Abstract
Main problem: Previous studies have demonstrated that sciatica patients have poorer postural control than healthy controls and that postural control remains unchanged 3 months after lumbar discectomy in sciatica patients. The aims of the current study were to investigate whether static balance control recovers in pain-free discectomy patients long-term after lumbar discectomy. Next is to determine whether static balance responses of asymptomatic and symptomatic lumbar discectomy patients differed from each other and from healthy controls. In addition, the influence of the extent of disc resection (unilateral/bilateral removal) and the side of operation on static balance control were investigated. Methods: Fifteen pain-free lumbar discectomy patients, 23 lumbar discectomy patients with residual pain and 72 controls performed unilateral stance tasks with eyes open and eyes closed on a force plate were taken up for the investigation. Three repetitions of a 10 s unilateral stance test were performed on each leg. Postural sway was determined. Patients were divided into three age groups. Results: In the eyes open condition, there was no significant difference between postural sway of pain-free lumbar discectomy patients and controls (P=0.68), whereas balance of patients with pain was significantly worse than in controls (P=0.003). In the eyes closed condition, the sway in both groups of lumbar discectomy patients was significantly worse than in controls (pain-free P=0.009/painful P<0.001). No significant differences were found in postural sway between patients with unilateral and bilateral disc resection. In unilateral stance on the leg of the operated side, centre of gravity sway was not significantly different in the eyes open condition compared to the eyes closed condition, whereas in stance on the leg of the non-operated side, postural sway was significantly lower in the eyes open condition compared to the eyes closed condition. In both conditions, postural sway in the age group of 50–65 years was significantly higher than in the age groups of 30–39 years (eyes open P=0.005; eyes closed P<0.001) and 40–49 years (eyes open P=0.002; eyes closed P=0.006). There was no significant difference between the age group of 30–39 years and the age group of 40–49 years (P=0.51). Conclusion: As for long-term following lumbar discectomy, there is no complete recovery of postural control. Patients seem to develop visual compensation mechanisms for underlying sensory–motor deficits, which are, however, sufficient in case of pain relief only. Further study is needed to determine the cause of the balance disturbances in lumbar discectomy patients.
Keywords: Postural control, Unilateral stance, Lumbar discectomy, Visual compensation
Introduction
Success rates of lumbar discectomy range from 56% to as high as 91%, depending on the outcome measures and follow-up period [1–3, 7–9, 11, 16, 20, and 34]. Residual complaints are, however, present in 28% [15] to 74.6% [34] of the patients. In daily practice, these patients are often left if standard technical examinations are inconclusive. Little hope lies in the amelioration of structural damage such as postoperative fibrosis or nerve damage. One could, however, hypothesize that functional instability of the lumbar spine might play a role in the pathogenesis of residual pain in failed back surgery patents, especially if computed tomography (CT) or magnetic resonance imaging (MRI) only show normal postoperative changes. Since different components are contributing to functional spinal stability, its quality is not easy to evaluate. A specific condition in which functional stability is challenged is postural control or balance. Balance is a measure of whole body performance, which relies on three interacting sensory systems (vestibular, visual and somatosensory system), on the motor output system, and a central processing system [13]. Several studies have identified impairment in postural control in patients with low back pain [18, 26]. A deficit in proprioception in the lumbar spine [32] and altered muscle control [19, 23, and 25] accompanied by alterations in the paravertebral musculature [6, 19] seem responsible for poorer balance control in low back pain (LBP). These alterations also affect the multifidus muscle, which has been shown to be important for spinal stability [6].
Previous studies have demonstrated that sciatica patients have a poorer postural control than healthy subjects [15]. Leinonen et al. [14, 15] reported that the deficiencies in postural control in sciatica patients remained unchanged for 3 months after lumbar discectomy. In this study, postural control measurements consisted of two-footed and one-footed trials, in both eyes open and eyes closed conditions, which were performed 1 day before lumbar microdiscectomy and 3 months after the surgery. However, no long-term results were available in this study and patients with and without residual complaints were not regarded separately [15]. The aims of the current study were to determine whether postural control recovers in pain-free lumbar discectomy patients long-term after lumbar discectomy, and whether balance responses of discectomy patients with residual back and/or leg pain differ from pain-free discectomy patients and control subjects. In addition, postural sway of patients with a unilateral disc resection was compared with postural sway of patients with a bilateral disc resection. The effect of the side of operation on balance in unilateral stance was investigated in the unilateral discectomy group. The effect of age was also regarded.
