Abstract
Objectives. We examined whether the risk of premature mortality associated with living in socioeconomically deprived neighborhoods varies according to the health status of individuals.
Methods. Community-dwelling adults (n = 566 402; age = 50–71 years) in 6 US states and 2 metropolitan areas participated in the ongoing prospective National Institutes of Health–AARP Diet and Health Study, which began in 1995. We used baseline data for 565 679 participants on health behaviors, self-rated health status, and medical history, collected by mailed questionnaires. Participants were linked to 2000 census data for an index of census tract socioeconomic deprivation. The main outcome was all-cause mortality ascertained through 2006.
Results. In adjusted survival analyses of persons in good-to-excellent health at baseline, risk of mortality increased with increasing levels of census tract socioeconomic deprivation. Neighborhood socioeconomic mortality disparities among persons in fair-to-poor health were not statistically significant after adjustment for demographic characteristics, educational achievement, lifestyle, and medical conditions.
Conclusions. Neighborhood socioeconomic inequalities lead to large disparities in risk of premature mortality among healthy US adults but not among those in poor health.
Research dating back to at least the 1920s has shown that the United States has experienced persistent and widening socioeconomic disparities in premature mortality over time.1–5 However, it has been unclear whether socioeconomic inequalities affect the longevity of persons in good and poor health equally. Socioeconomic status (SES) and health status are interrelated,6–8 and both are strong independent predictors of mortality.9 Low SES is associated with greater risk of ill health and premature death,1–5,8,10–13 partly attributable to disproportionately high prevalence of unhealthful lifestyle practices10,14,15 and physical and mental health conditions.13,16 Correspondingly, risk of premature mortality is higher in poor than in more affluent areas.16,17 Although the association between neighborhood poverty and mortality is independent of individual-level SES,17,18 aggregation of low-SES populations in poor areas may contribute to variations in health outcomes across neighborhoods. Conversely, economic hardships resulting from ill health may lead persons in poor physical or mental health to move to poor neighborhoods.19 This interrelatedness may create spurious associations between neighborhood poverty and mortality.
Although previous studies have found that the risk of premature death associated with poor health status varies according to individuals' SES,20,21 no published studies have examined whether the relative risks for premature mortality associated with living in neighborhoods with higher levels of socioeconomic deprivation vary by health status of individuals. Clarifying these relationships will inform social and public health policies and programs that aim to mitigate the health consequences of neighborhood poverty.22,23
We used data from a large prospective study to examine whether the risk of premature mortality associated with neighborhood socioeconomic context differs according to health status at baseline and remains after adjustment for person-level risk factors for mortality, such as SES, lifestyle practices, and chronic medical illnesses.
METHODS
Our data came from the ongoing prospective National Institutes of Health (NIH)–AARP Diet and Health Study. The details of the NIH–AARP study, which began in 1995, are described elsewhere.24 The primary goal of the NIH–AARP study is to examine the effect of lifestyle practices on cancer incidence and mortality. The original cohort comprised 567 169 AARP members aged 50 to 71 years at baseline who resided in 6 US states (CA, FL, LA, NJ, NC, and PA) and 2 metropolitan areas (Atlanta, GA, and Detroit, MI). Our analysis excluded participants who died or moved out of a study area before the start date of the NIH–AARP study or withdrew from the study at any point (n = 768), whose date of death was the same as the date of recruitment into the study (n = 12), or who had incomplete or missing geographical information or census measures (n = 710).
Data Collection
Person-level sociodemographic, dietary, lifestyle, and medical history factors.
A questionnaire mailed to participants at baseline (1995–1996) asked about date of birth, gender, marital status, race/ethnicity, level of educational achievement, current body weight and height, and health behaviors, including frequency of vigorous physical activity lasting at least 20 minutes, alcohol use, smoking status and frequency, and medical history. Several components of participants' diet over a previous 12-month period were assessed at baseline with a 124-item food frequency questionnaire.25 Participants were also asked to rate their health status as poor, fair, good, very good, or excellent. The NIH–AARP study also collected data from separate questionnaires mailed in 1996 to 1997 and 2004 to 2006, which included questions about history of hypercholesterolemia or hypertension (n = 334 497) and the occupation of participants' head of household during childhood (n = 317 933), respectively.
Area-level socioeconomic deprivation.
The main predictor in our analyses was neighborhood socioeconomic deprivation. The NIH–AARP study collected information on the residential address of each participant at baseline and transformed (geocoded) this information into geographical coordinates and linked to information collected by the 2000 US Census about the socioeconomic context and racial and ethnic composition of persons within census tracts. Socioeconomic measures obtained at census tract level have been found to be adequate for assessing the health effects of neighborhood socioeconomic context.26
We used the census data to generate an empirical index of neighborhood socioeconomic deprivation, as described previously.27 In brief, we considered for inclusion in the deprivation index 19 variables representing domains of racial/ethnic composition, education, income and poverty, occupation and employment, and housing and residential stability. We performed variable selection with principal component analysis stratified on state of residence to incorporate both unique and common contributors to deprivation across all study areas.27 Only 1 variable was retained in the factor analysis model if 2 or more within the same domain were highly correlated with each other (correlation coefficient ≥ 0.90). We then retained variables for which the 95% confidence interval (CI) of the loadings in all the study's states and metropolitan areas included the median of the lower 95% CI limit of loadings across all study areas, which in our analysis was 0.23 (Table 1).
TABLE 1.
