Abstract
Objectives. We investigated whether state-sponsored antitobacco advertisements are associated with reduced adult smoking, and interactions between smoking-related advertising types.
Methods. We measured mean exposure to smoking-related advertisements with television ratings for the top-75 US media markets from 1999 to 2007. We combined these data with individual-level Current Population Surveys Tobacco Use Supplement data and state tobacco control policy data.
Results. Higher exposure to state-sponsored, Legacy, and pharmaceutical advertisements was associated with less smoking; higher exposure to tobacco industry advertisements was associated with more smoking. Higher exposure to state- and Legacy-sponsored advertisements was positively associated with intentions to quit and having made a past-year quit attempt; higher exposure to ads for pharmaceutical cessation aids was negatively associated with having made a quit attempt. There was a significant negative interaction between state- and Legacy-sponsored advertisements.
Conclusions. Exposure to state-sponsored advertisements was far below Centers for Disease Control and Prevention–recommended best practices. The significant negative relationships between antismoking advertising and adult smoking provide strong evidence that tobacco-control media campaigns help reduce adult smoking. The significant negative interaction between state- and Legacy-sponsored advertising suggests that the campaigns reinforce one another.
Cigarette smoking remains the leading cause of preventable death in the United States. State tobacco control programs rely heavily on paid television advertising to promote tobacco control messages, with the goals of influencing attitudes and beliefs about tobacco use, and reducing population smoking. The California Tobacco Control Program, launched in 1990, is the largest and longest-running state-sponsored antismoking media campaign in the United States.1 Massachusetts introduced a campaign in 1994, Arizona in 1997, and Oregon and Florida in 1998.2,3 Between 1998 and 2002, at least 30 other states started antismoking media campaigns. Cigarette excise taxes and earmarked funds from the 1998 Master Settlement Agreement (MSA) have financed the majority of such campaigns4; in recent years, however, many of these state campaigns have been significantly cut, or even eliminated. The American Recovery and Reinvestment Act of 2009 allocated $650 million toward the Communities Putting Prevention to Work initiatives, many of which included significant tobacco control media campaigns.5 This recent infusion of funding represents the largest expansion of state and regional tobacco control media campaigns since 1998. In addition, the US Food and Drug Administration has announced its own sizable tobacco control media campaign scheduled in 2012.6
State-sponsored antitobacco advertisements are not the only smoking-related messages seen on television in the United States in recent years. Since 1996, when nicotine replacement therapies were approved for over-the-counter distribution, pharmaceutical companies have used television advertising extensively to promote smoking cessation aids.7 Also as a result of the MSA, the American Legacy Foundation (Legacy) was formed in 1999, and in 2000 introduced “truth,” its national antismoking advertising campaign. In addition, Philip Morris and Lorillard each launched media campaigns in 1998, which included television advertising with putatively antismoking messages.8
Early evidence has suggested that public investments in antismoking media campaigns contributed to reductions in smoking among youths.9 Research on the relationship between antismoking advertisements and adult smoking behavior is encouraging but less conclusive.4,10 Most studies have focused on individual media campaigns within a single state or country, and have not controlled for other smoking-related advertising or other tobacco control policies, such as cigarette excise taxes or clean indoor air regulations, which also influence smoking.11 For example, a recent Australian study showed that higher levels of televised antismoking advertising was associated with reduced adult smoking, with control for important concurrent tobacco control policies.12 One multistate study of the relationship between antismoking advertisements and adult smoking in the United States showed that smokers with higher levels of awareness of antismoking media campaigns were more likely to quit, even after control for other tobacco control policies in the 9 states studied.13 However, that study did not explore the impact of other antitobacco or cessation-related advertising, such as Legacy’s truth campaign or advertisements for pharmaceutical cessation aids. Adults in the United States received substantial levels of exposure to ads for pharmaceutical cessation aids, as well as to Legacy’s predominantly youth-targeted antitobacco media campaign.7 Exposure to either or both of these smoking-related messages may therefore have had important effects on adult smoking. To date, there has been no research on the relationship between smoking among US adults and concurrent exposure to smoking-related advertisements produced by various sponsors, or potential interactions among advertising produced by various sponsors.
