Abstract
The thoracic ossification of ligamentum flavum (OLF) is a disease that produces spastic paraparesis, and there are various factors that may affect the surgical outcome of thoracic OLF patients. The authors of this study treated 19 of these thoracic OLF patients from 1998 to 2002, and retrospectively reviewed the patients′ age, sex, symptom duration, involved disease level, preoperative clinical features, neurological findings, radiological findings, the other combined spinal diseases and the surgical outcomes. There were excellent or good surgical outcomes in 16 patients, but 3 patients did not improve after thoracic OLF surgery: this included 1 patient, whose motor function worsened after decompressive thoracic OLF surgery. The favorable contributing factors of surgical outcome in thoracic OLF are a short preoperative symptom duration, single-level lesion, and unilateral lesion type on CT axial scan. On the contrary, the poor prognostic factors are beak type lesion and intramedullary signal changes on T2-weighted sagittal MRI. The complete preoperative evaluation including radiologic findings will provide valuable aid in presuming the surgical outcome for the thoracic OLF patients.
Keywords: Thoracic Spine, Stenosis, Ossification of ligament flavum, Myelopathy, Surgical Outcome
Introduction
The thoracic ossification of ligamentum flavum (OLF) is a rare disease entity, that is most prevalent among Asians; it is a disease that produces myelopathy together with cervical ossification of posterior longitudinal ligament (OPLL), but this condition can be treated and is reversible with appropriate surgical decompression [1-3, 5-12, 14-18].
There are many problems for the diagnosis and treatment of thoracic OLF, because the thoracic OLF is a slowly progressive disease that is commonly revealed as severe spinal cord compression due to severe stenosis. Moreover, it is commonly combined with other spinal disorders, and it is not uncommon for this malady to be misdiagnosed or for there to be a delayed diagnosis [12, 13, 18].
Improved diagnostic tools such as whole spine MRI have recently increased the number of incidentally discovered patients who are without advanced symptoms.
Based on the assumption that early diagnosis in patients with less severe pathologic lesion and proper treatment according to complete evaluation improves the prognosis of thoracic OLF, we retrospectively reviewed the surgical outcome for this disease on the basis of symptom duration, the involved spinal levels, radiologic findings, and the co-presence of other combined spinal diseases.
Material and methods
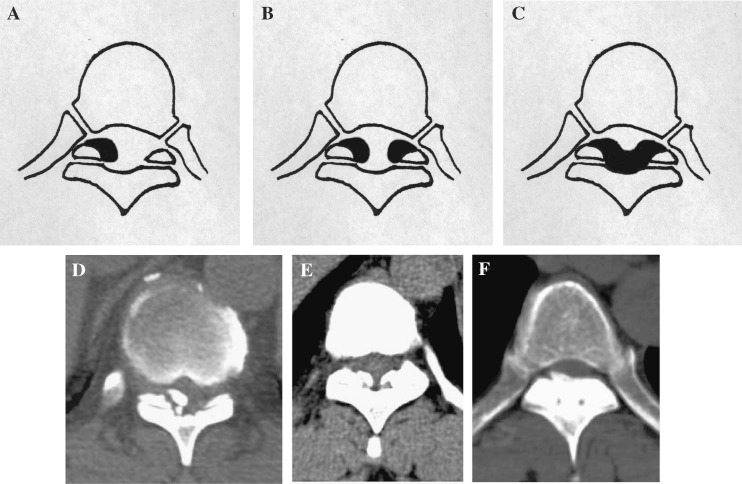
We analyzed 19 patients who underwent surgery between January 1998 and January 2002 for thoracic OLF at our institute. These patients had been followed up more than 2 years, and they also had had whole spinal CT scans and MRI performed on their lesion sites. We classified the type of OLF according to the radiologic findings of the symptomatic lesions that required surgical decompression. The thoracic OLF was classified as the unilateral, bilateral, and bridged types according to the OLF location and types on axial CT scan (Fig. 1).
Fig. 1.