Deprivation Score Loadings for Variables in the Socioeconomic Deprivation Index: National Institutes of Health–AARP Diet and Health Study, 1995 and 2006
| Factor Loadings for Each Variable Stratified on State of Residence (No. of Census Tracts) |
|||||||||
| Variables, % | CA (n = 6 814) | FL (n = 3 104) | Atlanta, GA (n = 504) | LA (n = 1 069) | Detroit, MI (n = 1 084) | NC (n = 1 487) | NJ (n = 1 896) | PA (n = 2 631) | All Locations (n = 18 589) |
| Poverty | |||||||||
| Public assistance | 0.35 | 0.34 | 0.33 | 0.32 | 0.34 | 0.34 | 0.33 | 0.35 | 0.33 |
| Female-headed households | 0.31 | 0.30 | 0.32 | 0.31 | 0.31 | 0.32 | 0.32 | 0.33 | 0.32 |
| Households without a car | 0.28 | 0.31 | 0.33 | 0.32 | 0.32 | 0.33 | 0.33 | 0.34 | 0.30 |
| Household annual income < $30 000 | 0.35 | 0.34 | 0.35 | 0.35 | 0.35 | 0.36 | 0.35 | 0.35 | 0.35 |
| Households below 1999 federal poverty levels | 0.36 | 0.36 | 0.34 | 0.36 | 0.35 | 0.36 | 0.35 | 0.35 | 0.36 |
| Occupation | |||||||||
| Unemployed | 0.31 | 0.26 | 0.26 | 0.31 | 0.33 | 0.26 | 0.30 | 0.30 | 0.30 |
| Females in managerial jobs | −0.33 | −0.30 | −0.30 | −0.29 | −0.27 | −0.29 | −0.29 | −0.26 | −0.30 |
| Men in managerial jobs | −0.33 | −0.30 | −0.30 | −0.26 | −0.29 | −0.28 | −0.28 | −0.25 | −0.30 |
| Education: <high school | 0.35 | 0.35 | 0.33 | 0.32 | 0.33 | 0.32 | 0.34 | 0.33 | 0.33 |
| Race/ethnicity: Non-Hispanic Blacks | 0.16 | 0.29 | 0.29 | 0.32 | 0.29 | 0.30 | 0.26 | 0.28 | 0.24 |
| Variance explained by first component | 64 | 63 | 70 | 67 | 74 | 64 | 70 | 64 | 63 |
We used pooled data on all the census tracts from the 6 states and 2 metropolitan areas to compute the final index with the following 10 variables: percentage of persons in the census tract who had less than high school education, were unemployed, were non-Hispanic Blacks, and worked in managerial jobs (separately for men and women) and the percentage of households that were below 1999 federal poverty levels, were on public assistance, had annual incomes less than $30 000, had no car, and were headed by women with dependent children (Table 1). The non-Hispanic Black variable did not meet the strict criteria but was retained because of its a priori interest. The internal consistency or intercorrelation between the 10 indicators was high (Cronbach's reliability coefficient = 0.93). We categorized the index into quintiles according to the distribution of the study's census tracts: the fifth quintile corresponded to the most deprived census tracts.
Mortality.
During follow-up from 1995 through December 31, 2006, we determined vital status through annual linkages of the cohort to the US Social Security Administration Death Master File. This approach made it possible to obtain complete information on all-cause mortality on the cohort.
Statistical Analysis
We used survival models with Weibull distribution and γ frailties to estimate the hazard ratios (HRs) and 95% CIs for death from all causes in relation to census tract socioeconomic deprivation (neighborhood SES). Cox proportional hazard models (without prescribed frailties) yielded almost identical results. Frailty models that accounted for clustering of participants within census tracts provided an estimate of variability in mortality between areas of residence for the cohort. We detected small but statistically significant heterogeneity in the risk of mortality between census tracts (frailty parameter = 0.02; 95% CI = 0.01, 0.02; likelihood ratio test P < .001). We assessed time to death from the date when the baseline questionnaire was received at the study center to the most recent date of vital status ascertainment (December 31, 2006).
We examined 2-way interactions among the following variables: self-rated health, body mass index (BMI; defined as weight in kg divided by height in m2), physical activity, dietary patterns, education, and neighborhood SES. We assessed the statistical significance of interactions with the Wald test with a Bonferroni correction (to account for multiple comparisons) and the likelihood ratio test. Because we found significant interaction between self-rated health and neighborhood SES, estimates of the effect of neighborhood SES on mortality were stratified on self-rated health. In our analyses, we combined the fair and poor response categories of the self-rated health variable because previous studies have found similar health trajectories for these 2 groups.28 Our analyses also showed similar neighborhood SES mortality gradients for those 2 groups, and the poor health group composed a relatively small proportion of the study population.
To assess the extent to which various factors incrementally accounted for the association between neighborhood SES and mortality, we constructed a base model (model 1) that adjusted for age (continuous), gender, race/ethnicity (non-Hispanic Whites, non-Hispanic Blacks, Hispanics, others, or unknown), marital status (married or living as married vs other), and state of residence at the time of recruitment into the study. Next, we sequentially added educational achievement (< high school, high school, vocational–technical, some college, college graduate, or unknown; model 2), followed by health behaviors (model 3) and history of the following chronic medical conditions at baseline: end-stage renal disease, diabetes, heart disease, stroke, emphysema, and cancer (model 4).
The health behaviors were smoking, Mediterranean diet scores (low, medium, or high),29 logarithmically transformed total daily caloric intake, BMI (< 25, 25–30, or > 30 kg/m2 or missing), and physical activity (never, rarely, 1 time/month to 2 times/week, ≥ 3 times/week, or missing). The traditional Mediterranean diet score was computed from reported intake of vegetables, legumes, fruit and nuts, fish and seafood, cereals, meat and meat products, dairy products, ratio of monounsaturates to saturates, and alcoholic beverages.29 Higher Mediterranean diet scores are associated with lower risk of death.30 Respondents were entered into 1 of 6 categories for cigarette smoking (never smoked, quit but previously smoked ≤ 20 cigarettes/day, quit but previously smoked > 20 cigarettes/day, currently smoking ≤ 20 cigarettes/day, currently smoking > 20 cigarettes/day, or unknown). We entered BMI–diet and smoking–physical activity interaction terms in appropriate models.