We examined the relationships between US adults’ smoking behaviors and their exposure to smoking-related television advertisements sponsored by state health departments, the American Legacy Foundation, tobacco companies, and pharmaceutical companies promoting their cessation products. We hypothesized that higher levels of exposure to state-sponsored antitobacco advertisements would be associated with reduced smoking. Our models controlled for individual characteristics, as well as state tobacco control policies and, therefore, overcame the limitations of previous research on the effects of antismoking advertising on smoking among adults.
METHODS
Commercial ratings data provided information on mean audience exposure to all tobacco-related advertising that appeared on any Nielsen Monitor-Plus monitored network and cable television distributors nationally and for local spot, clearance, and syndication television across the largest 75 US media markets for 1999 through 2007. These 75 markets accounted for 78% of US households.14 Ratings for each commercial occurrence were aggregated by market, month, year, and sponsor. Details of the methodology used for obtaining and aggregating the Nielsen data are reported elsewhere.15
Nielsen data provide individual ratings of television programs obtained by monitoring household audiences. Gross ratings points (GRPs) measure the percentage of households watching a program or advertisement in a media market over a specified time interval. For example, an advertisement with 80 GRPs per month is estimated to have been seen 1 time per month on average by 80% of the television households in that media market. We scaled the GRP data by 100; thus, we could offer an interpretation of the average number of exposures per person (0.80 for the example in this paragraph).
Data on individual characteristics and smoking behavior were obtained from the 1998–1999, 2000, 2001–2002, 2003, and 2006–2007 waves of the Tobacco Use Supplements of the Current Population Surveys (TUS-CPS). These are cross-sectional surveys, which provide the largest and most comprehensive data on smoking behavior among adults in the United States for the years they were administered. The TUS-CPS samples approximately 56 000 households per month per wave. Approximately 70% of respondents were surveyed by telephone, and 30% completed in-person interviews. We used self-respondent data (about 40% of respondents were self-respondents) because key outcome and control variables were not available on the proxy form. We conducted sensitivity analyses to compare smoking status between proxy and self-report respondents, and we observed no significant differences. Details on sampling methodology and response rates are available elsewhere.16
We calculated the average real price per pack of cigarettes by state and year with information from The Tax Burden on Tobacco17 and the US Bureau of Labor Statistics Consumer Price Index.18 A smoke-free air (SFA) index measured the strength of protection for schools (public and private), recreational facilities, cultural facilities, shopping malls, private work sites, public transit, restaurants, and health care facilities; points were subtracted for state SFA preemption laws.19
Measures and Analysis
We analyzed separate models for each of the following dependent variables:
Smoking status: Current smokers responded “yes” to the question “Have you smoked at least 100 cigarettes in your entire life?” and answered either “every day” or “some days” to the question “Do you now smoke every day, some days, or not at all?”
Intentions to quit smoking: We defined current smokers as having serious intentions to quit smoking if they responded “yes” to the question “Are you planning to quit in the next 30 days?”
Quit attempt in past year: Because the wording of the question probing quit attempts slightly changed in 2003, we classified current smokers from the 1999 through 2002 TUS-CPS waves as having made a quit attempt in the past year if they responded “yes” to the question “During the past 12 months, have you stopped smoking for one day or longer because you were trying to quit smoking?” For respondents to the 2003 through 2007 TUS-CPS waves, we classified some-day smokers who smoked less than 12 of the past 30 days and responded affirmatively to the question “During the past 12 months, have you tried to quit smoking completely?” as having made a quit attempt in the past year. We also classified every-day smokers and some-day smokers who smoked 12 or more of the past 30 days and answered affirmatively to the question “During the past 12 months, have you stopped smoking for one day or longer because you were trying to quit smoking?” as having made a quit attempt in the past year.
Average daily cigarette consumption: We calculated average daily cigarette consumption by using every-day smokers’ response to the question “On the average, about how many cigarettes do you now smoke each day?” For some-day smokers, we calculated a daily average by multiplying number of days per month they smoked and their answer to the question “On the days that you smoke, about how many cigarettes do you now smoke?” then dividing this value by 30.
Independent variables.
