Abstract
The aim of the study is to determine if leg pain can be caused by contralateral lumbar disk herniation and if intervention from only the herniation side would suffice in these patients. Five patients who had lumbar disk herniations with predominantly contralateral symptoms were operated from the side of disk herniation without exploring or decompressing the symptomatic side. Patients were evaluated pre- and postoperatively. To our knowledge, this is the first reported series of such patients who were operated only from the herniation side. The possible mechanisms of how contralateral symptoms predominate in these patients are also discussed. In all patients, the shape of disk herniations on imaging studies were quite similar: a broad-based posterior central–paracentral herniated disk with the apex deviated away from the side of the symptoms. The symptoms and signs resolved in the immediate postoperative period. Our data clears that sciatica can be caused by contralateral lumbar disk herniation. When operation is considered, intervention only from the herniation side is sufficient. It is probable that traction rather than direct compression is responsible from the emergence of contralateral symptoms.
Keywords: Contralateral symptoms, Disk herniation, Lumbar, CT, MRI
Introduction
During the workup of a patient with leg pain, finding a contralateral disk herniation without any significant abnormality on the ipsilateral side on imaging studies is a dilemma for a doctor. He is faced with the problem of deciding whether or not the presenting symptoms are related to the herniated disk. In such a situation, the spinal surgeon fears to offer operation due to the risk of failed back surgery syndrome and he either withholds surgery or chooses to explore both sides of the spinal canal not to miss a lesion that might be responsible for the symptoms. However, exploring the side without lesions on imaging studies in addition to diskectomy not only increases the operation time, but also doubles complication risks. Several authors have reported on patients with lumbar herniated disks and contralateral symptoms who recovered after operation, but all of them had operated the patients from both sides of the canal [2, 4, 5]. Therefore, in these cases, it is not possible to make sure that relief of symptoms were related only to removal of herniated disks; decompression at the symptomatic side might have also influenced the recovery.
We present a series of five patients with lumbar herniated disks and contralateral symptoms. In all patients, herniated disks were removed without intervention to the contralateral side. To our knowledge, this is the first reported series of such patients who were operated only from the herniation side. The possible mechanisms of how contralateral symptoms predominate in these patients are also discussed.
Materials and methods
Over the last 7 years, the neurosurgeon (HKS) has operated on five patients who had disk herniations with predominantly contralateral symptoms. All patients were operated from the side of disk herniation without exploring or decompressing the other side. They were evaluated preoperatively by neurological examination, imaging studies (computed tomography—CT, and/or magnetic resonance imaging—MRI), and in one patient by electromyography (EMG). Symptoms and signs of patients were evaluated in the immediate as well as in the late postoperative period (1–3 years of follow-up). The symptoms, findings of neurological examinations and imaging studies, operative data, and early and late postoperative evaluation data of all patients are listed in Table 1.
Table 1.
Pre-operative and postoperative evaluation of all patients
| Age, sex | Pre-operative evaluation | Imaging findings | Operation | Early postoperative evaluation | Late postoperative evaluation | ||||
|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Neurologic exam | Symptoms | Neurologic exam | Symptoms | Neurologic exam | ||||