Materials and methods
Subjects
One hundred and ten subjects, 38 lumbar discectomy patients and 72 controls, participated in the study .
Discectomy group
Forty-three patients (24 males/19 females) were recruited from the Department of Neurosurgery of the Ghent University Hospital. Thirty-eight patients could be included in the study. Standard lumbar discectomy had been performed because of lumbar disc herniation at the level L3–L4 in 1 (2.6%) case, L4–L5 in 16 (42%) cases and L5–S1 in 21 (55%) cases. The disc resection was unilateral in 19 (50%) and bilateral in 19 (50%) cases. Patients were divided into three age categories: 30–39 years (39 patients (39%), mean 34 years), 40–49 years (34 patients (26%), mean 45 years) and 50–65 years (38 patients (34%), mean 55 years). Time ranged from 42 to 83 months (mean 63 months) since surgery. Patients were divided into a pain-free post-discectomy group (n=15) and a post-discectomy group with pain (n=23), based on pain anamnesis and the results of a visual analogue scale for pain (VAS). Twelve of the 23 patients with pain had radicular pain (9 proximal pain, 3 distal pain) and 12 had pure low back pain (Table 2). Pain-free patients had experienced nil or occasional back pain following the operation, and scored 0–1.5 on VAS: the cut off point was set at 1.5 since seven patients pointed a score ranging from 0.5 to 1.5 on VAS, stating that this score was no real pain, but rather reflected the awareness of their back.
Table 2.
Questionnaire scores and clinical characteristics of the lumbar discectomy patients
| Discectomy, no pain | Discectomy with pain | P-value | ||
|---|---|---|---|---|
| N | 15 | 23 | ||
| Pain on VAS | Mean | 0.467, s.d.=0.58 | 3.7, s.d.=1.35 | |
| Range | 0–1.5 | 2–6 | 0<0.001 | |
| Radicular pain | 12 | |||
| Low back pain | 11 | |||
| Time since surgery (months) | 59, s.d.=13 | 66, s.d.=12 | 0.16 | |
| Motor | No paresis | 14 | 17 | 0.60 |
| Paresis | 1 | 5 | ||
| Sensibility | Normal | 11 | 9 | 0.52 |
| Abnormal | 4 | 12 | ||
| Reflexes | Normal | 12 | 8 | 0.093 |
| Abnormal | 2 | 12 | ||
| Lasègue | Positive | 0 | 4 | 0.073 |
| Negative | 15 | 18 | ||
| Kemp | Positive | 3 | 3 | 0.21 |
| Negative | 12 | 17 | ||
| Slump | Positive | 1 | 5 | 0.43 |
| Negative | 14 | 17 | ||
| Quebec | Mean | 14.47, s.d.=11.7 | 31.65, s.d. 15.8 | 0.001 |
| Range | 0–36 | 5–61 | ||
| PCS | Mean | 10.46, s.d.=7.46 | 15.81, s.d.=8.17 | 0.065 |
| Range | 0–23 | 2–33 |
Controls
Seventy-two healthy controls (36 males and 36 females) were recruited via diverse channels. Twenty-four persons were aged 30–39 years, 24 aged 40–49 years and 24 aged 50–65 years.
Exclusion criteria
A CT of the lumbar spine (volume scan, L3–S1) was taken in each lumbar discectomy patient on the day of postural testing to exclude patients with spondylolisthesis, spinal stenosis and recurrent disc herniation. Overall exclusion criteria were a history of balance problems, vestibular dysfunction, neurological impairments [31], unresolved hip/knee/ankle/foot pathology [19], use of medication [19] and scoliosis.
Five of the 43 discectomy patients were excluded from the study: the first person reported symptoms, which suggested recent onset of benign positional vertigo, the second had a degenerative spondylolisthesis on CT, a third person was excluded because of scoliosis, the fourth had a history of a cerebral vascular assault, and the fifth person took anti-depressants.
All participants read and signed an informed consent. The study was approved by the University Ethics Board of the Ghent University. Descriptive data of the healthy controls and the included discectomy patients are mentioned in Table 1.
Table 1.