We had complete data on 90% of eligible respondents. For our primary analyses, we used multiple imputations by chained equations for missing values of smoking status (5.3%), education (5.1%), BMI (4.2%), race/ethnicity (3.0%), self-rated health (1.6%), marital status (1.5%), and physical activity (1.1%). Although our results with imputed values did not differ from findings derived from missing value indicators or complete case analysis, the multiple imputation approach provided more stable results and a consistent analytic sample size across various models. We performed all analyses with Stata release 11.1 (StataCorp LP, College Station, TX).
RESULTS
Of the 565 679 eligible respondents at baseline, the mean age was 62 years, 60% were men, 9% were non-Whites, 9% reported a history of cancer, and fewer than 1% reported end-stage renal disease. Approximately 16% of participants reported their health as excellent, 35% very good, 35% good, 12% fair, and 2% poor. Among those who did not report any of the chronic medical conditions considered in the analyses, only 6% reported their health as fair and fewer than 1% as poor (data not shown).
A total of 18 592 census tracts across the 6 states and 2 metropolitan areas contained at least 1 study participant. The component loadings of the variables were consistent across the census tracts except for percentage of non-Hispanic Blacks (Table 1).
A higher percentage of respondents in more deprived than in the least deprived census tracts reported diabetes, stroke, hypertension, emphysema, and fair-to-poor health (P < .001; data not shown). Table 2 shows the social and demographic characteristics of the study population according to the census tract socioeconomic deprivation index, stratified by self-rated health at baseline. A higher percentage of participants in the more deprived than in the least deprived census tracts were Black, were not married, and had less than 12 years of education.
TABLE 2.
Characteristics of the Cohort According to Deprivation Index and Baseline Health Status: National Institutes of Health–AARP Diet and Health Study, 1995 and 2006
| Excellent Health |
Fair-to-Poor Health |
|||||
| Demographic and Social Characteristics | All (n = 92 243), % | Deprivation Quintile 1 (n = 36 112), % | Deprivation Quintile 5 (n = 4 277), % | All (n = 75 814), % | Deprivation Quintile 1 (n = 14 968), % | Deprivation Quintile 5 (n = 8 736), % |
| Age, y | ||||||
| < 55 | 16.2 | 17.5 | 15.4 | 10.5 | 10.6 | 11.4 |
| 55–59 | 25.5 | 26.9 | 25.3 | 19.9 | 19.3 | 21.6 |
| 60–64 | 28.3 | 27.5 | 28.3 | 28.4 | 28.1 | 30.2 |
| 65–69 | 27.3 | 25.6 | 28.1 | 36.6 | 37.0 | 33.2 |
| ≥ 70 | 2.8 | 2.5 | 2.9 | 4.6 | 4.9 | 3.6 |
| Women | 39.1 | 35.6 | 47.8 | 41.5 | 35.6 | 53.8 |
| Race/ethnicity | ||||||
| Non-Hispanic Whites | 93.7 | 95.8 | 75.3 | 87.8 | 93.4 | 60.0 |
| Non-Hispanic Blacks | 2.1 | 0.7 | 15.9 | 6.4 | 1.7 | 30.5 |
| Hispanics | 1.8 | 1.2 | 4.0 | 2.2 | 1.4 | 4.1 |
| API or AI/AN | 1.4 | 1.5 | 2.3 | 1.9 | 2.2 | 2.1 |
| Missing | 1.1 | 0.8 | 2.5 | 1.8 | 1.4 | 3.3 |
| Married | 71.5 | 76.5 | 56.6 | 63.9 | 70.5 | 47.6 |
| Educational achievement | ||||||
| < high school degree | 2.8 | 1.1 | 6.9 | 13.1 | 5.7 | 20.7 |
| High school degree | 12.4 | 7.1 | 18.3 | 24.3 | 16.6 | 26.1 |
| Technical/vocational | 7.3 | 4.8 | 8.8 | 11.0 | 8.2 | 11.0 |
| Some college | 21.3 | 18.3 | 23.0 | 22.8 | 23.5 | 21.0 |
| ≥ College degree | 54.1 | 67.5 | 38.9 | 24.9 | 43.2 | 15.6 |
| Missing | 2.1 | 1.3 | 4.2 | 4.0 | 2.7 | 5.6 |
| Proxy responses | 2.6 | 2.6 | 2.5 | 4.9 | 4.2 | 4.3 |
| Paternal occupation in childhooda | ||||||
| Professional or technical | 12.2 | 14.9 | 9.2 | 6.5 | 10.2 | 3.9 |
| Managerial | 17.7 | 21.0 | 11.7 | 11.1 | 15.8 | 6.5 |
| Other nonmanual | 14.3 | 16.3 | 10.3 | 10.5 | 14.0 | 7.3 |
| Manual, in a trade | 24.8 | 21.5 | 28.5 | 27.6 | 25.4 | 25.1 |
| Other manual | 21.1 | 16.2 | 31.2 | 33.0 | 23.3 | 45.2 |
| Missing | 9.8 | 10.1 | 9.0 | 11.4 | 11.3 | 12.1 |
Note. AI/AN = American Indian/Alaskan native; API = Asian/Pacific Islander. The sample size was n = 565 679. First quintile of census tract socioeconomic deprivation = lowest deprivation; fifth quintile = highest deprivation.
Applies only to participants (n = 317 933) who responded to a follow-up questionnaire in 2004 to 2006: excellent health, all, n = 59 003; excellent health, quintile 1, n = 15 439; excellent health, quintile 5, n = 2 325; fair-to-poor health, all, n = 30 475; fair-to-poor health, quintile 1, n = 6 604; fair-to-poor health, quintile 5, n = 3 226.
Associations With Census Tract Socioeconomic Deprivation
Health risks.
Among persons in excellent health, a higher percentage in the fifth quintile (most socioeconomically deprived) than in the first quintile of census tracts were obese (BMI > 30 kg/m2), had lower levels of physical activity, had lower Mediterranean diet scores, and had higher caloric intake (Table 3). The prevalence of cancer was lowest in the most deprived neighborhoods. Respondents who were in poor health reported a lower prevalence of cancer, heart disease, end-stage renal disease, and hypertension in the most deprived than in less deprived census tracts.