| 1 | 45, F | LBP for 1 year and right leg pain for 3 weeks | Right Lasegue (+) at 60–70° Left contralasegue (+) at 80–90°, Paresthesia–hypoesthesia of right foot. Scoliosis (tilt toward right side), marked muscle spasm on the left side. |
CT: L5-S1 posterior central and left paracentral disk herniation EMG: Right S1 radicular involvement |
Left L5 partial laminectomy; diskectomy from left | No symptoms | Normal | After 3 years | |
| No symptoms at routine life. Mild right leg pain after intense physical activity. | Right L5 paresthesia | ||||||||
| 2 | 35, F | LBP for 7 years and left leg pain for 2 years | Left Lasegue (+) at 70° | CT: L4–5 posterior central and right paracentral disk herniation | Right L4 lower partial laminectomy; diskectomy from right | No symptoms | Normal | After 3 years | |
| No symptoms | Normal | ||||||||
| 3 | 40, F | LBP for 11 months and bilateral leg pain. Right > Left for 10 months | Normal | MRI: L4–5 posterior central and left paracentral disk herniation | Left L4 partial laminectomy; diskectomy from left | No symptoms | Normal | After 2.5 years | |
| No symptoms | Normal | ||||||||
| 4 | 42, M | Left leg pain for the last 5 years, which subsided after rehabilitation. Sudden onset of intolerable—intractable right leg pain—in spite of the narcotic medication—1 week ago | Right Lasegue (+) at 20°, Left Lasegue (+) at 40°, Contralasegue (+) bilaterally, unable to walk because of the pain | MRI: L4–5 posterior central and left paracentral disk herniation | Left L4 partial laminectomy; diskectomy from left | Pain subsided, walks normally | Normal | After 2 years | |
| No symptoms | Normal | ||||||||
| 5 | 34, M | LBP and right leg pain 6 years prior, which subsided in a few months. Sudden onset of LBP and right leg pain 4 weeks ago after exercise | Absent right Achille reflex Lasegue bilateral (+) at 60° Hypoethesia in Right L5 dermatomal distribution |
MRI: L4–5 posterior central and left paracentral disk herniation | Left L4 and L5 partial laminectomy; diskectomy from left | No symptoms | Absent Achille reflex | After 1 year | |
| No symptoms | Absent Achille reflex | ||||||||
LBP, low back pain; EMG, electromyography; MRI, magnetic resonance imaging; CT, computed tomography
Results
All patients presented with symptoms and signs that showed dominant involvement of the contralateral side of disk herniations. In all patients, the shape of disk herniations on imaging studies were quite similar: a broad-based posterior central–paracentral herniated disk with the apex deviated away from the side of symptoms (Fig. 1–3). Dural sac was compressed ventrally at and close to midline; however, no direct compression was noted on the nerve root at the side of symptoms. There were also no signs of bony or ligamentous compression on nerve roots or dural sac. Partial unilateral laminectomy–facetectomy and removal of disk herniations were performed in all patients without exploring the contralateral side. The symptoms and signs resolved in the immediate postoperative period. Almost complete recovery was achieved in all patients in the follow-up examinations performed at 1–3 years after operation. No postoperative complications were encountered.
Fig. 2.
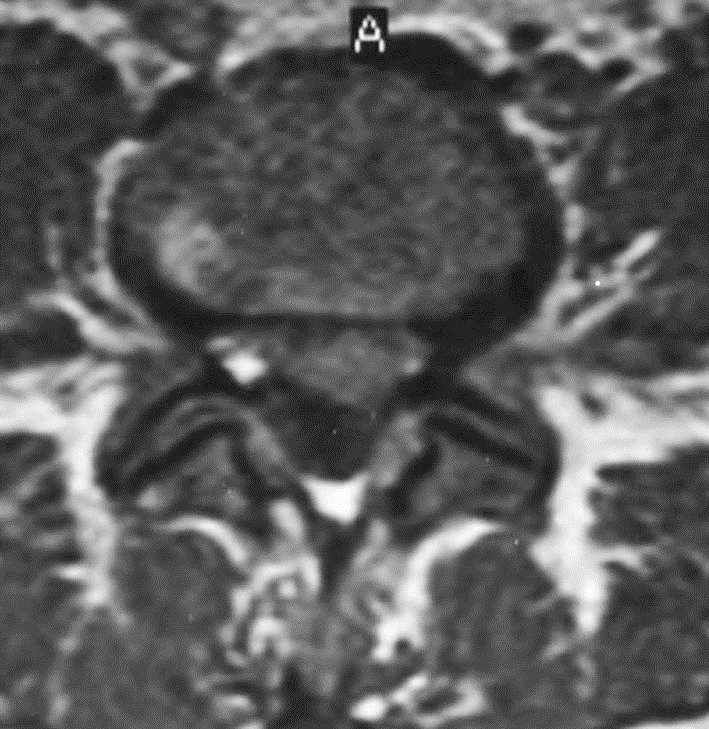
Case 3: 40-year-old female presented with low back pain and bilateral leg pain which was more prominent on the right side. The symptoms had started 11 months prior. MRI shows L4–5 posterior central and left paracentral disk herniation with the apex deviated to the left. Neither of the nerve roots are directly compressed. It may be assumed that an increased traction force is applied on the right L5 root than on the left L5 root
Fig. 1.

Case 1: 45-year-old-female patient presented with right leg pain which had started 15 days prior. She also had a history of low back pain for the last 1 year. CT shows L5–S1 posterior central and left paracentral disk herniation with the apex slightly deviated to the left
Fig. 3.
