Abstract
Tight hamstrings syndrome (THS) has been attributed to a number of disorders. Most authors argue that tight hamstring syndrome is determined in the majority of cases by a protruding or slipped vertebral disc. The term “disc related tight hamstring syndrome” is usually used to describe the condition. However, tight hamstring syndrome in childhood can also be an initial symptom of a usually severe disease. We reviewed retrospectively 102 children who had presented to our clinics with tight hamstring syndrome in the past 22 years (between 1980 and 2001). To our knowledge, this study includes the largest number of patients with tight hamstring syndrome analysed so far. Seventy four children (73%) suffered from severe underlying diseases. In more than one-third of all THS cases (38 of 102 cases; 37%), we observed intra- or extraspinal tumorous alterations. In 15% of the cases (15 of 102), osteomyelitis or spondylodiscitis was diagnosed. Only in 27% of the cases (28 of 102), disc protrusion, one of the commonly known underlying diagnoses (14 cases), or higher-grade spondylolisthesis/spondyloptosis (14 cases) were the inciters. Our results suggest that tight hamstring syndrome in childhood can be an initial symptom of an associated, usually severe disease. We conclude that therefore further diagnostic evaluation is required when tight hamstring syndrome is observed. A rapid initiation of an adequate primary therapy could be indicated.
Keywords: Tight hamstring syndrome, Extraspinal tumor, Intraspinal tumor, Spinal osteomyelitis, Tumor-like lesion, Childhood
Introduction
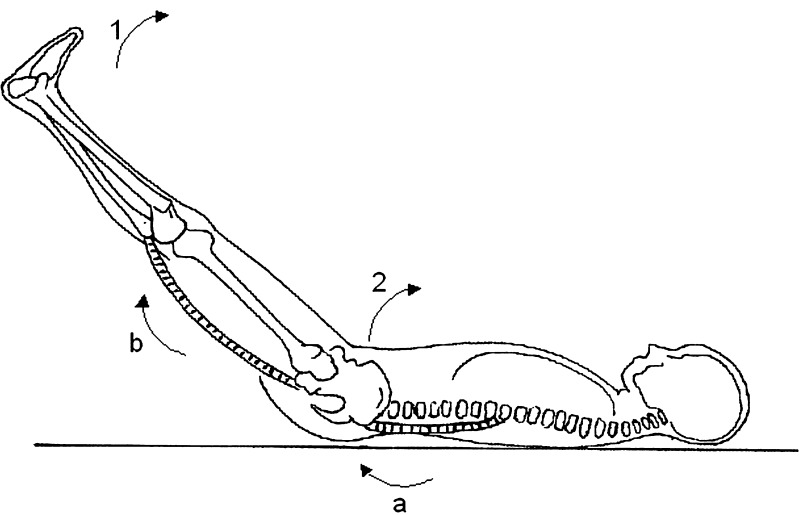
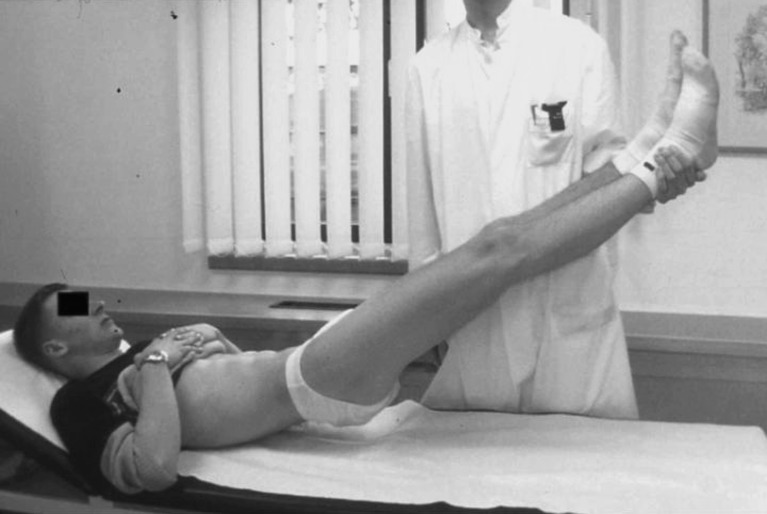
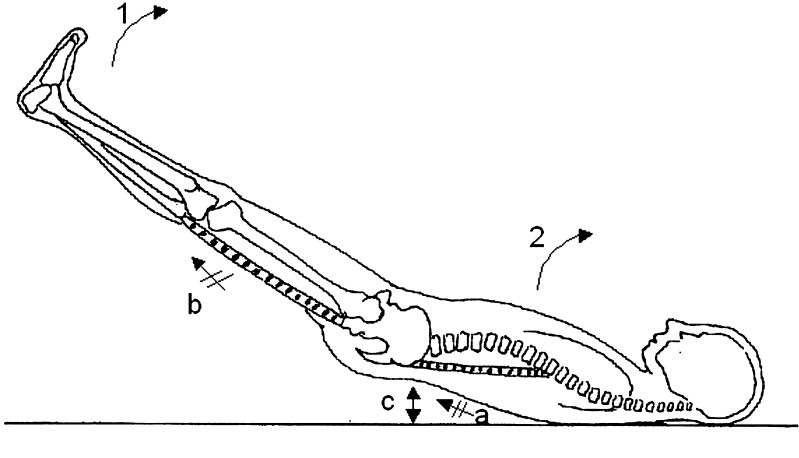
The symptom complex of tight hamstring syndrome (THS) in childhood is very rare and has a varied pathogenesis. Various intra- and extraspinal diseases are considered to be involved in bringing about THS. The clinical symptom complex is induced by 1) a fixed contraction of the lumbar, ischiocrural and gluteal musculature which 2) fixes the lumbar vertebral column and the hip joints typically in an extended position when the full extended leg is lifted up [Figs. 1, 2, 3], and 3) frequently results into a typical waddling gait (shifting gait) as well as a fixed scoliosis. The symptom complex usually exists bilaterally and can still be experienced under anaesthesia [16]. Even with extensive symptoms, complaints are usually indistinct. Since its first description by Stork in 1935 [17], this condition has been attributed to a number of disorders [Table 1]. Krämer [9] and others [6, 11, 14] argue that THS is determined in the majority of cases by a protruding or slipped vertebral disc. However, THS in childhood can also be an initial symptom of a usually severe disease [6, 10], which therefore requires further diagnostic evaluation.
Fig. 2.
Normal muscular lengthening (lumbar muscles (a), ischiocrural musculature (b)) when the full extended leg is lifted up (1). Flexion of the lumbar spine and of the hip joint (2). Modified figure according to STORCK, 1932 [2]
Fig. 1.
Tight hamstrings syndrome, clinical presentation of a 16-year-old boy (underlying disease: intraspinal lipoma)
Fig. 3.
Tight hamstrings syndrome Contraction of the lumbar (a) and ischiocrural (b) musculature which fixes the lumbar spine and the hip joints typically in a extended position when the full extended leg is lifted up (1). The entire trunk is lifted from the ground (c). Modified figure according to STORCK, 1932 [2]
Patients and Methods
In this multicenter study we reviewed retrospectively every case of THS in childhood presented to our three clinics (Magdeburg (32), Bad Berka (6), and Berlin (64)) in the past 22 years. All patients were diagnosed clinically with the help of a standardised evaluation. We recorded the following clinical criteria:
fixed contraction of the lumbar, ischiocrural and gluteal musculature
fixed lumbar vertebral column and hip joints when the full extended leg is lifted up
typical waddling gait (shifting gait)
fixed scoliosis.
There were 102 such children with various underlying diagnosis. The average age when the children became afflicted was 10.5 years (3–17 years). Fifty four of the children were female and 48 were males. At the time of hospitalisation, all children had sought medical attention because they had suffered restrictions of mobility, related particularly to impairments in walking and standing. Clear neurologic deficits relating to a radicular syndrome did exist in 14 children with herniated lumbar discs. However, the average duration of symptoms related with THS (e.g. gait abnormalities, pain and stiffness of the lumbar spine) and the time when patients appear in the hospital was 19 (9–41) days.