TABLE 3.
Distribution of Lifestyle and Medical History by Deprivation Index and Health Status: National Institutes of Health–AARP Diet and Health Study, 1995 and 2006
| Excellent Health |
Fair-to-Poor Health |
|||||||
| Lifestyle Practices and Medical Conditions | All n = 92 243, % | Deprivation Quintile 1 n = 36 112, % | Deprivation Quintile 5 n = 4 277, % | P for trend | All n = 75 814, % | Deprivation Quintile 1 n = 14 968, % | Deprivation Quintile 5 n = 8 736, % | P for trend |
| Cigarette smoking | <.01 | <.01 | ||||||
| Never smoked | 41.5 | 43.0 | 41.9 | 26.8 | 28.2 | 28.6 | ||
| Former (≤ 20/d) | 29.3 | 29.9 | 27.1 | 25.3 | 25.3 | 26.5 | ||
| Former (> 20/d) | 18.4 | 18.5 | 15.6 | 27.7 | 29.9 | 20.0 | ||
| Current (≤ 20/d) | 5.5 | 4.3 | 8.6 | 9.4 | 7.3 | 12.9 | ||
| Current (> 20/d) | 2.2 | 1.5 | 3.1 | 6.7 | 5.6 | 6.7 | ||
| Missing | 3.1 | 3.0 | 3.7 | 4.1 | 3.6 | 5.3 | ||
| Body mass index, kg/m2 | <.01 | <.01 | ||||||
| < 25 | 48.3 | 51.7 | 40.1 | 25.5 | 28.5 | 21.8 | ||
| 25–30 | 40.2 | 39.1 | 41.9 | 35.6 | 37.6 | 31.7 | ||
| > 30 | 9.7 | 7.7 | 14.9 | 35.4 | 31.0 | 40.9 | ||
| Missing | 1.9 | 1.6 | 3.1 | 3.6 | 2.9 | 5.6 | ||
| Physical activity | <.01 | <.01 | ||||||
| Never | 2.1 | 1.4 | 4.2 | 13.9 | 11.5 | 17.0 | ||
| Rarely | 7.2 | 6.1 | 10.0 | 24.8 | 23.7 | 25.9 | ||
| 1 time/mo to 2 times/wk | 28.3 | 27.8 | 30.2 | 32.1 | 33.6 | 30.9 | ||
| ≥ 3 times/wk | 62.1 | 64.7 | 54.8 | 28.5 | 30.7 | 25.1 | ||
| Missing | 0.3 | 0.2 | 0.8 | 0.6 | 0.5 | 1.1 | ||
| Mediterranean diet score | <.01 | <.01 | ||||||
| Low | 27.9 | 24.2 | 32.2 | 42.5 | 38.0 | 44.9 | ||
| Middle | 41.1 | 40.9 | 41.2 | 40.1 | 40.4 | 40.2 | ||
| High | 31.0 | 34.9 | 26.7 | 17.4 | 21.6 | 14.9 | ||
| Medical historya | ||||||||
| Prevalent cancers | 5.0 | 5.2 | 4.6 | .06 | 15.6 | 17.0 | 13.5 | <.01 |
| End-stage renal disease | 0.0 | 0.0 | 0.1 | .76 | 1.1 | 1.3 | 1.2 | .03 |
| Emphysema | 0.4 | 0.3 | 0.5 | <.01 | 10.5 | 8.9 | 9.8 | <.01 |
| Diabetes | 1.5 | 1.1 | 2.2 | <.01 | 25.7 | 22.9 | 29.3 | <.01 |
| Heart | 2.9 | 3.0 | 2.5 | .05 | 37.3 | 37.8 | 32.4 | <.01 |
| Stroke | 0.4 | 0.3 | 0.7 | <.01 | 7.7 | 6.9 | 8.5 | <.01 |
| Hypercholesterolemiab | 56.6 | 56.6 | 57.5 | <.01 | 31.9 | 32.3 | 29.9 | .52 |
| Hypertensionb | 20.1 | 19.6 | 23.0 | .01 | 59.2 | 57.2 | 64.8 | <.01 |
| Deaths/100 person-yc | 6.5 | 5.2 | 8.8 | 3.68 | 3.58 | 3.42 | ||
Note. First quintile of census tract socioeconomic deprivation = lowest deprivation; fifth quintile = highest deprivation.
Some respondents had ≥ 1 condition.
Derived from a subcohort (n = 334 498) who responded to a questionnaire in 1996 to 1997 that included these items. Respondents in excellent health, n = 23 154 for quintile 1, n = 2552 for quintile 5. Respondents in fair-to-poor health, n = 7905 for quintile 1, n = 4329 for quintile 5.
Adjusted for age, gender, race/ethnicity, marital status, and state of residence with Poisson regression models. A total of 6211 deaths were observed among participants in excellent: 1935 in the first quintile and 374 in the fifth; 24 560 deaths occurred among participants in fair-to-poor health: 4625 in the first quintile and 2626 in the fifth.
Health status and all-cause mortality.
The maximum follow-up time of the cohort was 11.2 years, for a total of 5 643 859 person-years. The estimated overall mortality rate among the cohort adjusted for variables in the base model was 14.1 per 1000 person-years: the rate was 6.5 among respondents in excellent health, 9.1 for very good health, 15.0 for good health, and 36.8 for fair-to-poor health (Table 3).
Risk of premature mortality by health status at baseline.