Mean age, gender and type of lumbar discectomy of controls and included discectomy patients
| Controls | Discectomy, no pain | Discectomy, pain | P-value | |
|---|---|---|---|---|
| N | 72 | 15 | 23 | |
| Age | ||||
| Mean (years) | 44.43, s.d.=9.5 | 42.73, s.d.=9.05 | 46.48, s.d.=9.5 | 0.42 |
| Range (years) | 30–65 | 28–61 | 31–62 | |
| Males | 36 | 8 | 14 | 0.74 |
| Females | 36 | 7 | 9 | |
| Body weight (kg) | 74, s.d. 16.1 | 79.4, s.d.=16.1 | 72.9, s.d.=8.8 | 0.73 |
| Length (cm) | 170.5, s.d.=8.7 | 173.1, s.d.=11.1 | 172.8, s.d.=10.6 | 0.51 |
| Discectomy | – | 8 unilateral, 7 bilateral | 11 unilateral, 12 bilateral | |
Procedure
Interview, clinical examination and questionnaires
All subjects were interviewed (medical history, current complaints, use of medication).
Lumbar discectomy patients were examined, and clinically observed motor deficits, sensory deficits and reflex abnormalities were recorded. Slump length provocation test, Kemp’s test and Lasègue’s test were assessed. Discectomy patients were asked to complete the Quebec Back Pain Disability Questionnaire (QBPDS), Dutch language version [29] and the Pain Catastrophizing Scale [30]. LBP and leg pain were measured on a 10-cm VAS. Descriptive data are given in Table 2.
Static postural control
Patients of three different groups were randomly invited to perform the postural control tests. All tests were under supervision of an independent examiner who was blinded on patient’s operation and symptoms. Postural control in unilateral stance, a test commonly used in clinical practice to test balance, was preferred. Measurements were made in a closed room, free from external distractions and all procedures and instructions were standardized. Postural sway in unilateral stance was tested on a force plate (Neurocom Balance Master) [22]. The patients stood barefoot on the force plate, hands rested on the iliac crests. Foot position was marked on the force plate. The right foot was lifted to a standard height of 10 cm. This 10-s test was performed three times with eyes open, and three times with eyes closed. The same procedure was followed for the other leg. The centre of gravity (COG) sway velocity (°/s), which is the ratio of the distance travelled by the COG to the time of the trial (10 s), was calculated for each trial.
All balance tests were performed three times to test for reliability. Intraclass correlation coefficients ranged from 0.70 to 0.98.
Data analysis
Descriptive statistics show the patient characteristics and clinical findings. One-way analysis of variance (ANOVA) was performed to investigate significant differences between controls, discectomy patients with pain and pain-free discectomy patients (Table 1): independent samples t-tests were performed to investigate differences between the discectomy groups (Table 2).
A repeated-measures ANOVA with four factors was performed to investigate possible differences in balance among the three groups in four different conditions. The two between-subject factors were “group” (with three sublevels: controls, pain-free patients, painful patients) and age group (30–39, 40–49, and 50–65 years) and two within subject factors of “side” (left/right side) and “condition” (open/closed eyes).
To investigate possible differences between healthy controls, and patients with a unilateral and bilateral disc resection, a repeated-measures ANOVA with five factors was used. Three between-subject factors: “surgery” (no surgery/unilateral/bilateral), “age group” (30–39, 40–49, and 50–65 years) and “pain” (present/absent). The two within-subject factors were “side” (left/right unilateral stance) and “condition” (eyes open/closed).
Unilateral discectomy patients were investigated separately to evaluate possible differences in quality of one leg stance on the ipsilateral side of the disc vs. stance on the contralateral leg. A repeated-measures ANOVA with four factors was used for this purpose; “age group” and “presence of pain” (pain/no pain) as between factors and “side” (affected side/non-affected side) and “condition” (eyes open/closed) as within factors. Least significant difference tests were performed in case of significant interactions between two factors.
The statistical analyses were performed with SPSS 10.0 software (SPSS, Chicago, IL), and statistical significance was set as P<0.05.
Results
The healthy controls, the pain-free discectomy patients and the discectomy patients with pain did not significantly differ in age, gender, and height and body weight. Time since surgery was not significantly different in lumbar discectomy patients with and without pain. Only QBPDQ score was significantly different between these two groups (mean score of 14.47 in the pain-free discectomy group; 31.65 in the group experiencing residual pain).
Comparison of controls, pain-free lumbar discectomy patients and painful lumbar discectomy patients
In the first repeated-measures ANOVA, the factor “side” was not significant (left vs. right unilateral stance: P=0.081). There was a significant interaction between the factor “condition” and the factor “age group” (P<0.001), and between the factor “condition” and the factor “group” (controls–pain-free discectomy–painful discectomy: P=0.001).