We calculated measures of exposure to each of the 4 categories of smoking-related television advertisements for each respondent based on the survey date and media market in which they resided. Our exposure measure represents total exposure over 4 months before an individual’s survey date, giving the greatest weight to more recent exposure.20 We used a slight variation of this exposure measure for our analyses of quit attempts, summing exposure over the past 12 months so that the period of observation corresponded to the 12-month time frame in the survey question about quit attempts. We merged the Nielsen ratings data with the individual-level TUS-CPS data by survey date and state and county Federal Information Processing Standards codes.21
Control variables.
All models included the following individual-level control variables known to be associated with smoking by adults22,23: gender, race/ethnicity, age, education, marital status, employment status, region of residence, and a linear time-trend variable, which controlled for secular trends in smoking prevalence that may be unrelated to the variables of interest. Our models also included a quadratic age term (age2) to account for the increasing probability of smoking as age increases, up to age 45 years approximately, and the diminishing influence of age on the probability of smoking after that. We included the following state-level tobacco policy variables, which have been shown to be significantly associated with smoking by adults24: average real price per pack of cigarettes at the year of survey, and an index measuring the strictness of SFA laws in the state at the year of survey. We also included a state-level measure of the adult population smoking prevalence in 1998 as an indicator of population tobacco milieu before the start of the analysis period.25 We merged the state-level data with the individual-level TUS-CPS data, by state and year of survey.
Analyses
We estimated logistic regression models for the dichotomous outcomes. To account for overdispersion in cigarette consumption among current smokers, we estimated a negative binomial model. In each model, we tested for interactions between exposure to state- and Legacy-sponsored ads, state-sponsored and pharmaceutical company ads, and state- and tobacco industry–sponsored ads. Because of the relatively high correlations between our measures of state-sponsored antitobacco television advertising and the other tobacco control policy variables, we tested the robustness of our models by estimating each model with and without both of the tobacco control policy variables and the 1998 state-level smoking prevalence values. In addition, we estimated each model with and without each of the tobacco control policy variables and the smoking prevalence variable individually. Finally, we also estimated each model with a 12-month sum of exposure to each type of smoking-related advertising. We used SAS version 9.2 (SAS Institute, Cary, NC) for all analyses.
RESULTS
After we retained only cases with data for at least 1 outcome, 433 232 respondents remained in the analytical sample. Table 1 summarizes the characteristics of these respondents, along with measures of ad exposure and state policy variables. Approximately 20% of the sample were current smokers, with about three quarters of these reporting that they smoked every day. Among current smokers, approximately 18% reported an intention to quit in the next 30 days, and the mean number of cigarettes per day was approximately 15.
TABLE 1—
Summary Statistics of Nielsen Ratings, Individual Data, and State Tobacco Control Policy Data: United States, 1999–2007
| Outcome Variables | Mean ±SD, No. (%), or Mean (Median; Range) |
| No. of cigarettes/da | 14.64 ±10.44 |
| Smoking status | |
| Current smokers | 87 961 (20.30) |
| Nonsmokers | 345 271 (79.70) |
| Intend to quit in the next 30 d | |
| Yes | 12 040 (18.31) |
| No | 53 707 (81.69) |
| Quit attempt in the past 12 mo | |
| Yes | 26 699 (42.17) |
| No | 36 617 (57.83) |
| Antismoking TV advertising (GRPs/100) | |
| State | 4.21 (0.76; 0–46.55) |
| Legacy | 3.42 (2.91; 0–17.97) |
| Pharmaceutical | 15.52 (13.99; 1.55–37.38) |
| Tobacco industry | 10.78 (8.15; 1.82–39.26) |
| Tobacco control policies | |
| Cigarette price per pack, $ | 1.95 ±0.33 |
| SFA score with preemption | 11.53 ±10.03 |
| Cigarette use in 1998, % | 22.88 ±2.89 |
| Individual-level covariates | |
| Age, y | 41.48 ±14.49 |
| Race/ethnicity | |
| White | 309 802 (71.51) |
| American Indian/Alaska Native | 2461 (0.57) |
| Asian/Pacific Islander/Hawaiian | 18 929 (4.37) |
| Hispanic | 50 476 (11.65) |
| Black | 49 359 (11.39) |
| Others | 2205 (0.51) |
| Education | |
| < 12th grade | 69 118 (15.95) |
| High school graduate or GED | 122 803 (28.35) |
| Some college or associate’s degree | 117 407 (27.10) |
| Bachelor’s, master’s, professional degree, or doctorate | 123 904 (28.60) |
| Gender | |
| Male | 188 000 (43.39) |
| Female | 245 232 (56.61) |
| Marital status | |
| Married | 236 631 (54.62) |
| Widowed, divorced, or separated | 77 058 (17.79) |
| Never married | 119 543 (27.59) |
| Employment, work area | |
| Full-time, indoor | 208 047 (48.02) |
| Part-time, indoor | 53 413 (12.33) |
| Part- and full-time, home | 26 044 (6.01) |
| Part- and full-time, outdoor | 6292 (1.45) |
| Not in labor force | 121 626 (28.07) |
| Unemployed | 17 810 (4.11) |
| Region | |
| South | 135 039 (31.17) |
| Midwest | 100 934 (23.30) |
| Northeast | 95 276 (21.99) |
| West | 101 983 (23.54) |
Notes. GED = general equivalency diploma; GRPs = gross ratings points; SFA = smoke-free air index. The sample size was n = 433 232.
