Abstract
Sacral insufficiency fractures have been described in association with conditions leading to osteoporosis. No association with spondylolisthesis has been described to date. A 60-year-old patient with known lumbosacral isthmic spondylolisthesis presented with exacerbation of symptoms initially thought to be linked to her known spinal pathology. Plain radiography, computer tomography, MRI and bone scan confirmed the presence of a recent sacral insufficiency fracture with anterior angulation. Conservative treatment resulted in improvement of symptoms after 6 months. Care should be taken when considering older patients for more aggressive treatment if they present with exacerbation of back pain and sciatica in the presence of a pre-existing spondylolisthesis. A suspicion of insufficiency fracture should be raised if risk factors exist and further investigations ordered in particular if plain radiography is normal. Lumbosacral fusion might be inappropriate in this setting.
Keywords: Spondylolisthesis, Sacral insufficiency fracture, Osteoporosis, Conservative treatment
Introduction
Sacral insufficiency fractures are seen mainly in patients suffering with osteoporosis. Back pain and spondylolisthesis are common conditions and patients presenting with the two above characteristics might not trigger suspicion of a sacral insufficiency fracture. We describe a rare case of a sacral insufficiency fracture associated with L5–S1 spondylolisthesis.
Case report
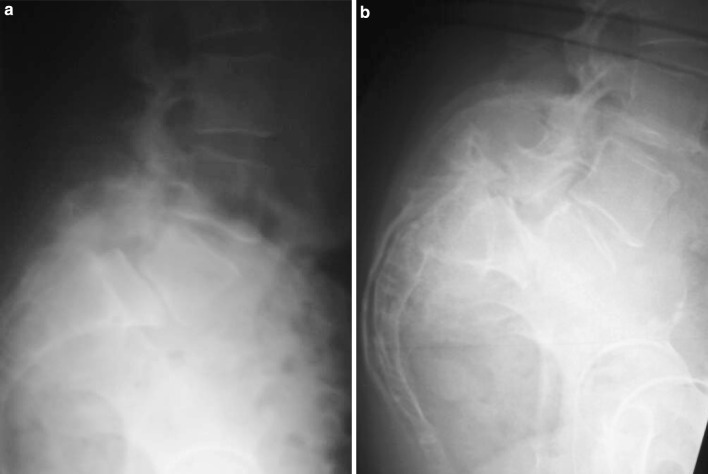
A 60-year-old lady with a 30-year history of intermittent low back pain and a diagnosis of spondylolisthesis treated conservatively presented with an acute exacerbation of low back pain and right sided S1 root symptoms 6 weeks following an uneventful left knee arthroplasty procedure. The initial diagnosis was back pain and sciatica in relation with her known spinal pathology and oral analgesia was prescribed. Due to persistence of symptoms she was referred to a specialist spinal clinic. Clinical examination revealed loss of lumbar mobility, tenderness in the lumbosacral region and diminished force and sensation suggesting left S1 root involvement. Plain radiography showed evidence of a long-standing grade II L5–S1 spondylolisthesis with loss of disc space height. Furthermore, a sharp angulation was noted in the upper end of the sacrum on the lateral films. This view was confronted with earlier films taken at the same institution some 30 years earlier (Fig. 1a, b). A suspicion of sacral insufficiency fracture was raised and further imaging was arranged. Computed tomography (CT) scan (Fig. 2) confirmed a fracture of the sacrum at the S1–S2 level with angulation whereas an MRI (Fig. 3) and a bone scan (Fig. 4) confirmed the recent nature of the pathology (hyperintense signal in MRI and classical H shaped appearance on bone scan). Bone density scan confirmed osteoporosis. Treatment consisted of oral analgesia, calcitonin and gentle physical therapy. Symptoms gradually improved although low back pain persisted to a level comparable to that suffered prior the diagnosis of the insufficiency fracture.
Fig. 1.
a Lateral view of the lumbar spine taken at the age of 30 years showing L5–S1 spondylolisthesis and normal sacral appearance. b Lateral view of the lumbosacral junction showing progression of the L5–S1 slip and disc degeneration associated with an angulation of the sacrum
Fig. 2.

Mid sagittal reformatted CT images showing the fracture at the S1–S2 level
Fig. 3.