Condition—group
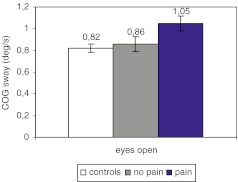
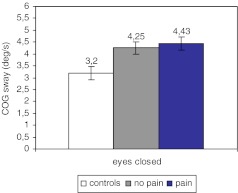
In healthy controls, and in both discectomy groups, COG sway was significantly higher in the eyes closed condition than in the eyes open condition (P<0.001; controls: eyes open 0.82°/s, eyes closed 3.20°/s; no pain: eyes open 0.86°/s, eyes closed 4.25°/s; with pain: eyes open 1.05°/s, eyes closed 4.43°/s).
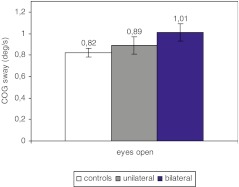
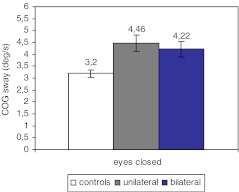
In the eyes open condition (Fig. 1), mean postural sway of the controls was significantly lower than mean postural sway of the painful discectomy patients (P=0.003). There was no significant difference between the controls and the pain-free discectomy patients (P=0.68). There was a slight tendency towards lower mean postural sway in the pain-free lumbar discectomy group compared to the painful discectomy group (P=0.085). In the eyes closed condition (Fig. 2), mean postural sway was significantly lower in the control group compared with both the painful discectomy group (P<0.001) and the pain-free lumbar discectomy group (P=0.009). There was no significant difference between mean postural sway of the pain-free discectomy group and the painful discectomy group (P=0.69) (Fig. 2).
Fig. 1.
COG sway in eyes open condition in controls, pain-free discectomy patients and painful discectomy patients
Fig. 2.
COG sway in eyes closed condition in controls, pain-free discectomy patients and painful discectomy patients
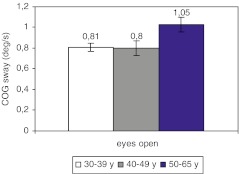
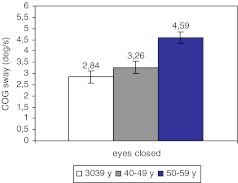
Condition—age group
In both conditions, postural sway was in the age group of 50–65 years (eyes open mean 1.05°/s, eyes closed 4.59°/s) significantly higher than in the age groups of 30–39 years (eyes open P=0.005, mean 0.81°/s; eyes closed P<0.001, mean 2.84°/s) and 40–49 years (eyes open P=0.002, mean 0.8°/s; eyes closed P=0.006, mean 3.26°/s) Figs. 3 and 4. There was no significant difference between the age group of 30–39 years and the age group of 40–49 years (P=0.51).
Fig. 3.
COG sway in eyes open condition in the age groups of 30–39, 40–49 and 50–65 years
Fig. 4.
COG sway in eyes closed condition in the age groups of 30–39, 40–49 and 50–65 years
In all age groups, postural sway was significantly higher in the eyes closed condition compared to the eyes open condition (P<0.001) (30–39 years: open 0.85°/s, closed 3.13°/s, 40–49 years: open 0.79°/s, closed 3.79°/s, 50–65 years: open 1.10°/s, closed 4.96°/s).
Comparison of controls, unilateral discectomy patients and bilateral discectomy patients
The factor “side” was not significant (P=0.06). There was a significant interaction between the factors “condition” and “surgery” (P=0.026) and between the factors “condition” and “age group” (P=0.001). The factor “pain” was not significant (P=0.42).
Condition—surgery
As for healthy controls, in patients with a unilateral disc resection and patients with a bilateral disc resection, postural sway in the eyes closed condition was higher than in the eyes open condition (P<0.001; controls: open 0.82°/s, closed 3.20°/s, unilateral: open 0.89°/s, closed 4.46°/s, bilateral: open 1.01°/s, closed 4.22°/s).
In the eyes open condition (Fig. 5), postural sway was significantly higher in bilateral discectomy patients than in controls (P=0.025). There was no significant difference between controls and unilateral discectomy patients (P=0.44), or between unilateral and bilateral discectomy patients (P=0.28).
Fig. 5.
COG sway in eyes open condition in controls, unilateral discectomy patients and bilateral discectomy patients
In the eyes closed condition (Fig. 6), postural sway were significantly lower in the control group compared with both the unilateral discectomy group (P<0.001) and the bilateral discectomy group (P=0.005). There was no significant difference between the unilateral discectomy patients and bilateral discectomy patients (P=0.60).
Fig. 6.