Among current smokers.
Pharmaceutical and tobacco industry advertising dominated that of states or the American Legacy Foundation. Over the 8 years described by our data, the national average of our recency-weighted sum of 4 months of exposure was 15.52 for pharmaceutical cessation aids and 10.78 for tobacco industry–sponsored ads compared with 4.21 for state-sponsored ads and 3.42 for Legacy ads.
Figure 1 illustrates the trends in national average monthly exposure levels for each type of tobacco-related advertising for 1999 through 2006.
FIGURE 1—
US annual average smoking-related television advertising exposure levels, by sponsor: 1999–2007.
Table 2 presents the results of multivariate models relating exposure to smoking-related advertising and the probability of (1) being a current smoker, compared with non–current smokers (never smokers or former smokers), (2) current smokers’ intention to quit smoking in the next 30 days, (3) current smokers’ report of having made a quit attempt in the past 12 months, and (4) amount smoked among current smokers.
TABLE 2—
Odds Ratios of Smoking Status and Intention to Quit, and Parameter Estimates of the Number of Cigarettes per Day: United States, 1999–2007.
| Variablesa | Current Smokers Versus Noncurrent (n = 433 232), ORb (P) | Intention to Quit, Yes Versus No (n = 65 747), ORb (P) | Quit Attempt, Yes Versus No (n = 63 316), ORc (P) | Number of Cigarettes per Day (n = 67 700), Bd (P) |
| GRP of antismoking TV ads | ||||
| State | 0.974 (< .001) | 1.046 (.006) | 0.998 (.392) | 0.0032 (.505) |
| Legacy | 0.962 (.003) | 1.110 (.003) | 1.019 (.043) | −0.0024 (.807) |
| Pharmaceutical | 0.967 (< .001) | 1.022 (.227) | 0.975 (< .001) | −0.0074 (.139) |
| Tobacco industry | 1.039 (< .001) | 1.093 (.013) | 0.992 (.007) | −0.0153 (.127) |
| Cigarette price per pack ($1 increments) | 0.945 (.002) | 1.121 (.01) | 1.121 (.003) | −0.0631 (< .001) |
| SFA score with preemption | 0.998 (.002) | 1.001 (.39) | 1.002 (.132) | 0.0002 (.492) |
| Cigarette use in 1998 (1% increments) | 1.024 (< .001) | 0.982 (< .001) | 0.979 (< .001) | 0.0159 (< .001) |
Notes. GRP = gross ratings points; OR = odds ratio; SFA = smoke-free air index.
Covariates not shown in this table are age, age-squared, time, race, education, gender, marital status, employment and work area, and region.
ORs are estimated for 10 recency-weighted exposures for 4 months before the date of Tobacco Use Supplements of the Current Population Surveys.
ORs estimated for 10 unweighted exposures for 12 months before the date of Tobacco Use Supplements of the Current Population Surveys.
Parameter estimates are from the negative binomial regression model for 10 recency-weighted exposures for 4 months before the survey.