Oblique coronal T2 weighted spin–echo image of the sacrum showing hyperintense signal in both sacral ala
Fig. 4.

Posterior view Tc 99m bone scan of the pelvis showing increased uptake with typical H sign appearance
Discussion
Sacral insufficiency fractures have first been described in 1982 [9]. Since, several reports have appeared in the literature relating those fractures to several conditions most of them resulting in osteoporosis. They include rheumatoid arthritis, use of steroids, radiation therapy, Paget’s disease, osteomalacia, hyperparathyroidism, anorexia nervosa and liver transplantation [1, 3, 6–8, 12–16, 19, 20]. Although several reports exist linking pelvic fractures to instrumented fusion [2, 10, 11], we found no description of sacral insufficiency fracture co-existing with nonsurgically treated spondylolisthesis. A single case has been reported of a transverse sacral fracture occurring 4 weeks after lumbosacral fusion for spondylolisthesis and was attributed to transfer of loads from the rigid spinal implants to the adjacent segments [5]. Bilateral spondylolysis abolishes the stabilizing role of the posterior elements in the spinal motion segment which then may lead to spondylolisthesis. The resulting anterior vertebral slippage can be explained by the fact that the lumbosacral junction is subjected to considerable anterior shear forces [4, 18]. In the presence of a bilateral spondylolysis, the main spinal structure resisting these anterior shear forces is the intervertebral disc. It is known that spondylolisthesis progresses in children and adolescents [17]. Although less often reported, progression of slippage in adults has also been shown and is thought to be due to disc degeneration [4]. When degeneration advances the disc height is reduced and ultimately as in this case L5 comes to rest literally on the superior end plate of the sacrum. It is possible that following severe disc degeneration the anterior shear forces have contributed in this osteoporotic patient suffering an anteriorly angulated sacral insufficiency fracture. The clinical relevance of this case is that care should be taken when considering older patients for more aggressive treatment when they present with exacerbation of LBP and sciatica in the presence of a pre-existing spondylolisthesis. A suspicion of insufficiency fracture should be raised if risk factors exist and further investigations ordered in particular if plain radiography is normal. Coronal MRI images with fat saturation sequences as well as bone scan appear to be the most helpful investigations in confirming this type of pathology. Unfortunately this MRI sequence was not available in our patient, the investigation having been organized in a different institution. CT in undisplaced fractures is of little help but in our case it confirmed the diagnosis since there was angulation already visible on plain films. Lumbosacral fusion for such cases might be inappropriate and cause further displacement of an undisplaced unrecognized sacral insufficiency fracture. The coexistence of spondylolisthesis and sacral insufficiency fracture might be unrelated but this case illustrates the importance of having a high suspicion of insufficiency fracture in a patient with risk factors even if an obvious spinal pathology is encountered.
References
- 1.Bliss P, Parsons CA, Blake PR. Incidence and possible aetiological factors in the development of pelvic insufficiency fractures following radical radiotherapy. Br J Radiol. 1996;69(822):548–554. doi: 10.1259/0007-1285-69-822-548. [DOI] [PubMed] [Google Scholar]
- 2.Bose B. Fracture of S1-2 after L4-S1 decompression and fusion. Case report and review of the literature. J Neurosurg. 2003;99(3 Suppl):310–312. doi: 10.3171/spi.2003.99.3.0310. [DOI] [PubMed] [Google Scholar]