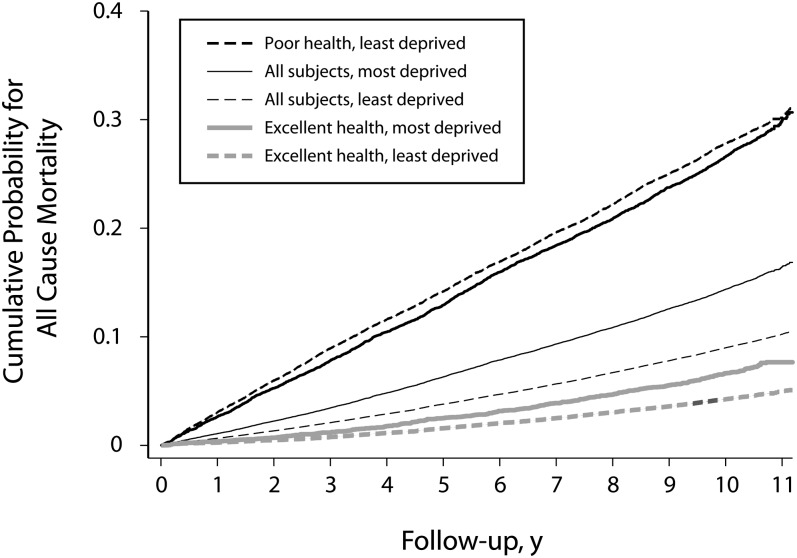
Among persons in good-to-excellent health, the adjusted mortality rate was highest in the most deprived census tracts, and the gap continued to widen over the study period (Figure 1). By contrast, the pattern of differences stratified by the deprivation index was less consistent among participants in fair-to-poor health at baseline. The mortality rates for the cohort according to census tract socioeconomic deprivation alone (without stratification on self-rated health) was most similar to estimates for respondents reporting good health (data not shown), and the cumulative mortality curves were between the curves for 2 extremes defined by health status (Figure 1).
FIGURE 1.
Age- and gender-adjusted cumulative mortality rate plots for all-cause mortality according to health status and neighborhood socioeconomic deprivation: The National Institutes of Health–AARP Diet and Health Study, 1995–2006.
Note. Least deprived is first quintile; most deprived is fifth quintile. Curves were obtained from fixed-effect Cox models stratified on health status and deprivation index as appropriate and were adjusted for age, gender, marital status, race/ethnicity, and state of residence health status. Higher curves correspond to higher mortality rates.
Table 4 shows the results of Weibull frailty models. The reference group in all survival analyses was the first deprivation quintile (or least deprived census tracts). In analyses controlling for variables in the base model (model 1) for respondents reporting good-to-excellent health, the HR of mortality increased with increasing levels of census tract socioeconomic deprivation (Table 4). For instance, among persons in excellent health, the adjusted HR was 1.31 (95% CI = 1.22, 1.41) for those residing in the third socioeconomic deprivation quintile and 1.68 (95% CI = 1.49, 1.86) for those in the fifth socioeconomic deprivation quintile. However, the strength of the association between census tract socioeconomic deprivation and risk of premature mortality decreased with worsening health status. The HRs for persons who reported good health were 1.15 (95% CI = 1.12, 1.19) for the third quintile and 1.35 (95% CI = 1.29, 1.41) for the fifth quintile. Among persons in fair-to-poor health, the HRs for each deprivation quintile were smaller than for those who were in good-to-excellent health (P for trend < .001) and, by contrast, did not exhibit a dose–response pattern (third-quintile HR = 1.12; 95% CI = 1.07, 1.16; fifth-quintile HR = 1.08; 95% CI = 1.03, 1.13; Table 4).
TABLE 4.
Association Between Neighborhood Socioeconomic Deprivation and Overall Mortality: National Institutes of Health–AARP Diet and Health Study, 1995 and 2006
| Strata of Self-Rated Health Status and Deprivation Quintiles | Model 1,a HR (95% CI) | Model 2,b HR (95% CI) | Model 3,c HR (95% CI) | Model 4,d HR (95% CI) |
| Excellent health | ||||
| Deprivation quintile | ||||
| 1 (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 1.24 (1.16, 1.32) | 1.21 (1.13, 1.30) | 1.19 (1.11, 1.27) | 1.19 (1.11, 1.26) |
| 3 | 1.31 (1.22, 1.41) | 1.27 (1.18, 1.36) | 1.23 (1.14, 1.32) | 1.23 (1.14, 1.32) |
| 4 | 1.52 (1.39, 1.64) | 1.46 (1.34, 1.58) | 1.39 (1.28, 1.50) | 1.39 (1.28, 1.50) |
| 5 | 1.68 (1.49, 1.86) | 1.61 (1.43, 1.79) | 1.51 (1.34, 1.68) | 1.48 (1.31, 1.64) |
| Very good health | ||||
| Deprivation quintile | ||||
| 1 (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 1.11 (1.07, 1.16) | 1.09 (1.04, 1.13) | 1.06 (1.02, 1.11) | 1.06 (1.02, 1.10) |
| 3 | 1.18 (1.13, 1.23) | 1.14 (1.10, 1.19) | 1.11 (1.07, 1.16) | 1.11 (1.06, 1.15) |
| 4 | 1.30 (1.24, 1.36) | 1.25 (1.19, 1.31) | 1.20 (1.14, 1.26) | 1.19 (1.13, 1.24) |
| 5 | 1.42 (1.33, 1.51) | 1.37 (1.28, 1.45) | 1.28 (1.20, 1.36) | 1.27 (1.19, 1.35) |
| Good health | ||||
| Deprivation quintile | ||||
| 1 (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 1.07 (1.03, 1.10) | 1.04 (1.01, 1.08) | 1.03 (0.99, 1.06) | 1.02 (0.98, 1.05) |
| 3 | 1.15 (1.12, 1.19) | 1.12 (1.08, 1.16) | 1.09 (1.05, 1.13) | 1.08 (1.05, 1.12) |
| 4 | 1.23 (1.18, 1.27) | 1.18 (1.13, 1.22) | 1.14 (1.10, 1.18) | 1.13 (1.09, 1.17) |
| 5 | 1.35 (1.29, 1.41) | 1.29 (1.23, 1.35) | 1.23 (1.17, 1.29) | 1.21 (1.15, 1.27) |
| Fair-to-poor health | ||||
| Deprivation quintile | ||||
| 1 (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 1.01 (0.97, 1.05) | 0.99 (0.95, 1.03) | 0.99 (0.95, 1.02) | 0.96 (0.93, 1.00) |
| 3 | 1.12 (1.07, 1.16) | 1.08 (1.04, 1.12) | 1.05 (1.01, 1.09) | 1.02 (0.98, 1.06) |
| 4 | 1.10 (1.06, 1.15) | 1.06 (1.01, 1.10) | 1.03 (0.98, 1.07) | 0.99 (0.95, 1.04) |
| 5 | 1.08 (1.03, 1.13) | 1.03 (0.98, 1.08) | 0.99 (0.94, 1.04) | 0.95 (0.90, 1.00) |
Note. CI = confidence interval; HR = hazard ratio. The sample size was n = 565 679. First quintile of census tract socioeconomic deprivation = least deprivation; fifth quintile = most deprivation. All estimates were derived from models that included a census tract–level socioeconomic deprivation index with self-rated health interaction term.