Results
All children showed a fixed contraction of the lumbar, ischiocrural and gluteal musculature which fixes the lumbar vertebral column and the hip joints typically in an extended position when the full extended leg is lifted up. A typical waddling gait (shifting gait) and a fixed scoliosis resulted in 88 and 64 children (89.8%, 65.2%), respectively. Seventy four of the 102 children (73%) with THS suffered from a severe or disabling underlying disease (Table 1). In 38 cases (37%), a tumor or a tumor-like lesion was observed. With seven children (7%), the diagnosis of a spinal Langerhans cell histiocytosis was confirmed. Amongst the four children (4%) with Ewing’s sarcoma [Figs. 4 and 5], the THS still persisted despite regression of local findings. Amongst the other 27 cases, we found five patients (5%) with an osteoid osteoma of the vertebral body, five with a spinal ependymoma (5%) of the filium terminale, four (4%) with an epidural lipoma, four (4%) with a leukemia focus, three (3%) with a fibrosus bone dysplasia (Jaffé-Lichtenstein), three (3%) an arachnoidal cyst and three (3%) with an aneurysmal bone cyst. Local osteomyelitis or spondylodiscitis was diagnosed on 15 separate occasions (15%). In 14 cases (14%) a slipped disc was observed. In 14 cases (14%), a higher-grade sondylolisthesis of the last lumbar segment was diagnosed (Table 1).
Table 1.
Our own sample of patients suffering from THS (n=102)
| Underlying Disease | Localisation | Number of cases observed |
|---|---|---|
| Slipped lumbar disc | L4/5=4, L5/S1=10 | 14 |
| Spondylolisthesis or spondyloptosis | L5/S1 | 14 |
| Fractures | L3=2, L4=4, L5=2, S1=1 | 9 |
| Langerhans’ cell histiocytosis | L3=2, L4=2, S1=3 | 7 |
| Spondylodiscitis | L1/2=2, L2/3=2, L4/5=4, L5/S1=1 | 9 |
| Osteomyelitis, facet joint | L4/5=4, L5/S1=2 | 6 |
| Osteoid osteoma | L3=2, L4=3 | 5 |
| Spinal ependymoma | lumbal | 5 |
| Epidural lipoma | L3/4=2, L4/5=2 | 4 |
| Ewing’s sarcoma | L5=2, pelvis, sacrum | 4 |
| Leukemia focus | lumbar spine | 4 |
| Arachnoidal cyst | L3=1,L5=2 | 3 |
| Meningitis | 3 | |
| Spinal stenosis | L4/5=3 | 3 |
| Aneurysmal bone cyst | L2=1, L5=2 | 3 |
| General fibrous bone dysplasia | lumbar spine | 3 |
| Myositis | lumbar errector muscle | 2 |
| General angiomatosis | 1 | |
| Dysplasia of the vertebral arch | L5 | 1 |
| Sacral meningocele | L5/S1 | 1 |
| Chordoma | L4/5 | 1 |
Fig. 4.
Tight hamstrings syndrome, Ewing’s sarcoma of the left iliac bone, X-ray of the pelvis anterior to posterior
Fig. 5.
MRT of 4) with illustration of soft tissue infiltration by the tumor
Discussion
After the first description of the symptom complex of THS by Stork et al. in 1935 [16] and the introduction of this term by Fürmaier et al. in 1947 [3], the first detailed description of the process was provided by Güntz [5]. An inflammatory state always played a decisive role in generating the symptom complex [3, 8, 16]. Subsequent reports emphasised the broadly diversified underlying diseases of THS [2, 7, 10, 11, 15]. There is broad agreement today with the assumption that the clinical symptom complex is determined by a fixed contraction of the lumbar, ischiocrural and gluteal musculature which fixes the lumbar spine and the hip joints typically in an extended position [8–11]. Hauberg et al. [7] drew a comparison with segmentally delimited, pain-reflecting muscle fixation. A fixed scoliosis and a typical waddling gait often exist. Even with extensive symptoms, however, complaints are usually indistinct.