The thoracic OLF was classified into 3 subgroups, unilateral (A,D), bilateral (B,E), and bridged (C,F) types on schematic drawings and axial CT scan
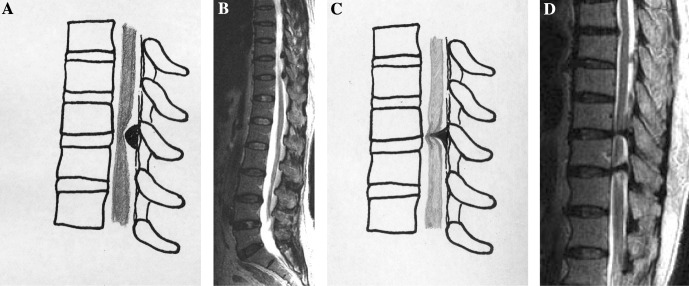
The authors also classified the thoracic OLF as beak and round types according to the OLF type on T2-weighted sagittal MRI image (Fig. 2).
Fig. 2.
The thoracic OLF was classified into 2 subgroups, round (A,B) and beak (C,D) types on schematic drawings and T2-weighted sagittal MRI
There were 10 men and 9 women who ranged in age from 39 years to 70 years (the mean age was 58.5 years old). Total or subtotal laminectomy was limited to the compressed spinal cord levels, and the OLF was completely resected using a high speed drill under microscopic visualization in all the patients.
We checked the Japanese Orthopedic Association (JOA) score for neurological evaluation of the thoracic OLF patients, and we evaluated the surgical outcome as the difference of JOA score, before and after the OLF surgery (Tables 1 and 2).
Table 1.
Scoring system of Japanese Orthopedic Association (JOA)
| Motor dysfunction of the lower extremity | |
| 0 | Cannot walk |
| 1 | Needs cane or aid on flat ground |
| 2 | Needs cane or aid only on stairs |
| 3 | Can walk without cane or aid, but slowly |
| 4 | No disability |
| Sensory deficit of lower extremities | |
| 0 | Severe sensory loss or pain |
| 1 | Mild sensory loss |
| 2 | None |
| Sphincter dysfunction | |
| 0 | Unable to void |
| 1 | Marked difficulty in micturition |
| 2 | Difficulty in micturition |
| 3 | None |
Table 2.
Evaluation of post-operative results
| Surgical outcome | Change of JOA score |
|---|---|
| Excellent | JOA score improved more than 3 points |
| Good | JOA score improved 1–2 points |
| Fair | No JOA score change |
| Poor | Worsening of JOA score |
The patients′ age, sex, the involved spinal levels, duration of symptoms, neurological signs, preoperative MRI and CT findings, coexistent combined spinal lesions, and the surgical outcome were studied (Table 3).
Table 3.
Demographics of the thoracic OLF patients
| Age | Sex | Op. levels | Sx. duration | Bladder and bowel Sx. | Motor weakness | Sensory change | Type of OLF (CT) | Type of OLF (MRI) | Intramedullary signal change(MRI) | Combined spinal lesions | Surgical outcome | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 69 | F | T8–11 | 24 | + | 3 | + | Unilateral | Beak | + | Fair | |
| 2 | 52 | F | T10-L5 | 6 | + | 4 | − | Unilateral | Round | − | C& L- stenosis | Excellent |
| 3 | 49 | F | T9 | 12 | − | 4 | − | Bilateral | Round | − | Good | |
| 4 | 59 | F | T12 | 6 | − | 4 | − | Bilateral | Round | − | Good | |
| 5 | 53 | F | T9–10 | 12 | + | 4 | + | Bilateral | Round | + | Fair | |
| 6 | 39 | F | T11–12 | 6 | + | 2 | + | Unilateral | Round | − | HLD, HCD | Excellent |
| 7 | 62 | F | T10–11 | 6 | + | 3 | + | Bilateral | Round | − | HLD, HCD | Excellent |
| 8 | 58 | F | T10 | 4 | − | 4 | + | Bilateral | Round | − | L- stenosis | Excellent |
| 9 | 61 | F | T9–10 | 12 | + | 4 | + | Unilateral | Round | + | Excellent | |
| 10 | 41 | M | T6–10 | 2 | + | 4 | − | Bilateral | Round | − | HLD, HTD | Good |
| 11 | 62 | M | T12 | 12 | + | 4 | + | Unilateral | Beak | + | Good | |
| 12 | 66 | M | T9 | 48 | − | 4 | − | Bilateral | Round | + | C- stenosis | Excellent |