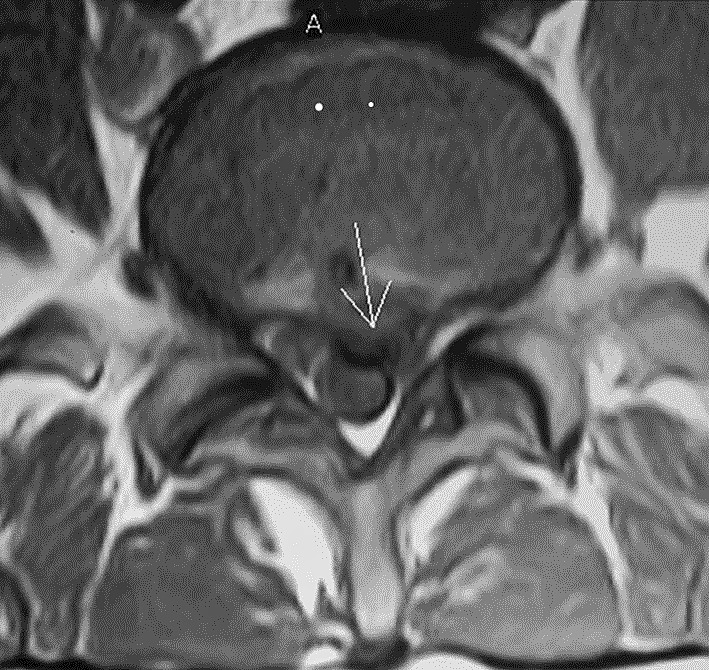
Case 4: 42-year-old male has had a history of left leg pain for the last 5 years, which subsided after rehabilitation. He presented with sudden onset of right leg pain starting 1 week prior. MRI shows L4–5 posterior central and left paracentral disk herniation. The apex of herniation is slightly deviated to the left
Discussion
The presence of a herniated disk on an imaging study does not guarantee that it is the cause of the patient’s symptoms; the cause of leg pain might be lying elsewhere. It is well known that occurrence of herniated disks in asymptomatic subjects is not uncommon. Many authors have shown the presence of disk herniations in asymptomatic individuals on myelography, CT, MRI, and diskography [1, 3, 7–9]. Jensen et al. have evaluated MRI of 98 asymptomatic subjects and have found that 52% of subjects had bulging at at least one level, 27% had a protrusion, and 1% had an extrusion [3]. They have concluded that discovery by MRI of bulges or protrusions in people with low back pain may frequently be coincidental. The question of whether or not the herniated disk is the cause of the patient’s presenting symptoms becomes even more challenging when the imaging studies show a herniated disk on the opposite side of the leg pain. Although it is not rare to see a patient with disk herniation and contralateral symptoms in daily practice, the practicing doctor is often confused, because of the fact that a disk herniation may cause dominantly contralateral symptoms has not yet been cleared in the literature. Only a few authors have reported on such patients, but none have presented a series in which they had operated the patients only from the herniation side to prove that the herniated disk is the cause of contralateral symptoms. Choudhury et al. have presented three cases of lumbar radiculopathy contralateral to an upper lumbar disk herniation. They have explained the syndrome by the prominence of spondylotic changes and stenosis contralateral to the side of disk herniation and have performed total laminectomy and facetectomy at at least two levels as well as removal of herniated disks [2]. Kornberg has reported on four patients with disk herniation, contralateral sciatica, and no evidence of lumbar spondylosis [4]. In addition to diskectomy, he has explored the symptomatic nerve roots including removal of portions of inferior and superior facets on that side. In the series of Mirovsky et al., out of five patients with eccentric compression of the spinal canal causing dominantly contralateral side symptoms, three patients had compression at the lumbar spine. They have performed diskectomy and have removed ligamentum flavum and lamina from both sides of the canal and have explored both nerve roots for any disk fragments [5].