COG sway in eyes closed condition in controls, unilateral discectomy patients and bilateral discectomy patients
Condition—age group
In both conditions, postural sway in the age group of 50–65 years was significantly higher than in the age groups of 30–39 years (eyes open P=0.016; eyes closed P<0.001) and 40–49 years (eyes open P=0.004; eyes closed P=0.044) Fig. 3.
In the three age groups, postural sway was higher in the eyes closed condition compared with the eyes open condition (P<0.001; 30–39 years: open 0.88°/s, closed 3.20°/s; 40–49 years: open 0.78°/s, closed 4.06°/s; 50–65 years: open 1.13°/s, closed 5.08°/s).
Unilateral discectomy: operated side vs. non-operated side
Regarding only unilateral discectomy patients, the interaction between the factors “affected side” and “age group” (P=0.009) and the interaction between “affected side” and “condition” (P=0.001) were significant. The factor “pain” was not significant (P=0.42).
Affected side—condition
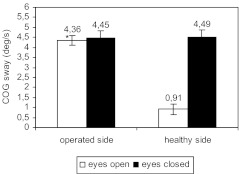
In the eyes open condition, postural sway was significantly higher in unilateral stance on the leg of the operated side compared to the non-operated side (P<0.001; operated side 4.38°/s, non-operated side 0.91°/s). In the eyes closed condition, there was no significant difference between stance on the leg of the operated side compared with stance on the leg of the non-operated side (P=0.94, operated side 4.45°/s, non-operated side 4.49°/s).
In unilateral stance on the leg of the affected side, COG sway was not significantly different in the eyes open condition compared to the eyes closed condition (P=0.87; eyes open 4.36°/s, eyes closed 4.45°/s) (Fig. 5). In unilateral stance on the leg of the non-operated side, postural sway was significantly lower in the eyes open condition compared to the eyes closed condition (P<0.001; eyes open 0.91°/s, eyes closed 4.49°/s) (Fig. 7).
Fig. 7.
COG sway in stance on the leg of the operated side vs. stance on the leg of the non-operated side in eyes open and eyes closed conditions
Affected side—age group
In the three age groups, postural sway was significantly higher in stance on the leg of the ipsilateral side of the disc resection (30–39 years: P=0.007; operated side 3.19°/s, non-operated side 2.36°/s; 40–49 years: P<0.001; operated side 4.72°/s, non-operated side 2.59°/s; 50–65 years: P<0.001; operated side 5.30°/s, non-operated side 3.14°/s).
Postural sway in unilateral stance on the leg of the operated side was significantly lower in the age group of 30–39 years than in age group of 50–65 years (P=0.004). There was a tendency towards significant lower postural sway in age group of 30–39 years compared to that of 40–49 years (P=0.05) (Fig. 7). The difference between age group of 40–49 years and age group of 50–65 years was not significant (P=0.45).
There were no significant differences among the three age groups in unilateral stance on the leg of the non-operated side.
Discussion
The current study aimed at testing postural control in lumbar discectomy patients and healthy controls. Unilateral stance was preferred: this condition is known to challenge balance, and is a commonly used test for balance in studies [15, 17] and in clinical practice. Since pain itself is a known cause of balance disturbances [4, 18], it was necessary to select a group of surgical patients, who were completely relieved from pain following surgery. The selection of this group was particularly difficult since patients also had to have been spared from health problems with possible influence on balance. Surgical patients with residual pain were also tested to investigate the difference in postural control with controls and with the pain-free lumbar discectomy patients. Two significant differences in patient characteristics were found between the two patient subgroups: the Quebec score was significantly higher in subjects with pain, and Lasègue’s test was significantly more positive in the group with pain.
Comparison of controls, pain-free lumbar discectomy patients and lumbar discectomy patients with pain
Condition—group
In healthy controls and in both lumbar discectomy groups, postural sway in the eyes closed condition was higher than in the eyes open condition, due to the absence of visual compensation. The eyes closed condition has previously been shown to be a greater challenge to the proprioceptive system [15, 18, and 26], and is an appropriate condition to uncover latent balance dysfunctions.
In both eyes open and eyes closed conditions, mean postural sway of the controls was significantly lower than mean postural sway of the discectomy patients with pain. There was, however, no significant difference between the controls and the pain-free discectomy patients in the eyes open condition, and there was a tendency towards lower mean postural sway in the pain-free lumbar discectomy group compared to the painful discectomy group (P=0.085), which was not present in the eyes closed condition (P=0.688).