Our models showed that higher levels of exposure to state-sponsored antitobacco advertisements were associated with a lower probability of being a current smoker. Each incremental increase of approximately 10 exposures over 4 months was associated with a 2.6% reduction in the odds of being a current smoker, with all other variables held constant. In a similar way, higher levels of exposure to Legacy-sponsored and pharmaceutical company advertisements were also associated with a lower probability of being a current smoker. By contrast, higher exposure to tobacco industry–sponsored advertising was positively associated with smoking—an average 4% increase in the odds of being a smoker for each increase of approximately 10 exposures over 4 months. Our substantive results were robust to the exclusion of both, or either, tobacco control policy variables and the 1998 state smoking prevalence variable, as well as to the choice of exposure measure.
Higher levels of exposure to state- and Legacy-sponsored antitobacco advertisements were positively associated with current smokers’ intention to quit. Exposure to advertisements for pharmaceutical cessation aids was unrelated to quitting intentions, but exposure to tobacco industry–sponsored advertising was positively associated with intention to quit smoking. Exposure to state-sponsored advertisements was unrelated to having made a quit attempt in the past 12 months, but exposure to Legacy-sponsored advertisements was positively associated with quit attempts. By contrast, exposure to advertisements for pharmaceutical cessation aids and tobacco industry–sponsored advertisements was negatively associated with quit attempts. None of the campaigns was associated with the amount smoked by current smokers.
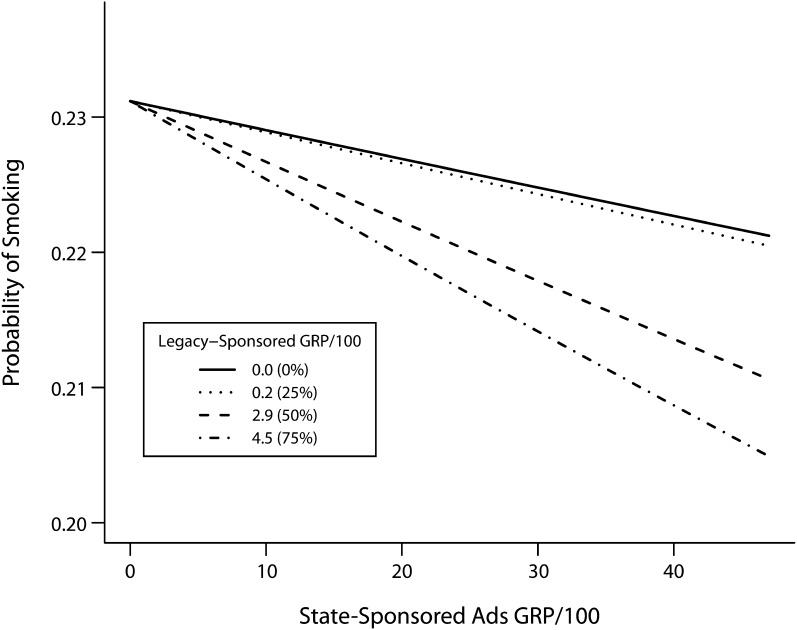
Our analyses showed no significant interactions between advertising sponsored by states and pharmaceutical companies, or for state- and tobacco industry–sponsored advertisements. Figure 2 illustrates the significant negative interaction between state- and Legacy-sponsored advertising (P = .05); the 4 lines represent the minimum, 25%, 50%, and 75% of the range of Legacy exposure; at lower levels of exposure to Legacy advertisements, the negative relationship between the probability of being a current smoker and exposure to state-sponsored advertisements was flatter than it was when levels of exposure to Legacy advertisements were higher.
FIGURE 2—
Interaction effect for state- and Legacy-sponsored advertisements United States, 1999–2007.
Note. The relationship between exposure levels for state-sponsored ads and smoking status varies by the amount of exposure to Legacy-sponsored ads:
DISCUSSION
Our models showed a significant negative relationship among US adults between exposure to state- and Legacy-sponsored antitobacco television advertising and the probability of being a smoker. Although the odds ratios for the relationship between exposure to antismoking advertising and adult smoking behaviors were smaller than those observed in similar analyses of youths,9 the effects were robust and important on a public health level. Furthermore, the relationship we observed was comparable to that found in other studies of exposure to antismoking media and smoking among adults.12,13 Previous work has shown that each of these campaigns helps reduce smoking among youths,9,26 but the current study provides the strongest evidence to date that tobacco control media contribute to reductions in adult smoking in the United States.
