Abstract
Microendoscopic discectomy (MED) has been accepted as a minimally invasive procedure for lumbar discectomy because of the small skin incision and short hospital stay required for this surgery. However, there are few objective laboratory data to confirm the reduced systemic responses in the early phase after this procedure. In order to substantiate the reduced invasiveness of MED compared to microdiscectomy (MD) or procedures involved in one-level unilateral laminotomy, the invasiveness of each surgical procedure was evaluated by measuring serum levels of biochemical parameters reflective of a post-operative inflammatory reaction and damage to the paravertebral muscles. Thirty-three patients who underwent lumbar discectomy or one-level unilateral laminotomy (MED in 15 cases, MD in 11 cases and one-level unilateral laminotomy in 7 cases with lumbar spinal canal stenosis) were included in this study. The serum levels of C-reactive protein (CRP) and creatine phosphokinase (CPK) were measured at 24 h after operation. Interleukin-6 (IL-6) and Interleukin-10 (IL-10) were measured at 2, 4, 8 and −24 h following the surgery to monitor the inflammatory response to the respective surgery. The post-operative serum CRP levels from both the MD and MED groups were significantly lower than those from the open laminotomy group. However, there was no significant difference in these serum levels between the MED and MD groups. The levels of IL-6 and IL-10 in the MED group during0 the first post-operative day were also significantly lower than those in the laminotomy group. When the MED and MD groups were compared, the IL-6 levels in the MED group were lower than in MD group at 2, 4 and 8 h after surgery, but the differences were not statistically significant. However, the level was significantly lower in the MED group at 24 h after surgery. In terms of IL-10, no significant difference was noted between the MED and MD groups over the study period. The changes in serum levels of post-operative inflammatory: markers (CRP, IL-6 and IL-10) in the early phase indicated reduced inflammatory reactions in MED as well as in MD when compared with classical open unilateral laminotomy. These data draw a direct link between the lower level of the inflammatory response and reduced invasiveness of MED. However, an indicator for muscle damage (CPK) appeared not to be affected by the type of surgical procedure used to correct disc herniation.
Keywords: Microendoscopic discectomy, Microdiscectomy, Lumbar disc herniation, Minimally invasive surgery
Introduction
Lumbar disc herniation is a common spinal disorder and surgical treatment is often indicated in patients who experience severe prolonged pain or significant neurological deficits. Discectomy through a posterior approach is widely performed and is associated with significant surgical insults. This procedure requires a median longitudinal skin incision, detachment of the paravertebral muscles from the spine and partial laminectomy. Advances in microdiscectomy [5] procedures have led to improved methods which are now widely used for the surgical treatment of lumbar disc herniation [1, 6, 20]. The MED system was introduced by Foley in 1997 [11] and has been used for resection of prolapsed and laterally herniated discs. Although this surgical approach requires considerable expertise, the techniques and the tools have been improved and refined to standardize the procedure [4, 8, 9, 10, 12, 14, 17]. Consequently, MED is now the procedure of choice in the field of spinal surgery—the skin incision can be minimized, and extensive detachment of the paravertebral muscle from the spine and laminotomy is not required. The absence of these surgical insults leads to attenuated post-operative inflammatory reactions, including pain and a shortened hospital stay. The reduction in the inflammatory response probably reflects the less invasive nature of this surgical procedure. To test this hypothesis, we measured inflammatory markers in the serum of patients who had been treated surgically for herniated discs using MED, microscopic discectomy (MD) or open unilateral laminotomy. Early recovery from endoscopic surgery has been attributed to reduced local production of pro-inflammatory cytokines such as Interleukin-1 (IL-1), Interleukin-6 (IL-6) or tumor necrosis factor-alpha (TNF-α) [2, 7, 15, 18]. In the present study, we collected laboratory data from patients who were treated surgically with MED for disc herniation. Data from MED patients were compared with similar parameters obtained from herniated disc patients who received open single-level unilateral laminotomy, or another less invasive procedure, microscopic discectomy.
Serum levels of C-reactive protein (CRP), which is produced in the liver and is released into the circulation in response to IL-1 produced at an inflammatory locus, were measured in all patients at 24 h after surgery. In addition, the amplitude of changes in serum levels of the pro-inflammatory cytokine IL-6 and anti-inflammatory cytokine IL-10 were assayed sequentially at 2, 4, 8 and 24 h post-operatively in patients who underwent MED. Measurements from MED patients were compared with data from patients treated with MD or single-level unilateral laminotomy.