| 13 | 59 | M | T11 | 36 | − | 4 | − | Bilateral | Round | + | C& L- stenosis | Fair |
| 14 | 67 | M | C2-T3 | 6 | − | 3 | + | Bilateral | Round | + | C- stenosis | Good |
| 15 | 64 | M | T9 | 36 | − | 4 | + | Bilateral | Round | − | Good | |
| 16 | 51 | M | T11 | 9 | + | 4 | + | Bilateral | Round | + | Excellent | |
| 17 | 69 | M | T10 | 60 | − | 4 | − | Bilateral | Round | + | L- stenosis | Good |
| 18 | 70 | M | T10 | 6 | − | 4 | − | Unilateral | Round | + | L- stenosis | Excellent |
| 19 | 60 | M | C2-T10 | 12 | + | 3 | + | Bridge | Round | − | C- stenosis | Good |
+: Existence, −: No existence
F female, M male, Op operation, Sx symptom, HLD Herniation of Lumbar Disc, HCD Herniation of Cervical Disc, HTD Herniation of Thoracic Disc, C Cervical, L Lumbar
Statistical analysis
Comparisons of surgical outcomes with duration of symptoms, involved spinal levels, radiologic findings, and combined spinal disease were made using a Mantel–Haenszel Chi-Square test. Significance was accepted for P-values of < 0.05.
Results
According to our surgical outcome criteria, the difference of JOA score, there were excellent and good results for eight patients and fair results for three patients. After the thoracic OLF surgery, five patients were recovered to a normal motor function from spastic paraparesis, 11 patients were definitely improved with some paraparesis, two patients were not improved, and one patient had worsened motor function, from grade 3 to grade 2 at the immediate post operative state, but, 2 months after operation, this patient improved to the preoperative neurological function state (Case 1).
Duration of symptoms
For the symptom duration, the average symptom duration was 16.6 (2–60) months. Two patients′ symptom duration were less than 6 months, twelve patients were from 6 months to 12 months, and five patients were more than 12 months. There was no statistical significance to surgical outcome owing to symptom duration, because the number of patients was so small amount (P-value: no significant). The patients that suffered from myelopathy for less than 6 months had excellent and good results after surgical decompression. 40 percent (2/5) of those patients who suffered from myelopathy for more than 12 months had fair outcomes (Table 4).
Table 4.
The surgical outcome according to symptom duration of OLF patients
| Excellent | Good | Fair | |
|---|---|---|---|
| < 6 months | 1 | 1 | 0 |
| 6–12 months | 6 | 5 | 1 |
| > 12 months | 1 | 2 | 2 |
Involved levels
There were ten single-level OLF patients, four double-level OLF patients, and five multilevel OLF patients that had involvement of more than three levels. All patients had involvement of the lower thoracic area except one patient. Among the five patients who had multilevel OLF, four patients had OLF disease that was combined with other spinal disease (Table 3). There was no statistical significance to surgical outcome owing to involved levels, because the number of patients was so small (P-value: no significant).
The single-level OLF patients had excellent and good results for 90% (9/10) after surgical OLF removal, and each one of the fair result patient were included in single, double, and multilevel OLF groups (Table 5).
Table 5.