Between 1999 and 2007, the average level of exposure to state-sponsored antismoking advertising was approximately 4.2 ads per 4-month period, but the median level was 0.76; both of these measures reflect levels far below the CDC’s Best Practices recommendations.27 If states had followed the CDC recommendations and increased their campaigns by 8 to 10 exposures per 4-month period, bringing the average to 10 to 12 exposures, our results suggest that the odds of being a smoker would have been reduced by approximately 2.1%. When we used the 2007 population and policy variable averages in our models, this reduction translated to approximately 640 000 fewer smokers for a 4-month period of observation.
Our results also provided evidence that exposure to state- and Legacy-sponsored advertisements is associated with a higher likelihood of intending to quit, and that exposure to the Legacy-sponsored advertisements was associated with a higher probability of current smokers having made a quit attempt in the past year. Hyland et al. found comparable effects of televised tobacco control advertisements and adult smoking cessation.13 Our findings are also consistent with recent research from Australia, which showed that higher levels of recent exposure to tobacco control advertising were positively associated with quit attempts.28
Although our research suggested that exposure to advertisements for pharmaceutical cessation aids is negatively associated with the probability of being a smoker, it is notable that our models also showed that such exposure was unrelated to current smokers’ intentions to quit smoking, and negatively associated with quit attempts. There has been relatively little research on the relationship between advertising for cessation aids and quitting behavior. Wakefield et al. have shown that, in Australia, exposure to advertisements for nicotine replacement therapies was unrelated to quit attempts.12,28 Tauras et al.29 showed that higher exposure to ads for nicotine replacement patches was positively associated with per capita sales of these products, but there was no significant relationship between ads for nicotine gum and sales.
Our analyses did not differentiate between advertisements for different cessation products, and therefore may have masked the effects of advertisements for specific cessation products on quitting intentions. The significant negative relationship we found between exposure to advertisements for pharmaceutical cessation aids and having made a quit attempt in the past year supports a hypothesis that these products may provide smokers with a rationale for putting off quitting. Bolton et al. showed in an experimental setting that exposure to ads for pharmaceutical cessation aids was associated with increased smoking—a boomerang effect that the authors explained by suggesting that cessation aids may act as a “get out of jail free” card, encouraging smoking by conveying a message that the cessation products minimize the smokers’ risk of long-term addiction.30
In contrast with the desirable effects for advertisements sponsored by states and the American Legacy Foundation, our models showed that higher exposure to tobacco industry–sponsored advertising was associated with a significant increase in the probability of being a smoker. These are the first analyses of the effects of the tobacco industry–sponsored advertising on smoking among adults. The tobacco industry–sponsored advertisements included in our analyses encompassed youth-prevention, parent-targeted and corporate responsibility messages. Although each type of advertisement promoted a slightly different message and targeted a different audience, it can be argued that, collectively, these advertisements were part of the industry’s broader efforts to enhance their corporate image and credibility.8,31 Others have found that, among youths, such advertisements were associated with more favorable attitudes toward the industry. Furthermore, research among youths found that higher levels of exposure to tobacco industry advertising were associated with lower perceived harm from smoking, stronger approval of smoking, stronger intentions to smoke in the future, and increased probability of smoking.32 Although the tobacco industry currently sponsors no major television advertising campaigns, the robustness of the positive association between tobacco industry–sponsored advertising and increased smoking across adults and youths suggests that extreme caution is warranted if the tobacco industry offers any other measures that putatively promote prevention.
Our models of the interactions between smoking-related advertising suggest that exposure to Legacy-sponsored advertisements strengthens the effects of state-sponsored advertisements on reducing adult smoking prevalence. These results provide the first evidence that antitobacco advertising sponsored by the largest public health organizations in the United States have both independent and complementary effects. This finding is consistent with the theory of media priming, whereby exposure to one message can increase the salience of another related message.33
There are limitations to our analyses and their interpretation. Our use of cross-sectional data allows us to report associations, but not to make direct causal inferences. Also, we were unable to categorically reject the hypothesis that an unmeasured factor related to both smoking behavior and exposure to antismoking advertising better explains the relationships observed in our models. However, by including important control variables, we believe it is unlikely we misrepresented the relationships between exposure to antismoking advertising and smoking among adults. In addition, our results reflect the relationships between the mean exposure to tobacco-related advertisement for each media market and individual smoking behaviors; individuals may have actually seen many more or fewer of such advertisements. Finally, very few respondents to the TUS-CPS lived in media markets with very high levels of exposure to state-sponsored antismoking advertising; had there been a larger number of respondents in such areas, further exploration of the relationship between intensive exposure to state-sponsored antismoking advertisements and adult smoking behaviors might have been possible. More research is needed to better understand and model whether there are threshold or ceiling effects for smoking-related advertising.