- 3.Cooper KL, Beabout JW, Swee RG. Insufficiency fractures of the sacrum. Radiology. 1985;156(1):15–20. doi: 10.1148/radiology.156.1.4001403. [DOI] [PubMed] [Google Scholar]
- 4.Floman Y. Progression of lumbosacral isthmic spondylolisthesis in adults. Spine. 2000;25(3):342–347. doi: 10.1097/00007632-200002010-00014. [DOI] [PubMed] [Google Scholar]
- 5.Fourney DR, Prabhu SS, Cohen ZR, Gokaslan ZL, Rhines LD. Early sacral stress fracture after reduction of spondylolisthesis and lumbosacral fixation: case report. Neurosurgery. 2002;51(6):1507–1510. doi: 10.1097/00006123-200212000-00024. [DOI] [PubMed] [Google Scholar]
- 6.Gotis-Graham I, McGuigan L, Diamond T, Portek I, Quinn R, Sturgess A, et al. Sacral insufficiency fractures in the elderly [Review with 19 Refs] J Bone Joint Surg Br. 1994;76(6):882–886. [PubMed] [Google Scholar]
- 7.Grasland A, Pouchot J, Mathieu A, Paycha F, Vinceneux P. Sacral insufficiency fractures: an easily overlooked cause of back pain in elderly women. Arch Intern Med. 1996;156(6):668–674. doi: 10.1001/archinte.156.6.668. [DOI] [PubMed] [Google Scholar]
- 8.Hauge MD, Cooper KL, Litin SC. Insufficiency fractures of the pelvis that simulate metastatic disease. Mayo Clin Proc. 1988;63(8):807–812. doi: 10.1016/s0025-6196(12)62361-1. [DOI] [PubMed] [Google Scholar]
- 9.Lourie H. Spontaneous osteoporotic fracture of the sacrum. An unrecognized syndrome of the elderly. JAMA. 1982;248(6):715–717. doi: 10.1001/jama.248.6.715. [DOI] [PubMed] [Google Scholar]
- 10.Mathews V, McCance SE, O’Leary PF. Early fracture of the sacrum or pelvis: an unusual complication after multilevel instrumented lumbosacral fusion. Spine. 2001;26(24):E571–E575. doi: 10.1097/00007632-200112150-00027. [DOI] [PubMed] [Google Scholar]
- 11.Morcuende JA, Arauz S, Weinstein SL. Stress fracture of the hip and pubic rami after fusion to the sacrum in an adult with scoliosis: a case report. Iowa Orthop J 20:79–84 [PMC free article] [PubMed]
- 12.Mumber MP, Greven KM, Haygood TM. Pelvic insufficiency fractures associated with radiation atrophy: clinical recognition and diagnostic evaluation. Skeletal Radiol. 1997;26(2):94–99. doi: 10.1007/s002560050200. [DOI] [PubMed] [Google Scholar]
- 13.Newhouse KE, el Khoury GY, Buckwalter JA. Occult sacral fractures in osteopenic patients [see comment] J Bone Joint Surg Am. 1992;74(10):1472–1477. [PubMed] [Google Scholar]
- 14.Peh WC, Khong PL, Ho WY. Insufficiency fractures of the sacrum and os pubis [Review] [20 Refs] Br J Hosp Med. 1995;54(1):15–19. [PubMed] [Google Scholar]
- 15.Peh WC, Khong PL, Ho WY, Yeung HW, Luk KD. Sacral insufficiency fractures. Spectrum of radiological features. Clin Imaging. 1995;19(2):92–101. doi: 10.1016/0899-7071(94)00030-G. [DOI] [PubMed] [Google Scholar]
- 16.Peris P, Navasa M, Guanabens N, Monegal A, Moya F, Brancos MA, et al. Sacral stress fracture after liver transplantation. Br J Rheumatol. 1993;32(8):702–704. doi: 10.1093/rheumatology/32.8.702. [DOI] [PubMed] [Google Scholar]
- 17.Seitsalo S, Osterman K, Hyvarinen H, Tallroth K, Schlenzka D, Poussa M. Progression of spondylolisthesis in children and adolescents. A long-term follow-up of 272 patients. Spine. 1991;16(4):417–421. doi: 10.1097/00007632-199104000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Troup JD. Mechanical factors in spondylolisthesis and spondylolysis. Clin Orthop Relat Res. 1976;June(117):59–67. [PubMed] [Google Scholar]
- 19.Weber M, Hasler P, Gerber H. Insufficiency fractures of the sacrum. Twenty cases and review of the literature [Review with 60 Refs] Spine. 1993;18(16):2507–2512. doi: 10.1097/00007632-199312000-00021. [DOI] [PubMed] [Google Scholar]
- 20.West SG, Troutner JL, Baker MR, Place HM. Sacral insufficiency fractures in rheumatoid arthritis. Spine. 1994;19(18):2117–2121. doi: 10.1097/00007632-199409150-00021. [DOI] [PubMed] [Google Scholar]