Publications about the THS syndrome can occasionally be found in the German and Japanese literature; however, most of them are case reports. The terminology regarding this symptom complex is not yet standardised. “Fixed lumbar lordosis”, “flat back syndrome”, and “lumbofemoral extension rigidity” are normally used to describe the symptom complex in the English literature, whereas “Hüftlendenstrecksteife” or “Lendenstrecksteife” as well as “fixed lumbar lordosis” is applied in the German literature [6, 9, 12]. “Tight hamstring syndrome” associated with spondylolisthesis was used by Phalen and Dickson in 1960 [13]. Martens et al. [10] used the same term and described various underlying pathologies. However, the described clinical symptoms often differ. In this study, the term “tight hamstring syndrome—THS” is used since it describes the most obvious feature of the symptom complex. Current data suggest that reflexogenic muscular reactions due to irritation of the lumbar nerve roots, the dorsal and medial branches of lumbar nerves as well as the meningeal branch of spinal nerves could be responsible for the syndrome. However, final neuro-physiological proof still needs to be delivered in order to confirm this hypothesis. Based on our observations here, one could argue that the local irritation of these branches of the lumbar spinal nerves (tumorous, inflammatory, mechanically) might be the cause of the reflexogenic muscular reactions and the resulting accelerated tonus of the lumbar, ischiocrural and gluteal musculature. This could explain the clinical pattern of the syndrome namely an inability of hip flexion and lumbar motion, especially movement pertaining to lumbar kyphosis in case of a full extended knee joint. Consequently, the entire trunk is lifted from the ground when the full extended leg is lifted up [Figs. 1–3]. This phenomenon would suggest that the term “wood board syndrome” should be better used in cases of tight hamstring syndrome. However, there is a list of suggested causative factors underlying the genesis of the symptom complex published in recent years e. g. by Hähnel et al. [6] or Martens et al. [10]. Krämer [9] and others [2, 10, 14] published cases of THS which were mainly determined by slipped or protruded discs. Together with Matzen and Polster [11], Krämer [9] deduced that there was an anatomically defined special form of lumbar syndrome in youths. In our study, a distinct accumulation of tumors and tumor-like diseases was observed amongst the population of diseased patients, suggesting that those tumors are either associated with the syndrome or are the cause of the syndrome. Tumours represented the most frequent association with THS. The second most frequent observation, albeit at a far lower incidence, was represented by inflammatory modifications. Only 14 children with THS revealed a slipped disc and a spondylolisthesis, respectively. A number of discrepancies with other authors were apparent regarding this point. However, considering the rarity of the symptom complex, no greater incidence of the disease should be expected even in larger studies.
Unfortunately, our study as well as previous studies lack the needed amount of epidemiological and physiological data to differentiate between a factor that is associated with the syndrome or that is the underlying cause of the syndrome. Clearly, different types of studies are needed to understand the cause of THS. However, that we observe specific tumors or tumor-like diseases in 37% of the THS cases in our study, which is the largest such study available so far, is remarkable and needs to be considered in the clinical management of THS (see conclusions below).
Since it is common knowledge that the prognosis of an underlying tumorous disease depends considerably on the timepoint of diagnostic evaluation, we are of the opinion that when a THS appears, the presence of any underlying cancerous disease should be ruled out as soon as possible. It is also known that tumors and tumor-like lesions in the area of the lumbar spine, especially when other symptoms are lacking, can manifest themselves exclusively in the form of a THS [1, 4, 12, 15]. In the area of strict differentiation between ward and ambulant treatment, the THS described by Krämer [9] as an early form of syndrome in youths might not have represented grounds for hospitalisation, so that this form might have escaped evaluation in our study. Our study does allow us to state, however, that for the most part severe and disabling diseases underlay the THS, and that these often had to be treated surgically. Malignant tumors are frequently causally associated with a THS. We are certainly aware of the fact that there could be other reasons for THS e.g. neuromuscular diseases not observed in our study simply because those patients would not be seen by an orthopaedic surgeon.
Conclusion
Based on our data set, which represents the largest collection of patients with tight hamstring syndrome currently available, we recommend a rapid-as-possible evaluation of the underlying basis of this symptom complex using all available imaging procedures, including laboratory investigations, X-ray, radioisotope imaging, CT scanning and MRT investigations. If diagnostic uncertainty persists, invasive procedures should be employed wherever necessary to clarify the situation. Despite the improved outpatient diagnostics, THS still remains an indication for hospitalisation since any delay might lead to a further unobserved growth of a malignant tumor. Furthermore, with a longer prevalence of a THS, a risk also exists for real contractures appearing in the lumbar spine and the hip region, the treatment of which is much more complicated than a rapid initiation of an adequate primary therapy. Although not all cases of THS are caused by a severe underlying disease such as malignant tumors, the fact that a considerable fraction of THS cases clearly, as shown here, should be seen as reason for drawing special attention to all THS patients to investigate the underlying disease of the symptom complex involving the tight hamstring syndrome.