Despite the limitations, this study represents the most comprehensive exploration to date of the relationship between smoking-related advertising and adult smoking behavior. Our findings suggest that the recent significant increases in funding for tobacco control media campaigns may contribute to meaningful reductions in smoking among US adults.
Acknowledgments
This study was funded by the National Cancer Institute (CA123444). Support was also provided by the Robert Wood Johnson Foundation.
We wish to dedicate this article to the memory of our esteemed colleague, Young Ku Choi, PhD (1971–2011).
Human Participant Protection
The research associated with this article was reviewed by the institutional review board of the University of Illinois at Chicago and determined to be exempt.
References
- 1.Pierce JP, Gilpin EA, Emery SLet al. Has the California Tobacco Control Program reduced smoking? JAMA. 2001;280(10):893–899 [DOI] [PubMed] [Google Scholar]
- 2.Ibrahim JK, Glantz SA. The rise and fall of tobacco control media campaigns, 1967–2006. Am J Public Health. 2007;97(8):1383–1396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sly DF, Hopkins RS, Trapido E, Ray S. Influence of a counteradvertising media campaign on initiation of smoking: the Florida “truth” campaign. Am J Public Health. 2001;91(2):233–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The Role of the Media in Promoting and Reducing Tobacco Use. Tobacco Control Monograph No. 19. Bethesda, MD: US Department of Health and Human Services, National Institutes of Health, National Cancer Institute. NIH publication no. 07–6242, June 2008; Available at: http://cancercontrol.cancer.gov/tcrb/monographs/19/monograph19.html. Accessed July 9, 2010 [Google Scholar]
- 5.Communities putting prevention to work: CDC awards $372.8 million to 44 communities. Atlanta, GA: Centers for Disease Control and Prevention; 2010. Available at: http://www.cdc.gov/Features/ChronicPreventionGrants. Accessed July 9, 2010 [Google Scholar]
- 6.Bruell A. FDA issues pair of proposals for $600 million combined anti-smoking push. Advertising Age, November 1, 2011. Available at: http://adage.com/article/news/fda-issues-proposals-600-million-anti-smoking-push/230763. Accessed January 23, 2012 [Google Scholar]
- 7.Wakefield M, Szczypka G, Terry-McElrath Yet al. Mixed messages on tobacco: comparative exposure to public health, tobacco company and pharmaceutical company sponsored tobacco-related television campaigns in the United States, 1999–2003. Addiction. 2005;100(12):1875–1883 [DOI] [PubMed] [Google Scholar]
- 8.Szczypka G, Wakefield MA, Emery S, Terry-McElrath YM, Flay BR, Chaloupka FJ. Working to make an image: an analysis of three Philip Morris corporate image media campaigns. Tob Control. 2007;16(5):344–350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Emery S, Wakefield MA, Terry-McElrath Yet al. Televised state-sponsored antitobacco advertising and youth smoking beliefs and behavior in the United States, 1999–2000. Arch Pediatr Adolesc Med. 2005;159(7):639–645 [DOI] [PubMed] [Google Scholar]
- 10.Wakefied MA, Loken B, Hornik RC. Use of mass media campaigns to change health behavior. Lancet. Published online October 7, 2010. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chaloupka FJ. Macro-social influences: the effects of prices and tobacco-control policies on the demand for tobacco products. Nicotine Tob Res. 1999;1(Suppl 1):S105–S109 [DOI] [PubMed] [Google Scholar]
- 12.Wakefield MA, Durkin S, Spittal Met al. Impact of tobacco control policies and mass media campaigns on monthly adult smoking prevalence: time series analysis. Am J Public Health. 2008;98(8):1443–1450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hyland A, Wakefield M, Higbee C, Szczypka G, Cummings KM. Anti-tobacco television advertising and indicators of smoking cessation in adults: a cohort study. Health Educ Res. 2006;21(3):348–354 [DOI] [PubMed] [Google Scholar]