In posterior lumbar spinal surgery, the degree of damage to the paravertebral muscles is a possible marker for surgical invasiveness. Therefore, the post-operative undulation in serum levels of CPK released from damaged muscles was adopted as a potential marker to evaluate the surgical invasiveness of MED, MD or open unilateral laminotomy in this study.
Patients
Thirty-three patients (19 men and 14 women) with a mean age of 42.4 years (range 20–72 years) were included in this study. Of these cases, 15 underwent MED and 11 underwent MD. The remaining seven cases had LSCS and received single-level unilateral laminotomy for radicular decompression. These patients were used as surrogates for classical open discectomy associated with partial laminectomy for the purpose of this study.
For this prospective study, MED or MD were randomly assigned to patients requiring surgical treatment for lumbar disc herniation. Gender, age and affected levels in each group are summarized in Table 1. None of these patients received any peri-operative anti-inflammatory or corticosteroid medication.
Table 1.
Patients’ data in this study
| Group | MED | Microdiscectomy | Open laminotomy |
|---|---|---|---|
| Number of cases | 15 | 11 | 7 |
| Gender | |||
| Male | 6 | 8 | 5 |
| Female | 9 | 3 | 2 |
| Age (Mean) | 36.5 | 37.7 | 59.6 |
| Age (Range) | 25–60 | 20–58 | 49–72 |
| Affected levels | |||
| L3/4 | 1 | ||
| L4/5 | 8 | 7 | 6 |
| L5/S | 7 | 3 | 1 |
Methods
Operation time and blood loss were collected from clinical records. Clinical outcomes were assessed according to a scoring system proposed by the Japanese Orthopaedic Association (JOA score) (Table 2). The incidence of persistent low back pain or lumbar discomfort in the MED and MD groups was assessed 1 year after the operation. CRP and CPK levels were measured in blood collected at 24 h after surgery.
Table 2.
Scoring system of the japanese orthopaedic association for low back pain (JOA score)
| 1. Subjective symptoms (9 points) | |||
| A. Low back pain | |||
| None (3) | Occasional mild pain (2) | Frequent mild or occational severe pain (1) | Frequent or continuous severe pain (0) |
| B. Leg pain and/or tingling | |||
| None (3) | Occasional slight symptom (2) | Frequent slight or occational severe symptom (1) | Frequent or continuous severe symptom (0) |
| C. Gait | |||
| Normal (3) | |||
| Able to walk farther than 500 M although it results in pain, tingling, and/or muscle weakness (2) | |||
| Unable to walk farther than 500 M owing to leg pain, tingling, and/or muscle weakness (1) | |||
| Unable to walk farther than 100 M owing to leg pain, tingling, and/or muscle weakness (0) | |||
| 2. Clinical signs (6 points) | |||
| A. Straight leg-raising tests (SLR) (including tight hamstrings) | |||
| Normal (2) | 30–70° (1) | Less than 30° (0) | |
| B. Sensory disturbance | |||
| None (2) | Slight disturbance (not subjective) (1) | Marked disturbance (0) | |
| C. Motor disturbance (MMT) | |||
| Normal (2) | Slight weakness (grade 4) (1) | Marked weakness (Grade 3-0) (0) | |
| 3. Restriction of ADL (14 points) | |||
| Turn over while lying | |||
| Standing | |||
| Washing | No restriction (2) | ||
| Leaning forwards | Moderate restriction (1) | ||
| Sitting (about 1 h) | Severe restriction (0) | ||
| Lifting or holding heavy objects | |||
| Walking | |||
| 4. Urinary Bladder Function (−6 points) | |||
| Normal (0) | Mild dysuria (−3) | Severe dysuria (−6) | |
Recovey rate: (B−A/29−A)×100 (%)
A JOA score at pre-op
B JOA score at the final follow-up
In order to measure cytokine levels, 2 ml of arterial blood was aspirated from the radial artery at 2, 4, 8 and 24 h after the operation through a catheter placed for monitoring blood pressure and respiratory function prior to surgery.
The blood samples were centrifuged to separate serum for the assay of IL-6 and IL-10 using assay kits (BIOTRAK High Sensitivity ELISA system®) with the minimum limit of detection for the assay at 0.1 pg/ml.
Statistical differences between parameters recorded for each group were tested using one-way analysis of variance (ANOVA) and post hoc testing was accomplished using the Bonferroni method. P values less than 0.05 were considered to be significant.