Adjusted for age at baseline, gender, race/ethnicity, marital status, and state of residence at baseline.
Model 1 adjustments plus level of educational achievement.
Model 2 adjustments plus logarithmically transformed caloric intake and smoking status with physical activity and Mediterranean diet with body mass index interaction terms.
Model 3 adjustments plus personal history of end-stage renal disease, diabetes, heart disease, stroke, emphysema, and cancer.
Further analyses assessed the impact of adjusting for other risk factors for death. Among persons in excellent health, the association between neighborhood socioeconomic deprivation and mortality was slightly attenuated but remained stable after further adjustment for education, health behaviors, and medical illnesses (fifth-quintile HR = 1.48; 95% CI = 1.31, 1.64). The estimates were similarly stable for participants in good or very good health. However, among persons in fair-to-poor health, the observed relatively small neighborhood SES mortality gradients were no longer statistically significant after further adjustment for health behaviors alone (data not shown).
Sensitivity Analyses
Previous studies suggest that self-rated health may not measure physical health in a similar way across strata of socioeconomic groups.21,31 Therefore, we performed several sensitivity analyses stratified on age groups, gender, and smoking history (Appendix A, available as a supplement to the online version of this article at http://www.ajph.org), as well as restricted to persons who (1) did not report any of the selected medical conditions at baseline (n = 327 195), (2) responded to the questionnaire without the help of a proxy or did not report end-stage renal disease (n = 565 591), and (3) had at least 2 years of follow-up in the study.
We also performed analyses with controls for self-reported history of hypertension or hypercholesterolemia and for paternal occupation on the subgroup of participants who responded to both of the 2 subsequent questionnaires with these items (n = 216 989; Appendix B, available as a supplement to the online version of this article at http://www.ajph.org). These analyses yielded findings similar to our main results. Among persons in fair-to-poor health who did not report medical illnesses, the effect sizes from the base model were similar in magnitude to model 2 (Table 4) and were no longer statistically significant after further adjustment for education.
DISCUSSION
We used a large prospective cohort to examine whether the risk of premature mortality associated with living in socioeconomically deprived neighborhoods differed according to individuals' health status. We found that neighborhood socioeconomic mortality disparities were less striking among persons in fair-to-poor health than among those in good-to-excellent health. Healthy adults residing in socioeconomically deprived neighborhoods died at a higher rate than did persons in relatively less deprived areas, even after accounting for individual-level SES, lifestyle practices, and medical history. By contrast, among respondents in fair-to-poor health at baseline, we detected relatively small neighborhood SES mortality disparities, and these were no longer significant after adjustment for health behaviors.
To our knowledge, no previous studies provide direct comparison to ours. However, 2 previous studies found a stronger association between individual-level SES and mortality in persons in good-to-excellent health than in those in poor health.20,21 Consistent with our findings, Waitzman and Smith found area-level SES mortality disparities for persons aged 25 to 54 years but not for those aged 55 to 74 years.32 These findings suggest that socioeconomic advantage does not confer a mortality advantage for persons in poor health. Alternatively, it is possible that people who were in poor health and resided in relatively poor neighborhoods were as resilient to the effects of ill health as their counterparts in more affluent areas.
We also sought to determine the impact of adjusting for other risk factors for death on neighborhood SES mortality disparities. Consistent with previous studies, we found a strong association between neighborhood SES conditions and health behaviors and prevalence of chronic medical conditions. Among respondents in poor health, the relatively small neighborhood SES mortality disparities were explained by differences in health behaviors. The large neighborhood SES mortality gaps among persons in good-to-excellent health were slightly attenuated, but they persisted even after adjustment for those factors. This finding further supports the hypothesis that neighborhood socioeconomic deprivation confers additional mortality risks beyond an individual's SES and health behaviors,10,17,18,33,34 and the higher mortality risks are not attributable solely to the clustering of persons with higher prevalence of unhealthful lifestyle practices in poor neighborhoods.7,15,16 Our study further extends this evidence and shows that neighborhood SES mortality disparities documented in long-term studies may reflect inequalities among people who were healthy at baseline. Our results suggest that valid analyses on neighborhood SES disparities require a careful assessment of participants' health status.
Self-reported health encompasses a broad range of medical conditions and may change over the life course of individuals.8,12,28 We found a higher prevalence of heart disease and cancer, the 2 leading causes of death in the United States,35 among participants in poor health residing in more affluent neighborhoods than among their counterparts in poorer areas. It is plausible that the relative proportion of persons with mental illness (which is more prevalent in poor areas36–38) or physical health conditions or differences in perceptions of health according to neighborhood SES may have contributed to our findings. However, the consistency and magnitude of our results, including the sensitivity analyses, show that our findings could not be attributed to systematic neighborhood SES differences in reporting of self-rated health or medical conditions, as has been suggested previously.21
Limitations
Studies have shown that the mortality risk associated with residing in socioeconomically deprived areas is attributable in part to poverty within neighborhoods and to the extent of relative inequality between neighborhoods.39–41 Thus, differences in access to health care resources are likely to contribute to neighborhood SES mortality disparities.36 Although we did not have data on access to health care, existing literature shows that the relationship between access to health care resources and neighborhood SES varies according to the population studied.42,43 Our study population was relatively homogeneous: non-Whites were a relatively small proportion (9%) of our cohort, and participants were predominantly older, upper- to middle-class Americans in urban centers. This finding suggests that the AARP populations may have had similar access to health care services irrespective of neighborhood SES, but this possibility needs further study.
