Introduction
In diarthrodial joint replacement (hip, knee etc.) it is established that results with joint replacement systems improve over time, parallel to their further development in design and along with the growths of surgeons’ experience.
Charnley for instance reported that it took him 14 years to reduce the loosening rate in his series of total hip replacements by 86% [4].
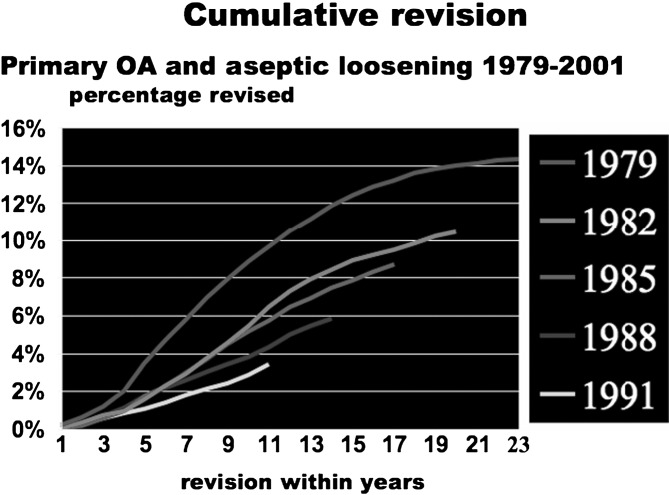
Malchau reflects in the Swedish Hip Study that the cumulative revision rate in Sweden in cemented hip replacement after a comparable follow-up of 11 years dropped from 9% (1979) to 3% (1991) over a time span of 12 years [2] (Fig. 1).
Fig. 1.
Table reflecting the learning curve in hip arthroplasty in Sweden—from Swedish Hip Register
The above paper reports on the long-term follow-up of the initially mixed series of early Charité artificial disc replacements. A large percentage of radiologically confirmed fusions are found and the authors state that “the Charité artificial disc replacement cannot guarantee long-term near to normal function of the spinal motion segment in patients with moderate to severe DDD”.
Firstly, are the evaluations in the publication based on all published literature? Secondly, considering the above-mentioned learning curve, is the conclusion drawn from the results of the initial series disc replacements justified?
Materials and methods
With emerging interest in artificial disc replacement throughout the last decade, the first series of SB Charité artificial disc replacements performed between 1984 and 1990 have been evaluated by several authors who had access to the Charité Hospital patient data [6, 7, 14].
Kiene’s studies in his dissertation over 90 pages are the most detailed and together with the joint publications from Zippel, published by Kiene in June 1997 at the spine symposium at Kloster Banz and Muschik, who lectured at IMAST Barcelona 2000, a relatively conclusive picture can be drawn.
Besides the demographic patient data, a valuation of the patient selection, mono or multilevel results, sizing of implant, it’s positioning and application–instrument availability has to be taken into consideration in order to establish a fair outcome judgement on the Charité’s first artificial disc series.
Results
Patient demographic data reflects a small discrepancy between the present paper’s figures and the previous literature. The authors report that a total of 71 patients with 84 disc prostheses have been operated, whereas Kiene, Lang, Zippel and Muschik reported on 71 patients with 90 prostheses [6, 7, 11, 14].
With respect to the outcome, no conclusions are made in the present paper if mono or multilevel application lead to superior or inferior results, although the prior publications clearly refer to the multi levels as being inferior in outcome.
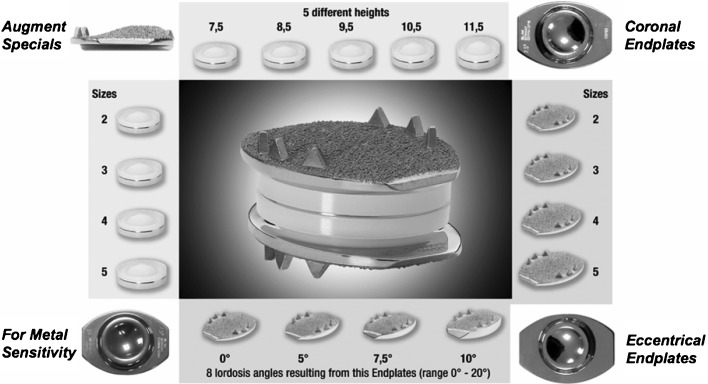
From the radiographs it can be taken that in the follow-up series of prosthesis type III at the Charité Hospital, too small implants of sizes 1 and 2 (the smallest sizes) were used, often in an unphysiological, too anterior position. Not only that meanwhile the smallest size 1 has been eliminated and two larger sizes 4 and 5 (1998, 1999) have been added, additional sagittal plates with angles of 7.5° and 10° (1999) as well as additional sliding cores have been introduced, which allow for anatomical reconstruction of the i.v. space and for large bony end-plate support to avoid subsidence; a bioconductive surface coating (since 1998) provides biological bone/implant bonding. Thus, the statement “The Charité III TDR is still in use today with only minor changes” is clearly misleading (Fig. 2).