The surgical outcome according to involved level of OLF
| Excellent | Good | Fair | |
|---|---|---|---|
| 1 Level | 4 | 5 | 1 |
| 2 Levels | 3 | 0 | 1 |
| Multi- level | 1 | 3 | 1 |
Radiologic findings
The thoracic OLF was classified as the unilateral, bilateral, and bridged types according to the OLF location and types on axial CT scan. Six patients were the unilateral type, twelve patients were the bilateral type, and one patient was the bridge type (Fig. 1, Table 3). The bilateral type, and especially bridge type, implies there was usually a more severe stenosis rather than for the unilateral type, although some large unilateral OLF produced a severe stenosis. There was no statistical significance to surgical outcome owing to axial CT image, because the number of patients was so small (P-value: no significant). The surgical outcomes for patients with the unilateral type were excellent and good except for one patient. According to the surgical outcome, the excellent group was 66.6% for the unilateral type (4/6) and 33.3% for the bilateral type (4/12). The patient with the bridge type has a good result after surgical OLF decompression (Table 6).
Table 6.
The surgical outcome according to OLF type in CT axial scan
| Excellent | Good | Fair | |
|---|---|---|---|
| Unilateral | 4 | 1 | 1 |
| Bilateral | 4 | 6 | 2 |
| Bridge, nodular | 0 | 1 | 0 |
The authors also classified the thoracic OLF as the beak and round types according to the OLF type on T2-weighted sagittal MRI image. Two patients who had OLF of the beak type, had a fair and good outcome without being excellent (Fig. 2). We also found out the intramedullary cord signal changes on T2-weighted sagittal MRI images for ten patients including two patients of the beak type that were noted as intramedullary cord signal changes. One patient of the beak type (Case 1) had a worsened motor function, from grade 3 to grade 2 at the immediate postoperative state, and then 2 months after the operation, the patient improved to the preoperative motor weakness grade 3.
Combined spinal disease
Thoracic OLF is a slowly progressive disease and it is sometimes combined with other spinal diseases. As a result, it is not uncommon to have a delayed diagnosis or for the patient to be misdiagnosed. Three patients′ OLF were combined with lumbar or cervical spinal stenosis and two patients′ OLF were simultaneously combined with cervical and lumbar stenosis. Among the 19 thoracic OLF patients, two patients had a simple discectomy performed due to lumbar disc herniation before and after the thoracic OLF surgery, and two patients had decompressive surgery performed at the same time for cervical OPLL and thoracic OLF (Table 3). There was also no statistical significance to surgical outcome owing to combined spinal disease.
According to our results, duration of symptoms, involved spinal levels, radiologic findings, and coexistent combined spinal lesions were not related to the surgical outcome statistically. But, short preoperative symptom duration, single-level lesion, and unilateral lesion type on CT axial scan have a tendency to favor the postoperative surgical outcome. On the contrary, the beak type lesion and intramedullary signal changes on T2-weighted sagittal MRI have a tendency to make worse the postoperative surgical outcome.
Discussion
Most of the thoracic OLF patients showed the typical features of thoracic myelopathy: that is, sensory and motor deficits in the trunk and lower extremities, sphincter disturbance, and exaggerated tendon reflexes.
The lower thoracic spine is the most frequently affected area and the patients initially present with posterior column disturbances that are followed by progressively increasing spastic paraparesis [5].
The chronic severe myelopathy caused by thoracic spinal stenosis can be reversible with appropriate decompression, and the surgical outcome was reported to depend on the initial symptom duration, sufficient decompression and the presence of an additional proximal stenosis. Early diagnosis and treatment are important for the postoperative functional prognosis. It is reported that the persistence of residual spasticity at follow-up may be due to irreversible changes within the cord that is caused by the significant cord compression and the delay between the onset of initial symptoms and surgical decompression [2, 9, 12, 14]. In our series, the symptom duration was not related to the surgical outcome statistically, but, especially the short symptom duration, less than 6 months, was a relatively favorable factor to the surgical outcome.