Results
Surgical procedures and clinical outcome
The mean operation times for the MED, MD and laminotomy groups were 119 min (77–207 min), 123 min (59–270 min) and 109 min (60–212 min), respectively. The mean blood loss in the same groups was 26.6 g (10–180 g), 55 g (10–50 g) and 120 g (50–180 g), respectively. The blood loss values in the MED and MD groups were not significantly different, but they were significantly less than that in the laminotomy group.
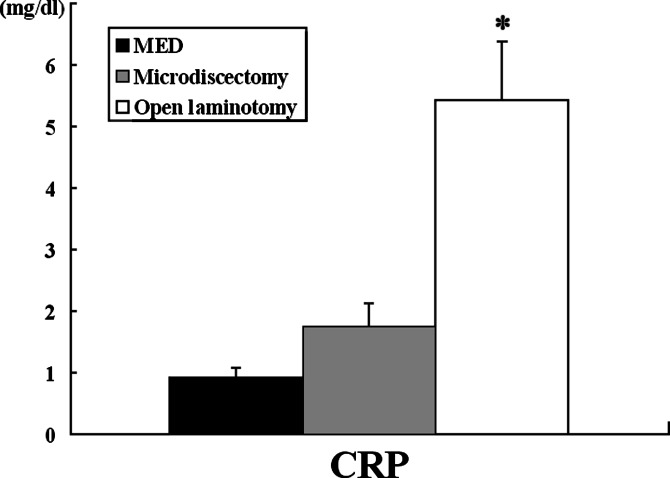
The percentage improvement of the JOA score at final follow-up was 88.6% in the microdiscectomy group and 84.7% in the MED group. This difference was not statistically significant. Residual low back pain or lumbar discomfort was experienced by 66.7% of the MD group and by 36.7% of the MED group. This difference was significant. CRP values at 24 h after surgery in the MED, MD and laminotomy groups were 0.91±0.18 mg/dl, 1.76±0.36 mg/dl and 5.44±0.94 mg/dl, respectively. Although no significant difference was noted between CRP values in the MED and in the MD groups, the CRP level in the laminotomy group was significantly higher than in the other two groups (Fig. 1).
Fig. 1.
CRP values 1 day post-operatively. The mean CRP level in the MED group was 0.91±0.18 mg/dl, 1.76±0.36 mg/dl in the MD group, and 5.44±0.94 mg/dl the open laminotomy group. The MED and MD groups showed statistically lower values compared with the open laminotomy group. No significant differences were observed between the MED and MD groups. *Significantly different from MED group (P<0.05)
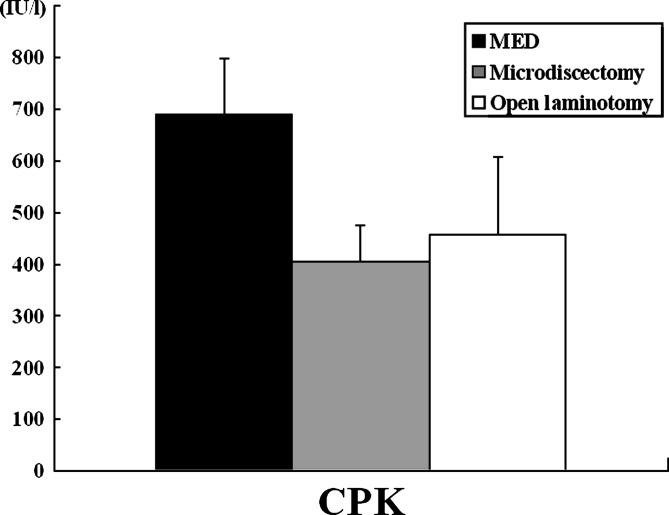
Serum CPK levels at 24 h after surgery tended to be higher in the MED group than in the other groups, but these differences were not statistically significant (Fig. 2).
Fig. 2.