We used baseline lifestyle and dietary measures obtained in late adulthood, which may not reflect health behaviors throughout the life course. Socioeconomically deprived environments increase the risk of both exposure and vulnerability to adverse health risk factors such as violence, prejudice, segregation, psychological stress, toxins, pollutants, and other environmental hazards.19 In addition, the socioeconomic context of the neighborhoods in which our study population lived may have changed during the study period, particularly during the period of economic growth prior to the current global recession. These factors and the potential impact of residential mobility44 could not be measured in this study.
Conclusions
It is well-known that socioeconomic circumstances determine the health status and longevity of individuals.22,45 We found that the risk of premature mortality associated with living in socioeconomically deprived neighborhoods varied according to health status of individuals. We found large, long-term neighborhood socioeconomic mortality disparities in healthy individuals but not in people who were already in poor health. This finding shows that neighborhood socioeconomic mortality disparities are not attributable solely to clustering of persons in poor health in poor areas.
Our study further showed that poor neighborhood socioeconomic conditions affect the longevity of healthy persons beyond personal attributes of demographics, education, or lifestyle practices. This finding represents a major public health challenge and reinforces the need for social policies and programs to mitigate health risks posed by neighborhood socioeconomic deprivation in the United States. Future studies are needed for a better understanding of why neighborhood SES mortality disparities vary by health status.
Acknowledgments
This research was supported in part by the Intramural Research Program of the NIH and the National Cancer Institute. C. A. Doubeni was supported by grants from the National Cancer Institute (5K01CA127118-04 and 1R01CA151736-01). M. Schootman and M. Lian were supported in part by a grant from the National Cancer Institute (5R01CA137750-02).
We are indebted to the participants in the NIH–AARP Diet and Health Study for their outstanding cooperation. We also thank Sigurd Hermansen and Kerry Grace Morrissey from Westat for study outcomes ascertainment and management and Michael Spriggs and Leslie Carroll at Information Management Services for data support and analysis.
We acknowledge the loss and memory of Arthur Schatzkin, the principal investigator for the NIH–AARP Diet and Health Study, who passed away on January 20, 2011.
Human Participant Protection
The National Cancer Institute special studies institutional review board approved the NIH–AARP study.
References
- 1.Antonovsky A. Social class, life expectancy and overall mortality. Milbank Mem Fund Q. 1967;45(2):31–73 [PubMed] [Google Scholar]
- 2.Feldman JJ, Makuc DM, Kleinman JC, Cornoni-Huntley J. National trends in educational differentials in mortality. Am J Epidemiol. 1989;129(5):919–933 [DOI] [PubMed] [Google Scholar]
- 3.Pappas G, Queen S, Hadden W, Fisher G. The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986. N Engl J Med. 1993;329(2):103–109 [DOI] [PubMed] [Google Scholar]
- 4.Singh GK. Area deprivation and widening inequalities in US mortality, 1969–1998. Am J Public Health. 2003;93(7):1137–1143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh GK, Siahpush M. Widening socioeconomic inequalities in US life expectancy, 1980–2000. Int J Epidemiol. 2006;35(4):969–979 [DOI] [PubMed] [Google Scholar]
- 6.Kondo N, Sembajwe G, Kawachi I, van Dam RM, Subramanian SV, Yamagata Z. Income inequality, mortality, and self rated health: meta-analysis of multilevel studies. BMJ. 2009;339:b4471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arber S. Social class, non-employment, and chronic illness: continuing the inequalities in health debate. Br Med J (Clin Res Ed). 1987;294(6579):1069–1073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Power C, Matthews S, Manor O. Inequalities in self rated health in the 1958 birth cohort: lifetime social circumstances or social mobility? BMJ. 1996;313(7055):449–453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sundquist J, Johansson SE. Self reported poor health and low educational level predictors for mortality: a population based follow up study of 39,156 people in Sweden. J Epidemiol Community Health. 1997;51(1):35–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lantz PM, House JS, Lepkowski JM, Williams DR, Mero RP, Chen J. Socioeconomic factors, health behaviors, and mortality: results from a nationally representative prospective study of US adults. JAMA. 1998;279(21):1703–1708 [DOI] [PubMed] [Google Scholar]
- 11.Hemingway H, Nicholson A, Stafford M, Roberts R, Marmot M. The impact of socioeconomic status on health functioning as assessed by the SF-36 questionnaire: the Whitehall II Study. Am J Public Health. 1997;87(9):1484–1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Breeze E, Fletcher AE, Leon DA, Marmot MG, Clarke RJ, Shipley MJ. Do socioeconomic disadvantages persist into old age? Self-reported morbidity in a 29-year follow-up of the Whitehall Study. Am J Public Health. 2001;91(2):277–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith GD, Bartley M, Blane D. The Black report on socioeconomic inequalities in health 10 years on. BMJ. 1990;301(6748):373–377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diez-Roux AV, Nieto FJ, Caulfield L, Tyroler HA, Watson RL, Szklo M. Neighbourhood differences in diet: the Atherosclerosis Risk in Communities (ARIC) Study. J Epidemiol Community Health. 1999;53(1):55–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chowdhury P, Balluz L, Town M, et al. Surveillance of certain health behaviors and conditions among states and selected local areas—Behavioral Risk Factor Surveillance System, United States, 2007. MMWR Surveill Summ. 2010;59(1):1–220 [PubMed] [Google Scholar]
- 16.Krieger N. Why epidemiologists cannot afford to ignore poverty. Epidemiology. 2007;18(6):658–663 [DOI] [PubMed] [Google Scholar]