Miyakoshi et al. [9] classified the thoracic OLF into five types according to the range and morphological features of the ossification depicted on the preoperative CT scans at the narrowest spinal level: lateral, extended, enlarged, fused, and tuberous. They reported that there were no correlations observed between the types of OLF and preoperative neurological status or postoperative prognosis. We thought that the classification of thoracic OLF by Miyakoshi N. was too complex for clinical application. So, we classified the OLF with into three types, unilateral, bilateral, and bridge type, concisely and plainly. In our series, there was no relationship between OLF type and the surgical outcome statistically, but the unilateral types and the single lesion of thoracic OLF was thought to be a relatively favorable factor to the surgical outcome.
The whole spine T2-weighted sagittal MRI is the modality of choice for the screening of the longitudinal extent of the OLF because of the common multiplicity of lesion sites, and OLF is often combined with other ossifying ligament diseases [3-5, 7, 9, 13, 14, 17, 18]. The whole spine MRI shows the entire spinal pathology at once, and so we can easily find out the exact pathology levels and sometimes, we can also see the combined spinal pathology such as hidden cervical and lumbar stenosis. Among our patients, five thoracic OLF patients had multiple lesions of the thoracic OLF, and eleven patients also had other combined spinal diseases, which were stenosis and disc herniation of the cervical and lumbar spine. Several patients with involvement of the thoracolumbar junction presented with atypical symptoms of thoracic myelopathy, and some patients had other combined spinal diseases such as cervical and lumbar lesions. Thus the thoracic OLF was infrequently misdiagnosed and treated inappropriately due to the presence of other spinal pathology. Whole spine MRI evaluation and a careful and complete neurologic examination should be performed preoperatively for thoracic OLF patients.
Among our patients, ten had intramedullary signal change on the T2-weighted sagittal MRI image. The three patients who had fair surgical outcomes, and the two patients who had the beak type OLF revealed intramedullary signal change. It is very difficult to remove it because the beak type OLF presses down the spinal cord like an awl. For these beak type lesions, we achieved one good and one fair surgical outcome each without getting any excellent results. We thought that the beak type OLF with intramedullary cord signal change was expected to have irreversible changes within the cord by significant cord compression.
The surgical priority is also very important for the thoracic OLF patient, who has coexistent lesions in the cervical or lumbar area. In my opinion, the priority for surgical decompression in multiple combined spinal stenosis patients is dictated by the patient‘s neurological sign and symptoms, and the best time for an operation is that time that causes the patient the least inconvenience of life style.
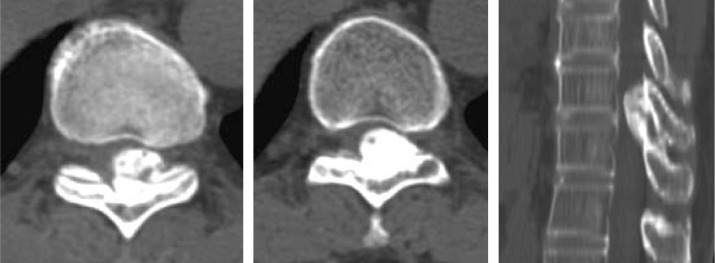
The 66-year old male (Case 12) complained of spastic paraparesis for 48 months and the symptoms had been aggravated for the last 2 months. On the thoracic MRI, thoracic OLF was noted at the T9 area, and this was also combined with cervical stenosis due to cervical OPLL. First of all, we removed the thoracic OLF because he complained of lower extremity spastic paraparesis without any symptom and signs of the upper extremities. His preoperative spastic paraparesis of the lower extremities was completely resolved in spite of the cervical OPLL (Fig. 3).
Fig. 3.