In our series, we chose to approach only through the herniation side without intervention to the contralateral symptomatic side. Resolution of symptoms and signs in all of our patients after operation proves that lumbar disk herniations can cause dominantly contralateral symptoms, and that our approach is sufficient and intervention to the contralateral side is unnecessary. This information cannot be deduced from the series of other authors [4, 5], since they had explored and decompressed the symptomatic side in addition to diskectomy. Our data suggests that performing laminectomy or facetectomy to explore the symptomatic nerve cannot be justified when there is no evidence of disk herniation or spinal stenosis on that side. Although unilateral intervention has been suggested by Mirovsky et al. [5], they have performed operation from both sides of lumbar spinal canal. Operation from the symptomatic side, where there is no lesion on imaging studies, is unnecessary and may be harmful to the patient. We certainly do not advocate to operate on every contralateral herniated disk just as it is not advocated to operate on every ipsilateral disk herniation. We suggest that when a herniated disk is encountered on the opposite side of symptoms, the patient should be managed as if the disk were on the side of symptoms: If the size, shape of the disk, compression of the radix or dural sac, or the patient’s neurologic findings justify operation, the operation should be performed. In patients with disk herniations on the correct and opposite side of symptoms, the decision for operation should be made taking the same issues into consideration. After an operation is justified, when we have no suspicion that the features of herniated disk would cause the patient’s symptoms if it had been on the correct side instead of being on the opposite side, and when we cannot find any other lesion that would explain the symptoms, we plan to operate only from the herniation side.
It is not clear why the symptoms and signs are dominantly on the contralateral side of disk herniations in some patients. While Mirovsky et al. [5] have had no explanation for it, Kornberg has suggested that absence of the dural attachments to the posterior longitudinal ligaments that fix the lumbar nerve roots at some levels might explain the situation [4, 6]. He has suggested that in the absence of the dural ligaments, the ipsilateral nerve root can simply be displaced posteriorly without being compressed significantly, while the contralateral nerve root is shifted laterally into the lateral recess, where it is exerted to significant contact force. We hypothesize that the contralateral findings may be related to traction forces rather than contact forces. When the projection of the apex is at the midpoint of the base of a paramedian disk herniation (symmetric disk herniation), the traction generated on both nerve roots is expected to be equal (Fig. 4a). However, when the apex of herniation is deviated laterally (laterally skewed disk herniation), the traction generated on the contralateral nerve root is expected to be more than that on the ipsilateral nerve root (Fig. 4b). Indeed, in all of our patients, there were posterior central–paracentral disk herniations with the apex deviated away from the symptomatic side. In all four cases of Kornberg [4] and one case of Mirovsky et al. [5] with given figures, the herniated disks had configurations similar to ours. The increased traction on the contralateral nerve root might have caused sciatic pain. The absence of