It thus seems that long-term after lumbar discectomy, impaired postural control is reversible in conditions that only slightly challenge balance. In pain-free patients, the balance disturbances seem to be discrete and they can be compensated by the visual system. In the eyes closed condition, postural sway in the pain-free lumbar discectomy patients relatively augmented more (mean of left and right side: 395%) than in controls (288%) and in discectomy patients with pain (318%), resulting in a significant difference between controls and pain-free discectomy patients.
In lumbar discectomy patients still suffering from pain, two factors seem to negatively interfere with proper balance responses: the above-mentioned latent disturbances, which are also present in the pain-free lumbar discectomy patients, and patients with presence of pain. It is hypothesized that the presence of pain causes additive disturbances of the balance control system, and overrules the visual compensation.
However, the actual cause of the postural disturbances in these patients cannot be derived from the current data. They could have been installed pre-operatively, as a consequence of disc herniation [15] and chronic LBP [17–19, 21, and 26], and never have completely disappeared; they could be related to muscle deconditioning or muscle inhibition, or to operatively induced changes [5, 10, and 31]. The latter seems unlikely since in a study comparing pre-operative and 2-month post-operative balance-testing, postural control was not worse (remained unchanged) after surgery [15]. The authors considered that the recovery of postural control could even have been still taking place. In the current study, postural control was evaluated at least 42 months after operation, and no changes were to be expected as a consequence of post-operative tissue healing. In contrast to Leinonen’s study, postural control of lumbar discectomy patients was in the eyes open condition similar to that of controls in case of absence of pain, which suggests a partial recovery of balance. Therefore, it seems plausible that not the surgical intervention, but rather a combination of multiple factors may contribute to ongoing postural control deficits after lumbar discectomy, such as proprioceptive dysfunctions [15], impaired feed-forward control [14], and psychological factors related with earlier pain experiences.
Condition—age group
The higher postural sway in the oldest patient group was expected: postural control is long known to become more disturbed with advancing age [27]. The increased postural sway in unilateral stance with age is in accordance with similar findings in previous studies [12, 33].
In all age groups, COG sway was again higher in the eyes closed condition than in the eyes open condition.
Comparison of healthy controls, unilateral discectomy patients and bilateral discectomy patients
No significant differences were found between unilateral and bilateral disc resection.
In theory, a unilateral disc resection differs from a bilateral one in the surgical approach and in the amount and location of disc tissue removed. In bilateral disc resections, muscle and ligament damage is likely to be more present than in unilateral disc resection, since the paraspinal muscles are stripped of the spinous process on both sides, and the ligaments can be bilaterally harmed. A difference in surgically induced damage of proprioceptors might thus be expected. The difference in muscle damage may however have been less present in our study population since a bilateral muscle spreader was used in the majority of the unilateral disc resections.
As a consequence of a difference in the amount and the location of disc tissue resection, the degenerative processes following a unilateral discectomy might differ from those following a unilateral discectomy. It was hypothesized that long term following unilateral discectomy, the degenerative changes would have been more pronounced on the ipsilateral side compared to the contra lateral side. However, CT scans showed only minor changes in disc height on the operated side compared to the non-operated side in 17 of the 19 unilateral discectomy patients. In six patients, an antero-posterior difference in disc height was present, but there was no left–right difference. In seven patients, the disc on the level of operation had completely disappeared.
In accordance with previous findings, postural sway was again significantly higher in the age group of 50–65 years compared to the age groups of 30–39 and 40–49 years. In the three age groups, postural sway in the eyes closed condition was higher than in the eyes open condition.
Unilateral discectomy: operated side vs. non-operated side
Affected side—condition
In Leinonen’s study, body sway was not associated with the side of sciatica in the one-footed test [15]. In the current study, COG sway was significantly higher in unilateral stance on the leg of the operated side compared to the non-operated side in the eyes open condition. Unilateral discectomy patients seem capable to overcome postural disturbances by visual compensation mechanisms in stance on the healthy side, but not in stance on the operated side. The presence of pain was not a significant factor for postural sway in this series. Since a bilateral muscle spreader was used in unilateral discectomy patients, the iatrogenic muscle damage was similar and was on both sides. The current study is therefore in favour of other mechanisms than iatrogenic muscle damage as the cause of balance disturbances. Psychological factors related with earlier pain experiences might, however, play a role: these patients have mainly experienced unilateral leg pain, and perhaps this former experience influences balance responses in a complicated manner.
Affected side—age group
In the three age groups, postural sway was significantly higher in stance on the leg of the ipsilateral side of the disc resection. A higher postural sway with advancing age was seen, but somewhat unexpectedly only on the side of the operation.