CPK values 1 day postoperatively. CPK in the MED group was 689 IU/l on average. Values for the MD and open laminotomy groups were 406 IU/l, 458 IU/l. There were no significant differences between these three groups
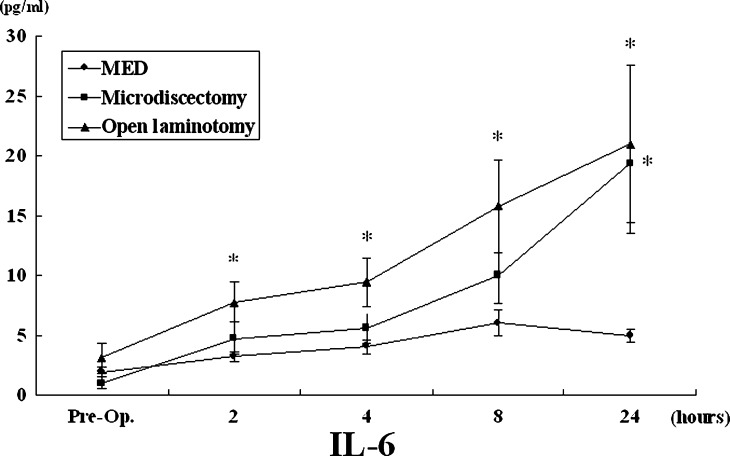
Figure 3 shows sequential changes of serum IL-6 level over the 24 h period after the operation. In the laminotomy group, the level was consistently higher over the 24 h period than in the MED or MD groups. Serum IL-6 levels in the MED and MD groups up to 8 h were not significantly different (6.06±1.06 pg/ml and 10.02±2.43 pg /ml, respectively). However, at 24 h, the IL-6 level in the MD group (19.34±5.75 pg/ml) was significantly higher than in the MED group (4.96±0.54 pg/ml).
Fig. 3.
The change in IL-6 values post-operatively. The values for the open laminotomy group were consistently higher and statistically different from those in the MED group. At 24 h after the operation, the IL-6 level following microdiscectomy was statistically higher than that following MED. *Significantly different from MED group (P<0.05)
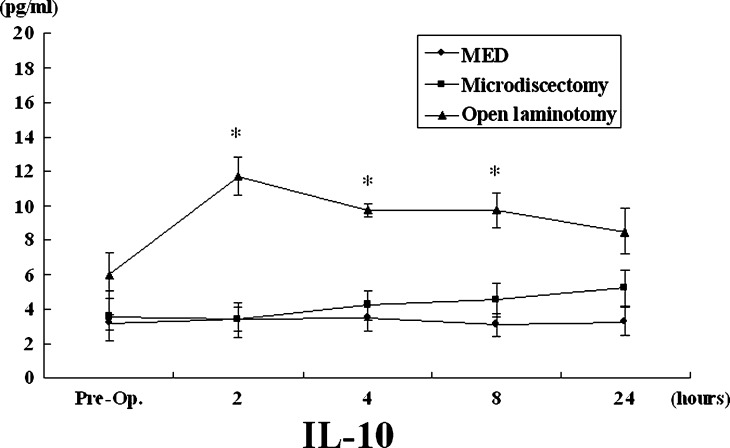
Serum levels of IL-10 over 24 h were also significantly higher in the laminectomy group than in the MED or MD groups. In the MED and MD groups, IL-10 levels remained low with no significant difference observed between these two groups (Fig. 4).
Fig. 4.
The changes in IL-10 levels post-operatively. At each time point, the open laminotomy group showed statistically higher IL-6 values than both the MED and MD groups. Between the MED and MD groups, however, there was no difference detected. *Significantly different from MED group (P<0.05)
The clinical parameters in each group have been summarized in Table 3.
Table 3.