Fig. 2.
Large variety of Charité modular components, adaptable to individual patient anatomy
From a biomechanical view and based on the experience in diarthrodial joint prostheses, implants must be chosen to provide large supportive surfaces towards bone and thus distribute the acting forces. That is crucial for motion retention because bone reacts following Wolff’s law [16] with bone remodelling and bridging (development of osteophytes) if the load transfer via implant surfaces is insufficient [13].
Implant choice (availability of sizes and types) and placement seemed to be central problems of the first Charité clinic series, if compared to the technique and results used in later series of other authors, for example as reported in Lemaire’s recent paper of a 10-year minimum follow-up of 100 patients (Clinical results 62% excellent, 28% good and 10% poor) [8]. He used endplates “adaptable to the size of the vertebral endplates” and reported that the majority of the prostheses (59.9%) were centered posterior to the center of the interspace; three quaters (75.5 %) of the implants were also properly centered in the frontal plane.
Kiene, Muschik and Zippel see the reason for the inferior Charité results of the first series mainly in three points [14].
Indications exaggerated (age of patients, diagnosis)
Failure of implants
Positioning of prosthesis
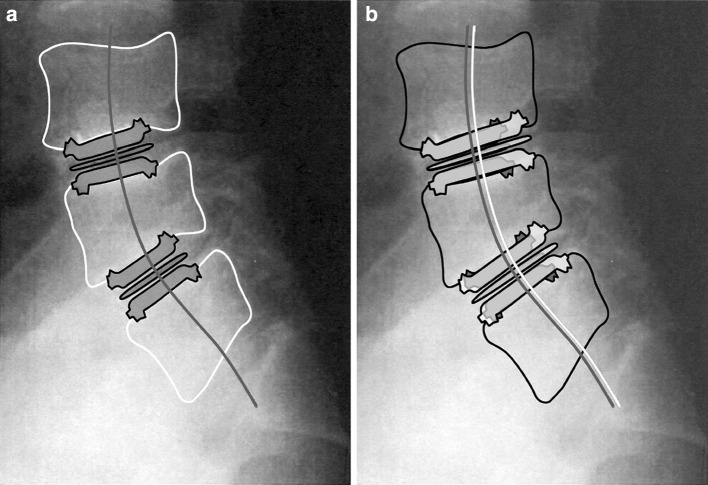
The latter (correct positioning) is, besides correct choice of size, equally important a crucial point to success and if failed may have a negative impact on the facet joints. Lemaire reports that “An implant position ≥4 mm anterior to the centerline creates a dysfunction of the posterior joints, loss of surface contact of the facets in extension and decapitation in flexion”. Figures 3 and 4 of the Charité follow-up publication reflect typical examples of such anterior malposition (here modified to point out insufficient sizing and positioning: Fig. 3a, b)
Fig. 3.
a Example of too small and malpositioned discs (from Putzier et al. article Charité case, Fig. 4). b Same case with two sizes larger discs positioned correct with center dorsally of midline
Putzier et al. state in their follow-up that “even with an ideal implantation technique the Charité TDR can only achieve the repositioning of the anterior column, while the degenerative disorders of the posterior elements are not addressed”.
On contrary Mayer describes in his general overview about contemporary lumbar disc replacements that prostheses with “sliding nucleus” have a certain ability to balance surgeons’ shortcomings in ventral–dorsal placement with respect to posterior structures [10].
Troullier, Kern, Refior and Müller-Gerbl published their findings of a CT osteoabsorptiometrical facet joint study following Charité disc implantation. They found a significant subchondral bone density decrease in the facets which might indicate reduced loading in the posterior vertebral column, quite in contrary to Putziers published assumption of a 2.5-fold load increase after artificial disc implantation in comparison to normal loading conditions [15].
Negative effects following artificial disc implantation in one or both, anterior and posterior column are of course possible if such important parameters as correct implant sizing and positioning are missed. Appropriate load transfer through proper sizing and positioning of implants are part of almost every “basic science” chapter of literature on diarthrodial joint replacement [1, 2, 5].
Conclusion
If it is true that surgeons’ experience with new demanding technologies require a certain time line in the learning curve, as diarthrodial joint replacement experience demonstrates, often a number of years until the peak level is reached, it is inadequate to judge such techniques by their first series of applications. This should be considered in early reports of new techniques as well as in comparative studies, such as the United States IDE’s, where surgeons are expected to produce equivalent or superior results compared to techniques that are in daily use for decades. In the case of Charité IDE it was criticized in a publication that 17% of the implants were suboptimal implanted “despite five training cases”(!) [18].
David, one of the early Charité users, reported a considerable difference in outcome comparing the different periods of learning curve.
In his initial period 1989–1991, he achieved 56% excellent or good results (including patients who received secondary fusion) [19].
In his second period 1992–1993, 82% excellent or good results were achieved (without secondary fusion).