- 14.Nielsen Station Index: US television household estimates. September 2007. New York, NY: Nielsen Media Research; 2007 [Google Scholar]
- 15.Szczypka G, Emery S, Wakefield MA, Chaloupka FJ. The Adaptation and Use of Nielsen Media Research Commercial Ratings Data to Measure Potential Exposure to Televised Smoking-Related Advertisements. Chicago, IL: University of Illinois at Chicago; 2003. ImpacTeen research paper no. 29 [Google Scholar]
- 16.Current Population Survey design and methodology, technical paper 66. Washington, DC: United States Census Bureau; 2006 [Google Scholar]
- 17.Orzechowski W, Walker R. The Tax Burden on Tobacco. Arlington, VA: Orzechowski and Walker; 2003 [Google Scholar]
- 18.Bureau of Labor Statistics Consumer Price Index database. Available at: http://www.bls.gov/cpi/home.htm#data. Accessed July 1, 2010
- 19.ImpacTeen Tobacco Control Policy and Prevalence Data: 1991–2008 Codebook and Definitions. Chicago, IL: University of Illinois at Chicago; 2009 [Google Scholar]
- 20.Pollay RW, Siddarth S, Siegel Met al. The last straw? Cigarette advertising and realized market shares among youths and adults, 1979–1993. J Mark. 1996;60(2):1–16 [Google Scholar]
- 21.Information Technology Laboratory of the National Institute of Standards and Technology Federal Information Processing Standards Publications. Washington, DC: FIPS PUBS; 2010 [Google Scholar]
- 22.Reducing the Health Consequences of Smoking: 25 Years of Progress—A Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Public Health Service; 1989. DHHS publication no. (CDC)89-8411 [Google Scholar]
- 23.Messer K, Trinidad DR, Al-Delaimy WK, Pierce JP. Smoking cessation rates in the United States: a comparison of young adult and older smokers. Am J Public Health. 2008;98(2):317–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reducing Tobacco Use: A Report of the Surgeon General. Atlanta, GA: National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2000 [Google Scholar]
- 25.Terry-McElrath YM, Wakefield MA, Emery Set al. State anti-tobacco advertising and smoking outcomes by gender and race/ethnicity. Ethn Health. 2007;12(4):339–362 [DOI] [PubMed] [Google Scholar]
- 26.Farrelly MC, Davis KC, Haviland ML, Messeri P, Healton CG. Evidence of a dose-response relationship between “truth” antismoking ads and youth smoking prevalence. Am J Public Health. 2005;95(3):425–431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention Best Practices for Comprehensive Tobacco Control Programs—2007. Atlanta, GA: National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; October 2007 [Google Scholar]
- 28.Wakefield MA, Spittal MJ, Yong H-H, Durkin SJ, Borland R. Effects of mass media campaign exposure intensity and durability on quit attempts in a population-based cohort study. Health Education Research. Advance access published July 5, 2011. Available at: http://www.ncbi.nlm.nih.gov/pubmed/21730252. Accessed July 12, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tauras JA, Chaloupka FJ, Emery S. The impact of advertising on nicotine replacement therapy demand. Soc Sci Med. 2005;60(10):2351–2358 [DOI] [PubMed] [Google Scholar]
- 30.Bolton LE, Cohen JB, Bloom PN. Does marketing products as remedies create “get out of jail free cards”? J Consum Res. 2006;33(June):71–81 [Google Scholar]
- 31.McDaniel PA, Malone RE. The role of corporate credibility in legitimizing disease promotion. Am J Public Health. 2009;99(3):452–461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wakefield M, Terry-McElrath Y, Emery Set al. Effect of televised, tobacco company-funded smoking prevention advertising on youth smoking-related beliefs, intentions, and behavior. Am J Public Health. 2006;96(12):2154–2160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fishbein M, Yzer MC. Using theory to design effective health behavior interventions. Commun Theory. 2003;13:164–183 [Google Scholar]