Mean values of clinical parameters
| Group | MED (mean±SE) | Microdiscectomy (mean±SE) | Open laminotomy (mean±SE) |
|---|---|---|---|
| Operation time (min) | 129±11.8 | 123±17.0 | 109±21.5 |
| Blood loss (g) | 26.7±11.3 | 55.0±12.8 | 120±24.3* |
| WBC | 7600±390 | 8200±450 | 7100±460 |
| CRP (mg/dl) | 0.91±0.18 | 1.76±0.36 | 5.44±0.94* |
| CPK (IU/l) | 689±108 | 406±71 | 458±149 |
| IL-6 pre-operation (pg/ml) | 1.93± 0.40 | 1.01±0.47 | 3.09± 1.25 |
| IL-6 2 h (pg/ml) | 3.23±0.44 | 4.76±1.36 | 7.77±1.65* |
| IL-6 4 h (pg/ml) | 4.07±0.59 | 5.59±1.32 | 9.41±2.03* |
| IL-6 8 h (pg/ml) | 6.06±1.06 | 10.02±2.43 | 15.8±3.91* |
| IL-6 24 h (pg/ml) | 4.96±0.54 | 19.34±5.75* | 21.0±6.58* |
| IL-10 pre-operation (pg/ml) | 3.19±0.44 | 3.57±1.45 | 5.95±1.31 |
| IL-10 2 h (pg/ml) | 3.37±0.67 | 3.38±1.01 | 11.71±1.11* |
| IL-10 4 h (pg/ml) | 3.46±0.78 | 4.19±0.86 | 9.74±0.36* |
| IL-10 8 h (pg/ml) | 3.06±0.64 | 4.51±1.00 | 9.70±0.99* |
| IL-10 24 h (pg/ml) | 3.28±0.79 | 5.18±1.06 | 8.47±1.33 |
*P<0.05 versus MED group
Discussion
The results from this clinical study indicated significantly lower levels of the inflammatory markers, CRP [3, 13, 21], IL-6 and IL-10 in the MED and MD groups than in the group treated with open unilateral laminotomy. These data confirm that the MED and MD procedures cause less tissue damage during surgery. Ideally, the appropriate control group for this study should have been patients who received the classical open discectomy associated with partial laminectomy. However, it was not possible to do this because we stopped using this procedure prior to the start of the present study. As an alternative, patients with lumbar spinal canal stenosis requiring unilateral laminotomy without discectomy were enrolled. Therefore, surgical invasiveness in the control group may have differed from patients treated by discectomy with partial laminectomy. We believe that the degree of invasiveness in the control group was similar to the level seen in classical discectomy with partial laminectomy.
The elevation of CRP level in serum has been widely recognized in the post-operative phase, typically peaks between 24 h to 72 h, and is an indicator for the intensity of post-operative inflammatory reactions. Therefore, the low levels of CRP, in the MED and MD groups at 24 h after surgery, are evidences of the lower surgical invasiveness of these surgical procedures when compared with the open laminotomy group. These data are further supported by the lower levels of inflammatory cytokines, IL-6 and IL-10 found in the MED and MD groups when compared with the open laminotomy group.
The IL-6 level at 24 h after surgery in the MD group was significantly higher than in the MED group. Although the reason for this was uncertain, it could mean that MED was less invasive than MD.
IL-10 is an anti-inflammatory agent which has been shown to regulate pro-inflammatory cytokines, including IL-6, at the transcriptional level [19]. The IL-10 level was also elevated in the early post-operative phase, probably as a result of the intense inflammatory reaction. The lower level of IL-10 in the MED and MD groups might also indicate a low level of inflammatory response in these patients.
Another problem encountered with posterior lumbar surgery has been the damage to soft tissues, especially the paravertebral muscles, which often causes persistent post-operative low back pain. In order to quantitate muscular damage, serum levels of CPK of muscle origin (CPK-MM) were measured [16]. Unexpectedly, the mean CPK level in the MED group was higher than in the other two groups, although this difference was not significant. This would indicate that damage to the paravertebral muscles was not minimized by the MED or MD techniques. The MED group showed a lower incidence of persistent post-operative low back pain than the MD group. Therefore, transient elevation of CPK in MED did not influence persistent low back pain.
In conclusion, the less invasive nature of the MED and MD procedures was substantiated by inflammatory markers in serum in the early post-operative phase. Although the post-operative inflammatory reactions were attenuated, the level of a marker for damage to the paravertebral muscles (CPK-MM) was not affected. This did not directly relate to persistent low back pain. However, there may be further opportunities to minimize muscle damage during MED.