The T9 thoracic OLF is combined with cervical ossification of posterior longitudinal ligament (Case 12)
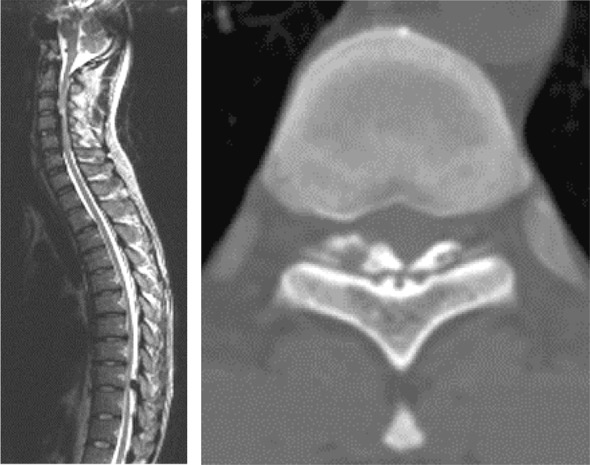
The 61-year old female (Case 9) complained of spastic paraparesis due to severe OLF on the T9, T10 areas. The unilateral and round type OLF had developed from the left side T10 ligament flavum. Operative findings, showed that the OLF was severely adhered to the posterior dura, which made the resection difficult because it cannot well be dissected between the OLF and dura. The OLF was removed with attached dura after thinning the OLF by using a high speed drill under microscopic visualization. The defected dura was repaired with lyodura and the patient‘s motor weakness was improved from grade 4 to grade 5. After the operation, she has been neurologically normalized without any postoperative complications (Case 9) (Fig. 4).
Fig. 4.
The thoracic OLF was adhered to the posterior dura. The thoracic OLF was completely removed with the attached dura and then repaired with the lyodura (Case 9)
In spite of unilateral OLF, we did total or subtotal laminectomy, not hemilaminectomy, to remove the thoracic OLF safely, after removal of the spinous process. we thought that the total or subtotal laminectomy without facet injury of the opposite site, not has pathology has no problem and I placed the emphasis on decompression on OLF lesion site in surgery.
Conclusion
Thoracic OLF is a relatively common disease that produces myelopathy in the thoracic area. The thoracic OLF has the problems of relatively high surgical risk and unpredictable surgical outcome.
In our study, short preoperative symptom duration, single-level lesion, and the unilateral type were relatively favorable prognostic factors, but the beak type and intramedullary signal changes on T2-weighted sagittal MRI image were relatively poor prognostic factors for the thoracic OLF surgery. The combined presence of other spinal diseases with thoracic OLF patients is not related with surgical outcome.
The complete preoperative evaluation including radiologic findings will provide valuable aid in presuming the surgical outcome for the thoracic OLF s according to the results of our study.
Footnotes
A comment to this article can be found at http://dx.doi.org/10.1007/s00586-005-0908-4.
References
- 1.Ben Hamouda K, Jemel H, Haouet S, Khaldi M. Thoracic myelopathy caused by ossification of the ligamentum flavum: a report of 18 cases. J Neurosurg. 2003;99:157–161. doi: 10.3171/spi.2003.99.2.0157. [DOI] [PubMed] [Google Scholar]
- 2.Chang UK, Choe WJ, Chung CK, Kim HJ. Surgical treatment for thoracic spinal stenosis. Spinal Cord. 2001;39:362–369. doi: 10.1038/sj.sc.3101174. [DOI] [PubMed] [Google Scholar]
- 3.Enomoto H, Kuwayama N, Katsumata T, Doi T. Ossification of the ligamentum flavum. A case report and its MRI finding. Neuroradiology. 1988;30:571–573. doi: 10.1007/BF00339704. [DOI] [PubMed] [Google Scholar]
- 4.Epstein NE. Ossification of the yellow ligament and spondylosis and/or ossification of the posterior longitudinal ligament of the thoracic and lumbar spine. J Spinal Disord. 1999;12:250–256. [PubMed] [Google Scholar]