Contributor Information
Ralph Kayser, Phone: +49 30 8445 64 9614, FAX: +49 30 8445 4464, Email: Ralph.Kayser-Berlin@t-online.de.
Konrad Mahlfeld, Phone: +49 391 6714000, FAX: 49 391 6714006.
Christoph E. Heyde, Phone: +49 36458 50, FAX: +49 36458 42180
Holger Mellerowicz, Phone: +49 30 8102 1131, FAX: +49 30 8102 1133.
References
- 1.Berger G. The symptom “Hüft-Lendenstrecksteife”. Chir Prax. 1990;42:717–726. [Google Scholar]
- 2.Fen G. “Hüftlendenstrecksteife”–a report of 100 cases. J Jpn Orthop Ass. 1982;56:791–796. [PubMed] [Google Scholar]
- 3.Fürmaier A.The “Hüft-Lenden-Strecksteife” Chirurg 195122183–184.14822116 [Google Scholar]
- 4.Graf R. Aetiology of the “Hüft-Lendenstrecksteife”: The lumbal dermoid. Z Orthop. 1982;120:770–773. doi: 10.1055/s-2008-1051394. [DOI] [PubMed] [Google Scholar]
- 5.Güntz E (1958) The clinical examination of the spine. In: Hohmann G (ed) Handbuch der Orthopädie, vol. 2, 2nd edn. Thieme Stuttgart, p 42
- 6.Hähnel H, Pfeiffer U, Marks P. The “Hüft-Lenden-Strecksteife”—Equivalent of sciatica in adolescents. Beitr Orthop Traumatol. 1988;35:294–305. [PubMed] [Google Scholar]
- 7.Hauberg G. Causes and treatment of “Lendenstrecksteife”. Verh Dtsch Orthop Ges. 1957;88:444–446. [Google Scholar]
- 8.Hohmann G, Güntz E. Unilateral inflammatory bone changings of lumbar articular processes as a cause of severe movement disorders. Z Orthop. 1937;66:115–130. [Google Scholar]
- 9.Krämer J (1997) Discogenic “Hüft-Lenden-Strecksteife”. In: Krämer J. Bandscheibenbedingte Erkrankungen. 4th edn. Thieme Stuttgart, pp 217–219
- 10.Martens G, Hoogmartens M, Vanisegheim J. Tight hamstring syndrome. Acta Orthop Belgica. 1981;47:560–569. [PubMed] [Google Scholar]
- 11.Matzen PF, Polster J. The symptom complex “Hüft-Lenden-Strecksteife”. Arch Orthop Unfallchir. 1960;51:399–409. doi: 10.1007/BF00415134. [DOI] [Google Scholar]
- 12.Mau H. “Hüft-Lendenstrecksteife”. Therapiewoche. 1981;31:1840–1845. [Google Scholar]
- 13.Phalen GS, Dickson JA. Spondylolisthesis and tight hamstrings. J Bone Joint Surg. 1961;43(A):505–512. [Google Scholar]
- 14.Polster J, Buesenez EK. Causes and significance of the symptom “Hüft-Lenden-Strecksteife”. Orthop Praxis. 1972;11:273–278. [Google Scholar]
- 15.Schramm G. Unilateral inflammatory bone changings of lumbar facet joints as a cause of severe movement disorders. Verh Dtsch Orthop Ges. 1937;67:274–277. [Google Scholar]
- 16.Seyfarth H. Hüft-Lenden-Strecksteife (1982) In: Matzen PF (ed) Orthopädie, vol 2, 3rd edn. Volk und Gesundheit Berlin, pp 747–750
- 17.Stork H. Contracture of the lumbar spine and its relationship to body bearing and movement. Verh Dtsch Orthop Ges. 1935;62:102–107. [Google Scholar]