References
- 1.Andrews DW, Lavyne MH. Retrospective analysis of microsurgical and standard lumbar discectomy. Spine. 1990;15(4):329–335. doi: 10.1097/00007632-199004000-00015. [DOI] [PubMed] [Google Scholar]
- 2.Baigrie RJ, Lamont PM, Kwiatkowski D, Dallman MJ, Morris PJ. Systemic cytokine response after major surgery. Br J Surg. 1992;79:757–760. doi: 10.1002/bjs.1800790813. [DOI] [PubMed] [Google Scholar]
- 3.Blomqvist L, Malm M, Berg A, Svelander L, Kleinau S. The inflammatory reaction in elective flap surgery. Plast Reconstr Surg. 1998;101(6):1524–1528. doi: 10.1097/00006534-199805000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Brayda-Bruno M, Cinnella P. Posterior endoscopic discectomy (and other procedures) Eur Spine J. 2000;9(Suppl1):S24–S29. doi: 10.1007/PL00010018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Casper W. A new surgical procedure for lumbar disc herniation causing less tissue damage through a microsurgical approach. Advances in Neurosurgery. 1977;4:74–77. [Google Scholar]
- 6.Caspar W, Campbell B, Barbier DD, Kretschmmer R, Gotfried Y. The Caspar microsurgical discectomy and comparison with a conventional standard lumbar disc procedure (discussion 86–87) Neurosurgery. 1991;28(1):78–86. doi: 10.1097/00006123-199101000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Castell JV, Gomez-Lechon MJ, David M. Acute-phase response of human hepatocytes: regulation of acute-phase protein synthesis by interleukin-6. Hepatology. 1990;12(5):1179–1186. doi: 10.1002/hep.1840120517. [DOI] [PubMed] [Google Scholar]
- 8.Destandau J. A special device for endoscopic surgery of lumbar disc herniation. Neurol Res. 1999;21(1):39–42. doi: 10.1080/01616412.1999.11740889. [DOI] [PubMed] [Google Scholar]
- 9.Dirksmeier PJ, Parsons IM, Kang JD. Microendoscopic and open laminectomy and discectomy in lumbar disc disease. Sem Spine Surg. 1999;11:138–146. [Google Scholar]
- 10.Fessler RG. Microendoscopic lumbar discectomy: technical note. Neurosurgery. 2002;51(2):129–136. [PubMed] [Google Scholar]
- 11.Foley KT, Smith MM. Microendoscopic discectomy. Tech Neurosurg. 1997;3:301–307. [Google Scholar]
- 12.Guiot BH, Khoo LT, Fesler RG. A minimally invasive technique for decompression of the lumbar spine. Spine. 2002;27(4):432–438. doi: 10.1097/00007632-200202150-00021. [DOI] [PubMed] [Google Scholar]
- 13.Gunel E, Caglayan O, Caglayan F, Sahin TK. Acute-phase changes in children recovering from minor surgery. Pediatr Surg Int. 1998;14(3):199–201. doi: 10.1007/s003830050700. [DOI] [PubMed] [Google Scholar]
- 14.Huang TJ, Hsu RW, Lee YY, Chen SH. Video-assisted endoscopic lumbar discectomy. Surg Endosc. 2001;15(10):1175–1178. doi: 10.1007/s004640090125. [DOI] [PubMed] [Google Scholar]
- 15.Karayiannakis AJ, Makri GG, Mantzioka A, Karousos D, Karatzas G. Systemic stress response after laparoscopic or open cholecystectomy: a randomized trial. Br J Surg. 1997;84(4):467–471. doi: 10.1046/j.1365-2168.1997.02622.x. [DOI] [PubMed] [Google Scholar]
- 16.Kawaguchi Y, Matsui H, Tsuji H. Changes in serum creatine phosphokinase MM isoenzyme after lumbar spine surgery. Spine. 1997;22(9):1018–1023. doi: 10.1097/00007632-199705010-00015. [DOI] [PubMed] [Google Scholar]
- 17.Khoo LT, Fessler RG. Microendoscopic decompressive laminotomy for the treatment of lumbar stenosis. Neurosurgery. 2002;51(Suppl5):146–154. [PubMed] [Google Scholar]
- 18.Leung KL, Lai PB, Ho RL, Meng WC, Yiu RY, Lee JF, Lau WY. Systemic cytokine response after laparoscopic-assisted resection of rectosigmoid carcinoma: a prospective randomized trial. Ann Surg. 2000;231(4):506–511. doi: 10.1097/00000658-200004000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mahdy AM, Galley HF, Abdel-Wahed MA, el-Korny KF, Sheta SA, Webster NR. Differential modulation of interleukin-6 and interleukin-10 by diclofenac in patients undergoing major surgery. Br J Anaesth. 2002;88(6):797–802. doi: 10.1093/bja/88.6.797. [DOI] [PubMed] [Google Scholar]
- 20.McCulloch JA. Focus issue on lumbar disc herniation: macro- and microdiscectomy. Spine. 1996;21(Suppl24):45S–56S. doi: 10.1097/00007632-199601010-00010. [DOI] [PubMed] [Google Scholar]
- 21.Stahl WM. Acute phase protein response to tissue injury. Crit Care Med Jun. 1987;15(6):545–50. doi: 10.1097/00003246-198706000-00001. [DOI] [PubMed] [Google Scholar]