedicle screw fixation for nontraumatic lesions of the cervical spine. Spine. 1997;22:1853–1863. doi: 10.1097/00007632-199708150-00010. [DOI] [PubMed] [Google Scholar]
- 4.Albert TJ, Vacarro A. Postlaminectomy kyphosis. Spine. 1998;23:2738–2745. doi: 10.1097/00007632-199812150-00014. [DOI] [PubMed] [Google Scholar]
- 5.Heller JG, Silcox DH, Sutterlin CE. Complications of posterior cervical plating. Spine. 1995;20:2442–2448. doi: 10.1097/00007632-199511001-00013. [DOI] [PubMed] [Google Scholar]
- 6.Jones EL, Heller JG, Silcox DH, Hutton WC. Cervical pedicle screws versus lateral mass screws. Anatomic feasibility and biomechanical comparison. Spine. 1997;22:977–982. doi: 10.1097/00007632-199705010-00009. [DOI] [PubMed] [Google Scholar]
- 7.Judet J, Roy-Camille R, Joillant G. Actualités de chirurgie orthopédique de l‘Hôspital Raymond Poincarré, No VIII Fractures du rachis cervical. Paris: Masson; 1970. pp. 174–195. [Google Scholar]
- 8.Kamimura M, Ebara S, Itoh H, Tateiwa Y, Kinoshita T, Takaoka K. Cervical pedicle screw insertion: assessment of safety and accuracy with computer assisted image guidance. J Spinal Disord. 2000;13:218–224. doi: 10.1097/00002517-200006000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Karaikovic EE, Daubs MD, Madsen RW, Gaines RW. Morphologic characteristics of human cervical pedicles. Spine. 1997;22:493–500. doi: 10.1097/00007632-199703010-00005. [DOI] [PubMed] [Google Scholar]
- 10.Kowalski JM, Ludwig SC, Hutton WC, Heller JG. Cervical spine pedicle screws, a biomechanical comparison of two insertion techniques. Spine. 2000;25:2865–2867. doi: 10.1097/00007632-200011150-00005. [DOI] [PubMed] [Google Scholar]
- 11.Ludwig SC, Kowaslki JM, Edwards CC, Heller JG. Cervical pedicle screws: comparative accuracy of two insertion techniques. Spine. 2000;25:2675–2681. doi: 10.1097/00007632-200010150-00022. [DOI] [PubMed] [Google Scholar]
- 12.Ludwig SC, Kramer DL, Balderston RA, Vaccaro AR, Foley KF, Albert TJ. Placement of pedicle screws in the human cadaveric cervical spine. Spine. 2000;25:1655–1667. doi: 10.1097/00007632-200007010-00009. [DOI] [PubMed] [Google Scholar]
- 13.Levine AM, Mazel C, Roy-Camille R. Management of fracture separations of the articular mass using posterior cervical plating. Spine. 1992;17(Suppl):S447–S454. doi: 10.1097/00007632-199210001-00018. [DOI] [PubMed] [Google Scholar]
- 14.Panjabi MM, Shin EK, Chen NC, Wang JL. Internal morphology of human cervical pedicles. Spine. 2000;25:1197–1205. doi: 10.1097/00007632-200005150-00002. [DOI] [PubMed] [Google Scholar]
- 15.Richter M, Wilke HJ, Kluger P, Neller S, Claes L, Puhl W. Biomechanical evaluation of a new modular rod-screw implant system for posterior instrumentation of the occipitocervical spine: in-vitro comparison with two established implant systems. Eur Spine J. 2000;9:417–442. doi: 10.1007/s005860000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roy-Camille R, Salient G, Mazel C (1989) Internal fixation of the unstable cervical spine by a posterior osteosynthesis with plates and screws. In: The cervical spine, 2nd edn. Lippincott, Philadelphia, pp 390–403
- 17.Tanaka N, Fujimoto Y, An HS, Ikuta Y, Yasuda M. The anatomic relation among the nerve roots, intervertebral foramina, and intervertebral discs of the cervical spine. Spine. 2000;25:286–291. doi: 10.1097/00007632-200002010-00005. [DOI] [PubMed] [Google Scholar]
- 18.Ugur HC, Attar A, Tekdemir I, Egemen N, Caglar S, Genc Y. Surgical anatomic evaluation of the cervical pedicle and adjacent neural structures. Neurosurgery. 2000;47:1162–1168. doi: 10.1097/00006123-200011000-00029. [DOI] [PubMed] [Google Scholar]
- 19.Veras LM, Pedraza-Gutiérrez S, Castellanos J, Capellades J, Casamitjana J, Rovira-Cañellas A. Vertebral artery occlusion after acute cervical spine trauma. Spine. 2000;25:1171–1177. doi: 10.1097/00007632-200005010-00019. [DOI] [PubMed] [Google Scholar]
- 20.Yamazaki T, Yanaka K, Sato H, Uemura K, Tsukada A, Nose T. Cervical spondylotic myelopathy: surgical results and factors affecting outcome with special reference to age differences. Neurosurgery. 2003;52:122–126. doi: 10.1097/00006123-200301000-00015. [DOI] [PubMed] [Google Scholar]