pain on the ipsilateral nerve root might be explained by the location of herniation: when the disk herniation is slightly paramedian, as in our cases, the ipsilateral nerve root is not directly compressed, and there is lesser probability for the nerve root to be compressed between the disk and articular facet–ligamentum flavum complex than it would happen in a more laterally directed disk herniation. All laterally skewed paramedian lumbar disk herniations may not produce contralateral symptoms; however, we believe that our hypothesis regarding traction forces could explain the mechanism of contralateral symptoms in at least some of the patients with herniated disks.
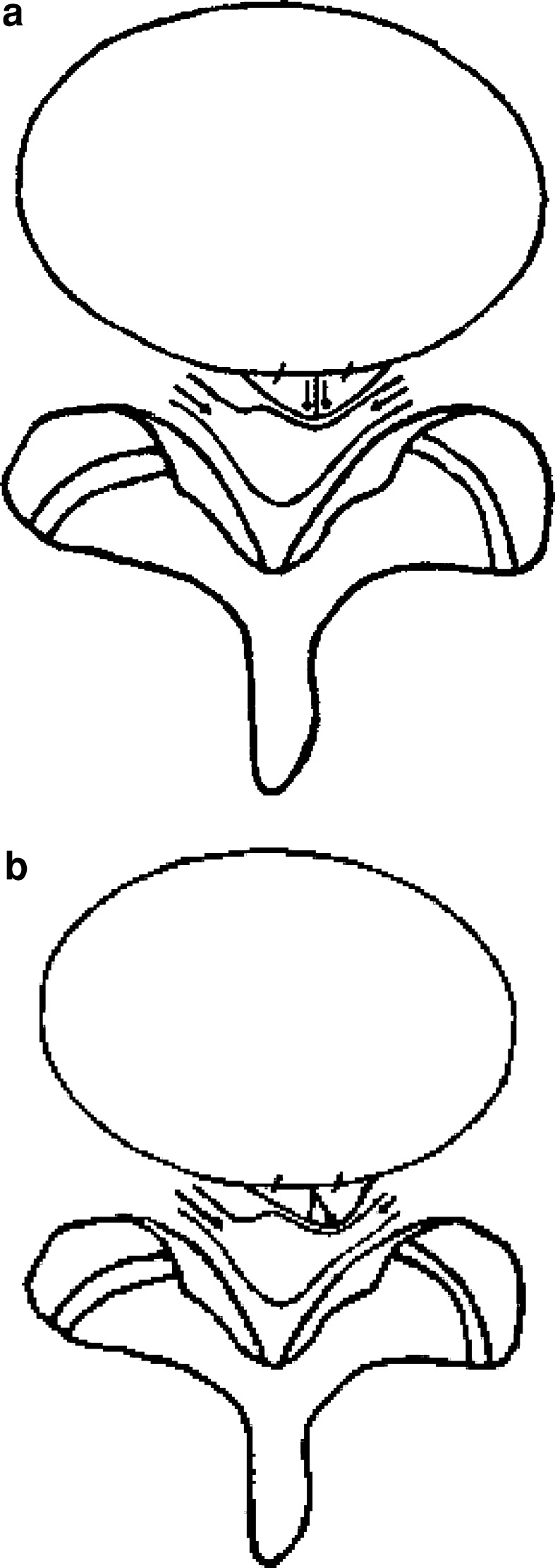
Fig. 4.
Schematic drawings showing that dominance of the contralateral findings may be related to traction forces in some patients. a When the projection of the apex is at the midpoint of the base of a disk herniation, the traction generated on both nerve roots is expected to be equal. b However, when the apex of herniation is deviated laterally, the traction generated on the contralateral nerve root is more than that on the ipsilateral nerve root
Although patients with unilateral leg pain and contralateral disk herniations are occasionally encountered, the incidence of such patients is not known. Unfortunately, we do not have statistical data regarding how often those patients are seen; this would, however, be interesting to know.
Conclusion
Our study clearly shows that sciatica can be caused by contralateral lumbar disk herniation. When operation is considered, intervention only from the herniation side is sufficient. It is probable that traction rather than direct compression is responsible for the emergence of contralateral symptoms.
Footnotes
A reviewer’s comment on this paper is available at http://dx.doi.org/10.1007/s00586-005-0982-7
References
- 1.Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72:403–408. [PubMed] [Google Scholar]
- 2.Choudhury AR, Taylor JC, Worthington BS, Whitaker R. Lumbar radiculopathy contralateral to upper lumbar disc herniation: report of 3 cases. Br J Surg. 1978;65:842–844. doi: 10.1002/bjs.1800651205. [DOI] [PubMed] [Google Scholar]
- 3.Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69–73. doi: 10.1056/NEJM199407143310201. [DOI] [PubMed] [Google Scholar]
- 4.Kornberg M. Sciatica contralateral to lumbar disk herniation. Orthopedics. 1994;17:362–364. doi: 10.3928/0147-7447-19940401-12. [DOI] [PubMed] [Google Scholar]
- 5.Mirovsky Y, Halperin N. Eccentric compression of the spinal canal causing dominantly contralateral-side symptoms. Spinal Disord. 2000;13:174–177. doi: 10.1097/00002517-200004000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Spencer DL, Irwin GS, Miller JA. Anatomy and significance of fixation of the lumbosacral nerve roots in sciatica. Spine. 1983;8:672–679. doi: 10.1097/00007632-198309000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Walsh TR, Weinstein JN, Spratt KF, Lehmann TR, Aprill C, Sayre H. Lumbar discography in normal subjects. A controlled, prospective study. J Bone Joint Surg Am. 1990;72:1081–1088. [PubMed] [Google Scholar]
- 8.Wiesel SW, Tsourmas N, Feffer HL, Citrin CM, Patronas N. A study of computer-assisted tomography. I. The incidence of positive CAT scans in an asymptomatic group of patients. Spine. 1984;9:549–551. [PubMed] [Google Scholar]
- 9.Wilberger JE, Jr, Pang D. Syndrome of the incidental herniated lumbar disc. J Neurosurg. 1983;59:137–141. doi: 10.3171/jns.1983.59.1.0137. [DOI] [PubMed] [Google Scholar]