Conclusion
In lumbar discectomy patients, postural sway in unilateral stance is influenced by age, the presence of pain and the side of former disc herniation. Long-term following lumbar discectomy, there is no complete recovery of postural control. Patients develop visual compensation mechanisms for underlying sensory–motor deficits, which seem, however, sufficient only in case of pain relief.
The maintenance of whole-body postural balance is a complex task, and recovery of postural control in sciatica patients seems likely in case of pain relief by the surgical intervention. Further study is needed to investigate the cause of balance deficits in lumbar discectomy patients.
References
- 1.Abramovitz JM, Neff SR. Lumbar disc surgery: Results of the prospective lumbar discectomy study of the joint section disorders of the spine and peripheral nerves of the American Association of Neurological Surgeons and the Congress of Neurological Surgeons. Neurosurgery. 1991;29:301–308. doi: 10.1097/00006123-199108000-00027. [DOI] [PubMed] [Google Scholar]
- 2.Atlas J, Chang Y, Kammann E, et al. Long-term disability and return to work among patients who have a herniated lumbar disc: the effect of disability compensation. J Bone Joint Surg. 2000;82:4–14. doi: 10.2106/00004623-200001000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Atlas SJ, Keller RB, Chang YC, et al. Surgical and non-surgical management of sciatica secondary to a lumbar disc herniation. Five-year outcomes from the Maine. Spine. 2001;26:1179–1187. doi: 10.1097/00007632-200105150-00017. [DOI] [PubMed] [Google Scholar]
- 4.Byl NN, Sinnott PL. in balance and body sway in middle-aged adults with healthy backs compacted with subjects low-back dysfunction. Spine. 1991;16(3):325–330. doi: 10.1097/00007632-199103000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Cooper RG, Jayson MIV. Radiographic demonstration of paraspinal muscle waisting in patients with chronic low back pain. Br J Rheumatol. 1992;31:389–394. doi: 10.1093/rheumatology/31.6.389. [DOI] [PubMed] [Google Scholar]
- 6.Danneels LA, Vanderstraeten GG, Canmbier DC, et al. JCT imaging of trunk muscles in chronic low back pain patients and healthy control subjects. Eur Spine J. 2000;9:266–272. doi: 10.1007/s005860000190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davis RA. A long-term analysis of 984 surgically treated herniated lumbar discs. J Neurosurg. 1994;80:415–421. doi: 10.3171/jns.1994.80.3.0415. [DOI] [PubMed] [Google Scholar]
- 8.Dvorak J, Guachat MH, Valach L. The outcome of surgery for lumbar disc herniation: a 4–17 years follow-up with emphasis on somatic aspects. Spine. 1988;13:1418–422. doi: 10.1097/00007632-198812000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Findlay GF, Hall B, Musa BS, et al. A ten-year follow-up of the outcome of lumbar microdiscectomy. Spine. 1998;23:1168–1171. doi: 10.1097/00007632-199805150-00019. [DOI] [PubMed] [Google Scholar]
- 10.Gejo R, Matsui H, Kawaguchi Y, et al. Serial changes in trunk muscle performance after posterior lumbar surgery. Spine. 1999;24(10):1023–1028. doi: 10.1097/00007632-199905150-00017. [DOI] [PubMed] [Google Scholar]
- 11.Gibson JMA, Grant IC Waddell G (2002) Surgery for lumbar disc prolapse (Cochrane Review). In: The Cochrane Library, Issue 4 2002. Oxford: Update Software
- 12.Hageman PA, Leibowitz JM, Banks D. Age and gender effects on postural control measures. Arch Phys Med Rehabil. 1995;76:961–964. doi: 10.1016/S0003-9993(95)80075-1. [DOI] [PubMed] [Google Scholar]
- 13.Horak FB, Shupert CL, Marka A. A comparison of postural dyscontrol in the elderly. A review. Neurobiol Aging. 1989;10:727–738. doi: 10.1016/0197-4580(89)90010-9. [DOI] [PubMed] [Google Scholar]
- 14.Leinonen V, Kankaanpaa M, Luukkonen M, et al. Disc herniation-related back pain impairs feed-forward control of paraspinal muscles. Spine. 2001;26(16):367–372. doi: 10.1097/00007632-200108150-00014. [DOI] [PubMed] [Google Scholar]