The results of the first series of disc replacements from Charité Hospital cannot be taken as a measure for outcome in today’s Charité disc replacement. Since these first series much work has been done in the field of research and development. Not only that implant variety and design and instrumentation has been adapted to present biomechanical knowledge; experience in patient selection and operative technique has been gained considerably by spine surgeons and design engineers. Basic tips on principles for successful application of the SB Charité are published in a number of papers since these first series [3, 12, 17]. In artificial disc replacement today excellent training and scientific support is provided by every serious implant supplier. Compared to the difficulties of implantation which were experienced in the first patient cohorts in the Charité Hospital in the 1980s, the learning curve in total disc replacement is still present, but has become shorter.
Footnotes
The article to which this letter refers can be found at http://dx.doi.org/10.1007/s00586-005-1022-3. An author’s reply to this letter is available at http://dx.doi.org/10.1007/s00586-006-1082-z
References
- 1.Amstutz HC. Hip arthroplasty. London: Churchill Livingstone; 1991. pp. 261–270. [Google Scholar]
- 2.Balderston RA, Rothman R, Booth RE, Hozack WJ. The hip. Philadelphia: Lea & Febiger; 1992. pp. 3–91. [Google Scholar]
- 3.Büttner-Janz K, Hahn S, Schikora K, Link HD (2002) Grundlagen einer erfolgreichen Anwendung der LINK Zwischenwirbel-Endoprothese Modell SB Charité, Springer, Orthopäde, 31:441–453 [DOI] [PubMed]
- 4.Charnley, John (1979) Low friction arthroplasty. Springer, Berlin Heidelberg New York, pp 65
- 5.Eftekar NS. Total hip arthroplasty. St Louis: Mosby; 1993. pp. 223–312. [Google Scholar]
- 6.Kiene W, Lang K, Zippel H (1997) Experience with the SB Charité intervertebral disc endoprosthesis and conclusions regarding the possibilities of functional intervertebral disc substitution. In: Matzen KA (ed) Therapie des Bandscheibenvorfalls. W. Zuckschwerdt Verlag, München
- 7.Kiene Wolfram (1998) Erfahrungen mit der Bandscheibenprothese SB Charité und Schlussfolgerungen für die Möglichkeit eines funktionellen Bandscheibenersatzes, Dissertation
- 8.Lemaire J Spinal Disord Tech. 2005;18:353. doi: 10.1097/01.bsd.0000172361.07479.6b. [DOI] [PubMed] [Google Scholar]
- 9.Malchau H, Herberts P, Eisler T, Garellick G, Söderman P. The Swedish total hip replacement register. J Bone Joint Surg (Am) 2002;84(Suppl 2):2–20. doi: 10.2106/00004623-200200002-00002. [DOI] [PubMed] [Google Scholar]
- 10.Mayer HH. Degenerative Erkrankungen der Lendenwirbelsäule. Orthopäde. 2005;34:1007–1020. doi: 10.1007/s00132-005-0836-3. [DOI] [PubMed] [Google Scholar]
- 11.McAfee PC (2003) An explanation of early, suboptimal results from Charité Hospital. Büttner-Janz K, Hochschuler (eds) McAfee philosophical and metallurgical differences in the artificial disc. Springer, Berlin Heidelberg New York, pp 11–18
- 12.McAfee PC, Guyer RD. Charité artificial disc replacement. In: Corbin PC, Connolly PJ, Yuan HA, Bao QB, Boden SD, editors. Emerging spine surgery technologies. Los Angeles: Quality Medical Publishing; 2006. pp. 527–561. [Google Scholar]
- 13.Middleditch Alison, Oliver Jean (2005) Functional anatomy of the spine. Elsevier, Amsterdam, ISBN 0-7506-2717-4, pp 304–306
- 14.Muschik M, Zippel H, Kiene W (2000) The Artificial Disc SB Charité – Long Term Results and Conclusions for Chances for an Artificial Spacer. In: 8th international meeting on spine techniques (IMAST), Barcelona, Spain
- 15.Troullier H, Kern P, Refior HJ, Müller-Gerbl M (2005) A prospective morphological study of facet joint integrity following intervertebral disc replacement with the CharitéTM Artificial Disc. Eur Spine J (in press) [DOI] [PMC free article] [PubMed]
- 16.Wolff J. Das Gesetz der Transformation der Knochen. Berlin: Hirschwald; 1892. [Google Scholar]
- 17.Zeegers WS (2003) LINK Lumbar Artificial Disc – Operative Technique: Büttner-Janz, Hochschuler, McAfee The Artificial Disc, Springer, pp 115–138
- 18.Mirza KS. Point of view : commentary on the research reports that led to food and drug administration approval of an artificial disc. Spine. 2005;30(14):1561–1564. doi: 10.1097/01.brs.0000171806.30401.40. [DOI] [PubMed] [Google Scholar]
- 19.David TH. Lumbar disc prosthesis: a study of 85 patients reviewd after a minimum follow-up period of five years. Gieda, Paris, Rachis. 1999;II(4–5):314–315. [Google Scholar]