- 17.Yen IH, Kaplan GA. Neighborhood social environment and risk of death: multilevel evidence from the Alameda County Study. Am J Epidemiol. 1999;149(10):898–907 [DOI] [PubMed] [Google Scholar]
- 18.Winkleby MA, Cubbin C. Influence of individual and neighbourhood socioeconomic status on mortality among Black, Mexican-American, and White women and men in the United States. J Epidemiol Community Health. 2003;57(6):444–452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fiscella K, Williams DR. Health disparities based on socioeconomic inequities: implications for urban health care. Acad Med. 2004;79(12):1139–1147 [DOI] [PubMed] [Google Scholar]
- 20.Burstrom B, Fredlund P. Self rated health: is it as good a predictor of subsequent mortality among adults in lower as well as in higher social classes? J Epidemiol Community Health. 2001;55(11):836–840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Regidor E, Guallar-Castillon P, Gutierrez-Fisac JL, Banegas JR, Rodriguez-Artalejo F. Socioeconomic variation in the magnitude of the association between self-rated health and mortality. Ann Epidemiol. 2010;20(5):395–400 [DOI] [PubMed] [Google Scholar]
- 22.Commission on Social Determinants of Health Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. Final Report of the Commission on Social Determinants of Health. Geneva, Switzerland: World Health Organization; 2008 [Google Scholar]
- 23.Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294(22):2879–2888 [DOI] [PubMed] [Google Scholar]
- 24.Schatzkin A, Subar AF, Thompson FE, et al. Design and serendipity in establishing a large cohort with wide dietary intake distributions: the National Institutes of Health–American Association of Retired Persons Diet and Health Study. Am J Epidemiol. 2001;154(12):1119–1125 [DOI] [PubMed] [Google Scholar]
- 25.Thompson FE, Kipnis V, Midthune D, et al. Performance of a food-frequency questionnaire in the US NIH–AARP (National Institutes of Health–American Association of Retired Persons) Diet and Health Study. Public Health Nutr. 2008;11(2):183–195 [DOI] [PubMed] [Google Scholar]
- 26.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: the Public Health Disparities Geocoding Project (US). J Epidemiol Community Health. 2003;57(3):186–199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Messer LC, Laraia BA, Kaufman JS, et al. The development of a standardized neighborhood deprivation index. J Urban Health. 2006;83(6):1041–1062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wolinsky FD, Miller TR, Malmstrom TK, et al. Self-rated health: changes, trajectories, and their antecedents among African Americans. J Aging Health. 2008;20(2):143–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599–2608 [DOI] [PubMed] [Google Scholar]
- 30.Mitrou PN, Kipnis V, Thiebaut AC, et al. Mediterranean dietary pattern and prediction of all-cause mortality in a US population: results from the NIH–AARP Diet and Health Study. Arch Intern Med. 2007;167(22):2461–2468 [DOI] [PubMed] [Google Scholar]
- 31.Singh-Manoux A, Dugravot A, Shipley MJ, et al. The association between self-rated health and mortality in different socioeconomic groups in the GAZEL cohort study. Int J Epidemiol. 2007;36(6):1222–1228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Waitzman NJ, Smith KR. Phantom of the area: poverty-area residence and mortality in the United States. Am J Public Health. 1998;88(6):973–976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rosvall M, Chaix B, Lynch J, Lindström M, Merlo J. Contribution of main causes of death to social inequalities in mortality in the whole population of Scania, Sweden. BMC Public Health. 2006;6:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stringhini S, Sabia S, Shipley M, et al. Association of socioeconomic position with health behaviors and mortality. JAMA. 2010;303(12):1159–1166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xu JQ, Kochanek KD, Tejada-Vera B. Deaths: preliminary data for 2007. National Vital Statistics Reports. 2009;58(1). Hyattsville, MD: National Center for Health Statistics; Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr58/nvsr58_01.pdf. Accessed: May 16, 2011 [Google Scholar]
- 36.Ellen IG, Mijanovich T, Dillman K- N. Neighborhood effects on health: exploring the links and assessing the evidence. J Urban Aff. 2001;23(3–4):391–408 [Google Scholar]
- 37.Do DP, Finch BK. The link between neighborhood poverty and health: context or composition? Am J Epidemiol. 2008;168(6):611–619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Eibner C, Sturn R, Gresenz CR. Does relative deprivation predict the need for mental health services? J Ment Health Policy Econ. 2004;7(4):167–175 [PubMed] [Google Scholar]
- 39.Carstairs V, Morris R. Deprivation, mortality and resource allocation. Community Med. 1989;11(4):364–372 [PubMed] [Google Scholar]
- 40.Wilkinson RG. Income distribution and life expectancy. BMJ. 1992;304(6820):165–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wilkinson RG. National mortality rates: the impact of inequality? Am J Public Health. 1992;82(8):1082–1084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Iribarren C, Tolstykh I, Somkin CP, et al. Sex and racial/ethnic disparities in outcomes after acute myocardial infarction: a cohort study among members of a large integrated health care delivery system in northern California. Arch Intern Med. 2005;165(18):2105–2113 [DOI] [PubMed] [Google Scholar]
- 43.Pilote L, Tu JV, Humphries K, et al. Socioeconomic status, access to health care, and outcomes after acute myocardial infarction in Canada's universal health care system. Med Care. 2007;45(7):638–646 [DOI] [PubMed] [Google Scholar]
- 44.He W, Schachter JP. Internal Migration of the Older Population: 1995 to 2000. Washington, DC: US Census Bureau; 2003. Census 2000 Special Reports [Google Scholar]
- 45.Phelan JC, Link BG, Diez-Roux A, Kawachi I, Levin B. “Fundamental causes” of social inequalities in mortality: a test of the theory. J Health Soc Behav. 2004;45(3):265–285 [DOI] [PubMed] [Google Scholar]