- 5.Fong SY, Wong HK. Thoracic myelopathy secondary to ligamentum flavum ossification. Ann Acad Med Singapore. 2004;33:340–346. [PubMed] [Google Scholar]
- 6.Gil-Salu JL, Lopez-Escobar M, Gomez-Cardenas E, Rodriguez-Pena F, Repeto-Lopez JA, Lopez Lopez J, Garcia-Vazquez F. Calcification of the thoracic yellow ligament as a cause of myelopathy. Rev Neurol. 2002;34:750–753. [PubMed] [Google Scholar]
- 7.Hanakita J, Suwa H, Nagayasu S, Nishi S, Ohta F, Sakaida H. Clinical analysis of ossified thoracic ligaments and thoracic disc hernia. Neurol Med Chir (Tokyo) 1991;31:936–942. doi: 10.2176/nmc.31.936. [DOI] [PubMed] [Google Scholar]
- 8.Kudo S, Ono M, Russell WJ. Ossification of thoracic ligamenta flava. AJR Am J Roentgenol. 1983;141:117–121. doi: 10.2214/ajr.141.1.117. [DOI] [PubMed] [Google Scholar]
- 9.Miyakoshi N, Shimada Y, Suzuki T, Hongo M, Kasukawa Y, Okada K, Itoi E. Factors related to long-term outcome after decompressive surgery for ossification of the ligamentum flavum of the thoracic spine. J Neurosurg. 2003;99:251–256. doi: 10.3171/spi.2003.99.3.0251. [DOI] [PubMed] [Google Scholar]
- 10.Nishiura I, Isozumi T, Nishihara K, Handa H, Koyama T. Surgical approach to ossification of the thoracic yellow ligament. Surg Neurol. 1999;51:368–372. doi: 10.1016/S0090-3019(98)00051-2. [DOI] [PubMed] [Google Scholar]
- 11.Parekh HC, Gurusinghe NT, Perera SS, Prabhu SS. Ossification of the ligamentum flavum in a Caucasian: case report. Br J Neurosurg. 1993;7:687–690. doi: 10.3109/02688699308995100. [DOI] [PubMed] [Google Scholar]
- 12.Shiokawa K, Hanakita J, Suwa H, Saiki M, Oda M, Kajiwara M. Clinical analysis and prognostic study of ossified ligamentum flavum of the thoracic spine. J Neurosurg. 2001;94:221–226. doi: 10.3171/spi.2001.94.2.0221. [DOI] [PubMed] [Google Scholar]
- 13.Takeuchi A, Miyamoto K, Hosoe H, Shimizu K. Thoracic paraplegia due to missed thoracic compressive lesions after lumbar spinal decompression surgery. Report of three cases. J Neurosurg. 2004;100:71–74. doi: 10.3171/spi.2004.100.1.0071. [DOI] [PubMed] [Google Scholar]
- 14.Trivedi P, Behari S, Paul L, Banerji D, Jain VK, Chhabra DK. Thoracic myelopathy secondary to ossified ligamentum flavum. Acta Neurochir (Wien) 2001;143:775–782. doi: 10.1007/s007010170031. [DOI] [PubMed] [Google Scholar]
- 15.Vasudevan A, Knuckey NW. Ossification of the ligamentum flavum. J Clin Neurosci. 2002;9:311–313. doi: 10.1054/jocn.2001.0962. [DOI] [PubMed] [Google Scholar]
- 16.Xiong L, Zeng QY, Jinkins JR. CT and MRI characteristics of ossification of the ligamenta flava in the thoracic spine. Eur Radiol. 2001;11:1798–1802. doi: 10.1007/s003300000788. [DOI] [PubMed] [Google Scholar]
- 17.Yatsuzuka H, Kitajima T, Taguchi Y, Sakai H, Nakamura N. A case of ossified yellow ligaments (ossified ligamenta flava) of the thoraco-lumbar region and magnetic resonance imaging. No Shinkei Geka. 1986;14:1121–1125. [PubMed] [Google Scholar]
- 18.Yonenobu K, Ebara S, Fujiwara K, Yamashita K, Ono K, Yamamoto T, Harada N, Ogino H, Ojima S. Thoracic myelopathy secondary to ossification of the spinal ligament. J Neurosurg. 1987;66:511–518. doi: 10.3171/jns.1987.66.4.0511. [DOI] [PubMed] [Google Scholar]