- 15.Leinonen V, Kankaanppää M, Luukkonen M, et al. Lumbar paraspinal muscle function, perception of lumbar position, and postural control in disc herniation-related back pain. Spine. 2003;28(8):842–848. doi: 10.1097/00007632-200304150-00019. [DOI] [PubMed] [Google Scholar]
- 16.Loupasis GA, Stanos K, Katonis PG, et al. Seven-to 20-year outcome of lumbar discectomy. Spine. 1999;24:2313–2317. doi: 10.1097/00007632-199911150-00005. [DOI] [PubMed] [Google Scholar]
- 17.Luoto Spine. 1998;23:2081. doi: 10.1097/00007632-199810010-00008. [DOI] [PubMed] [Google Scholar]
- 18.Mientjes MI, Frank JS. Balance in chronic low back pain patients compared to healthy people under various conditions in upright standing. Clin Biomech (Bristol, Avon) 1999;14(10):710–716. doi: 10.1016/s0268-0033(99)00025-x. [DOI] [PubMed] [Google Scholar]
- 19.Mok NW, Brauer SG, Hodges PW, et al. Hip strategy for balance control in quiet standing is reduced in people with low back pain. Spine. 2004;29(6):E107–E112. doi: 10.1097/01.BRS.0000115134.97854.C9. [DOI] [PubMed] [Google Scholar]
- 20.Naylor A. The late results for laminectomy for lumbar disc prolapse: a review after ten to twenty-five years follow-up. J Bone Joint Surg. 1974;56:17–29. [PubMed] [Google Scholar]
- 21.Nies N, Sinnott PL. Variations in balance and body sway in middle-aged adults. Subjects with healthy backs compared with subjects with low-back dysfunction. Spine. 1991;16(3):325–330. doi: 10.1097/00007632-199103000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Operators manual. Neurocom Balance Master, version 6.1.Neurocom International, Inc., 1998
- 23.Panjabi J Spinal Disord. 1992;5:383. doi: 10.1097/00002517-199212000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Parkola R, Rytokoski U, Kormano M. Magnetic Resonance imaging of the dsics and trunk muscles in patients with chronic low back pain and healthy control subjects. Spine. 1993;18:830–836. doi: 10.1097/00007632-199306000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Radebold A, Andrea MD, Cholewicki J, et al. muscle response pattern to sudden trunk loading in healthy individuals and in patients with chronic low back pain. Spine. 2000;25(8):947–954. doi: 10.1097/00007632-200004150-00009. [DOI] [PubMed] [Google Scholar]
- 26.Radebold A, Cholewicki J, Polzhofer GK, Greene HS. Impaired postural control of the lumbar spine is associated with delayed muscle response times in patients with chronic idiopathic low back pain. Spine. 2001;26(7):724–730. doi: 10.1097/00007632-200104010-00004. [DOI] [PubMed] [Google Scholar]
- 27.Regind H, Lykkegaard JJ, Bliddal H. Postural sway in normal subjects aged 20–70 years. Clin Physiol Funct Imaging. 2003;23:171–176. doi: 10.1046/j.1475-097X.2003.00492.x. [DOI] [PubMed] [Google Scholar]
- 28.Runge CF, Shupert CL, Horak B, et al. Ankle and hip postural strategies defined by joint torques. Gait Posture. 1999;10(2):161–167. doi: 10.1016/S0966-6362(99)00032-6. [DOI] [PubMed] [Google Scholar]
- 29.Schoppink LEM, Tulder MW, Koes BW, et al. Reliability and validity of the Dutch Adaptation of the Quebec Back Pain Disability Scale. Phys Ther. 1996;76:268–27. doi: 10.1093/ptj/76.3.268. [DOI] [PubMed] [Google Scholar]
- 30.Severeijns R, Hout MA, Vlaeyen JW, et al. Pain catastrophizing and general health status in a large Dutch community sample. Pain. 2002;99(1–2):367–376. doi: 10.1016/S0304-3959(02)00219-1. [DOI] [PubMed] [Google Scholar]
- 31.Sihvonen T, Herno A, Paljarvi L, et al. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine. 1993;5:575–581. doi: 10.1097/00007632-199304000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Teasdale N, Stelmach GE, Breunig A. Postural sway characteristics of the elderly under normal and altered visual and support surface conditions. J Gerontol. 1991;46(6):238–244. doi: 10.1093/geronj/46.6.b238. [DOI] [PubMed] [Google Scholar]
- 33.Yorimitsu E, Chiba K, Toyama Y, et al. Long-term outcomes of standard discectomy for lumbar disc herniation. A follow-up study of more than 10 years. Spine. 2001;26:652–657. doi: 10.1097/00007632-200103150-00019. [DOI] [PubMed] [Google Scholar]